Abstract
This study investigates the impact of subsidising community-based health insurance (mutuelle) enrolment, removing point-of-service co-payments, and improving service delivery on health facility utilisation rates in Mayange, a sector of rural Rwanda of approximately 25,000 people divided among five ‘imidugudu’ or small villages. While comprehensive service upgrades were introduced in the Mayange Health Centre between April 2006 and February 2007, utilisation rates remained similar to comparison sites. Between February 2007 and April 2007, subsidies for mutuelle enrolment established virtually 100% coverage. Immediately after co-payments were eliminated in February 2007, patient visits levelled at a rate triple the previous value. Regression analyses using data from Mayange and two comparison sites indicate that removing financial barriers resulted in about 0.6 additional annual visits for curative care per capita.
Although based on a single local pilot, these findings suggest that in order to achieve improved health outcomes, key short-term objectives include improved service delivery and reduced financial barriers. Based on this pilot, higher utilisation rates may be affected if broader swaths of the population are enrolled in mutuelle and co-payments are eliminated. Health leaders in Rwanda should consider further studies to determine if the impact of eliminating co-payments and increasing subsidies for mutuelle enrolment as seen in Mayange holds at greater levels of scale. Broader studies to better elucidate the impact of enrolment subsidies and co-payment subsidies on utilisation, health outcomes, and costs would also provide policy insights.
Keywords: user fees, community-based health insurance, Rwanda, mutuelle, Mayange
Introduction
Amid the widespread poor health conditions of Sub-Saharan Africa, Rwanda has made notable progress. Through strong leadership, good governance and effective implementation, Rwanda has rebuilt its health system from the 1994 genocide and consequently has achieved significant improvements in many health indicators, including a drop in the under-five mortality rate by nearly 50% between 2000 and 2007 (Table 1). The level of contraceptive prevalence in Rwanda has been rising among women of all ages, nearly tripling from 13% to 36% between 2000 and 2008 (National Institute of Statistics of Rwanda [NISR] 2008). Childbirth conditions have improved significantly as the proportion of women giving birth in a health facility rose from 28% to 45% between 2005 and 2008 (NISR 2008). These results are especially attributable to comprehensive strategic improvements in the health system supported by substantial increases in healthcare funding (Table 2). This funding has resulted in increases in staff at health centres and hospitals, improvements in the national drug supply, and general infrastructure improvement including increases in running water and electricity for health facilities. Many chronic persistent health issues associated with poverty have persisted: nearly half the children under the age of five are stunted and about two-thirds of the population suffers from intestinal parasites (Ministry of Health [MoH] 2009).
Table 1.
Key health indicators in Rwanda, 2000–2007.
| 2000 | 2005 | 2007 | |
|---|---|---|---|
| Under-five mortality per thousand births | 196 | 152 | 103 |
| Infant mortality per thousand births | 107 | 86 | 62 |
| Stunting | 0.409 | 0.442 | – |
| Delivery in health facility | 27% | 28% | 45% |
| Fully immunised, 12–23 months | 76% | 75% | 80% |
| Access to safe drinking water | 40 | 34 | 41 |
| ARI, taken for treatment | 15 | 27 | 28 |
Data Source: NISR (2006, 2008), Hong et al. (2009).
Table 2.
Total health spending in Rwanda.
| Country | Total health spending per capita (US$) |
% from public | % from private | % from donor |
|---|---|---|---|---|
| 2000 | 9.49 | 18 | 30 | 52 |
| 2002 | 9.94 | 25 | 42 | 33 |
| 2003 | 16.94 | 32 | 25 | 42 |
| 2006 | 33.93 | 19 | 28 | 53 |
Data Source: MOH (2008a).
Investments in health have contributed to significant improvements in outpatient utilisation rates, which nearly tripled from 2001 to 2007 (Table 3). However, they still remain far below international norms. In 2007, the average Rwandan visited a health centre only 0.72 times per year, compared to an average of 3–5 visits per year for middle-income African countries with better-funded health systems (e.g., Botswana, South Africa; Doherty et al. 1996). Rwanda’s lagging utilisation rates remain largely attributable to financial constraints at all levels of the health system. However, Rwandan utilisation does not look dramatically different from neighbouring countries with higher per capita incomes, such as Tanzania (Table 4). Health spending has grown rapidly in the past decade and total per capita spending in 2007 was 35.87 USD, a rise from 9.49 USD in 2000 (MoH 2008a, WHO 2011). While point-of-service healthcare expenses have been broadly reduced, they may continue to be significant determinants of health-seeking behaviour, especially among the 57% of Rwandans who live in poverty (MoH 2009).
Table 3.
Mutuelle coverage, utilization and health spending in Rwanda, 2001–2007.
| Year | Mutuelle coverage (% of national population) |
Outpatient utilisation (annual visits per capita) |
Total health spending (per capita US$) |
|---|---|---|---|
| 2001 | Not reported | 0.25 | 8.76 |
| 2002 | Not reported | 0.28 | 9.94 |
| 2003 | 7% | 0.31 | 16.94 |
| 2004 | 27% | 0.39 | 15.95 |
| 2005 | 44% | 0.47 | 20.39 |
| 2006 | 73% | 0.61 | 33.93 |
| 2007 | 75% | 0.72 | 35.87 |
| 2008 | 85% | Not available | 45.42 |
Data Source: MOH (2008a, 2008b, 2009), WHO (2011).
Table 4.
Outpatient utilization and health spending in East Africa, 2007 (unless indicated).
| Country | Outpatient utilisation (annual visits per capita) |
Total health spending (US$ per capita) |
GNI per capita (current US$) |
|---|---|---|---|
| Rwanda | 0.72 | 35.87 | 360 |
| Uganda | 0.8 | 36.31 | 370 |
| Malawi | 0.92 | 16.56 | 230 |
| Tanzania | 0.77 (2005) | 19.60 | 410 |
While investments in the health system constitute critical steps towards improving population health, the impacts are ultimately constrained by demand-side factors that influence healthcare utilisation. One of the core objectives of Rwanda’s Health Sector Strategic Plan is thus to ensure ‘financial accessibility to health services for all,’ a goal for which the government of Rwanda (GoR) has instituted a set of strategic finance structures (MoH 2009). Preventative interventions in Rwanda such as antenatal care, immunisation and family planning are provided free of charge to the population. To cover patient costs for curative services, the GoR initiated a community-based health insurance programme known as Mutuelle de Sante (‘mutuelle’). Mutuelle premiums are 1000 RWF (1.69 USD) per person annually, and cover the majority of outpatient service costs at the primary care level. (The MoH recently announced plans to increase this premium, but have not yet specified the new rate and when it will take effect.) Mutuelle is a locally-based mechanism: each sector in the country (representing about 25,000 people) has a mutuelle committee that is responsible for accounting for mutuelle payments and reimbursements. Referral care for members is paid for by a combination of mutuelle financing and funds pooled at the district and national levels from donors and NGOs. With mutuelle, clients are also expected to cover a co-payment at each visit that is typically 200 RWF (0.33 USD) or 10% of the billable cost of service. The fees are designed to generate financing at the facility level as well as to compel people to ‘value’ care, avoid becoming dependent on free services, and diminish abuse of the system through overutilisation. Such an orientation towards self-sufficiency is partly based on a post-genocide resolve by Rwanda to not be reliant on donors for critical services. The country’s leadership thus aims to balance the goals of policies that are ‘pro-poor’ while inculcating a culture of independence, which it hopes will help Rwanda reach middle-income status by 2020 (MOFEP 2000).
Low facility utilisation rates translate directly to lower facility incomes and thus lower quality of care at health centres. These problems were confronted at the local level at the Mayange Health Centre, a Ministry of Health (MoH) primary care facility that was also supported by the Millennium Villages Project, which serves a sector with a population of 25,000, composed of five ‘imidugudu’ or small villages. Prior to January 2006, the Mayange Health Centre had a staff of four, left its doors shut and locked to the public most days (patients were expected to track down nurses in the community), and was devoid of most essential drugs. Due to a series of integrated interventions as well as additional funding and oversight, the quality of healthcare in Mayange improved dramatically from April 2006 to February 2007, but was not accompanied by dramatic increases in utilisation. Examples of major improvements included an end to drug stockouts, improvements in laboratory reagent availability and diagnostic capabilities, and round-the-clock staffing.
Concerns over the ability of poor households to access healthcare led to an additional initiative by the health centre to subsidise mutuelle enrolment premiums and suspend the associated co-payments which resulted in the tripling of utilisation within a single month. In order to understand the influence of the financial barriers on healthcare utilisation, we constructed a panel set of data on the health system and utilisation from health centres in Mayange and neighbouring comparison areas. Regression analysis of monthly clinic utilisation rates suggests that the removal of financial barriers increased utilisation of curative services by 0.6 visits per person per year. These findings provide evidence that nominal financial barriers can have significant impact on healthcare utilisation in areas of extreme poverty.
Between March 2007 and July 2007, three satellite health posts, each staffed by two nurses from the health centre, were set-up within the community in community-donated structures that could serve clients who lived farthest from Mayange Health Centre. The goal of these posts was to provide more immediately available care for minor health concerns and early identification of more serious problems to refer to the health centre. The posts were open between 9 am and 4 pm, and health issues covered initially at the health post included common colds, basic wound treatment and other routine ailments. Analysis of the health post utilisation is not contained in this paper. However, we contend that change in utilisation rates of the health centre followed suspension of co-payments and subsidisation of mutuelle enrolment premiums. Initial utilisation of health posts was 10–20 visits per day with little referral to the health centre and these visits are not included in this paper’s data on health centre utilisation. We therefore assert that if anything, the health posts likely reduced the utilisation of the health centre though we do not possess the data to definitively demonstrate this.
The remainder of this article provides additional background on the relationship between out-of-pocket healthcare expenses and healthcare utilisation in Rwanda; the experience in Mayange, Rwanda; and a description of the statistical methods used followed by a discussion of the results and implications for Rwandan health policy.
Out-of-pocket healthcare expenses and utilisation of healthcare
The mutuelle system in Rwanda was first initiated at a pilot scale in 1999 (Logie et al. 1999, Schneider et al. 2001a, Diop et al. 2007). While other forms of health insurance exist in the formal sector, mutuelle is currently the least expensive and most common form of health insurance in Rwanda, reaching 85% of the population in 2008 (Table 3). The system is designed explicitly as a policy instrument for meeting one of the key strategic programme areas in Rwanda’s Health Sector Strategic Plan, which is ‘to ensure financial accessibility to health services for all and sustainable and equitable financing of the health sector’ (MoH 2009). Annual mutuelle premiums are 1000 RWF (1.69 USD), with more than 20% of those enrolled in 2007 receiving sponsorship from government (9%), and donor and NGO programmes (13%). The premiums currently comprise less than 5% of total healthcare costs in Rwanda (MoH 2008a).
All indications suggest that the mutuelle system has been effective at increasing financial accessibility of healthcare in Rwanda. During the pilot phase, data from 54 health centres showed that individuals who participated in the mutuelle scheme were up to six times more likely to seek treatment when sick (Schneider et al. 2001b, Diop et al. 2007, Schneider and Hanson 2007).1 Since the pilot phase, as mutuelle coverage has expanded throughout the country, health facility utilisation has grown substantially. Inference here, however, is slightly confounded by the significant simultaneous investments in healthcare services, which have also increased demand as well as by the enforcement of laws requiring mutuelle enrolment. Total health spending has increased by more than 200% from 2000 to 2006. While the mutuelle system has reduced the point-of-service costs of healthcare by approximately 90% for the majority of health services (such as treatment of infections and wound care, delivery and c-sections which were previously charged at full cost) there remains a requisite co-payment of 10% of the cost of services billable to the mutuelle which tends to be 200 RWF (0.33 USD) for most ordinary visits. The co-payment is designed to generate revenue for the providing facility as well as create a financial stake in the utilisation of care so as to prevent ‘moral hazard’, – the overuse of healthcare that results from the patient not internalising the full cost of care (Schneider et al. 2001a). To-date, overutilisation does not seem to be an issue in Rwanda, and chronic problems, many of which are the consequences of poverty, continue to result in health burdens. Outside of urban areas, which are few, there is a very limited private healthcare sector; thus, the data on health centre utilisation paints an accurate view of actual utilisation of health services in rural Rwanda.
The potential problem with mutuelle co-payments is their influence on the allocation of healthcare: point-of-service payments discriminate against the poor, resulting in a disproportionate use of healthcare by the wealthy (Gilson 1996, Falkingham 2004). A lack of money was reported to be a barrier to healthcare among 83% of the lowest wealth quintile in the 2005 Rwanda DHS, compared to 52% of the highest wealth quintile (NISR 2006).
Even in the absence of co-payments there are meaningful economic costs, in the form of time and energy, to seeking healthcare. The cost of travel alone is a significant expense for the extremely poor in Rwanda who are more likely to live in rural areas. Nearly one quarter of all Rwandans live more than 5 km from the nearest health facility, and thusmust walk for more than an hour to seek care (World Bank and MOH 2009). In 2005, 46% of the lowest wealth quintile reported that geographic distance was a barrier to access compared to 28% of the top wealth quintile (NISR 2006). Furthermore, 80% of Rwandans are subsistence farmers with important opportunity costs borne by time spent seeking care away from the fields (UNDP 2007).
We are not aware of any previous studies on the impact of mutuelle payments (including co-payments) on clinic utilisation in Rwanda. The literature on the impact of user fees on health facility utilisation in developing countries is mixed. In cases where healthcare was originally free to the patient, the most common reported result from newly instituted user fees is a marked decrease in patient visits, while consultation rates almost invariably rise with their removal (Collins et al. 1996, Muela et al. 2000, Ridde 2003, Burnham et al. 2004, James et al. 2006). In some cases, however, utilisation eventually increases over time, which is often attributed to improvements in service delivery related to the effects of fees on provider incentives (Litvack and Bodart 1993, Levy-Bruhl et al. 1997, Chawla and Ellis 2000, Palmer et al. 2004). All of the evidence available suggests that, when fees for service are charged, the impacts disproportionately affect the poor (Gertler et al. 1987, Gilson 1996, Falkingham 2004). While exemption schemes for the poor have been proposed, many studies have described their limited success (Creese 1991, Gilson et al. 1995, Kivumbi and Kintu 2002, Bitran and Giedion 2003, Meesson et al. 2006). A confounding factor in drawing conclusions about user fees is the challenge of differentiating the relative impact of improvements in services from the financial barrier generated for poor households.
The importance of understanding the impact of mutuelle co-payments on health-seeking behaviour in Rwanda arises from the stated goal of the GoR for universal and equitable access to care, and the importance of identifying mechanisms and costs, for fulfilling that goal in cases where it is not fulfilled. Our goal here is to learn from the experience in Mayange to identify the extent to which financial barriers in general and mutuelle co-payment in particular may influence access to health care in the context of expanded health services. In light of the national objectives of a sustainably financed health system that ensures access to all, does the mutuelle co-payment fulfil its objectives?
Experience in Mayange, Rwanda
Mayange is a rural sector of approximately 25,000 people in Rwanda’s Eastern Province. Prior to 2006, Mayange Health Centre, the sole health facility for the area, struggled with minimal staffing (4 A2 nurses),2 frequent stock-outs of the GoR’s formulary of essential drugs for the health centre level, and limited supplies.3 Consequently, the facility saw only 0.24 annual visits per capita in 2005. Provincial indicators showed 23.3% under-five mortality, 12.5% infant mortality and 42.4% prevalence of childhood stunting (NISR 2006). This situation was caused by extreme poverty (i.e., food insecurity, poor sanitary conditions), multiple health emergencies (i.e., malaria epidemics) and an inadequate health system response. Community focus groups revealed that the latter resulted from insufficient resources and multiple barriers to access with fees and transportation highlighted as major obstacles. In order to address these challenges, the GoR partnered with the Millennium Villages Project, an international organisation affiliated with the Earth Institute at Columbia University and Millennium Promise.
From April 2006 until January 2007, comprehensive health system upgrades were made including an expanded pharmacy, health centre electrification, the introduction of a free ambulance service and expansion of health centre staff. Interventions were financed and implemented by health centre staff, local leaders and the Millennium Villages Project (Table 5). In Mayange, even with improved service quality in 2006, mutuelle coverage peaked at 57.3% with 32.3% of those enrolled receiving full subsidy from the government, donors, or NGOs. Due to the persistence of low utilisation, starting in February 2007 progressive mutuelle subsidies were offered based on household wealth and by April 2007 mutuelle enrolment approached 100%. Community-reported levels of household wealth placed families in categories ranging from ‘able to fully pay for mutuelle’ to ‘100% loan required’.4 Loans were provided against anticipated harvest gains and enabled farmers to pay within the year in cash or in kind with farm produce (dried maize or beans). If farmers purchased mutuelle or obtained it through credit, they qualified to receive seed and fertiliser loans. Taking these agricultural loans, however, was not required in order to receive mutuelle on credit. No cash was given to borrowers and all loans were administered directly in the form of insurance coverage, seeds, and fertiliser, minimising the chance they could be used for unintended purposes. The linkage of health and agriculture interventions was intended to be mutually reinforcing: farmers who prioritised their health (i.e., sought mutuelle coverage for their entire household) were incentivised to simultaneously improve their agricultural practices through securing loans for new seed and fertiliser. Existing mechanisms through GoR to provide free mutuelle (for example, for certain genocide survivors) were also reinforced. By allowing poor farmers to use their field productivity to purchase mutuelle, the system intentionally lowered the immediate financial barrier to health mutuelle purchase. In addition, on 16 February 2007, co-payments were suspended at Mayange Health Centre.
Table 5.
Health interventions in Mayange.
| Interventions | Dates |
|---|---|
| Emergency and supplemental feeding introduced | April 2006 |
| Community health representatives elected | April 2006 |
| Health Centre connected to the power grid | May 2006 |
| 8 nurses are added, making a total of 12. Nurses paid salary top-up | June 2006 |
| Ambulance introduced | June 2006 |
| Reliable medicine supply established | June 2006 |
| Administrative supplies provided | June 2006 |
| Furniture and equipment supplied | July 2006 to March 2007 |
| 3 nurses are added to staff, making a total of 15 | September 2006 |
| Artemisinin-based combination therapy for malaria introduced | October 2006 |
| Insecticide-treated anti-malaria bednets distributed | October 2006 |
| Services reorganised into departments | October 2006 |
| ‘Checklist’ medical record forms introduced | October 2006 to February 2007 |
| Pharmacy management and procurement system established | January 2007 to March 2007 |
| Subsidies and credit schemes established | February 2007 |
| Point-of-service co-payments suspended | February 2007 |
| Three satellite health posts established (outpatient data not included in analysis) | March 2007 to July 2007 |
| Nearly 100% Mutuelle coverage achieveda | April 2007 |
| HIV testing by sending out samples started | April 2007 |
| TB diagnosis and treatment introduced | May 2007 |
| Deworming conducted | July 2007 |
| In-house PMTCT and VCT launched | September 2007 |
The MVP provided agricultural loans of improved seeds and fertilizer to households in which all members were enrolled in mutuelle. Alternatively, households could add the subsidized cost of members’ mutuelle subscription to the loans of seed and fertilizer and receive a voucher which could be immediately redeemed at Mayange Health Centre for health insurance coverage. These loans for seed and fertilizer could be repaid after harvest in either cash or harvested crop, and individuals seeking such loans could simultaneously enroll in mutuelle with their premiums added to their agricultural debt.
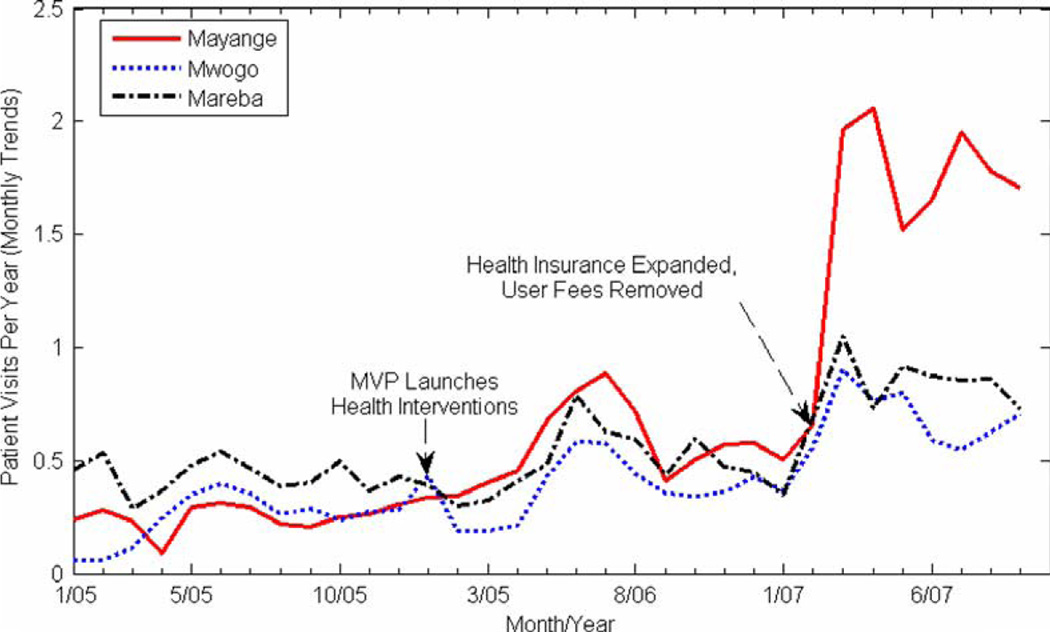
Mayange Health Centre records indicate that during the month previous to the removal of co-payments and the expansion of mutuelle, the health centre treated 1354 individuals, which is an annualised rate of 0.65 visits per person; a rate about equal to the health centres in the neighbouring sectors of Mwogo and Mareba. The following month, records reported a threefold increase to 4083 patient visits (annualised rate of 1.96 visits per person) in comparison with little or no change in Mwogo and Mareba (see Figure 1).
Figure 1.
Annualised utilization rates for Mayange and two neighbouring health centres between January 2005 and September 2007.
Methods
To more precisely measure the impact of the intervention on utilisation rates we conducted a regression analysis of outpatient utilisation rates in Mayange, Mwogo and Mareba. Mwogo and Mareba were selected as comparison sites because of their similar socio-economic status, close geographic proximity, similar burden of communicable disease, and equivalent baseline infrastructure, nursing staff and outpatient services.
From monthly MoH reports, we constructed a simple panel set consisting of data on outpatient utilisation rates and personnel for each of the health centre from January 2005 to September 2007 and estimated the following general dynamic panel data regression model:
| (1.0) |
where Yi,t represents the number of consultations in month t at health centre i, C represents the removal of financial barriers and Q is the number of nurses at the health centre, which is correlated with health centre budgets and serves as a proxy for quality of care. Nurses also directly reduce patient wait times and allow health centres to offer more clinical services and overnight emergency shifts that many Rwandan health centres cannot provide due to staffing constraints. The variable, η, is a clinic dummy variable and ε is the error term, which is assumed to be normally distributed with a mean of zero. Because health-seeking behaviour among a population may be a dynamic process that is based on the cumulative impact of interventions over time, the basic model includes a lagged value of health centre use, Yi,t − 1, as an explanatory variable. We used an Arellano-Bond General Method of Moments (GMM) estimator to generate unbiased coefficient estimates in the presence of autocorrelation. This technique first differences the data and then uses observations from previous years (i.e., Yi,t − 2) as instrumental variables to estimate the coefficient of the lagged dependent variable (Yi,t − 2). Because the data are first differenced, the fixed-effects feature, η, is lost and the estimation effectively becomes a random-effects model. GMM estimators are generally robust to heteroscedasticity.
Results
The results of the regression analysis are presented in Table 6, which shows that the removal of financial barriers had the single greatest impact on monthly utilisation rates. Its coefficient estimate of 0.6 indicates that the effect of the event of removing financial barriers resulted in a near 100% increase in utilisation from the rate of 0.65 visits per capita per year before the intervention. The lagged consultation rate accounted for a statistically significant increase of about 0.39 annual visits per capita. This may be explained by several phenomena including changes in health-seeking behaviours, community mobilisation efforts, gradual increases in mutuelle enrolment over time and the impact of upgrades not captured by the nurse proxy.
Table 6.
Regression results.
| Variable | Coefficient estimates |
| Health centre utilisation in previous month, Yi,t−1 | 0.393*** (0.088) |
| Removal of financial barriers, Ci,t | 0.595*** (0.118) |
| Number of nurses, Qi,t | 0.007 (0.008) |
| Constant | 0.009*** (0.003) |
| N | 84 |
Note: The estimated standard errors are presented below the corresponding coefficient estimates.
Significant at the 1% level
Arellano-Bond test indicates autocorrelation of order 1 (z = −3.85, Pr > z = 0.001) but not of order 2 (z = −1.51, Pr > z = 0.130).
The effects of these demand-side interventions are especially significant when compared to the supply-side investments. When improvements such as increased staffing, fortified drug supplies and electrification began in Mayange, utilisation was virtually identical for all three facilities. Over the first nine months of upgrades, utilisation steadily rose and nearly doubled from this baseline; however, a similar increase was seen in the neighbouring areas and, by February 2007, all three health centres had nearly equal utilisation.5 However, when mutuelle coverage was expanded and co-payments were removed in February 2007, patient visits in Mayange rose to three times their previous level before levelling to a sustained increase of two times the previous baseline. Holding the financial barriers constant, the regression results indicate no statistically significant effect of increased nursing staff on utilisation rates.
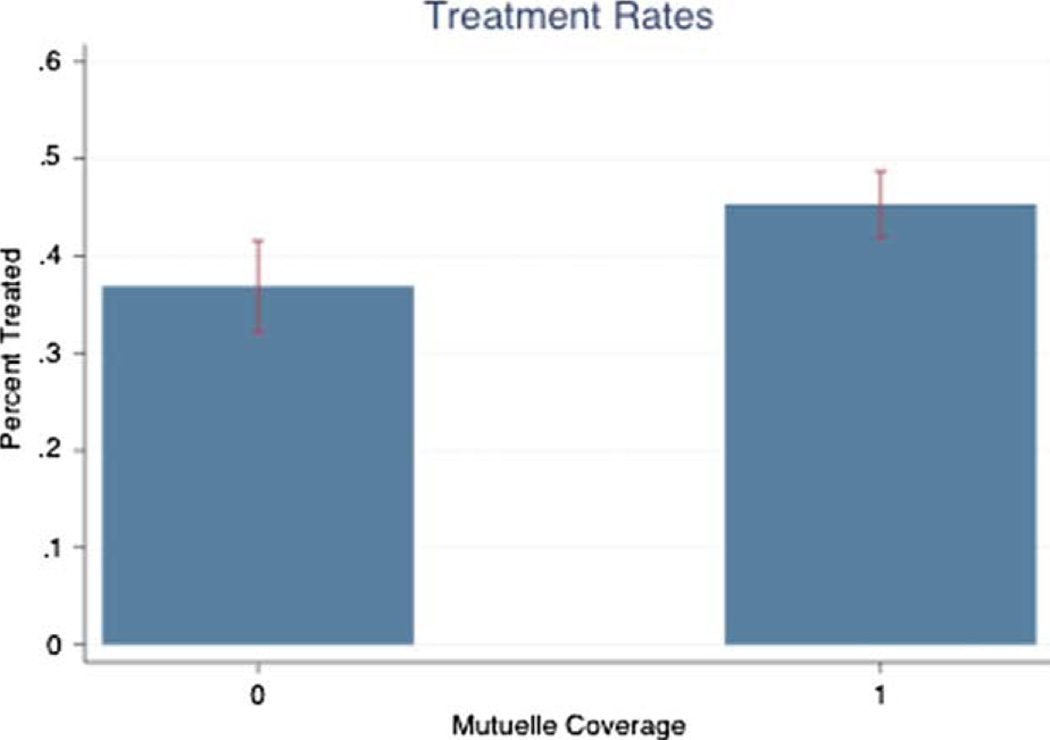
To get an additional indication of the independent impact of mutuelle on outpatient utilisation during the period of the intervention, we analysed the data on treatment rates of children with diarrhoea, fever and cough from the 2007 Interim DHS. These data, presented in Appendix 1, suggest that children covered by mutuelle are 30%–60% more likely to be treated when sick. These estimates are likely to be biased upwards because citizens can purchase mutuelle at the health centre, and thus are more likely to have mutuelle because they are sick. In other words, these data suggest that a 40% increase in mutuelle coverage would be expected to result in less than a 25% increase in utilisation. These results would not adequately explain the 200% increase in utilisation observed in Mayange after the financial barriers were removed.
Discussion
Fees appear to limit access
The existing literature remains inconclusive as to whether improvements in service delivery accompanied by user fees outweigh the barrier to access created by these fees. The sequence of implementation in Mayange provides an unusual comparison. Our analysis shows that improved services alone did not boost patient visits significantly more than what was seen at comparison sites without these upgrades. Only after financial barriers were removed did consultation rates in Mayange rise above these comparison sites.
Access implications of mutuelle
Because mutuelle enrolment was expanded near the time of co-payment removal, it is impossible to infer from the regression results alone (Table 6) the relative impacts of mutuelle enrolment versus co-payments, but there are convincing reasons to conclude that the co-payment removal had an independently important effect. Firstly, the mutuelle system was already a relatively popular programme in Rwanda prior to the intervention in Mayange, with an average national enrolment of 73% in 2006. Secondly, the mutuelle subsidy in Mayange occurred gradually between February 2007 and April 2007. Conversely, the suspension of the co-payment was an instantaneous event and the impact on health centre utilisation was correspondingly immediate: one week after co-payments were annulled, Mayange Health Centre saw an average of 141.7 visits per day, up from an average of 52.9 patients per day during the previous week. The nature of visits and pharmaceutical dispensation do not reflect any epidemiological changes, but rather, a simple rise in rate of utilisation of services for similar complaints as before the removal of co-payments.
Raw data from the ‘grey’ literature estimate that mutuelle facilitates access; utilisation in Rwanda was 0.72 annual visits per capita with 75% national coverage in 2007 (Table 4). In the three facilities in this study, rising enrolment in 2006 likely contributed to increases in facility utilisation as the year progressed, and some of this effect is captured by the coefficient of the lagged-dependent variable in the regression model.
These findings suggest that co-payments remain an important barrier to access. Furthermore, the impact of expanding coverage and raising utilisation rates – the focus of current subsidies – may be contingent on their concurrent elimination. This echoes previous warnings that higher coverage rates, which are often used to measure the success of insurance programmes, are not sufficient to improve access (ILO 2002). These results also add to the substantial literature already underscoring the hindrance posed by point-of-service charges. Furthermore, co-payments appear to make minimal contributions to local healthcare financing in 2008, co-payments in Mwogo and Mareba accounted for only 4% and 6% of health centre budgets, respectively.
Despite high insurance coverage rates nationally, previous studies in Rwanda have raised concerns over the affordability of mutuelle premiums and the financial hardship incurred by households who enroll nonetheless (Kalk et al. 2005, Schmidt et al. 2006). Our figures suggest that mutuelle subscriptions remained inaccessible for many more households than those 37% receiving sponsorships. Altogether, these findings indicate that, while mutuelle may improve access compared to traditional fee-for-service charges, it still poses financial barriers. These concerns are further exacerbated by the MoH’s recently announced plan to raise premiums.
Strengthening health services
The results suggest that strengthening service delivery, eliminating pre-payment barriers, and removing co-payments must happen together to enhance utilisation at the health centre level in rural Rwanda. Cases have been described where utilisation has overwhelmed capacity when financial barriers have been removed without concurrent increases in resources (Gilson and McIntyre 2005, IRIN 2006). Based on the Millennium Villages Project’s costing of inputs in Mayange, roughly 5 USD per capita for additional staff, salary increases, and essential drugs and supplies are needed to manage utilisation at the higher rates expected after financial barriers are removed. With close to 10 million people in Rwanda, this calls for approximately 50 million USD simply to keep up with the likely increased utilisation. The current cost of fully subsidising all mutuelle premiums and co-payments is estimated at 25 million USD. Thus, the total cost of absorbing the cost of co-payments, continuing to deliver care for the increased utilisation resulting from removing financial barriers, and the complete subsidisation of mutuelle, would cost roughly 75 million USD. The cost of a hybrid system which targets lower utilisation among those in most desperate need would be considerably less than this figure. Additional studies seeking to optimise utilisation while minimising public outlays could prove invaluable for future policy recommendations.
Conclusions
Rwanda has achieved astonishing progress in health indicators. Ongoing efforts in economic development, food security, and clean water and sanitation will undoubtedly go a long way towards improving the health of the average Rwandan. With many poor health outcomes caused by curable diseases, we believe that many gains can also be achieved by increased healthcare utilisation and improvements in service delivery. To do this, Rwanda must determine an approach to user fees that balances its competing priorities of expanding access without becoming reliant on aid or breeding a culture of dependence. Although drawn from a single site of only 25,000 people, these findings can serve as the basis for larger future pilots and help inform the government’s approach.
Among the possibilities, Rwanda could depart from its current system and instead provide centrally financed care that is free to the population. Although this would surely boost utilisation, it goes against the government’s commitment to self-sufficiency and would require sizable donor contributions for many years. Alternatively, Rwanda can seek a middle ground that establishes frequent and timely access for the poor, achieves excellent health and still avoids overdependence on aid.
Based on the presented evidence, Rwanda should pursue further studies to evaluate the possibility of eliminating mutuelle co-payments and increasing subsidies for enrolment while allocating more resources to primary care. Even at high coverage rates, mutuelle contributes nominally to overall health financing and already relies heavily on external subsidies to establish enrolment. Given this and the financial burden placed on households, the government could assess a strategy of expanding its package of free services to include curative care for common illnesses or provide all primary care free to priority populations (i.e., children and pregnant women). Given Rwanda’s track record to date and its clear commitment to expanding health care to its entire population, it seems likely Rwanda can pioneer a way forward that meets the immediate needs of its poorest households while still serving its ultimate goals of sustainability.
Appendix 1
The removal of co-payments coincided the expansion of mutuelle coverage, making it difficult to determine with certainty which of these financial barriers was most influential in changing utilization rates. To get a better sense of the impact of mutuelle on facility utilisation, we analysed data from the 2007/2008 Interim Demographic and Health Survey (NISR 2008) on children under five with fever, cough, or diarrhoea within 2 weeks of the survey. The bar graph (Figure 2) indicates that children with mutuelle are about 8 percentage points more likely to seek health care at a health care facility (health post, health centre, or district hospital). This represents a more than 22% increase in utilisation rates.
Figure 2.
Rates of facility utilisation of children under five with fever, cough, or diarrhoea. 1 refers to children with mutuelle and 0 refers to children without mutuelle. The red bars represent standard errors (0.05%). Data source: NISR (2008).
While Figure 2 reveals a statistically significant difference in rates of facility utilisation of children with mutuelle, the inference may be confounded by the fact that mutuelle coverage is also correlated with socio-economic factors, such as income and education, which are known to also contribute to health-seeking behaviour. To control for these potential confounding factors, we estimated the following linear model via a simple logistic regression analysis of children under five who had fever, cough, or diarrhoea 2 weeks before the survey:
| (A.1) |
where U is a dummy variable for whether the child sought care at health post, health facility, or district hospital, M is a dummy variable for whether the child had mutuelle, W is the household wealth status based on a composite index of household assets and E is the number of years of education of the mother. The results, presented in Table 7, indicate that children with mutuelle are 60% more likely to seek healthcare than children without it, after controlling for key socio-economic factors. This coefficient estimate represents an upper bound, due to an upward bias from potential endogeneity of the mutuelle variable, which may be the consequence of children seeking care.
Table 7.
Logistic regression results of treatment probabilities of children under five.
| Independent variables | Coefficient estimates |
|---|---|
| Covered by mutuelle, M | 1.592*** (0.234) |
| Wealth status, W | 0.925** (0.036) |
| Years of education of mother | 0.947* (0.029) |
| N | 950 |
Note: The estimated standard errors are presented below the corresponding coefficient estimates.
Significant at the 1% level.
Significant at the 5% level.
Significant at the 10% level.
Footnotes
These data were synthesised in Schneider and Hansen (2007) who found that members of the micro-insurance scheme visited health centres at an average annualised rate of 1.3 versus 0.2 of non-members. More recent data from the Interim DHS 2007 indicate that mutuelle increases treatment rates for children with diarrhoea, fever and respiratory problems by 30%–60% (Appendix 1).
Nurses have been ranked based on the years of training: A0 (bachelors degree), A1 (Registered Nurse with 4 years professional training) and A2 (high school training).
No drugs besides those on the government’s formulary list were stocked.
The project wealth ranking found dozens of families uncovered by government subsidies who clearly should have qualified for free mutuelle. In the years since, government has made improvements to its evaluation system to better identify the neediest.
During this period, the other health centres did not make any substantial upgrades nor receive new support from the millennium villages project nor from the GoR.
References
- Bitran R, Giedion U. World Bank Institute for Social Protection Discussion Papers. Washington, DC: The World Bank; 2003. Waivers and exemptions for health services in developing countries. [Google Scholar]
- Burnham GM, Pariyo G, Galiwango E, Wabwire-Mangen F. Discontinuation of cost sharing in Uganda. Bulletin of the World Health Organization. 2004;82(3):187–195. [PMC free article] [PubMed]
- Carlson C, Boivin M, Chirwa A, Chirwa S, Chitalu F, Hoare G, Huelsmann M, Ilunga W, Maleta K, Marsden A, Martineau T, Minett C, Mlambala A, von Massow F, Njie H, Olsen IT. Oslo: Norwegian Agency for Development Cooperation; 2008. Malawi health SWAp mid-term review summary report. [Google Scholar]
- Chawla M, Ellis RP. The impact of financing and quality changes on health care demand in Niger. Health Policy and Planning. 2000;15(1):76–84. doi: 10.1093/heapol/15.1.76. [DOI] [PubMed] [Google Scholar]
- Collins D, Quick JD, Musau SN, Kraushaar D, Hussein IM. The fall and rise of cost sharing in Kenya: the impact of phased implementation. Health Policy and Planning. 1996;11(1):52–63. doi: 10.1093/heapol/11.1.52. [DOI] [PubMed] [Google Scholar]
- Creese AL. User charges for health care: a review of recent experiences. Health Policy and Planning. 1991;6(4):309–319. doi: 10.1093/heapol/6.4.309. [DOI] [PubMed] [Google Scholar]
- Diop F, Leighton C, Butera D. Washington, DC: Health Financing Task Force; 2007. Health financing task force discussion paper: policy crossroads for mutuelles and health financing in Rwanda. [Google Scholar]
- Doherty J, Rispel L, Webb N. Developing a plan for primary health care facilities in Soweto, South Africa. Part II: applying locational criteria. Health Policy and Planning. 1996;11(4):394–405. doi: 10.1093/heapol/11.4.394. [DOI] [PubMed] [Google Scholar]
- Falkingham J. Poverty, out-of-pocket payments and access to health care: evidence from Tajikistan. Social Science and Medicine. 2004;58(2):247–258. doi: 10.1016/s0277-9536(03)00008-x. [DOI] [PubMed] [Google Scholar]
- Gertler P, Locay L, Sanderson W. Are user fees regressive? Journal of Econometrics. 1987;36(1–2):67–88. [Google Scholar]
- Gilson L. The lesson of user fee experience in Africa. In: Beattie A, Doherty J, Gilson L, Lambo E, Shaw P, editors. Sustainable health care financing in Southern Africa. Washington, DC: The World Bank; 1996. pp. 35–48. [Google Scholar]
- Gilson L, McIntyre D. Removing user fees for primary care in Africa: the need for careful action. British Medical Journal. 2005;331(7519):762–765. doi: 10.1136/bmj.331.7519.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilson L, Russell S, Buse K. The political economy of user fees with targeting: developing equitable health financing policies. Journal of International Development. 1995;7(3):369–401. [Google Scholar]
- Hong R, Ayad M, Rutstein S, Ren R. DHS Further Analysis Reports No. 66. Calverton, Maryland, USA: ICF Macro; 2009. Childhood mortality in Rwanda: levels, trends, and differentials; further analysis of the Rwanda Demographic and Health Surveys, 1992–2007/08. [Google Scholar]
- Integrated Regional Information Networks (IRIN) Side effects of free maternal, child healthcare. [Accessed 28 May 2011];2006 [online]. Available from: http://www.irinnews.org/report.aspx?reportid=59267.
- International Labour Organization (ILO) Geneva: International Labour Office Universitas Programme; 2002. Extending social protection in health through community based health organizations. [Google Scholar]
- James CD, Hanson K, McPake B, Balabanova D, Gwatkin D, Hopwood I, Kirunga C, Knippenberg R, Meessen B, Morris SS, Preker A, Souteyrand Y, Tibouti A, Villeneuve P, Xu K. To retain or remove user fees? Reflections on the current debate in low- and middle-income countries. Applied Health Economics and Health Policy. 2006;5(3):137–153. doi: 10.2165/00148365-200605030-00001. [DOI] [PubMed] [Google Scholar]
- Kalk A, Mayindo JK, Musango L, Foulon G. Paying for health in two Rwandan provinces: financial flows and flaws. Tropical Medicine and International Health. 2005;10(9):872–878. doi: 10.1111/j.1365-3156.2005.01464.x. [DOI] [PubMed] [Google Scholar]
- Kivumbi GW, Kintu F. Exemptions and waivers from cost sharing: ineffective safety nets in decentralized districts in Uganda. Health Policy and Planning. 2002;17(Suppl. 1):64–71. doi: 10.1093/heapol/17.suppl_1.64. [DOI] [PubMed] [Google Scholar]
- Levy-Bruhl D, Soucat A, Osseni R, Ndiaye J, Dieng B, De Bethune X, Diallo AT, Conde M, Cisse M, Moussa Y, Drame K, Knippenberg R. The Bamako Initiative in Benin and Guinea: improving the effectiveness of primary health care. International Journal of Health Planning and Management. 1997;12 Suppl. 1:S49–S79. doi: 10.1002/(sici)1099-1751(199706)12:1+<s49::aid-hpm466>3.3.co;2-g. [DOI] [PubMed] [Google Scholar]
- Litvack J, Bodart C. User fees plus quality equals improved access to health care: results of a field experiment in Cameroon. Social Science and Medicine. 1993;37(3):369–383. doi: 10.1016/0277-9536(93)90267-8. [DOI] [PubMed] [Google Scholar]
- Logie DE, Rowson M, Ndagije F. Innovations in Rwanda’s health system: looking to the future. Lancet. 1999;372(9634):256–261. doi: 10.1016/S0140-6736(08)60962-9. [DOI] [PubMed] [Google Scholar]
- Meesson B, Van Damme W, Tashobya CK, Tibouti A. Poverty and user fees for public health care in low-income countries: lessons from Uganda and Cambodia. Lancet. 2006;368(9554):2253–2257. doi: 10.1016/S0140-6736(06)69899-1. [DOI] [PubMed] [Google Scholar]
- Ministry of Finance and Economic Planning, Republic of Rwanda (MOFEP) Rwanda Vision 2020. Kigali: MOFEP; 2000. [Google Scholar]
- Ministry of Health and Social Welfare, United Republic of Tanzania. Annual health statistical abstract. Dar es Salaam: Policy and Planning Department; 2006. [Google Scholar]
- Ministry of Health (MoH), Republic of Rwanda. Kigali: MoH; 2008a. National health accounts Rwanda 2006 with HIV/AIDS, malaria, and reproductive health subaccounts. [Google Scholar]
- Ministry of Health (MoH), Republic of Rwanda. Annual report 2007. Kigali: MoH; 2008b. [Google Scholar]
- Ministry of Health (MoH), Republic of Rwanda. Kigali: MoH; 2009. Health sector strategic plan July 2009– June 2012. [Google Scholar]
- Ministry of Health, Republic of Uganda. Kampala: MoH; 2008. Annual health sector performance report financial year 2007/2008. [Google Scholar]
- Muela SH, Mushi AK, Ribera JM. The paradox of the cost and affordability of traditional and government health services in Tanzania. Health Policy and Planning. 2000;15(3):296–302. doi: 10.1093/heapol/15.3.296. [DOI] [PubMed] [Google Scholar]
- National Institute of Statistics of Rwanda (NISR) Calverton, Maryland, USA: NISR and ORC Macro; 2006. Rwanda demographic and health survey 2005. [Google Scholar]
- National Institute of Statistics of Rwanda (NISR) Kigali: NISR; 2008. Preliminary results of interim demographic and health survey 2007–2008. [Google Scholar]
- Palmer N, Mueller DH, Gilson L, Mills A, Haines A. Health financing to promote access in low income settings: how much do we know? Lancet. 2004;364(9442):1365–1370. doi: 10.1016/S0140-6736(04)17195-X. [DOI] [PubMed] [Google Scholar]
- Ridde V. Fees-for-services, cost recovery, and equity in a district of Burkina Faso operating the Bamako Initiative. Bulletin of the World Health Organization. 2003;81(17):532–538. [PMC free article] [PubMed]
- Schmidt JO, Mayindo JK, tand Kalk A. Thresholds for health insurance in Rwanda: who should pay how much? Tropical Medicine and International Health. 2006;11(8):1327–1333. doi: 10.1111/j.1365-3156.2006.01661.x. [DOI] [PubMed] [Google Scholar]
- Schneider P, Diop F, Leighton C. Technical Report No. 66. Bethesda, MD: Partnership for Health Reform (PHR), Abt Associates Inc; 2001a. Pilot testing prepayment for health services in Rwanda: results and recommendations for policy directions and implementation. [Google Scholar]
- Schneider P, Diop F, Maceira D, Butera D. Technical Report No. 61. Bethesda, MD: Partnership for Health Reform (PHR), Abt Associates Inc; 2001b. Utilization, cost, and financing of district health services in Rwanda. [Google Scholar]
- Schneider P, Hanson K. The impact of micro health insurance on Rwandan health centre costs. Health Policy and Planning. 2007;22(1):40–48. doi: 10.1093/heapol/czl030. [DOI] [PubMed] [Google Scholar]
- United Nations Development Programme (UNDP) National Human Development Report. Kigali: UNDP; 2007. Turning Vision 2020 into reality: from recovery to sustainable human development. [Google Scholar]
- World Bank. Data: GNI per capita. [Accessed 28 May 2011];2007 [online]. Available from: http://data.worldbank.org/indicator/NY.GNP.PCAP.CD.
- World Bank and Ministry of Health. Kigali: The World Bank; 2009. Country status report on health and poverty in Rwanda. [Google Scholar]
- World Health Organization (WHO) National health accounts: country health information. [Accessed 28 May 2011];2011 [online]. Available from: http://www.who.int/nha/country/en/