Abstract
This study was done to find out modern demographic trends of aspiration and different foreign bodies posing a risk. For this study, 94 patients with suspected foreign body aspiration (FBA) were selected. Detailed history, especially age, suspected Foreign body (FB) and mode of onset were noted and a thorough clinical examination was done. X-ray chest and neck, antero-posterior and lateral view was the only investigation done in all. Rigid bronchoscopy under general anaesthesia was done in all the cases of suspected FBA for diagnostic cum therapeutic purpose. Among 94 patients 70.2% i.e. 66 were within 5 years of age and most were within 2–3 years of age. Rigid bronchoscopy was done in all the cases and foreign body was successfully retrieved in 78.7% of cases. Bronchoscopy was negative in the rest of the cases. The Most common site of lodgment was the right bronchus followed by the left bronchus, the trachea and other sites. Vegetables were the most common FBs as they were found in 26 cases. Whistles from small plastic toys were the single most common FB(15). Other foreign bodies were small plastic and metallic parts, safety pins, jewellery etc. Children under 5 years of age are at greatest risk of FBA. Different vegetables and whistles of low grade toys are the most commonly aspirated FB. Detailed history is most important for diagnosis. X-ray is not a reliable tool for diagnosis. Bronchoscopy should be done whenever a foreign body is suspected in the airway.
Keywords: Bronchoscopy, Foreign body aspiration, Demography, Children
Introduction
Foreign body (FB) in the air way is an emergency situation. A sizeable number of patients succumb to death before they reach any medical centre. Management consists of resuscitation followed by preparation of the patient for bronchoscopic removal of foreign body as early as possible. The paediatric population suffers from foreign body aspiration (FBA) most commonly. Aspirated FBs vary from region to region as well as on the age groups. Nonetheless few FBs are found frequently on bronchoscopy.
Aims and Objectives
This study was designed with following aims.
Modern demographic trends of aspiration.
To find out different foreign bodies posing a risk.
Materials and Methods
This study was done on 94 patients with suspected FBA who were managed at ENT dept. of IPGMER and SSKM Hospital, Kolkata. This is the apex hospital in West Bengal and caters not only to this state but other neighboring states like Bihar, Jharkhand and the northeastern region of India. The study period was 2 years, from September 2006 to October 2008. Cases were collected from emergency care and ENT OPD as well as from the dept. of Paediatrics and Chest Medicine.
A detailed history, especially mode of onset of symptoms was taken and a thorough clinical examination was done. Their signs and symptoms were noted as history of choking; cough and respiratory distress; unilateral wheeze, added sounds and diminished air entry in one lung on auscultation. Emergency condition at the time of presentation like severe respiratory distress, stridor, cyanosis etc. were noted also.
Foreign bodies above the larynx were not included in this study.
Presentation
The classic triad of presentation is choking/cough, unilateral wheeze and diminished air entry in one side of lung. Few patients presented in emergency care with severe respiratory distress and cyanosis.
Pediatricians often refer the cases of lobar pneumonia not responding to conservative management.
A good number of cases presented with just suggestive history of FBA without any other symptoms. They generally describe a history of sudden choking during eating or playing with toys made of small parts. The symptoms subside after about half an hour and patient may even forget the event till the further complications develop. In this study 12 cases were referred by pediatrician, 44 cases were received in emergency condition and rest of the patients had attended OPD.
Investigations
A wet film X-Ray of chest and neck antero-posterior and lateral view were done in all the cases. Cases were classified in two groups according to the X-ray findings.
Group one: consists of 24 cases where X-ray finding was abnormal. Findings were radio opaque FB, pneumonic changes and unilateral hyperinflation of lung.
Group two: contains 70 cases where FBA was suspected clinically as radiologically no abnormality was detected.
Bronchoscopy
Rigid bronchoscopy under general anaesthesia is the gold standard diagnostic and therapeutic procedure for FBA. Rigid bronchoscopes of different internal diameters (3, 4, 5, 6, and 8 mm) and different lengths were chosen depending on the age of patients. It is mandatory to keep one size larger and one size smaller than the estimated one. A tracheostomy set is always kept ready for emergency purpose.
Routine preoperative preparations are sufficient for most of the cases. Special care is required for patients presenting with respiratory tract infection due to old/vegetable FB. The vegetable FBs are hygroscopic and swell up causing blockage of the lumen of the bronchus. Antibiotics are given parenterally. Nebulization is done with adrenaline, bronchodilators and steroids. This helps to reduce edema and infection of the tracheo-bronchial tree.
All the bronchoscopies were done by a well trained team consisting of an experienced anaesthesiologist and surgeon. Very good co-ordination between the two is a must. It was done under general anaesthesia with a ventilating bronchoscope. The type of FB and site of lodgments were noted.
Post operative managements are minimal in successful cases. Intravenous fluids, steroids and antibiotic were prescribed for 1–2 days, and then changed to oral medications. Nebulization with bronchodilators and steroids control edema and help rapid recovery. Four cases who suffered severe hypoxic injury during bronchoscopy were shifted to ITU.
Results and Analysis
Sex Incidence
Females (52) out numbered males (42).
Age Incidence
70.2% patients belong to less than 5 years of age. Among these most were within 2–3 years of age. We have found no patient below 1 year and above 13 year of age. So airway foreign body is predominantly a problem of younger children. Age incidence is described in Table 1.
Table 1.
Age incidence (n = 94)
| Age groups (years) | 1–2 | 2–3 | 3–5 | 5–10 | 10–13 |
|---|---|---|---|---|---|
| No. of pts. | 9 | 36 | 21 | 22 | 6 |
Outcome
In group 1: foreign body was removed in 22 cases and no FB was seen in 2 cases.
In group 2: foreign body was retrieved in 52 cases and bronchoscopy was negative in 18 cases.
In total a foreign body was retrieved successfully in 74(78.7%) of cases.
Different Foreign Bodies
Different types of foreign bodies retrieved by bronchoscopy are tabulated below (Table 2). Vegetable foreign bodies are most common as it was seen in 26 cases. Common vegetable were peas, Bengal gram, ground nut, beetle nut, different coated seeds and other food stuffs. Here pneumonic changes occur earlier which is detected by X-ray chest.
Table 2.
Incidence of different foreign bodies retrieved by bronchoscopy
| Types of F.B. | Vegetables | Whistle | Small plastic parts | Small metallic parts | Jewellery | Safety pins | LED | Miscellaneous |
|---|---|---|---|---|---|---|---|---|
| Numbers | 26(35%) | 15(20%) | 12(16%) | 10(14%) | 2(3%) | 3(4%) | 2(3%) | 4(5%) |
Whistles (from toys) are very common foreign bodies in children. It was seen in 15 cases. Above 3 years of age it is the single most common FB. Above this age they learn to blow the whistle of toys. Most of these toys make sound both during blowing in as well as blowing out and they are aspirated during deep inspiration. Patients can often blow them voluntarily. Small plastic parts, mostly from pens were seen in 12 cases. X-ray changes are late here.
Other foreign bodies were safety pins (3), LED i.e. light emitting diode (2), small metallic parts (10), jewellery (2) and miscellaneous (4).
Site of Lodgments
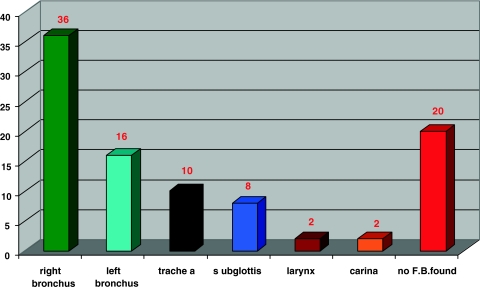
The most common site is the right bronchus due to its anatomical alignment with the trachea. The next common sites are the left bronchus, trachea, subglottis, larynx, and carina (Chart 1).
Chart 1.
Different site of lodgments of foreign bodies (n = 94)
No foreign body was found in 20 cases.
Discussion
Provisional diagnosis of FBA was done in 94 cases based on history and thorough examination. Rigid bronchoscopy was performed in all these cases and the FB retrieved in 78.7% cases. Evan et al. removed FB by bronchoscopy in 57% of cases with suspected FBA [1]. Clinical diagnosis was done in 70 cases where X-ray showed nothing significant. In this group foreign body was successfully removed in 52 (74.2%) of cases. No foreign body was found in 18 cases. The positive predictive accuracy of clinical diagnosis is 74.2%. So bronchoscopy should be done in all the suspected cases of FBA.
Demographic trends of FBA are very significant. All are paediatric cases, within 1–13 years of age. 70.2% children belong to less than 5 years and most (38.2%) within 2–3 years of age. Morley RE et al. have done rigid bronchoscopy in 51 children under 3 years of age between July 1997 and July 2001 and found FB in 22 children [2]. Children under 2 years of age can not grind and swallow hard, crunchy food as they lack the second molar teeth and are still adjusting to the descent of larynx. They suggested that children under 3 years of age should never be fed nuts and other hard crunchy foods. Their eating should always be supervised.
In this study females (52) out numbered males (42). This may reflect a social factor as most of the cases came from poor socioeconomic class where female child are neglected more than the male one.
Whistles from toys are the single most common FB found in children above 3 years of age. Above this age they learn to blow the whistle of toys. Most of these toys make sound both during blowing in as well as blowing out and it is aspirated during deep inspiration. They can often make sound voluntarily. Sound of whistle is heard during cough or deep inspiration also. We have found a 10 years boy who was able to make peculiar whistling sound form his chest. This boy was used to earn money in local village fairs showing this unnatural power.
An extensive educational campaign is required regarding FBA, their presentation, and feeding of children. Cheap quality toys with whistle should be banned by the government as it was the single most common FB found in the tracheo-broncheal tree. In Israel in 1982–83 intensive educational campaign was done through television, radio broadcast and news papers. This initiative reduced incidence of FBA in Israel [3].
Vegetable FBs are most commonly aspirated. These are very dangerous as most of them are hygroscopic. They swell up within a few days causing blockage of the lumen of the bronchus and retention of secretion distal to it. Secondary infection occurs easily leading to lobar pneumonia.
Signs and symptoms of FBA are not always straight forward. Asymptomatic bronchial foreign bodies are found frequently. Cylindrical tubular FB may remain asymptomatic as air pass freely through it [4].
In our study 65% of the cases had no distress at the time of examination. They presented with a history of choking followed by an acute episode of coughing which subsided after a few hours. After the initial paroxysm of coughing the tracheo-bronchial mucosa becomes tolerant of the FB and coughing ceases. This feature is often responsible for delays in diagnosis. Pediatricians should be aware of the fact and think of foreign body in the air way in the cases of pneumonia not responding to conventional management. Mukherjee A et al. extracted the nozzle of a pen in a case of four and half year old boy presenting with recurrent cough and cold for 2 years [5]. Rothmann BF [6] in their review article described that 18% cases were diagnosed after 1 week and 8% after 1 month of the event. Thorough clinical examination can detect reduced air entry and/or added sound in one lung. Only ten cases (9.4%) were received in emergency condition with history of FBA and severe respiratory distress. Other cases presented with mild stridor, dry cough, whistling sound during cough.
Common presentations as found in this study are history of choking (100%), cough (25%) and respiratory distress (19%), blow whistle (3.8%), diminished air entry in one lung (59%), wheeze/added sound (49%). Black et al. described symptom triad—coughing, choking and wheeze in 91% of patients presented with FBA [7].
Key Messages
Under five paediatric patients are at greatest risk of FBA. Children under 3 years of age should not be given hard crunchy foods as they can not grind and swallow this type of food. Whistles of low grade soft toys are the single most common foreign bodies found in airway. Guardians should be aware of this fact.
Detailed history is most important for diagnosis. Roentgenography is not a reliable method for diagnosis of FBA. Bronchoscopy should be done whenever foreign body is suspected in the airway.
Management of a foreign body in the airway is a discipline unto itself. Cases should be referred to a highly specialized centre with sophisticated setup.
References
- 1.Even L, Heno N, et al. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatr Surg. 2005;40(7):1122–1127. doi: 10.1016/j.jpedsurg.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 2.Morley RE, Ludmann JP, Moxham JP, Kozak FK, Riding KH. Foreign body aspiration in infants and toddlers: recent trends in British Columbia. J Otolaryngol. 2004;33(1):37–41. doi: 10.2310/7070.2004.00310. [DOI] [PubMed] [Google Scholar]
- 3.Sadan N, Raz A, Wolach B. Impact of community educational programme on foreign body aspiration in Israel. Eur J Paediatr. 1995;154:859–862. doi: 10.1007/BF01959798. [DOI] [PubMed] [Google Scholar]
- 4.Mathiasen RA, Cruz RM. Asymptomatic near-total airway obstruction by a cylindrical tracheal foreign body. Laryngoscope. 2005;115(2):274–277. doi: 10.1097/01.mlg.0000154732.16034.83. [DOI] [PubMed] [Google Scholar]
- 5.Mukherjee A, Basu AK, Chakraborty S. Non-resolving pneumonia in a young boy–beware of foreign body aspiration. J Indian Med Assoc. 2006;104(3):145–147. [PubMed] [Google Scholar]
- 6.Rothmann BF, Boeckman CR. Foreign bodies in the larynx and tracheobrochiiall tree in children. A review of 225 cases. Ann Otol Rhinol Laryngol. 1980;89:434–436. doi: 10.1177/000348948008900512. [DOI] [PubMed] [Google Scholar]
- 7.Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. Am J Surg. 1984;148:778–781. doi: 10.1016/0002-9610(84)90436-7. [DOI] [PubMed] [Google Scholar]