Abstract
Wegener’s granulomatosis is an uncommon Condition characterized by necrotising granulomatosis of upper and lowers respiratory tract and glomerulonephritis. We present here a unique case of 50 year old female with localised involvement of nose and adjoining area.
Keywords: Wegener’s granulomatosis, Nasal cavity
Case Report
A 50 year Hindu female patient presented with history of nasal obstruction and nasal discharge for 2 years, swelling in both cheek and nostril and loss of sense of smell for 6 months. She also complained of headache and deafness for the last 6 months.
On examination, general condition was poor. There was oedema and excoriation of skin around both nostrils. Nasal cavity was full of foul smelling secretion and crusts. There was septal perforation and perforation of hard palate. Infraorbital area of both sides were swollen Figs. 1, 2, and 3.
Fig. 1.
Clinical picture showing excoriation and crusts on nasal cavity
Fig. 2.
Clinical picture showing palatal perforation
Fig. 3.
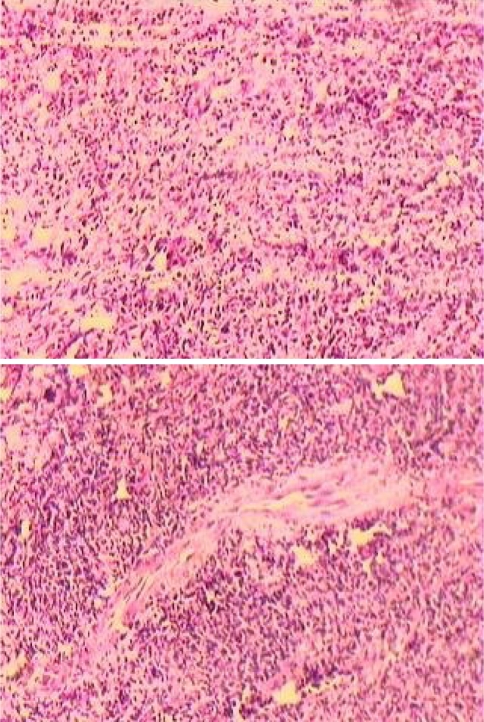
Photomicrography showing granulomatous inflammation and vasculitis
Routine blood, urine, stool examination were within normal limits. Nasal smear for AFB and fungal culture were negative. Chest X-ray and USG of whole abdomen was normal. C-ANCA was negative. Biopsy was taken from nasal cavity and it revealed Wegener’s granulomatosis. Diognosis was done according to ACR (1990) criteria [1]. The patient was treated with prednisolone and azathioprine and showed clinical improvement.
| 1990 ACR criteria for the classification of Wegener’s granulomatosis (number of criteria present rule) | |
|---|---|
| Criteria | Definition |
| Nasal/Oral inflammation | Development of painful or painless oral ulcer or purulent or bloody nasal discharge. |
| Abnormal chest X-ray | Roentgenogram of chest showing the presence of nodules, fixed infiltrates or cavities. |
| Urinary sediment | Microhaematuria (over five red blood cells/HPF) or red cell casts in the urine sediment. |
| Granulomatous inflammation on biopsy | Histologic changes showing granulomatous inflammation within the wall of an artery or in the peri-or extravascular area (artery or arteriole) |
For the classification purpose, a patient shall be said to have Wegener’s granulomatosis if he/she has satisfied any two or more of these four criteria. This rule is associated with a sensitivity of 88.2% and a specificity of 92%.
Discussion
Wegener’s granulomatosis was first described by Klinger in 1933, followed by other investigators including Rossle in 1933, Wegener in 1936 and 1939, and Ringertz in 1947 [2].
It is characterized by granulomatous inflammation involving the respiratory tract and necrotising vasculitis affecting small to medium size vessels with necrotising glomerulonephritis. The pathological hallmark is the coexistence of vasculitis and granulomas and classically involves a triad of airway, lung and kidney.
There is a strong and specific association with autoantibodies directed against proteinase-3 (C-ANCA) [3]. In Wegener’s granulomatosis C-ANCA test is positive in 95% of cases with generalised active disease. This sensitivity falls to 60% with localised disease affecting respiratory tract [4]. Most patients are white and the sex distribution is equal, and most present in the fifth decade, although the age range extends to both extremes [5].
The upper airway disease is the most common presenting feature of Wegener’s granulomatosis. This includes sinusitis, oral lesions, otitis media, hearing loss, epistaxis, and saddle nose deformity. Sinusitis is the most common initial presentation in about half to two-third of patients with Wegener’s granulomatosis [5, 6].
Pulmonary involvement is one of the cardinal features of Wegener’s granulomatosis. Cough, haemoptysis and pleuritis are the most common pulmonary symptoms. There may be cavitary lesions in lung. Renal disease also may be seen as the initial presentation or during the course of the disease in the form of glomerulonephiritis and may result in end stage renal failure.
Our case is peculiar in the fact that there is only nasal involvement without any lung or kidney involvement and the case is C-ANCA negative.
Glossary
- USG
Ultrasonography
- C-ANCA
Cytoplasmic-staining anti-neutrophil cytoplasmic antibody
- ACR
American College of rheumatology
- HPF
High power field
- AFB
Acid fast bacilli
References
- 1.Leavitt RY, Fauci AS, Bloch DA, Michel BA, Hunder GG, Arend WP, et al. The American college of rheumatology 1990. Criteria for the classification of Wegener’s granulomatosis. Arthritis Rheum. 1990;33:1101–1106. doi: 10.1002/art.1780330807. [DOI] [PubMed] [Google Scholar]
- 2.Lie JT. Illustrated histologic classification criteria for selected vasculitis syndromes. Arthritis Rheum. 1990;33:1074–1087. doi: 10.1002/art.1780330804. [DOI] [PubMed] [Google Scholar]
- 3.Hewins P, Tervaert JW, Savage CO, Kallenberg CG. Is Wegener’s granulomatosis an autoimmune disease? Curr Opin Rheumatol. 2000;12:3–10. doi: 10.1097/00002281-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Howard DJ, Lund VJ (2008) Granulomatous conditions of nose. In: Scott Brown’s otolaryngology, head and neck surgery, vol 2. Hodder Arnold, London, pp 1651–1652
- 5.Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener’s granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992;116:488–498. doi: 10.7326/0003-4819-116-6-488. [DOI] [PubMed] [Google Scholar]
- 6.Fauci AS, Haynes BF, Katz P, Wolff SM. Wegener’s granulomatosis: prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med. 1983;98:76–85. doi: 10.7326/0003-4819-98-1-76. [DOI] [PubMed] [Google Scholar]