Abstract
Aim
To generate a theoretical model how patients experience their management of rheumatoid arthritis (RA) in everyday life.
Method
An explorative design with the grounded theory approach was used by interviewing 16 informants with RA.
Results
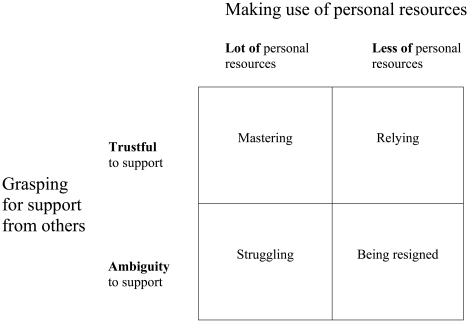
The generated theoretical model emerged in a core category- Striving for a good life with two categories; making use of personal resources and grasping for support from others, which formed the base of managing RA. When relating these categories together, four dimensions emerged which characterised patients’ different ways of managing RA: mastering, relying, struggling and being resigned.
Discussion
The management of RA incorporated the use of personal resources and the grasping for support from others. Both self-management strategies and patients’ need of support were highlighted as aspects that were of importance when managing RA. Patients’ experiences of their need of support to manage RA give extended knowledge that is of importance for nurses and other healthcare providers. The relationship between patients and healthcare providers is always the key to a good encounter. Interventions to increase self-management in RA have to incorporate this knowledge when trying to increase patients’ self-efficacy and with their experience of support.
Keywords: Rheumatoid arthritis, patient perspective, grounded theory, chronic disease.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic illness and the most common of the inflammatory rheumatic joint diseases, affecting 0.5- 1% of the population [1, 2]. Pain, impaired physical function and fatigue are some of the symptoms of RA. The treatment consists of both pharmacological therapies and non-pharmacological therapy [3]. Despite that patients have new possibilities in the medical treatment, the disease is still chronic and they have to deal with the consequences in everyday life. The disease implies different patterns of flares, which leads to unpredictability that requires a continuous adaptation to the disease, both from patients as well as from nurses and other healthcare providers [3]. The knowledge about how people experience living with RA and deal with the consequences of the disease is divergent. This is illustrated by Dildy [4], who describes having RA as a suffering, while Stamm et al. [5] reports a process of mastery. Several studies have also shown that healthcare providers and patients have different views of the impact of rheumatic diseases [6-9].
For several decades the management of chronic diseases has been discussed in terms of coping [10]. Several studiesin the field of coping and RA have tried to explain the correlation between coping style and disease outcome, but the results are dubious [11-14]. Ramjeet et al. [14] concluded that there was limited evidence that coping strategies contributed to the prediction of disease outcome. Maybe this shortcoming of evidence is related to the concept of coping itself. Lazarus and Folkman (1996) grounded the concept of coping in relation to dealing with stressful events, but living with and managing RA is maybe not always a stressful event. There is a need of a more comprehensive understanding about the management of RA and a broader view in the discussion of chronic illness experience is of importance [10]. Self-management and self-care have been highlighted as important factors for patients in their management of chronic illness [15]. In order to support self-care and self-management we have to know more from the patient’s inside view [10]. There is a need to increase the knowledge from the patient perspective and develop a more person-centred care in the rheumatology field [16-18]. The aim of this study was to generate a theoretical model how patients experience their management of RA in everyday life.
MATERIALS AND METHODOLOGY
Design and Method Description
An explorative design with the grounded theory (GT) approach by Corbin and Strauss [19] was used. GT has been developed from symbolic interactionism which requires the individual to develop through social interaction and the creation of meaning [19, 20]. The main purpose of doing GT studies is to generate concepts, models or theories developed from empirical data in order to explain the phenomenon under study. Data collection and data analysis is a process that intertwines the two with each other. The collection of data begins with a purposeful sampling followed by theoretical sampling. Theoretical sampling includes both new collection of data as well as a theoretical sampling of the existing data when a theory is arising to look for aspects to confirm the arising theory or to object to the theory. The steps of data analysis are: open coding, axial coding and selective coding. Throughout the analysis process asking questions about the data and constant comparison are of importance. Questions useful to ask could be: “What is going on?” and “Who are the actors involved and what is the meaning to them?” The constant comparison means to compare each situation with other situations for similarities and differences. During the analysis process ideas, preliminary assumptions and theoretical reflection are written down in memos in order to help with the generation of a theoretical model [19].
Informants and Data Collection
During autumn 2009 and spring 2010, 16 informants were asked to participate in an interview and all agreed to join the study. The inclusion criteria for participation were that they were diagnosed with RA and could speak the Swedish language. To gain the variation of different ways of management, a purposeful sample was used with regard to: age, sex and disease duration. The overview of background factors (Table 1) shows that the mean age for women was 62 years (28-82) and for men 61 years (42-70). They had different levels of education and civil status. Disease duration varied between 2-42 years with a mean value of 14 years. They all were treated at a rheumatology hospital either at the day-care clinic or at the rehabilitation department and were contacted by a nurse in adjacent to their planned visit. They received written information and if willing to attend, the nurse at the hospital got in contact with the first author (UB) who contacted the informants to give more information and set the day and place for the interview. The interviews were done by the first author at the rheumatology hospital in a private room. Each interview lasted between 20 and 50 minutes and was transcribed verbatim. The interview began with the opening question, “How do you manage your rheumatic disease, RA?” Questions that followed were given in order to deepen the answers, “Can you tell me more about that?” and “What did you do then?” so as to gain rich meaning and experiences from the informants.
Table 1.
Characteristics of the 16 Informants with Rheumatoid Arthritis (RA)
| Informant | Sex | Age (Years) | Education Level * | Marital Status | Disease Duration (Years) |
|---|---|---|---|---|---|
| 1 | Male | 67 | 1 | Married | 15 |
| 2 | Female | 77 | 1 | Divorced | 7 |
| 3 | Female | 65 | 3 | Divorced | 15 |
| 4 | Female | 64 | 1 | Married | 16 |
| 5 | Female | 82 | 1 | Married | 19 |
| 6 | Male | 65 | 2 | Married | 10 |
| 7 | Male | 58 | 2 | Single | 10 |
| 8 | Male | 70 | 3 | Married | 6 |
| 9 | Male | 66 | 1 | Married | 24 |
| 10 | Male | 42 | 2 | Cohabitant | 2 |
| 11 | Female | 46 | 1 | Married | 15 |
| 12 | Female | 28 | 2 | Married | 2 |
| 13 | Female | 63 | 3 | Divorced | 27 |
| 14 | Female | 73 | 1 | Married | 42 |
| 15 | Female | 58 | 1 | Married | 10 |
| 16 | Female | 60 | 1 | Married | 3 |
Education level: 1 = Comprehensive school, 2 = Upper secondary school, 3 = University degree.
The informants were interviewed at one occasion but had the opportunity to contact the interviewer if further questions or comments occurred. One informant contacted the interviewer to clarify the time of diagnose of RA.
Data Analysis
The open coding began directly with the first interview, through reading the text line by line to identify words, phrases and sentences which were then labeled with codes that captured the meaning according to the aim. By asking questions about the data this coding process moved on to the next level of analysis where these codes were clustered into higher categories (axial coding). In the axial coding process two categories were defined; making use of personal resources and grasping for support from others, as important parts of the management process. In the selective coding process the core category, striving for a good life, emerged as the overall theme. The theory arose when linking the core category with these two categories; making use of personal resources and grasping for support from others together. Through theoretical sampling in the selective coding process four dimensions of managing of RA emerged by constant comparison and asking theoretical questions to the data. Throughout the data collection and analysis the first author wrote memos according to GT methodology. After 13 interviews and analyses no more meaningful information was gained indicating theoretical saturation. An additional three interviews were conducted to ensure that the information from the patient was theory based.
Ethical Considerations
The study was approved by the regional Ethics Committee at Lund University (LU-2009/391). The study was explained both verbally and in writing to informants and informed consent was obtained. They were informed that participation was voluntary and that they could withdraw without any further explanation. Confidentiality was guaranteed and it was emphasized that none of the informants would be identifiable. None of the researchers were involved in the care of the informants.
RESULTS
The generated theoretical model emerged in a core category, striving for a good life. A good life was expressed as making the best of the situation. They gained a sense of meaning when they strove forward to a good life despite the disease. The management of RA was an ongoing process involving all parts of life and not only the disease. The process began with an individual reflection in making use of the personal resources. Patients’ personal resources including illness perceptions, self-confidence and self-efficacy were used to analyse and deal with situations in everyday life. There were differences in personal resources within as well as between patients, depending on the situation they experienced. Illness perception was described as different ways to understand and explain the disease in everyday life. Self-confidence was expressed by patients in terms of believing and fighting for themselves or in the opposite way, by not believing and not fighting for their rights. Self-efficacy was framed as believing in their capability to change the situation or in the opposite way, by not mentioning their capability at all.
The process of managing RA also involved a grasping for support from others. Patients described the need of support from relatives and friends when doing household duties or other things in everyday life. They also expressed a need for support from nurses and other healthcare providers including non-medical as well as medical treatment. There was a relationship between the grasping for support from others and the outcome of the support where patients were either trustful or ambiguous to the support given. The personal resources and the outcome of the support formed the base of how they chose to manage their striving for a good life.
When relating the core category and the two categories together (making use of personal resources and grasping for support from others) four dimensions emerged which characterised patients’ different ways of managing RA: mastering, relying, struggling and being resigned (Fig. 1). These different ways of management could change over time. The four dimensions were not completely fixed and in each patient there could be a transition between the various dimensions. When other situations in life happened, like hassles and crises that disturbed the everyday life, the need of grasping for support and their personal resources could change.
Fig. (1).
Striving for a good life contains a process of making use of personal resources in relation to grasping for support of others four dimensions emerged.
Mastering
This way of managing RA was characterised by experiencing their situation in a way of acceptance. They used their personal resources, felt confident in themselves and expressed trustfulness in the support from others in their striving for a good life. Patients described personal resources, such as having a positive attitude to life and an optimistic personality, that were used as sources to manage the disease as well as other problems in life. Mastering was a way of management that could involve a long process before it was reached. A woman expressed,”…but I can’t stop and live… I have to overcome so to speak…through building up in some way a confidence in oneself, that you can fix this. I think that you can be quite capable if you focus and most things are able to be solved with a little thought.” There were patients that drafted a more direct way of mastering. A woman said, ”So, it is just so recently... but I’ve accepted it…and it’s just so nice…already from the beginning so to speak… It was just obvious that I would have medicine that would help…and it has done a great deal of good…I have all support from home... and I have been able to work... it means a great deal to not feel sick.” Patients described their need to continue with leisure-time activities and to feel that they still were in charge over their lives. In having a chronic disease with disabilities they believed and framed a need for support in everyday life, as well as quick support from healthcare providers when symptoms arose or when there were problems with the medications. Hence, the mastering way of managing RA was to put the person’s life in front of the disease and not focus on the disease. Patients showed both faith and gratitude to the support around them.
Relying
This way of managing RA in striving for a good life was depending on others and the patients experienced trustfulness in their grasping for support from healthcare providers, relatives and friends. The support from healthcare providers was equally valued as the support from relatives and friends. Patients did not mention their own capability or their own responsibility in the management of RA, but that they depended on others. They described their experience of the healthcare as good, felt secure and expressed gratitude to have access to their healthcare. Patients had experienced episodes of caring where nurses suggested helpful hints which they could not have figured out by themselves. There was also a gratitude to the medical treatment and care they were offered, but they still related some worry about the future. A man treated with an intravenous medicine each 8 weeks at the rheumatology clinic expressed, ”Some week before I come here I feel... how I start to have pain in my joints again... just a little bit, swollen up some joint like that... know that I soon am coming to the nurse (name given) and then it becomes good again. You can’t do anything about it (the disease)... it was when I received this (the medicine) then…a real miracle for me…if you don’t get this… How would it have been then?…The future, yes... that maybe you are a little worried about... regarding the medicines, if it stops working or side effects…a little worried.” Relatives were also important and often mentioned in relation to the need for more personal care or help with household work. A woman claimed, ”I have had terrifically good help…it means so much of course…so what I can’t do, he does (the husband), so I have very good help in the household and things like that... only a thing like going to the store…I can carry one or two kilograms, but that is nothing if you are going to shop for the household... and so, therefore, you are very dependent on someone else.” Accordingly, the relying way of managing RA showed that patients striving for a good life were depending on the good support they had. Their own responsibility was not in focus when expressing their ways of managing RA.
Struggling
This way of managing RA was characterised by patients that were in an active role in order to gain respect, particularly from others. They expressed high self-confidence, but they were in ambivalence. In one way they wanted to look after themselves, but they were still depending on the support from others. One aspect of this struggling was described in not reaching the right support from healthcare providers. They had to fight for seeing a doctor whom they felt trust in. One man said, ”He didn’t give any confidence as a doctor should do... it became totally wrong... for me it didn’t feel right... it became so that I wasn’t welcome anymore... but I care how they treat me... it maybe is the difference in those who are 70 years old or more… I say no.” Another way of struggling was for independence. They described a strong belief in managing RA themselves with a minimum of support from others. Their personal resources were not in balance with their need of support, so they were struggling with accepting support from relatives when offered. They wanted to manage more than they could and battled with the fact that they had a chronic disease. The struggle could also incorporate different illness perceptions in relation to the healthcare system. Patients were not satisfied with how the healthcare providers expressed themselves in the encounter with the patient. A woman formulated her experience like this, ”I see myself as healthy... I consider myself to be in very good health... I am the type of person who has a difficult time in how people express themselves... it shows a lot about what kind of view of humanity a person has... I consider that everyone all around should express themselves in the right way.” Thus, the struggling way of managing RA was for the patients a battle that was hard to accept and they were fighting for respect. The outcome of the struggle was of importance when they tried to strive for a good life.
Being Resigned
This way of managing RA expressed less of personal resources in combination with ambiguity to the support from others. Patients experienced a wish for something to happen and they did not think that they had the possibility to choose or the ability to change this on their own. Patients were describing this kind of management in the beginning of the disease and often they moved forward to another way of management, but still there were patients in this dimension a couple of years after the diagnosis. They expressed that their RA led to various types of restrictions. They could not, for example, do certain specific physical activities any longer, discussed in a way of letting the disease take a greater part in their lives and how the disease became the main focus. A woman commented,” Yes, I have adjusted my life entirely... I live through the rheumatism.” In regard to their need for support from others they expressed difficulties in being taken seriously by relatives as well as healthcare providers. Friends and relatives could have difficulties to understand the problems the disease created and that could lead to social restrictions in life. As one woman said,”What do you do all day?’ people say. They don’t understand that... that everything takes time... A person isn’t so quick and you have to take little detours. But I never can manage so much as I would like, am never finished with anything... there isn’t enough energy?”
There were also difficulties in the encounter with healthcare providers by not being taken seriously, as well as the problems reaching the rheumatologist and getting an appointment at the clinic. As a result, this way of management possessed characteristics of the patients letting the disease take a great part in life and that they felt ambiguity to the support from others they received. Their striving for a good life was sometimes not fulfilled.
DISCUSSION
Striving for a good life was expressed as an ongoing process through managing everyday life with RA. Both self-management strategies and patients’ need for support from others were highlighted as aspects that were of importance when managing RA. In the four dimensions of managing RA, mastering, relying, struggling and being resigned, the patients expressed different ways of management and included tasks that patients undertake in their everyday life to control or reduce the impact of the disease.
This present study showed a need of both personal resources as well as a need of support from others to manage RA, which has also been reported by Ryan et al. [21]. To control the disease patients expressed a need to reduce physical symptoms, have sufficient social support and a good medical consultation. The good consultation included patient involvement, feedback, reassurance, empathy and access to an expert. The consequences of living with a chronic condition were expressed in the need of external support to positively influence the more personal control [21]. The findings in the present study are in discordance with the more common way of explaining coping as a passive or active action. Passive coping is referring to external control and active coping to an internal control [22]. The consequences of using the terms of coping in an active or passive action could lead to a belief that management of the chronic disease is up to the person himself to deal with, leading to a misunderstanding of the patient’s need of care. The present study showed the importance of the support from others and that the medical encounter was of great importance when discussing the patient’s way of managing RA.
It is common to offer interventions like patient education with the purpose of strengthening patients’ self-management through increasing their level of self-efficacy [3]. In the present study the use of personal resources incorporated illness perception, self-efficacy and self-confidence and they were expressed differently between the four dimensions. Patients with the relying and/or being resigned way of managing RA showed a lack of self-confidence and self-efficacy and could probably gain most of interventions with the purpose of increasing self.-efficacy. Illness perceptions could also interfere with things related to suggesting medications, physical exercise or other advice that healthcare providers recommend as treatments.
Mastering RA included reconciliation in the patients’ everyday life with the disease. This process was influenced by the patients’ personal resources and their trust in the support from others as they decided to take an active part in their management. This result is supported by Kralik et al. [23] that presented self-management as an action to create order. Patients’ personal resources included self-confidence and self-efficacy as a source from which to draw strength. They had a belief in themselves that could be used in their everyday life. Verduin [24] showed that patients with more sense of purpose in life had an association with better mental health status and an optimistic coping style. Similar results were shown by Stamm et al. [5] where they concluded that people with RA could explain their disease as a source for new challenges as one typology of patients’ life stories of RA. Patients mastering their disease experienced their grasping for support from others in a positive way in that they had family and friends they could rely on and that their experiences with healthcare providers were good. They saw themselves as an active partner in the medical encounter and felt trust and hope for the future. Lempp et al. [25] confirmed this way of managing in the present study by showing that patients no longer are seeing themselves as passive patients of care and that they are welcoming an equal dialogue with healthcare providers.
Relying was a way of managing RA expressed by depending on others and patients did not mention their own responsibility to manage the disease. Patients expressed both trust and gratitude for the support from relatives as well from healthcare providers. Ryan et al. [21] showed that medical consultation, when including the patient to interact and with a feeling of partnership, was an important factor that positively influenced patients’ perception of control over their situation. In this way of managing RA the patient did not talk about their level of control, but they expressed their dependency on others, in a positive way, in their striving for a good life. Covic et al. [11] discussed that since treatment of RA has been predominantly influenced by pharmacological treatment, patients consequently trust external resources rather than their own personal resources. In the present study patients that were using relying as their way of managing RA seemed rather satisfied with their situation. For patients with this way of management of the disease, interventions that increase self-efficacy could be useful in order to encourage them to use their personal resources when needed.
The patients that used the struggling way of managing RA were contending with a struggle to gain respect from others, expressed ambivalence in the need of support from others and experienced a battle for independence. Similar results are shown in a study by Ward et al. [26] who reported that patients gained a sense of control by refusing interventions or medication when not feeling listened to in the meeting with healthcare providers. The difficulties in the medical encounter are highlighted by others as an important issue to gain a more equal dialogue between patients and healthcare providers [7, 25]. The struggling way of managing RA was also related to patients’ illness perceptions. If the illness perception was incongruence with the healthcare providers’ view of the disease there was also a struggle for respect. This incongruence is also shown in other studies that highlight the differences between patients’ explanations and the medical explanation of the disease [7, 27, 28]. The patients with this struggling way of managing RA could be a challenge for healthcare providers, but healthcare providers should act in a professional way, focus on the patient’s needs and build a trusting relationship with the patient. The struggling way of managing RA could also involve a lack of acceptance of having a chronic disease and is therefore more common in the beginning of the disease but could, as shown in the present study, even exist after several years of the disease.
The being resigned way of managing RA is defined by having less of personal resources and less of good experiences of support from others. Patients described lack of strength to do things and that they surrendered completely to the disease. This is the opposite way of management compared to the mastering way of managing RA, where patients take control over the situation. In the being resigned way patients describe an adjustment to the disease, did not think they could change their situation and they had no faith in the healthcare system. Stamm [5] showed similar results describing patients expressing RA as “something to get use to” as one typology of the life story with RA. Being resigned could involve helplessness, a concept which is shown to correlate with depression, decreased physical and functional status and with greater levels of pain [4, 29]. Individuals that view themselves as less capable of caring for themselves may also suffer from poorer health [30]. Suffering from RA is shown as a process in three phases: disintegration of personhood, the shattered self and reconstruction of self [4]. Being resigned involves the first two steps but not the reconstruction phase. This could be of importance to recognise and could create a possibility to increase the patients’ belief in themselves through self-management interventions. It could be of importance to achieve trustful relationships with nurses in order to move from this way of management of RA to a more beneficial way of management.
Methodological Considerations
The present study had a qualitative design using grounded theory as the approach to answer the research question. In order to meet the methodological considerations of data collection and analysis, the following four terms were used: applicability, reasonableness, trustworthiness and conscientiousness [31]. Applicability was addressed by using relevant method for the aim of the study, as well as using purposeful and theoretical sampling in order to obtain a good representation of informants with different experiences of everyday life with RA. Reasonableness was ensured by describing the concordance between the data collection method and the area of investigation and through continuous movement back and forth between the whole and the parts during the constant comparison analysis [19]. Trustworthiness was guaranteed by the systematic and methodical approach to data analysis and by the co-researchers who had earlier experience with this method. Conscientiousness and honesty towards the informants was important from the start of the research process, through the different stages of analysis and to the presentation of a clear and comprehensive picture. This was achieved by indentifying statements from the informants and making continuous comparisons between data, codes and categories throughout the analysis process. The informants’ integrity was respected all through the research process. A possible limitation in the study was that all interviews where done at the same hospital but the patients in the study had experiences from other settings to.
CONCLUSIONS
Striving for a good life was the core category of patients’ management of RA and incorporated the making use of personal resources as well as the grasping for support from others. When linking together the outcome of the personal resources and the support four dimensions emerged: mastering, relying, struggling and being resigned. These four dimensions showed different ways of managing RA that could change over time and involved different aspects of the human being and not only the disease.
ACKNOWLEDGEMENT:
None declared.
IMPLICATION FOR CLINICAL PRACTICE
Patients’ experience of their need for support from others to manage RA gives extended knowledge that is of importance for nurses and other healthcare providers. The relationship between patients and healthcare providers is always the key to a good encounter. Interventions to increase self-management in RA have to incorporate this knowledge when trying to increase patients’ self-efficacy and with their experience of support from others. The findings in this study could be used in the development of a more person-centred care and there is an opportunity for nurses in rheumatology care to strengthen patients’ own resources and supporting their need of support from others.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Simonsson M, Bergman S, Jacobsson LT, Petersson IF, Svensson B. The prevalence of rheumatoid arthritis in Sweden. Scand J Rheumatol. 1999;28(6 ):340–3. doi: 10.1080/03009749950155319. [DOI] [PubMed] [Google Scholar]
- 2.Englund M, Joud A, Geborek P, Felson DT, Jacobsson LT, Petersson IF. Prevalence and incidence of rheumatoid arthritis in southern Sweden 2008 and their relation to prescribed biologics. Rheumatology (Oxford) 2010;49(8 ):1563–9. doi: 10.1093/rheumatology/keq127. [DOI] [PubMed] [Google Scholar]
- 3.Hill J. Rheumatology Nursing: A Creative Approach. 2. Chichester: Whurr Publishers Limited; 2006. [Google Scholar]
- 4.Dildy SP. Suffering in people with rheumatoid arthritis. Appl Nurs Res. 1996;9(4 ):177–83. doi: 10.1016/s0897-1897(96)80043-7. [DOI] [PubMed] [Google Scholar]
- 5.Stamm T, Lovelock L, Stew G, et al. I have mastered the challenge of living with a chronic disease: life stories of people with rheumatoid arthritis. Qual Health Res. 2008;18(5 ):658–69. doi: 10.1177/1049732308316348. [DOI] [PubMed] [Google Scholar]
- 6.Carr A, Hewlett S, Hughes R, et al. Rheumatology outcomes: the patient's perspective. J Rheumatol. 2003;30(4 ):880–3. [PubMed] [Google Scholar]
- 7.Fair BS. Contrasts in patients' and providers' explanations of rheumatoid arthritis. J Nurs Scholarsh. 2003;35(4 ):339–44. doi: 10.1111/j.1547-5069.2003.00339.x. [DOI] [PubMed] [Google Scholar]
- 8.Heller JE, Shadick NA. Outcomes in rheumatoid arthritis: incorporating the patient perspective. Curr Opin Rheumatol. 2007;19(2 ):101–5. doi: 10.1097/BOR.0b013e32802bf79d. [DOI] [PubMed] [Google Scholar]
- 9.Hewlett S, Cockshott Z, Almeida C, et al. Sensitivity to change of the Rheumatoid Arthritis Self-Efficacy scale (RASE) and predictors of change in self-efficacy. Musculoskeletal Care. 2008;6(1 ):49–67. doi: 10.1002/msc.125. [DOI] [PubMed] [Google Scholar]
- 10.Larsen P. Illness behavior. In: Lubkin I, Larsen P, editors. Chronic Illness Impact and Intervention. Boston: Jones and Bartlett Publishers; 2009. pp. 25–42. [Google Scholar]
- 11.Covic T, Adamson B, Hough M. The impact of passive coping on rheumatoid arthritis pain. Rheumatology (Oxford) 2000;39(9 ):1027–30. doi: 10.1093/rheumatology/39.9.1027. [DOI] [PubMed] [Google Scholar]
- 12.Carlisle AC, John AM, Fife-Schaw C, Lloyd M. The self-regulatory model in women with rheumatoid arthritis: relationships between illness representations, coping strategies, and illness outcome. Br J Health Psychol. 2005;10:571–87. doi: 10.1348/135910705X52309. [DOI] [PubMed] [Google Scholar]
- 13.Lowe R, Cockshott Z, Greenwood R, et al. Self-efficacy as an appraisal that moderates the coping-emotion relationship: associations among people with rheumatoid arthritis. Psychol Health. 2008;23(2 ):155–74. doi: 10.1080/14768320601139160. [DOI] [PubMed] [Google Scholar]
- 14.Ramjeet J, Smith J, Adams M. The relationship between coping and psychological and physical adjustment in rheumatoid arthritis: a literature review. J Nurs Healthc Chronic Illn. 2008;17:418–28. doi: 10.1111/j.1365-2702.2008.02579.x. [DOI] [PubMed] [Google Scholar]
- 15.Kralik D, Van Loon AM. Editorial: Transition and chronic illness experience. J Nurs Healthc Chronic Illn. 2009;1(2 ):113–5. [Google Scholar]
- 16.Kirwan JR, Hewlett SE, Heiberg T, et al. Incorporating the patient perspective into outcome assessment in rheumatoid arthritis--progress at OMERACT 7. J Rheumatol. 2005;32(11 ):2250–6. [PubMed] [Google Scholar]
- 17.Arvidsson SB, Petersson A, Nilsson I, et al. A nurse-led rheumatology clinic's impact on empowering patients with rheumatoid arthritis: A qualitative study. Nurs Health Sci. 2006;8(3 ):133–9. doi: 10.1111/j.1442-2018.2006.00269.x. [DOI] [PubMed] [Google Scholar]
- 18.Dougados M. Can we combine patient's and doctor's perspective when assessing rheumatoid arthritis disease activity? J Rheumatol. 2007;34(10 ):1949–52. [PubMed] [Google Scholar]
- 19.Corbin J, Strauss A. Basics of Qualitative Research. 3. Thousands Oaks: Sage publications; 2008. [Google Scholar]
- 20.Blumer H. Symbolic Interactions Perspective and Method. California: University of California press; 1986. [Google Scholar]
- 21.Ryan S, Hassell A, Dawes P, Kendall S. Perceptions of control in patients with rheumatoid arthritis. Nurs Times. 2003;99(13 ):36–8. [PubMed] [Google Scholar]
- 22.Brown S, Williams A. Women's experiences of rheumatoid arthritis. J Adv Nurs. 1995;21(4 ):695–701. doi: 10.1046/j.1365-2648.1995.21040695.x. [DOI] [PubMed] [Google Scholar]
- 23.Kralik D, Koch T, Price K, Howard N. Chronic illness self-management: taking action to create order. J Clin Nurs. 2004;13(2 ):259–67. doi: 10.1046/j.1365-2702.2003.00826.x. [DOI] [PubMed] [Google Scholar]
- 24.Verduin PJ, de Bock GH, Vliet Vlieland TP, Peeters AJ, Verhoef J, Otten W. Purpose in life in patients with rheumatoid arthritis. Clin Rheumatol. 2008;27(7 ):899–908. doi: 10.1007/s10067-007-0822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lempp H, Scott DL, Kingsley GH. Patients' views on the quality of health care for rheumatoid arthritis. Rheumatology (Oxford) 2006;45(12 ):1522–8. doi: 10.1093/rheumatology/kel132. [DOI] [PubMed] [Google Scholar]
- 26.Ward V, Hill J, Hale C, Bird H, Quinn H, Thorpe R. Patient priorities of care in rheumatology outpatient clinics: a qualitative study. Musculoskeletal Care. 2007;5(4 ):216–28. doi: 10.1002/msc.111. [DOI] [PubMed] [Google Scholar]
- 27.Bergsten U, Bergman S, Fridlund B, et al. Patients' conceptions of the cause of their rheumatoid arthritis: a qualitative study. Musculoskeletal Care. 2009;7(4 ):243–55. doi: 10.1002/msc.156. [DOI] [PubMed] [Google Scholar]
- 28.Graves H, Scott DL, Lempp H, Weinman J. Illness beliefs predict disability in rheumatoid arthritis. J Psychosom Res. 2009;67(5 ):417–23. doi: 10.1016/j.jpsychores.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Nicassio PM, Wallston KA, Callahan LF, Herbert M, Pincus T. The measurement of helplessness in rheumatoid arthritis. The development of the arthritis helplessness index. J Rheumatol. 1985;12(3 ):462–7. [PubMed] [Google Scholar]
- 30.McDonald-Miszczak L, Wister AV. Predicting self-care behaviors among older adults coping with arthritis: a cross-sectional and 1-year longitudinal comparative analysis. J Aging Health. 2005;17(6 ):836–57. doi: 10.1177/0898264305280984. [DOI] [PubMed] [Google Scholar]
- 31.Fridlund B, Hildingh C. Qualitative Research Methods in the Service of Health. Lund: Studentlitteratur; 2000. [Google Scholar]