The current treatment options for patients with unresectable and metastatic cutaneous squamous cell carcinoma are reviewed.
Keywords: Cutaneous squamous cell carcinoma, Epidermal growth factor receptor, Skin cancer treatment
Abstract
Cutaneous squamous cell carcinoma (SCC) is an already common disorder with a rapidly increasing incidence. Treatment of early disease depends primarily on surgery or destructive techniques. In contrast to the frequency of early SCC, unresectable or metastatic SCC is relatively rare, but potentially life-threatening without clearly proven treatment options. Few rigorous studies of the treatment of advanced SCC have been undertaken. In the past, various agents have been explored in a limited fashion, including chemotherapy (cisplatin, fluoropyrimidines, bleomycin, doxorubicin), 13-cis-retinoic acid, and interferon-α2a. Clinical activity has been suggested by these trials, but their small sizes, heterogeneous patient populations, and lack of randomization have hindered the use of their results in defining treatment paradigms. Only one rigorous randomized trial has focused on cutaneous SCC. Enrolling 66 patients, that trial randomized patients at high recurrence risk to either observation or postoperative interferon-α2a and 13-cis-retinoic acid. This treatment did not improve time to recurrence or prevent secondary cutaneous SCC from developing. Though not in the metastatic setting, this study casts doubt on the ability of this regimen to control metastatic disease. Recently, agents targeting the human epidermal growth factor receptor (erlotinib, gefitinib, cetuximab) have displayed preliminary evidence of activity in phase II clinical trials and case series reports. Expression of this receptor is frequent in cutaneous SCC and appears to be prognostically adverse. Only the conduct of rigorous trials, with well-defined endpoints, adequate patient numbers, and preferably randomization, can prove the clinical efficacy of this promising treatment approach and define better therapy for this vexing clinical problem.
Introduction
Nonmelanoma skin cancer (NMSC) is the most common malignancy worldwide, consisting primarily of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) [1]. SCC, making up 20% of all NMSC cases, is the second most common skin cancer after BCC in the U.S. [2]. The lifetime risk for developing SCC is 7%–11%, and this has been increasing epidemically in the last several decades [3]. SCC is generally more aggressive, and potentially life-threatening, than BCC. The mortality rate from SCC of the skin is difficult to estimate, partly because of inadequate data regarding its overall incidence. A study from Australia estimated the case fatality rate at 4%–5%, whereas U.S. studies suggest a 1% rate [4, 5]. Most (>90%) patients with SCC are cured by local therapies [6]. The remaining patients are not cured and require additional treatment.
Treatment of Early Disease
Primary SCC may be classified as low or high risk, depending on the likelihood of recurrence, metastasis, and death. Both tumoral and host factors may be important (Table 1) [7, 8]. The possession of any of the factors in Table 1 should alert the clinician to a less than optimal prognosis. For example, one prospective analysis of 210 cutaneous SCC patients identified primary tumor diameter ≥4 cm, invasion of s.c. tissues, and perineural invasion as adverse factors [5]. Patients possessing one of these high-risk factors displayed a 3-year disease-specific survival rate of only 70%, versus 100% for patients without any of these factors.
Table 1.
Factors increasing the risk for recurrence, metastasis, or death in patients with squamous cell carcinoma of the skin [7, 8]
Existence of any of these factors implies high risk.
For low-risk, local lesions, the usual treatment is surgical excision, electrodessication, and curettage, or cryosurgery. Destructive treatment methods leave no tissue to analyze for marginal control. Nevertheless, using these methods, the 5-year control rate in patients with low-risk primary lesions can be as high as 96% [7, 9].
For higher risk tumors, the primary treatment is surgical excision. The key factor in determining the cure rate is the ability to achieve negative surgical margins [7, 8]. Surgery may be conventional or microscopically controlled, the later procedure referred to as “Mohs' surgery,” after its originator. In this procedure, the targeted lesion is excised and the circumferential margins are assessed microscopically for residual tumor. Margins remaining involved undergo repeated excisions, followed by histological assessment, until negative margins are obtained. Mohs' surgery yields local control rates of 92%–100%, versus 38%–87% for standard surgical excision [10]. Mohs' surgery cure rates decrease as tumor grade increases, with a 45.2% cure rate for grade 4 SCC [9]. For inoperable, aggressive or recurrent lesions, adjuvant or primary radiation therapy may play a role [8, 10]. The extent of benefit conveyed by adjuvant radiation therapy has not, however, been clearly quantified.
Treatment of Advanced Disease
Cytotoxic Chemotherapy
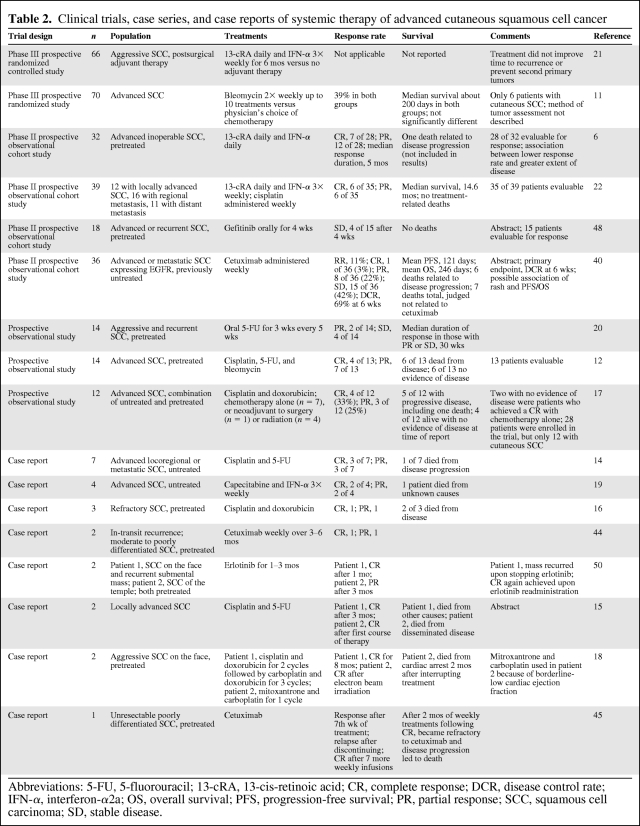
In its most advanced form, cutaneous SCC is treated systemically. Investigation of systemic therapy for this disease has been very limited. Recommendations are based wholly on the results of one adjuvant phase III trial, four single-arm phase II trials, and a number of case series/reports. A number of systemic therapies have been used to treat advanced cutaneous SCC, including cytotoxic chemotherapy (cisplatin, 5-fluorouracil [5-FU], bleomycin, and doxorubicin), 13-cis-retinoic acid (13cRA), immunotherapy (interferon α2a [IFN-α]), and molecularly targeted agents (gefitinib, cetuximab, and erlotinib) (Table 2).
Table 2.
Clinical trials, case series, and case reports of systemic therapy of advanced cutaneous squamous cell cancer
Abbreviations: 5-FU, 5-fluorouracil; 13-cRA, 13-cis-retinoic acid; CR, complete response; DCR, disease control rate; IFN-α, interferon-α2a; OS, overall survival; PFS, progression-free survival; PR, partial response; SCC, squamous cell carcinoma; SD, stable disease.
A nonrigorous randomized trial comparing bleomycin with other cytotoxic agents (cyclophosphamide, vincristine, methotrexate, and procarbazine) as treatment for 70 patients with SCC, only six of whom had cutaneous SCC, showed no statistically significant difference between the two treatment groups [11]. Sadek et al. [12] reported on 14 patients (13 evaluable) from a prospective observational study of patients with advanced cutaneous SCC treated with cisplatin, 5-FU, and bleomycin for 1–4 months. That study resulted in four of 13 patients with a complete response (CR) and seven of 13 with a partial response (PR) [13]. After 1 year, six of 13 patients had died from their disease and six of 13 had no evidence of disease. One patient who achieved a CR had local recurrence at 8 months, but achieved a second CR after surgery and adjuvant radiotherapy.
Two case series reported patients achieving a CR with the combination of cisplatin and 5-FU [14, 15]. Khansur et al. [14] reported on seven patients with primary cutaneous SCC and locoregional progression treated with cisplatin and 5-FU. A CR was achieved in three of seven patients and a PR was achieved in three of seven patients. The median duration of CR was 1 year. Two of the three patients with a CR were disease free at a 13-month and 24-month follow-up. Fujisawa et al. [15] reported on two patients achieving a CR after one or two cycles of cisplatin and 5-FU. In one of the patients, therapy was discontinued after achieving a surgically confirmed CR. That patient eventually developed disseminated disease, leading to death 2 years after initial presentation. The authors concluded that this therapy appeared to be effective in terms of local control, but was ineffective in preventing hematologic dissemination.
Guthrie et al. [16] treated three SCC patients with cisplatin and doxorubicin. One patient had a CR for 17 months, one had a PR for 3 months, and one had stable disease (SD). The authors suggested that the combination of cisplatin and doxorubicin had activity in cutaneous SCC. A phase II trial by the same group used this regimen in 12 cutaneous SCC patients [17]. Interpretation of that trial's results was hampered by the low numbers of enrolled patients and their heterogeneity. Seven patients were treated with chemotherapy alone: two achieved a CR for 4–12 months, two achieved a PR for 3–6 months, and three had no response. Five patients received neoadjuvant chemotherapy followed by surgery (n = 1) or definitive radiation therapy (n = 2), with two CRs and one PR after induction chemotherapy. The authors concluded that this combination had activity in advanced cutaneous SCC patients, and that multimodality therapy was to be preferred over chemotherapy alone. A case report of combined cisplatin and doxorubicin-based therapy also indicated that this combination may be active [18].
Wollina et al. [19] used oral capecitabine and s.c. IFN-α in four patients with advanced cutaneous SCC. Capecitabine is an orally bioavailable fluoropyrimidine chemotherapy agent that is converted to 5-FU in tumor cells. They reported two patients with CRs and two patients with PRs using this regimen.
Oral 5-FU was administered to 14 patients with advanced cutaneous SCC as a single agent [20]. Two patients experienced a PR and seven had SD of varying duration. This 5-FU preparation is not commonly available in the U.S. This report, however, supports the use of fluoropyrimidine-based therapy in advanced cutaneous SCC patients, because there may be palliative benefit even with the use of single-agent therapy.
Retinoids and IFN-α in Cutaneous SCC
Retinoids modulate cell differentiation and proliferation; in vitro, some cytokines can act synergistically with retinoids to inhibit cell proliferation and increase apoptosis [21]. Shin et al. [22] assessed the effects of IFN-α, 13cRA, and cisplatin used to treat unresectable SCC of the skin in a prospective phase II trial. Thirty-nine patients were enrolled and 35 were considered evaluable. Of these, six of 35 (17%) experienced a CR and six of 35 (17%) had a PR. The response rate of patients with locoregional disease was higher (67%) than that of patients with metastatic disease (17%; p = .007). They concluded that this combination was useful in treating locally advanced disease, but less so in metastatic disease.
Lippman et al. [6] used 13cRA in combination with IFN-α in a prospective phase II trial enrolling 32 patients with inoperable cutaneous SCC. They observed a response in 19 (68%) of the 28 evaluable patients (seven CRs, 12 PRs). The median duration of response was 5 months. Response rates varied with the extent of disease: 93% (13 of 14) responded among patients with advanced local disease, 67% (four of six) responded among patients with regional disease, and 25% (two of eight) responded among those with distant metastases. This combination appeared to be effective in advanced SCC patients, albeit with greater efficacy in less advanced disease.
Although not focused on treatment of unresectable disease, Brewster and coworkers reported on a phase III trial testing whether adjuvant therapy with 13cRA and IFN-α was effective in preventing recurrences and increasing time to recurrence [21]. Their adjuvant study enrolled 66 patients with “aggressive” SCC, defined as having one of the following characteristics: size ≥2 cm, perineural invasion, radiological or pathological evidence of deep invasion into nearby structures, or proven regional metastasis. The 66 patients were randomly assigned, following initial surgery, to receive either a combination of 13cRA and IFN-α for 6 months or no systemic adjuvant therapy. Adjuvant radiotherapy was added to the initial treatment plan for tumors with perineural invasion, more than two positive nodes, extracapsular nodal disease, or microscopically positive margins. With a median follow-up of 21.5 months, this systemic treatment did not improve time to recurrence or prevent secondary tumors. Although this study was in the adjuvant setting, the results argue that this combination is unlikely to be highly active in the setting of macroscopic residual disease. This is particularly notable given the relatively high quality of this study, compared with others testing this regimen or indeed any other regimen in this disease.
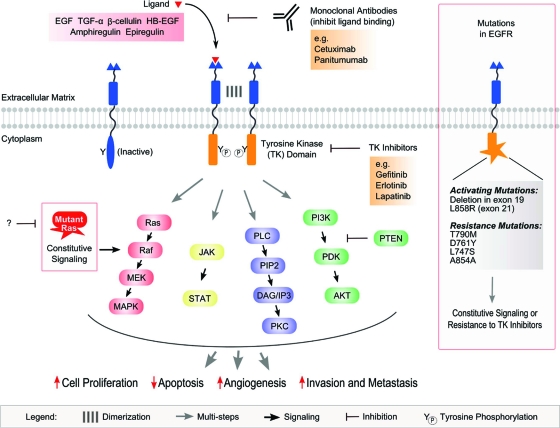
The Human Epidermal Growth Factor Receptor
The epidermal growth factor receptor (EGFR, HER-1, erbB) is a transmembrane receptor tyrosine kinase that belongs to a family of four kinases, with the other members being designated HER-2, HER-3, and HER-4 [23, 24]. Binding of any of several ligands to the extracellular domain of the receptor results in formation of EGFR homodimers and heterodimers with other members of the family. The intracellular domain of the receptors is activated in the dimerization process, leading to autophosphorylation of tyrosine residues and to phosphorylation and activation of downstream pathways (Fig. 1). These include Ras/Raf/mitogen-activated protein kinase (MAPK), phospholipase C, phosphatidylinositol 3-kinase (PI3K)–Akt, and Janus kinase–signal transducer and activator of transcription (JAK-STAT) [25]. The MAPK pathway is involved in cell proliferation and survival. The PI3K–Akt pathway is involved in cell proliferation and cell migration. The JAK-STAT pathway is involved in the transcription of genes involved in oncogenesis. The different EGFR signaling pathways are depicted in Figure 1.
Figure 1.
Signaling pathways and effects of EGFR. Upon binding to one of multiple ligands, EGFR dimerizes with another member of the EGFR family, leading to the activation of the TK domain, phosphorylation of critical tyrosine residues in the EGFR intracellular domain, and activation of downstream signaling pathways, including MAPK, JAK-STAT, PLC, and PI3K–Akt. Collectively, EGFR signaling may lead to increased cell proliferation, decreased apoptosis, increased angiogenesis, increased invasion, and increased metastasis. As depicted above, multiple opportunities exist to inhibit EGFR signaling; for example, monoclonal antibodies (e.g., cetuximab and panitumumab) interact with the extracellular domain of EGFR preventing ligand-induced activation of the receptor, and small-molecule inhibitors (e.g., gefitinib, erlotinib, and lapatinib) block activation of the TK domain preventing induction of EGFR signaling pathways. Specific EGFR mutations may lead to constitutive activation of EGFR regardless of ligand binding and/or resistance of EGFR to the effects of TK inhibitors. Independent of receptor status, EGFR downstream signaling may become aberrantly activated; for example, mutant Ras may lead to constitutive activation of the MAPK pathway or mutation/loss of PTEN may lead to loss of negative regulation of the PI3K–Akt pathway.
Abbreviations: DAG, diacylglycerol; EGFR, epidermal growth factor receptor; IP3, inositol triphosphate; JAK, Janus kinase; MAPK, mitogen-activated protein kinase; MEK, MAPK/extracellular signal–related kinase kinase; PDK, 3-phosphoinositide-dependent protein kinase; PI3K, phosphoinositide 3-kinase; PIP2, phosphatidylinositol bisphosphate; PKC, protein kinase C; PLC, phospholipase C; PTEN, phosphatase and tensin homologue deleted on chromosome ten; STAT, signal transducer and activator of transcription; TGF, transforming growth factor; TK, tyrosine kinase.
The EGFR pathway is important in a range of cancers. Positive randomized trial results have led to the approval of agents targeting these pathways in non-small cell lung cancer, colorectal cancer, squamous cell cancer of the head and neck, and pancreatic cancer [26–30]. The relationship between this therapy and benefit is not, however, simple. Different factors predict response in different types of tumors.
A variety of biomarkers have been analyzed to assess their utility in predicting benefit. For example, in metastatic colorectal cancer treated with cetuximab, a monoclonal antibody targeting the extracellular domain of EGFR, the presence of activating mutations in exon 2 of downstream KRAS either leads to no benefit of cetuximab monotherapy or confers an adverse effect on outcome when cetuximab is combined with chemotherapy and bevacizumab [27, 31]. In contrast, KRAS exon 2 mutational status did not correlate with benefit in a study of non-small cell lung cancer patients treated with cetuximab and chemotherapy [32]. The presence of activating mutations in EGFR itself, elevated EGFR gene copy number, and positive immunohistochemistry (IHC) for EGFR have been shown, in randomized trials, to be useful in predicting benefit from small molecule inhibitors directed at the EGFR tyrosine kinase domain [33–35].
Given the paucity of unresectable or metastatic cutaneous SCC, reliable information on the frequency of EGFR expression is limited. One study of 13 metastatic specimens by IHC demonstrated that all had strong membranous expression of EGFR [36]. Another study of locally advanced and nodally metastatic cutaneous SCC demonstrated EGFR expression above background in only nine of 21 (43%) specimens using a quantitative Western blotting technique [37]. Another study using IHC and fluorescence in situ hybridization demonstrated higher levels of EGFR protein expression in cutaneous SCC than in the precursor actinic keratoses and an association between this elevated protein expression and higher EGFR gene copy number [38]. One study, examining the role of EGFR in cutaneous SCC arising in the head and neck, demonstrated that primary lesions associated with subsequent metastasis were more likely to overexpress EGFR (79%) than those not associated with subsequent metastasis (36%) [39]. Interestingly, metastatic nodal disease exhibited only a 47% rate of EGFR overexpression; EGFR overexpression in that study was not associated with EGFR gene amplification.
Anti-EGFR Therapy in Cutaneous SCC
Cetuximab, a humanized monoclonal antibody, inhibits EGFR by blocking the extracellular domain of EGFR. This prevents the receptor's ligand from binding and consequent dimerization. One phase II study and two case reports have described its effects in cutaneous SCC. Maubec and coworkers recently reported final results from a phase II trial enrolling 36 patients with unresectable or metastatic cutaneous SCC that expressed EGFR [40]. None of the patients received prior chemotherapy. Thirty-one patients of 36 enrolled were evaluable for tumor response. The study's primary endpoint was the disease control rate (DCR = CR + PR + SD) after 6 weeks of treatment. In the intent-to-treat population, the DCR was 69% and the overall response rate was 11%. The mean progression-free survival (PFS) and overall survival (OS) times were 121 days and 246 days, respectively. Grade 3–4 toxicities judged to be associated with cetuximab therapy were seen in three patients (infusion-related reactions in two patients and interstitial pulmonary syndrome in one patient). Among the 31 evaluable patients, development of an acneiform rash did not predict response to treatment, but did predict the mean PFS and OS times. Such drug rashes have been associated with better outcome in other diseases treated with cetuximab, such as SCC of the head and neck [28].
Randomized trials of cetuximab in metastatic colorectal cancer (mCRC) patients have confirmed the importance of mutational status in the signal transduction apparatus downstream from EGFR, including KRAS and BRAF, and in an immune marker, the Fc antibody receptor [41–43]. In a subset of 28 patients studied by Maubec and coworkers, mutational status was assessed in exon 2 (n = 28) and exon 3 (n = 25) of KRAS and exon 15 (n = 23) of BRAF kinase. All were found to be wild-type; mutations in these sites in mCRC patients predict lower responsiveness to cetuximab. Cutaneous SCC patients possessing the FcγIIa-131 H/H or FcγIIIa-158 V/V variants, associated with better outcome in mCRC patients, had a PFS interval similar to the wild-type 131R and 158F carriers in the Maubec et al. [40] study.
Two case reports of cutaneous SCC patients treated with cetuximab have also been published, both achieving CRs [44, 45]. All three reports suggest that cetuximab may be a therapeutic option in patients with unresectable cutaneous SCC. These results must be taken with caution, because they are preliminary. One report of two lung transplant patients receiving cetuximab for advanced cutaneous SCC suggested that fatal diffuse alveolar damage may have been caused by cetuximab [46]. Four cases of interstitial pneumonitis and one fatality are reported in the cetuximab package insert, of 1,570 patients treated [47].
Gefitinib inhibits binding to the ATP-binding site of EGFR, rendering it unable to autophosphorylate and activate the receptor. Glisson et al. [48] used gefitinib in a prospective phase II trial, enrolling 18 patients with advanced or recurrent cutaneous SCC. Gefitinib had already been reported to have an 11% response rate and 53% control rate in head and neck SCC patients [49]. Four of the fifteen evaluable cutaneous SCC patients had SD after 4 weeks of treatment.
Erlotinib, much like gefitinib, competitively binds to the ATP-binding site of EGFR. It has been approved for use in non-small cell lung cancer patients who have failed to respond to chemotherapy, and in advanced pancreatic cancer patients, combined with gemcitabine. Read et al. [50] reported results from two patients with unresectable cutaneous SCC. One patient achieved a CR after 1 month of treatment and the other achieved a PR after 3 months of treatment. The patient that achieved a CR had a recurrence when the therapy was discontinued.
Treatment Recommendations
Treatment recommendations in this setting are difficult to promulgate, because the quality of information available is clearly suboptimal. If available, a clinical trial should be the first choice for treatment of these patients. Such trials are uncommon, because of the relative rarity of the condition. Furthermore, patients requiring treatment for advanced SCC may have serious medical comorbidities (such as iatrogenic immunosuppression for organ transplant) that prevent clinical trial participation, even if disease-specific trials are available.
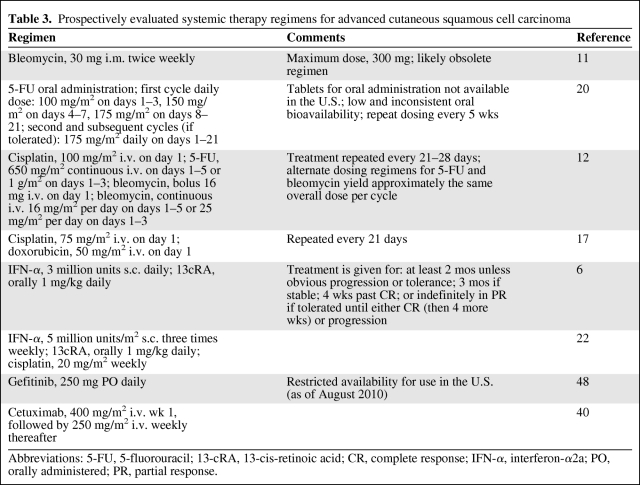
Table 3 provides details of the systemic treatment regimens that have been studied prospectively and are described herein. Several of these regimens appear to be obsolete (i.m. bleomycin) or use a preparation (oral 5-FU) that may not be easily obtainable [11, 20]. Beyond this, no specific efficacy data argue for the use of any particular regimen in the off-protocol treatment of cutaneous SCC. All the prospectively studied regimens demonstrate clinical benefits in some patients, albeit in small studies with significant design limitations. Thus, logistical considerations and patient comorbidities play a major role in treatment selection. Platinum- or fluoropyrimidine-based systemic chemotherapy regimens could be considered standard cytotoxic regimens. Combinations of 13cRA and IFN-α would also be reasonable systemic options.
Table 3.
Prospectively evaluated systemic therapy regimens for advanced cutaneous squamous cell carcinoma
Abbreviations: 5-FU, 5-fluorouracil; 13-cRA, 13-cis-retinoic acid; CR, complete response; IFN-α, interferon-α2a; PO, orally administered; PR, partial response.
Despite the limited information regarding the use of EGFR inhibitors in cutaneous SCC, the volume of evidence for efficacy, in reported numbers of treated patients, approximates that supporting any other treatment regimen, and this is likely to continue to accumulate. EGFR inhibitors may also be tolerable in clinical situations in which cytotoxic or biological therapies may be contraindicated. Furthermore, phase I clinical trials of EGFR-targeting agents are likely to be available as new agents are developed, offering a possible avenue for biologically rational treatment of these patients in an experimental setting, without requiring a disease-specific trial.
If a patient is not eligible for a clinical trial, but requires palliative therapy for advanced cutaneous SCC, treatment with an EGFR-inhibiting agent might be appropriate. The largest trial of EGFR inhibition completed to date assessed cetuximab. Data also exist for gefitinib. The choice of agent may, however, be dictated by nonmedical considerations, such as which EGFR-inhibiting agent can be obtained for a given patient. Assessment of tumoral EGFR expression, easily performed by IHC in most pathology laboratories, would be reasonable to confirm that the biological target of EGFR-inhibiting agents is at least present prior to treatment. Notably in this regard, the study of Maubec and coworkers required EGFR expression for participation [36, 40].
Conclusions
Although cutaneous SCC is quite common, surprisingly little reliable information exists regarding the management of advanced disease. The literature primarily consists of isolated case reports and small case series. Several prospective studies have been conducted, but they are hampered by limited study designs, relatively small patient numbers, and the consequent requirement for enrolling a heterogeneous group of patients. Studies using 13cRA and IFN-α, with or without cisplatin, seem to be the most rigorous, and suggest clinical activity in the metastatic setting. Enthusiasm for the nonexperimental use of these regimens must be tempered by the negative results of the only rigorous randomized trial in this disease setting, in which adjuvant therapy with 13cRA and IFN-α was ineffective [21]. Rigorous studies of chemotherapy in this disease have demonstrated activity, but have only been conducted in the phase II setting, and are similarly afflicted by limited patient numbers.
Targeting EGFR may be a biologically rational approach to the treatment of cutaneous SCC. EGFR is expressed in a significant fraction of cutaneous SCC tumors. Approved agents targeting this receptor exist, and data from phase II trials of gefitinib and cetuximab suggest clinically significant activity. Further rigorous trials are warranted. Strong correlative studies would be highly desirable; the extensive investigation of the EGFR pathway in other tumors should provide more than adequate guidance to the investigative plan in these efforts.
Significant barriers exist to the rigorous assessment of strategies to treat advanced cutaneous SCC. Patients with advanced disease are relatively rare. Thus, multi-institutional trials must be conducted to accrue adequate patient numbers. Reliable baseline data regarding the efficacy of existing treatment regimens (such as carboplatin and paclitaxel, widely used in other types of SCC but without data in cutaneous SCC) must be generated, both to assess activity and for comparison in future studies of novel agents, such as EGFR inhibitors. Finally, positive findings must be confirmed in well-conducted randomized trials, accompanied by correlative studies to validate (or exclude) potential biomarkers of activity. Only by doing so can new treatment paradigms for this vexing problem come to fruition.
Acknowledgments
We would like to thank Jennie Brown and Allison Kleine for administrative support in the preparation of this manuscript. The work of Drs. Cranmer and Morgan is supported, in part, by a Career Development Award from the Phoenix Friends of the Arizona Cancer Center.
Author Contributions
Conception/Design: Lee D. Cranmer
Administrative support: Lee D. Cranmer
Collection and/or assembly of data: Candace Engelhardt
Manuscript writing: Lee D. Cranmer, Candace Engelhardt, Sherif S. Morgan
Final approval of manuscript: Lee D. Cranmer, Candace Engelhardt, Sherif S. Morgan
References
- 1.Veness MJ, Morgan GJ, Palme CE, et al. Surgery and adjuvant radiotherapy in patients with cutaneous head and neck squamous cell carcinoma metastatic to lymph nodes: Combined treatment should be considered best practice. Laryngoscope. 2005;115:870–875. doi: 10.1097/01.MLG.0000158349.64337.ED. [DOI] [PubMed] [Google Scholar]
- 2.Alam M, Ratner D. Cutaneous squamous-cell carcinoma. N Engl J Med. 2001;344:975–983. doi: 10.1056/NEJM200103293441306. [DOI] [PubMed] [Google Scholar]
- 3.Miller DL, Weinstock MA. Nonmelanoma skin cancer in the United States: Incidence. J Am Acad Dermatol. 1994;30:774–778. doi: 10.1016/s0190-9622(08)81509-5. [DOI] [PubMed] [Google Scholar]
- 4.Joseph MG, Zulueta WP, Kennedy PJ. Squamous cell carcinoma of the skin of the trunk and limbs: The incidence of metastases and their outcome. Aust N Z J Surg. 1992;62:697–701. doi: 10.1111/j.1445-2197.1992.tb07065.x. [DOI] [PubMed] [Google Scholar]
- 5.Clayman GL, Lee JJ, Holsinger FC, et al. Mortality risk from squamous cell skin cancer. J Clin Oncol. 2005;23:759–765. doi: 10.1200/JCO.2005.02.155. [DOI] [PubMed] [Google Scholar]
- 6.Lippman SM, Parkinson DR, Itri LM, et al. 13-cis-retinoic acid and interferon alpha-2a: Effective combination therapy for advanced squamous cell carcinoma of the skin. J Natl Cancer Inst. 1992;84:235–241. doi: 10.1093/jnci/84.4.235. [DOI] [PubMed] [Google Scholar]
- 7.Minton TJ. Contemporary Mohs surgery applications. Curr Opin Otolaryngol Head Neck Surg. 2008;16:376–380. doi: 10.1097/MOO.0b013e3283079cac. [DOI] [PubMed] [Google Scholar]
- 8.Jambusaria-Pahlajani A, Miller CJ, Quon H, et al. Surgical monotherapy versus surgery plus adjuvant radiotherapy in high-risk cutaneous squamous cell carcinoma: A systematic review of outcomes. Dermatol Surg. 2009;35:574–585. doi: 10.1111/j.1524-4725.2009.01095.x. [DOI] [PubMed] [Google Scholar]
- 9.Mohs F. Chemosurgery: Microscopically Controlled Surgery for Skin Cancer. Springfield, IL: Charles C. Thomas; 1978. pp. 153–164. [Google Scholar]
- 10.Han A, Ratner D. What is the role of adjuvant radiotherapy in the treatment of cutaneous squamous cell carcinoma with perineural invasion? Cancer. 2007;109:1053–1059. doi: 10.1002/cncr.22509. [DOI] [PubMed] [Google Scholar]
- 11.Bleomycin in advanced squamous cell carcinoma: A random controlled trial. Report of Medical Research Council Working Party on Bleomycin. Br Med J. 1976;1:188–190. doi: 10.1136/bmj.1.6003.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadek H, Azli N, Wendling JL, et al. Treatment of advanced squamous cell carcinoma of the skin with cisplatin, 5-fluorouracil, and bleomycin. Cancer. 1990;66:1692–1696. doi: 10.1002/1097-0142(19901015)66:8<1692::aid-cncr2820660807>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 13.Miller AB, Hoogstraten B, Staquet M, et al. Reporting results of cancer treatment. Cancer. 1981;47:207–214. doi: 10.1002/1097-0142(19810101)47:1<207::aid-cncr2820470134>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 14.Khansur T, Kennedy A. Cisplatin and 5-fluorouracil for advanced locoregional and metastatic squamous cell carcinoma of the skin. Cancer. 1991;67:2030–2032. doi: 10.1002/1097-0142(19910415)67:8<2030::aid-cncr2820670803>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 15.Fujisawa Y, Umebayashi Y, Ichikawa E, et al. Chemoradiation using low-dose cisplatin and 5-fluorouracil in locally advanced squamous cell carcinoma of the skin: A report of two cases. J Am Acad Dermatol. 2006;55(5 suppl):S81–S85. doi: 10.1016/j.jaad.2005.12.035. [DOI] [PubMed] [Google Scholar]
- 16.Guthrie TH, Jr, McElveen LJ, Porubsky ES, et al. Cisplatin and doxorubicin. An effective chemotherapy combination in the treatment of advanced basal cell and squamous carcinoma of the skin. Cancer. 1985;55:1629–1632. doi: 10.1002/1097-0142(19850415)55:8<1629::aid-cncr2820550802>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 17.Guthrie TH, Jr, Porubsky ES, Luxenberg MN, et al. Cisplatin-based chemotherapy in advanced basal and squamous cell carcinomas of the skin: Results in 28 patients including 13 patients receiving multimodality therapy. J Clin Oncol. 1990;8:342–346. doi: 10.1200/JCO.1990.8.2.342. [DOI] [PubMed] [Google Scholar]
- 18.Merimsky O, Neudorfer M, Spitzer E, et al. Salvage cisplatin and adriamycin for advanced or recurrent basal or squamous cell carcinoma of the face. Anticancer Drugs. 1992;3:481–484. doi: 10.1097/00001813-199210000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Wollina U, Hansel G, Koch A, et al. Oral capecitabine plus subcutaneous interferon alpha in advanced squamous cell carcinoma of the skin. J Cancer Res Clin Oncol. 2005;131:300–304. doi: 10.1007/s00432-004-0656-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cartei G, Cartei F, Interlandi G, et al. Oral 5-fluorouracil in squamous cell carcinoma of the skin in the aged. Am J Clin Oncol. 2000;23:181–184. doi: 10.1097/00000421-200004000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Brewster AM, Lee JJ, Clayman GL, et al. Randomized trial of adjuvant 13-cis-retinoic acid and interferon alfa for patients with aggressive skin squamous cell carcinoma. J Clin Oncol. 2007;25:1974–1978. doi: 10.1200/JCO.2006.05.9873. [DOI] [PubMed] [Google Scholar]
- 22.Shin DM, Glisson BS, Khuri FR, et al. Phase II and biologic study of interferon alfa, retinoic acid, and cisplatin in advanced squamous skin cancer. J Clin Oncol. 2002;20:364–370. doi: 10.1200/JCO.2002.20.2.364. [DOI] [PubMed] [Google Scholar]
- 23.Modjtahedi H, Essapen S. Epidermal growth factor receptor inhibitors in cancer treatment: Advances, challenges and opportunities. Anticancer Drugs. 2009;20:851–855. doi: 10.1097/CAD.0b013e3283330590. [DOI] [PubMed] [Google Scholar]
- 24.Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med. 2008;358:1160–1174. doi: 10.1056/NEJMra0707704. [DOI] [PubMed] [Google Scholar]
- 25.Laurent-Puig P, Lievre A, Blons H. Mutations and response to epidermal growth factor receptor inhibitors. Clin Cancer Res. 2009;15:1133–1139. doi: 10.1158/1078-0432.CCR-08-0905. [DOI] [PubMed] [Google Scholar]
- 26.Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): An open-label randomised phase III trial. Lancet. 2009;373:1525–1531. doi: 10.1016/S0140-6736(09)60569-9. [DOI] [PubMed] [Google Scholar]
- 27.Karapetis CS, Khambata-Ford S, Jonker DJ, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–1765. doi: 10.1056/NEJMoa0804385. [DOI] [PubMed] [Google Scholar]
- 28.Bonner JA, Harari PM, Giralt J, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–28. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- 29.Vermorken JB, Mesia R, Rivera F, et al. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359:1116–1127. doi: 10.1056/NEJMoa0802656. [DOI] [PubMed] [Google Scholar]
- 30.Moore MJ, Goldstein D, Hamm J, et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol. 2007;25:1960–1966. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 31.Tol J, Koopman M, Cats A, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360:563–572. doi: 10.1056/NEJMoa0808268. [DOI] [PubMed] [Google Scholar]
- 32.Khambata-Ford S, Harbison CT, Hart LL, et al. Analysis of potential predictive markers of cetuximab benefit in BMS099, a phase III study of cetuximab and first-line taxane/carboplatin in advanced non-small-cell lung cancer. J Clin Oncol. 2010;28:918–927. doi: 10.1200/JCO.2009.25.2890. [DOI] [PubMed] [Google Scholar]
- 33.Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 34.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: Correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 35.Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- 36.Maubec E, Duvillard P, Velasco VR, et al. Immunohistochemical analysis of EGFR and HER-2 in patients with metastatic squamous cell carcinoma of the skin. Anticancer Res. 2005;25:1205–1210. [PubMed] [Google Scholar]
- 37.Fogarty GB, Conus NM, Chu J, et al. Characterization of the expression and activation of the epidermal growth factor receptor in squamous cell carcinoma of the skin. Br J Dermatol. 2007;156:92–98. doi: 10.1111/j.1365-2133.2006.07603.x. [DOI] [PubMed] [Google Scholar]
- 38.Toll A, Salgado R, Yébenes M, et al. Epidermal growth factor receptor gene numerical aberrations are frequent events in actinic keratoses and invasive cutaneous squamous cell carcinomas. Exp Dermatol. 2010;19:151–153. doi: 10.1111/j.1600-0625.2009.01028.x. [DOI] [PubMed] [Google Scholar]
- 39.Ch'ng S, Low I, Ng D, et al. Epidermal growth factor receptor: A novel biomarker for aggressive head and neck cutaneous squamous cell carcinoma. Hum Pathol. 2008;39:344–349. doi: 10.1016/j.humpath.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Maubec E, Petrow P, Duvillard P, et al. Cetuximab as first-line monotherapy in patients with skin unresectable squamous cell carcinoma: Final results of a phase II multicenter study [abstract] J Clin Oncol. 2010;28:8510. [Google Scholar]
- 41.Laurent-Puig P, Cayre A, Manceau G, et al. Analysis of PTEN, BRAF, and EGFR status in determining benefit from cetuximab therapy in wild-type KRAS metastatic colon cancer. J Clin Oncol. 2009;27:5924–5930. doi: 10.1200/JCO.2008.21.6796. [DOI] [PubMed] [Google Scholar]
- 42.Van Cutsem E, Köhne C-H, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;360:1408–1417. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 43.Bibeau F, Lopez-Crapez E, Di Fiore F, et al. Impact of FcγRIIa-FcγRIIIa polymorphisms and KRAS mutations on the clinical outcome of patients with metastatic colorectal cancer treated with cetuximab plus irinotecan. J Clin Oncol. 2009;27:1122–1129. doi: 10.1200/JCO.2008.18.0463. [DOI] [PubMed] [Google Scholar]
- 44.Bauman JE, Eaton KD, Martins RG. Treatment of recurrent squamous cell carcinoma of the skin with cetuximab. Arch Dermatol. 2007;143:889–892. doi: 10.1001/archderm.143.7.889. [DOI] [PubMed] [Google Scholar]
- 45.Suen JK, Bressler L, Shord SS, et al. Cutaneous squamous cell carcinoma responding serially to single-agent cetuximab. Anticancer Drugs. 2007;18:827–829. doi: 10.1097/CAD.0b013e32809ef9e0. [DOI] [PubMed] [Google Scholar]
- 46.Leard LE, Cho BK, Jones KD, et al. Fatal diffuse alveolar damage in two lung transplant patients treated with cetuximab. J Heart Lung Transplant. 2007;26:1340–1344. doi: 10.1016/j.healun.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 47.Cetuximab [package insert] Branchburg, NJ: ImClone Systems Incorporated; 2010. [Google Scholar]
- 48.Glisson B, Kim S, Kies M, et al. Phase II study of gefitinib in patients with metastatic/recurrent squamous cell carcinoma of the skin. J Clin Oncol. 2006;24(18 suppl):5331. [Google Scholar]
- 49.Cohen EE, Rosen F, Stadler WM, et al. Phase II trial of ZD1839 in recurrent or metastatic squamous cell carcinoma of the head and neck. J Clin Oncol. 2003;21:1980–1987. doi: 10.1200/JCO.2003.10.051. [DOI] [PubMed] [Google Scholar]
- 50.Read W. Squamous carcinoma of the skin responding to erlotinib: Three cases. J Clin Oncol. 2007;25(18 suppl):16519. [Google Scholar]