A steady improvement in imaging diagnostics has been observed together with a rising adherence to regular clinical breast examinations. As a result, the detection of small clinically occult (nonpalpable) lesions has progressively increased. Nonpalpable carcinomas show very favorable prognostic features and high survival rates, showing the important role of modern imaging techniques.
Keywords: Nonpalpable breast cancer, Radioguided occult lesion localization, Diagnostics by imaging, Early detection
Abstract
Introduction.
In recent decades, a steady improvement in imaging diagnostics has been observed together with a rising adherence to regular clinical breast examinations. As a result, the detection of small clinically occult (nonpalpable) lesions has progressively increased. At present in our institution some 20% of the cases are treated when nonpalpable. The aim of the present study is to analyze the characteristics and prognosis of such tumors treated in a single institution.
Methods.
The analysis focused on 1,258 women who presented at the European Institute of Oncology with a primary clinically occult carcinoma between 2000 and 2006. All patients underwent radioguided occult lesion localization (ROLL), axillary dissection when appropriate, whole breast radiotherapy, or partial breast intraoperative irradiation and received tailored adjuvant systemic treatment.
Results.
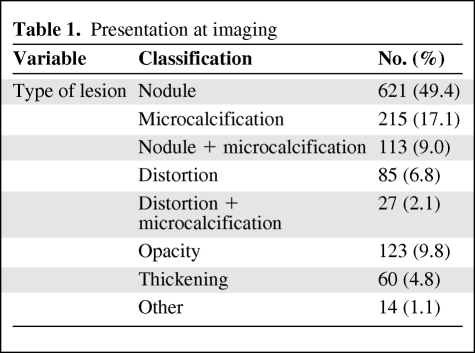
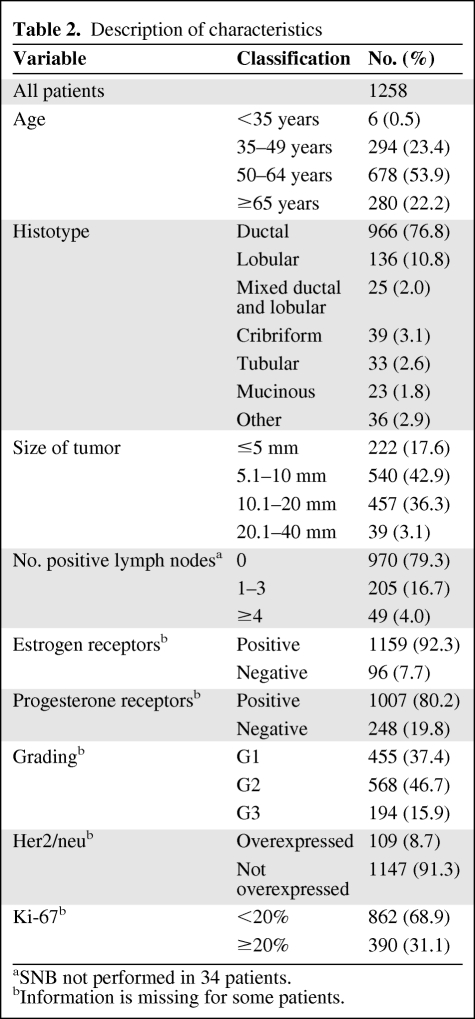
Median age was 56 years. Imaging showed a breast nodule in half of the cases and a breast nodule accompanied by microcalcifications in 9%. Microcalcifications alone were present in 17.1% of the cases, whereas suspicious opacity, distortion, or thickening represented the remaining 24.6%. Most tumors were characterized by low proliferative rates (68.9%), positive estrogen receptors (92.3%), and non-overexpressed Her2/neu (91.3%). After a median follow-up of 60 months, we observed 19 local events (1.5%), 12 regional events (1%), and 20 distant metastases (1.6%). Five-year overall survival was 98.6%.
Conclusions.
Clinically occult (nonpalpable) carcinomas show very favorable prognostic features and high survival rates, showing the important role of modern imaging techniques.
Introduction
The improved rates of curability of breast cancer have been undoubtedly influenced by the revolution in diagnostic imaging over the last 30 years. The advent of mammography in the 1960s, of ultrasound scan in the 1970s, and of magnetic resonance imaging in the 1990s have greatly improved the ability to recognize very early carcinomas [1–3]. Moreover, the great development of conservative techniques to preserve the breast in the majority of cases and also preserve the axillary lymph nodes, when not involved, have positively influenced general populations of women and convinced them to undergo regular breast examinations.
All this has led to the frequent observation of occult carcinomas, detectable only by special diagnostic equipment. The rates of the “nonpalpable” tumors increase year by year and today account for some 20% of all breast cancers treated in oncological institutes and breast units in general hospitals [4–6].
At the European Institute of Oncology (IEO), between the years 2000 and 2006, we treated 1,258 patients whose diagnosis of breast cancer was obtained solely by images, and without any clinical signs. We analyzed the whole series of those nonpalpable cancers to evaluate the rate of local recurrences, of distant metastases, and of long-term curability.
Patients and Methods
From January 2000 to December 2006 2,917 patients were treated at the IEO for breast lesions discovered by mammography, ultrasound, or magnetic resonance imaging (MRI), which were not perceivable at palpation.
Of the 2,917 cases, 1,482 (50.8%) had a final diagnosis of carcinoma, whereas 597 (20.5%) were ductal intraepithelial neoplasias (DIN) (ductal carcinoma in situ) 1, 2, or 3. The 2,067 cases (carcinoma plus DIN) represented the 13% of a total of 16,000 patients with breast carcinomas and DINs treated in the same period of time.
An additional 838 (28.7%) cases were benign. Of the 1,482 cases of occult carcinoma, 224 had suffered from previous oncological events and were therefore not considered. Table 1 shows the type of imaging presentation: half of the cases showed a breast nodule, and in another 9% the isolated breast nodule was accompanied by microcalcifications. Microcalcifications only were present in 17.1% of the cases. A suspicious opacity was present in 9.8% of the cases, whereas suspicious distortion and thickening represented the remaining 13.7% of the cases.
Table 1.
Presentation at imaging
The distribution of the 1,258 cases according to various parameters is shown in Table 2.
Table 2.
Description of characteristics
aSNB not performed in 34 patients.
bInformation is missing for some patients.
Surgery
All nonpalpable tumors were treated with an innovative surgical technique that we defined as ROLL (radioguided occult lesion localization), as described in previous papers [7, 8].
Briefly, excision biopsy is guided by a handheld γ-ray detection probe (Neo2000; Neoprobe Corporation, Dublin, OH) after the injection of a macroaggregate of 99Tc-labeled human serum albumin (Maasol; GE Healthcare, Netherlands) into the center of the suspicious lesion using either stereotactic mammography guidance (when only microcalcifications were present) or ultrasounds graphic guidance for the operation.
Using the probe, the surgeon is able to find the skin projection of the lesion and decide the most appropriate incision. After incision of the skin, the area of maximum radioactivity, which corresponds to the site of the lesion, is identified using the probe. The edges of the excision are defined as the locus of points surrounding the hot spot where radioactivity falls off sharply. After excision of the specimen, the probe is used to check for residual radioactivity at the excision site; if this is present, the excision is enlarged.
Axillary Nodes
As a rule, axillary nodes are not dissected at our institute unless affected by metastases, mostly identified by the sentinel node biopsy (SNB) procedure [8–10]. In 1,224 cases, SNB was performed. In 970 (79.3%) cases, patients proved negative and the axillary nodes were not removed. In 254 (20.7%) cases the positive SNB led to axillary clearance. The distribution of cases according to the extent of axillary nodes involvement is shown in Table 2.
Radiotherapy
Whole breast radiotherapy or partial breast intraoperative irradiation in a single dose (21 Gy) with ELIOT were regularly administered.
Systemic Treatments
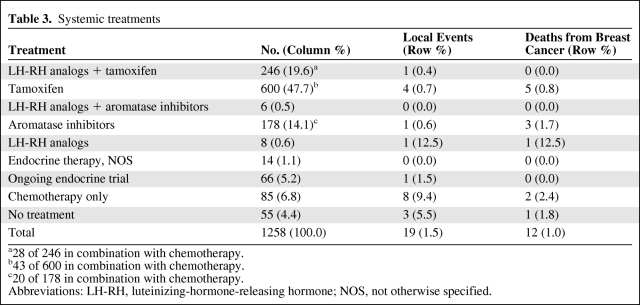
Patients with positive estrogen receptor tumors and/or progesterone receptor tumors were proposed tailored endocrine treatment, whereas patients with negative estrogen and progesterone receptors were proposed either chemotherapy or no treatment. In Table 3, all systemic treatments administered are summarized: 246 (20.3%) patients had ovarian suppression with luteinizing-hormone-releasing hormone analogs plus tamoxifen (28 of 246 in combination with chemotherapy), 6 (0.5%) ovarian suppression plus aromatase inhibitors (AI), 600 (4770%) tamoxifen alone (43 of 600 in combination with chemotherapy), and 178 (14.1%) AI alone (20 of 178 in combination with chemotherapy). Twenty-two cases (1.7%) received another endocrine treatment whereas 66 cases (5.2%) were in ongoing double-blind trials. Eighty-five patients (6.8%) received chemotherapy, whereas 55 patients (4.4%) did not receive any treatment.
Table 3.
Systemic treatments
a28 of 246 in combination with chemotherapy.
b43 of 600 in combination with chemotherapy.
c20 of 178 in combination with chemotherapy.
Abbreviations: LH-RH, luteinizing-hormone-releasing hormone; NOS, not otherwise specified.
Statistical Considerations
Primary endpoints were cumulative incidence of local events and overall survival. Cumulative incidence of local events was computed in a competing risk framework as described by Marubini and Valsecchi [11], and compared across different subgroups by means of the Gray test [12]. Overall survival was defined as the time interval from surgery to death from any cause or last date of follow-up, and plotted using the Kaplan-Meier method. All analyses were performed with the SAS software (SAS Institute, Cary, NC) and the R software (The R Development Core Team 2004; Free Software Foundation, Boston, MA).
Follow-up
The patients were followed with an annual mammography and ultrasound scan and MRI when required. Lung, bones, and liver examinations were performed whenever a suspicion was present and were carried out yearly in cases with a substantial axillary involvement. The average follow-up time is 60 months (range 1–111 months).
Results
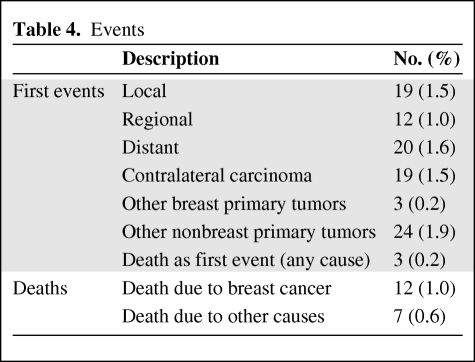
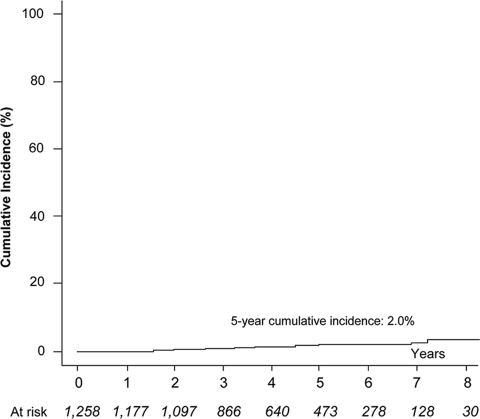
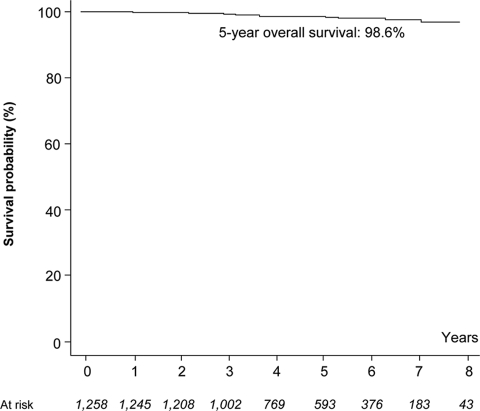
The long-term observation of the cases showed a limited number of local events (19%–1.5%) and of regional events (12%–1.0%). Twenty cases developed distant metastases (1.6%), 19 cases developed contralateral carcinoma (1.5%), 3 cases developed a new breast primary carcinoma (0.2%), and 24 cases developed primary carcinoma in other organs (1.9%). Deaths due to breast cancer were 12 (1.0%) and 7 other patients died from other causes (0.6%) (Table 4).
Table 4.
Events
The cumulative incidence of local events is shown in Figure 1. In Figure 2 the curve shows the overall survival (98.6% at 5 years).
Figure 1.
Cumulative incidence of local events.
Figure 2.
Overall survival.
Discussion and Conclusions
The first comment to be made on analyzing the present series is that the incidence of occult, nonpalpable breast carcinomas is progressively increasing and we expect that in the future a considerable proportion of breast carcinoma will fall into this category. It is therefore important that current practice includes the evaluation of case series of occult carcinomas.
The second observation refers to the ability of radioguided surgery to identify the occult lesion and to make an immediate extensive breast resection with good and safe margins of normal tissue around the primary lesion.
A third important point regards the characteristics of these lesions whose parameters show values indicating low aggressivity. Most patients (68.9%) have a low proliferative rate, grade 3 cases are infrequent, endocrine receptors have high values in most cases, and Her2/neu is rarely overexpressed. The condition of low malignancy may be interpreted as a selection of the cases, as patients with highly proliferative cancer will quickly become palpable and will therefore not fulfill the conditions for accrual in the present series. Another hypothesis is that small carcinomas have low aggressivity, which will increase with time, because of a clonal selection leading to progressive predominance of the more aggressive clones.
Finally, the fourth and most important point is the exceptionally high curability of these patients. The curve of overall survival shows a survival of 98.6% at 5 years. During the observation period only 12 patients died from breast carcinoma (1%).
The very high level of curability of patients whose breast carcinoma is not palpable and is discovered only with mammography, ultrasound, and MRI underlines the fundamental role of the imaging progress for the control of this disease.
Nevertheless, the data presented must not lead to the conclusion that detection of breast carcinoma in its occult stage can by itself solve the breast cancer problem as the selection bias (length bias) and the lead-time bias may exert an important influence.
We are aware that a number of occult carcinomas discovered with modern imaging techniques might be harmless and that surgical treatment may be an overtreatment.
For this reason we are planning a randomized trial in healthy women where half of them are submitted to the normal control (mammography every second year) and the other half to a very intense program such as annual mammography plus ultrasound examination every 6 months and MRI every year in selected cases.
If the trial will show that patients submitted to the intense detection program will be cured in a higher proportion compared to patients following the present screening procedure, the conclusion will lead to new updated programs for breast cancer control.
Moreover, the trial will hopefully clarify the advantages of early detection programs in terms of improved survival and the disadvantages in terms of overdiagnosis and overtreatment. Recent data from Swedish and English screening programs show that the benefit of screening in terms of life saved is greater in absolute terms than the harm in terms of overdiagnosis [13]. Another recent paper shows that the breast density is an obstacle to mammographic diagnosis and that other diagnostic techniques (US or MRI) should be introduced in future detection programs [14].
Acknowledgments
The authors thank William Russell-Edu for help with the English language and Maria Grazia Villardita for her constant help in the preparation of the manuscript.
Author Contributions
Conception/Design: Umberto Veronesi
Provision of study material or patients: Umberto Veronesi, Alberto Luini, Stefano Zurrida, Simonetta Monti, Viviana Galimberti, Enrico Cassano, Nicole Rotmensz, Fabio Bassi, Loredana Burgoa, Paolo Veronesi
Collection and/or assembly of data: Edoardo Botteri, Stefano Zurrida, Simonetta Monti, Enrico Cassano, Antuono Latronico, Maria Pizzamiglio, Nicole Rotmensz, Simona Musmeci, Fabio Bassi, Loredana Burgoa, Giovanni Paganelli
Data analysis and interpretation: Umberto Veronesi, Alberto Luini, Edoardo Botteri, Viviana Galimberti, Giuseppe Viale, Dario Vezzoli, Simona Musmeci, Patrick Maisonneuve, Paolo Veronesi
Manuscript writing: Umberto Veronesi
Final approval of manuscript: Umberto Veronesi, Alberto Luini, Edoardo Botteri, Stefano Zurrida, Simonetta Monti, Viviana Galimberti, Enrico Cassano, Antuono Latronico, Maria Pizzamiglio, Giuseppe Viale, Dario Vezzoli, Nicole Rotmensz, Simona Musmeci, Fabio Bassi, Loredana Burgoa, Patrick Maisonneuve, Giovanni Paganelli, Paolo Veronesi
References
- 1.Frank HA, Hall FM, Steer ML. Preoperative localization of nonpalpable breast lesions demonstrated by mammography. N Engl J Med. 1976;295(5):259–260. doi: 10.1056/NEJM197607292950506. [DOI] [PubMed] [Google Scholar]
- 2.Tabar L, Yen MF, Vitak B, et al. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361(9367):1405–1410. doi: 10.1016/S0140-6736(03)13143-1. [DOI] [PubMed] [Google Scholar]
- 3.Weiss L, Rosner D, Glenn WE. Visualization of breast lesions with an advanced ultrasonic device: results of a pilot study. J Surg Oncol. 1978;10(3):251–271. doi: 10.1002/jso.2930100312. [DOI] [PubMed] [Google Scholar]
- 4.Schreiman JS, Gisvold JJ, Greenleaf JF, et al. Ultrasound transmission computed tomography of the breast. Radiology. 1984;150(2):523–530. doi: 10.1148/radiology.150.2.6691113. [DOI] [PubMed] [Google Scholar]
- 5.El Yousef SJ, Duchesneau RH, Alfidi RJ, et al. Magnetic resonance imaging of the breast. Work in progress. Radiology. 1984;150(3):761–766. doi: 10.1148/radiology.150.3.6695077. [DOI] [PubMed] [Google Scholar]
- 6.Luini A, Zurrida S, Paganelli G, et al. Comparison of radioguided excision with wire localization of occult breast lesions. Br J Surg. 1999;86(4):522–525. doi: 10.1046/j.1365-2168.1999.01078.x. [DOI] [PubMed] [Google Scholar]
- 7.De Cicco C, Pizzamiglio M, Trifirò G, et al. Radioguided occult lesion localisation (ROLL) and surgical biopsy in breast cancer. Technical aspects. Q J Nucl Med. 2002;46(2):145–151. [PubMed] [Google Scholar]
- 8.Paganelli G, Luini A, Veronesi U. Radioguided occult lesion localization (ROLL) in breast cancer: maximizing efficacy whilst minimizing mutilation. Ann Oncol. 2002;13:1839–1840. doi: 10.1093/annonc/mdf343. [DOI] [PubMed] [Google Scholar]
- 9.Veronesi U, Paganelli G, Viale G, et al. Sentinel-lymph-node biopsy as a staging procedure in breast cancer: update of a randomised controlled study. Lancet Oncol. 2006;7(12):983–990. doi: 10.1016/S1470-2045(06)70947-0. [DOI] [PubMed] [Google Scholar]
- 10.Veronesi U, Galimberti V, Paganelli G, et al. Axillary metastases in breast cancer patients with negative sentinel nodes: a follow-up of 3548 cases. Eur J Cancer. 2009;45(8):1381–1388. doi: 10.1016/j.ejca.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 11.Marubini E, Valsecchi MG. Chichester, England: Wiley; 1995. Analysing Survival Data from Clinical Trials and Observational Studies; p. 331. [Google Scholar]
- 12.Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Statist. 1988;16:1141–1154. [Google Scholar]
- 13.Duffy SW, Tabar L, Olsen AH, et al. Absolute numbers of lives saved and overdiagnosis in breast cancer screening, from a randomized trial and from the Breast Screening Programme in England. J Med Screen. 2010;17:25–30. doi: 10.1258/jms.2009.009094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiu SYH, Dutty S, Yen A M-H, et al. Effect of baseline breast density on breast cancer incidence, stage, mortality, and screening parameters: 25-year follow-up of a Swedish mammographic-screening. Cancer Epidemiol Biomarkers Prev. 2010;19(5):1219–1228. doi: 10.1158/1055-9965.EPI-09-1028. [DOI] [PubMed] [Google Scholar]