This study quantified the economic burden for informal caregivers of lung cancer and colorectal cancer patients, by cancer type, phase of disease, stage at diagnosis, patient age, and relationship, and found this burden to be substantial.
Keywords: Informal care, Opportunity costs, Out-of-pocket costs, Cancer caregiving, Stage of disease, Phase of disease, Lung cancer, Colorectal cancer
Abstract
Background.
Informal care provides many benefits to cancer patients, but can be costly to caregivers. This study quantified the economic burden for informal caregivers of lung cancer (LC) and colorectal cancer (CRC) patients, examining differences by cancer type, phase of disease, stage at diagnosis, patient age, and relationship.
Methods.
A cross-sectional survey of caregivers of LC and CRC patients participating in the Share Thoughts on Care survey was conducted. Economic burden was calculated using the opportunity cost of caregiver time, the value of work hours lost, and out-of-pocket expenditures. Factors associated with economic burden to caregivers were modeled using fixed-effects generalized least squares estimation.
Results.
Informal caregivers (1,629) completed mailed surveys. Of these, 663, 822, and 144 were surveyed during the patient's initial phase (first year after diagnosis, not within 6 months of death), continuing phase (after 1 year, not within 6 months of death), and terminal phase (within 6 months of death) of disease, respectively. The accumulated economic burdens for caregivers were $7,028, $19,701, and $14,234 for those evaluated during the patient's initial phase, continuing phase, and terminal phase of disease, respectively. Economic burden was higher for caregivers of LC patients than CRC patients (p = .044) and for caregivers of patients diagnosed at stage 4 versus stage 1 (p = .001). Spouses faced higher economic burden than other relatives (p = .000) or friends (p = .000).
Conclusions.
Economic burden for informal caregivers of LC and CRC patients is substantial and should be included in estimates of the societal cost of cancer care.
Background
Informal care of persons with a serious medical illness provides many benefits to patients, but can be costly to family members and friends both in monetary terms and in terms of the value of time spent in caregiving and learning new caregiving skills. Researchers have found that caregiving leads to reduced working hours [1–4] or wage penalties [5], significant outlays for medical treatment [6, 7], as well as other direct costs such as hiring of home health workers. Caregivers also sacrifice leisure time and time managing a patient's treatment, among other indirect costs.
Lung cancer (LC) and colorectal cancer (CRC) are among the most common [8] types of cancer, and patients with these cancers often have substantial caregiving needs. Prior studies have evaluated the economic impact of caregiving in the last year of life [9], but few studies have looked at the economic impact of caregiving across various phases or stages of disease. Both cancer-related morbidity and morbidity related to treatment vary greatly depending on stage at diagnosis and phase of disease. These differences are likely to represent different costs for caregivers.
To better understand the costs for caregivers, we conducted a retrospective analysis of economic burden based on a survey of informal caregivers of LC and CRC patients. We hypothesized that the economic burden for caregivers would be higher for LC patients than for CRC patients, higher in the terminal phase of disease (than in the initial and continuing phases), higher with later stage of disease at diagnosis, higher with older patient age at diagnosis, and be highest for spouses because of the financial interdependence of the marital relationship.
Methods
Study Design
A retrospective analysis of the total economic burden experienced by caregivers of LC and CRC patients was conducted using caregiver-reported data from the 2005 Share Thoughts on Care mailed survey. Caregivers were nominated by a consecutive subsample of recently diagnosed LC and CRC patients in the Cancer Care Outcomes Research and Surveillance (CanCORS) consortium study. The CanCORS consortium is comprised of seven independent study sites that used identical lock-step data collection methods. Five of the seven sites obtained patients from cancer registries and two obtained patients from health care systems. The CanCORS consortium [10] and Share Thoughts on Care Survey [11] are described in more detail elsewhere.
Two separate cross-sectional samples of caregivers were evaluated, either 6 months to 1 year after the patient's cancer diagnosis or 1–2 years after the patient's cancer diagnosis. Because caregivers were interviewed at different points in time, and reflect distinct periods in which the economic burden was accrued based on the patient's clinical course, we focused the analysis on the following three categories: (a) caregivers surveyed during the patient's initial phase of disease, defined as up to 1 year since diagnosis but not in the 6 months before the patient's death; (b) caregivers surveyed during the patient's terminal phase of disease, or 6 months before the patient's death; and (c) caregivers surveyed during the patient's continuing phase of disease, encompassing all other time periods (≥1 year postdiagnosis, but not within 6 months of the patient's death).
Of the 3,056 identified caregivers who were sent a survey, 383 were ineligible because the cancer patient had not needed or received informal care at the time and 87 were ineligible for other reasons, such as language barriers, a wrong address, or the patient was deceased. Of the remaining 2,586 active caregivers, 1,629 returned a completed survey, for a response rate of 63%. Of the 1,629 caregivers remaining, 663 respondents were evaluated during the patient's initial phase of disease, 822 were evaluated during the patient's continuing phase of disease, and 144 were evaluated during the patient's terminal phase of disease.
The vast majority of caregivers (85%) reported that they provided either half or all of the help the care recipient needed in the home. The remaining 15% provided less than half of the informal care that the cancer patient received. We did not exclude caregivers who reported providing less than half of all care, but controlled for variations in effort in the multivariable models.
Caregiver survey data were merged with patient survey (version 5.1.2) and medical record (version 1.9) information in order to include the patient's date of diagnosis, cancer type, stage at diagnosis, and phase of disease at the time of the caregiver survey, and other patient characteristics.
Measures
Total Economic Burden
We calculated the total economic burden for informal caregivers by valuing the time spent on direct caregiving effort and direct expenditures spent on cancer care of the patient. All costs are in 2005 dollars. Time costs are the total value of a caregiver's time spent providing informal care since the onset of the patient's cancer. We multiplied a caregiver's hourly wage by the hours of informal care they reported providing in a typical week, and then by the total weeks elapsed between the date of diagnosis and the survey date.
For employed caregivers, self-reported hourly wage rates were used. One's wage rate shows the opportunity cost of caregiving, or how much money a caregiver could have earned at work in the amount of time devoted to direct care effort. For caregivers not working for pay, we valued an hour spent on informal care using minimum wage rates [12], a conservative approach.
Nontime costs were comprised of direct out-of-pocket expenditures for the patient's medical care as well as nonmedical expenditures, such as home modifications or transportation, or help with activities of daily living and instrumental activities of daily living and skilled nursing help. If home health care was purchased and the rate was missing, we assigned the median home health care worker wage. Finally, a caregiver who relocated to provide informal care was assumed to have incurred $3,000 in moving expenses.
Type of Cancer
The two cancer types examined were CRC and LC.
Classifying Patient Severity: Phase, Stage, and Comorbid Conditions
We accounted for the phase of disease the patient was in at the time of the caregiver survey—initial, continuing, or terminal. It is important to keep in mind that economic burden is the cumulative costs to caregivers from the date of a patient's diagnosis until the date of the caregiver survey. Some of the economic burden, therefore, occurred at a phase of disease different from the one that the patient was in at the time of the caregiver survey.
Following Brown and colleagues [13], we also examined cumulative economic burden by stage of disease at diagnosis, using the following classifications: (a) stage 1, stage 0 or stage I; (b) stage 2, stage II or local site of cancer; (c) stage 3, stage III or regional site of cancer; (d) stage 4, stage IV or distant site of cancer; and (d) a dichotomous variable of “missing stage.”
A patient who had surgery, chemotherapy, or radiation treatment in the 3 months prior to the caregiver survey was considered to have been in recent treatment (Treatment = 1). Another signal of greater severity that was measured was whether or not a paid helper in the home had been hired since the cancer diagnosis.
Patient Demographics
Patient age was assessed through self-report and coded as ≥65 years or <65 years. Further details on age were masked to protect the confidentiality of respondents. Gender, marital status, race and ethnicity, and education also characterized patients.
The caregiver–patient relationship was assessed using the question “What is your relationship to the person you are helping?” Response options included husband or wife; girlfriend, boyfriend or romantic partner; son or daughter; mother or father; sister or brother; friend; other family member; and other. The relationship was important because spousal caregivers generally provide the most intensive care [14], and because financial outlay may differ by relationship. We further controlled for whether a caregiver provided almost or all (reference), half, or less than half of all caregiving, given that economic burden is likely to be less for less intensive caregivers.
Patient Health
In the CanCORS consortium patient survey, patients completed the mental component summary (MCS) and physical component summary subscales of the SF-12 [15]. Higher scores indicate better health.
Caregiver Health, Demographics, and Economic Resources
Caregiver health was measured by the number of comorbid conditions and the Center for Epidemiologic Studies–Depression (CES-D) score [16]. Caregiver age was measured as <65 years or ≥65 years, education was measured in years, and race/ethnicity was assessed. Caregiver economic resource measures were annual household income (including retirement income), work status, and health insurance status.
Statistical Analysis
Descriptive and Bivariate Analyses
We examined the mean total economic burden for the full sample and by phase of the patient's disease using an opportunity cost to value a caregiver's time.
LC and CRC patients typically have different courses of treatment and survival times, and thus their informal caregivers may experience different economic burdens. We examined whether economic burden was significantly different by cancer type of the patient using two-sided exact χ2 tests. A Chow test was used to establish the appropriateness of pooling the data by cancer type (LC and CRC) [17].
Multivariable Analysis
We tested the following hypotheses using multivariable cost models: (a) the total economic burden of informal care is higher for LC patients than for CRC patients; (b) the total economic burden of informal care is higher in the terminal phase of disease than in other phases; (c) the total economic burden of informal care is higher with later stage at diagnosis than with earlier stage at diagnosis; (d) the total economic burden of informal care is higher with greater patient age; and, finally, (e) the total economic burden of informal care is higher for caregivers married to care recipients than for other caregivers.
 |
Total economic burden included time costs and expenditures born by the caregiver resulting from cancer care since diagnosis. Subscript c refers to caregiver characteristics and subscript p refers to patient characteristics. We statistically adjusted for caregivers evaluated at different phases of the patient's disease—initial and terminal (continuing was the reference group). We tested the hypotheses by examination of the sign and significance of the key covariates of interest—cancer type, stage, phase, age, and caregiver relationship. Patient demographics were highly correlated with caregiver demographics and thus, except for age and patient gender, were excluded.
We examined the skewness of the cost data to ascertain whether a semilogarithmic regression model was appropriate. The Kennedy correction [18] for dichotomous explanatory variables was applied to interpret marginal effects. Cancer patients were from seven health care centers and thus we controlled for site-specific heterogeneity using fixed-effects generalized least squares (GLS) models based on joint F-tests of the site dummy variables. Hausman tests ascertained whether fixed effects were preferred to random effects. Stata 10.0 SE (StataCorp LP, College Station, TX) was used for the analysis.
Results
The caregivers in the sample had been caring for their cancer patients for about 1 year, on average, at the time of the caregiver interview, with caregivers evaluated during the patient's initial or terminal phase of disease having a shorter duration of care (29.9 weeks and 37 weeks, respectively) than those evaluated during the patient's continuing phase of disease (71.5 weeks). Caregivers were primarily married, white, females aged <65 years, and around half of the caregivers reported working for pay (Table 1). About 64% of the caregivers were spouses of the patient and 32% were other relatives (Table 1). The average CES-D score for caregivers was 8, and this was higher for caregivers of patients in the terminal phase of disease. A CES-D score >8 suggests clinically significant depressive symptoms [16].
Table 1.
Caregiver characteristics by patient phase of disease at caregiver survey and for the full sample (n = 1,629)
aCaregivers could report multiple race categories.
bA value of 5 indicates an annual total household income of $20,000–$39,999. This variable includes income from jobs, self-employment, Social Security, Railroad Retirement, other retirement income source, Supplemental Security Income, pensions, interest, and any other sources.
cCategory means do not add up to 1 because a caregiver can have multiple insurance plans.
Most patients (85%) in the terminal phase of disease were LC patients and 15% were CRC patients (Table 2). Similarly, 44.4% of patients in the terminal phase had stage 4 disease at diagnosis, whereas patients in the initial or continuing phases of disease were in an earlier stage, on average. Across the full sample (Table 2), 31% of caregivers cared for patients diagnosed at stage 3, 27% cared for patients diagnosed at stage 1, 18.9% cared for patients diagnosed at stage 2, and 16.2% cared for patients diagnosed at stage 4.
Table 2.
Patient characteristics by patient phase of disease at caregiver survey and for the full sample of caregivers
Abbreviations: CRC, colorectal cancer; MCS, mental component summary; PCS, physical component summary.
Bivariate Analysis of Differences in Economic Burden by Type of Cancer
There were no differences in economic burden from direct caregiving effort or total economic burden by type of cancer (results not shown). Additionally, a Chow test showed it was appropriate to pool the data across cancer types.
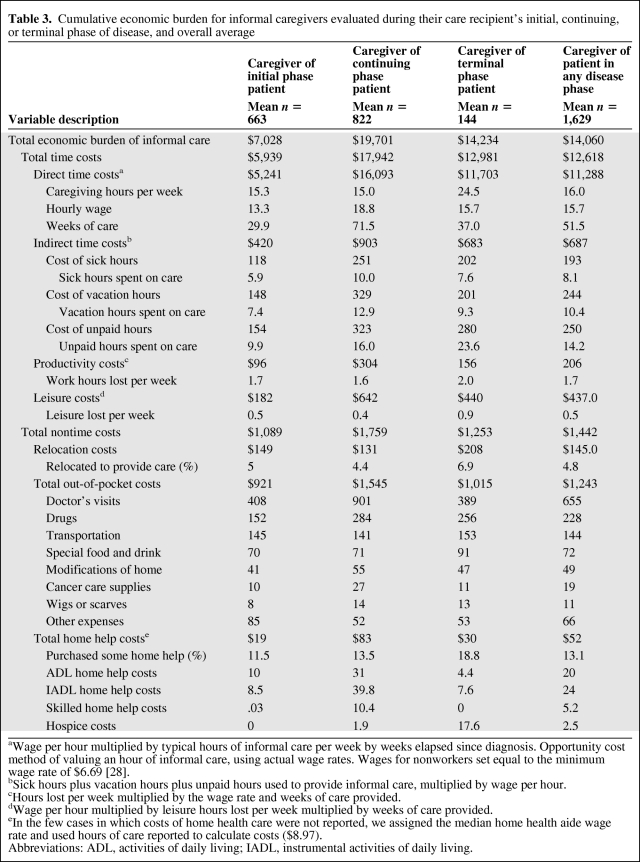
Total Economic Burden of Caregiving
We present a detailed breakdown of costs for all caregivers and by the patient's phase of disease in Table 3. For the full sample of caregivers, the average accumulated total economic burden was $14,000 (Table 3), accrued roughly over 1 year since diagnosis. The total economic burden for caregivers evaluated during the patient's initial phase of disease averaged $7,028; for those evaluated during the patient's terminal phase of disease, it was $14,234, and for those evaluated during the patient's continuing phase of disease, it was $19,701. For caregivers evaluated during the patient's continuing phase, costs had accrued over 17 months since diagnosis on average, compared with roughly 7 months and 8 months for caregivers of initial and terminal phase patients, respectively.
Table 3.
Cumulative economic burden for informal caregivers evaluated during their care recipient's initial, continuing, or terminal phase of disease, and overall average
aWage per hour multiplied by typical hours of informal care per week by weeks elapsed since diagnosis. Opportunity cost method of valuing an hour of informal care, using actual wage rates. Wages for nonworkers set equal to the minimum wage rate of $6.69 [28].
bSick hours plus vacation hours plus unpaid hours used to provide informal care, multiplied by wage per hour.
cHours lost per week multiplied by the wage rate and weeks of care provided.
dWage per hour multiplied by leisure hours lost per week multiplied by weeks of care provided.
eIn the few cases in which costs of home health care were not reported, we assigned the median home health aide wage rate and used hours of care reported to calculate costs ($8.97).
Abbreviations: ADL, activities of daily living; IADL, instrumental activities of daily living.
The mean time cost for caregivers overall was $12,618, and it ranged from $5,939 when caregivers were evaluated during the patient's initial phase of disease to $17,942 when caregivers were evaluated during the patient's continuing phase of disease (Table 3). Continuing phase caregivers had the highest costs because they had provided care for the longest and economic burden was measured cumulatively. Time costs comprised 91% of the total economic burden for caregivers.
Of the total informal care time costs, the caregiver's direct care effort contributed to the majority of the total time costs across all phases of disease (averages of $5,241, $16,093, and $11,703 by phase, respectively, and $11,288 overall). The remainder of the time costs was from indirect time costs, such as the value of sick leave, unpaid hours, lost productivity, and lost leisure time (Table 3).
In the category of nontime costs, total out-of-pocket costs were the largest (mean of around $1,089, $1,759, and $1,253 by phase, respectively, and $1,442 across the full sample). The largest share of out-of-pocket costs came from direct medical expenditures on cancer care—doctor's visits and drugs for the patient (Table 3). The largest category of nonmedical expenditures resulting from cancer care was the value of time spent transporting patients to medical appointments ($145, $141, and $153 by phase, respectively). A small proportion of caregivers reported purchasing help for the patient in the home, and this varied by phase, with nearly 19% of caregivers of terminal patients purchasing help in the home, versus 13.5% of caregivers of continuing phase patients (Table 3).
Multivariable Results
A fixed-effects GLS semilogarithmic regression model was estimated to test the hypotheses. This specification was chosen because a joint F-test on the site dummy variables showed that they were significant at the 1% level (χ2 = 51.93) and a Hausman test did not reject in favor of random effects (χ2 = 54.11) We took the natural log of the dependent variable (all values were nonzero and positive) to correct for skewness (−0.38).
Controlling for phase of disease and other important factors hypothesized to affect economic burden, the total cumulative economic burden for caregivers was 16.5% lower for CRC patient caregivers than for LC patient caregivers (p = .032). Caregivers of initial phase patients had a 46.0% lower total economic burden than caregivers of continuing phase patients (p = .000) but caregivers of terminal phase patients were no different from caregivers of continuing phase patients (p = .486). Caring for a patient diagnosed with cancer at stage 4 was associated with a 53.9% higher economic burden than caring for a patient diagnosed at stage 1 (p = .001). Correlation between stage and phase was low (maximum correlation was 0.22 between stage 4 and terminal phase), justifying both variables in the model. Caregivers of patients aged ≥65 years faced no higher economic burden than caregivers of patients aged <65 years (p = .475), lending no support to our hypothesis that costs to informal caregivers would be higher with older patient age.
Our final hypothesis, that is, that economic burden would be higher for spouse caregivers, was supported. Caregivers who were nonspousal relatives had a 43% lower total economic burden than spouses (p = .000), whereas friends had a 59% lower economic burden than spouses (p = .000) (Table 4). That said, married caregivers had a lower economic burden than unmarried caregivers (by 26%).
Table 4.
Factors associated with total economic burden faced by informal caregivers of lung and colorectal cancer patients, measured as opportunity costs of a caregiver's time (model (1), n = 1,629)
*Significant at the 5% level; **significant at the 1% level.
aKennedy correction applied to dichotomous variables to correctly interpret the marginal effects [18].
Abbreviations: MCS, mental component summary; PCS, physical component summary.
The total economic burden for caregivers of male patients was 29% lower than that for caregivers of female patients (p = .001). Working caregivers had nearly 100% higher total costs of informal care than nonworkers (p = .000), reflecting in part the higher wages of workers than of nonworkers. Similarly, caregivers whose patients had a paid helper in the home had a 74% higher total economic burden (p = .000), holding all else constant. Caring for a patient who had a better SF-12 MCS score was associated with a significantly lower economic burden that was very small in magnitude (p = .001). A one-unit higher patient MCS score was associated with a 2% lower economic burden.
Sensitivity Analysis
Because total hours of informal care were calculated using self-reported information on the hours provided in a typical week since the patient's diagnosis, there was a concern that this approach overestimated the accumulated total hours of caregiving and the economic burden from direct caregiving effort. We therefore assumed that active caregiving occurred in only 50% and 75% of the weeks since the cancer patient's diagnosis, and re-examined the average economic burden. Under these assumptions, the total cumulative economic burden for informal caregivers across the full sample averaged $8,343 (50% of the weeks) and $11,165 (75%), compared with the main results average of $14,060.
Conclusions
The economic burden experienced by caregivers of LC and CRC patients was significant, ranging from $7,028 for caregivers surveyed when their care recipient was in the initial phase of disease, to $14,234 for caregivers surveyed when the patient was in the terminal phase of disease, and to $19,701 for caregivers surveyed when their care recipient was in the continuing phase of disease. Comparing economic burden for initial and terminal phase patients can be done with a similar time frame in mind (about 7 months), but continuing phase patients had over twice as much time to accrue economic burden (average, 16.7 months). The overall average economic burden for caregivers was around $14,000 (economic burden accrued for 1 year since the patient's diagnosis, on average).
The majority of the total economic burden experienced by informal caregivers of cancer patients—91%—arose from the direct effort of providing informal care to the patient. Nontime costs, comprised of out-of-pocket costs for cancer care, purchases of help in the home, and relocation costs, accounted for the remaining 9%. Given that these latter categories represent direct outlays reported by caregivers ($1,000–$1,800 depending on phase of disease), this category of costs should be of particular concern.
We tested five hypotheses in the multivariable models. Economic burden was greater for caregivers of LC patients than for caregivers of CRC patients, for caregivers evaluated during the patient's continuing phase of disease than for those evaluated during the patient's initial phase of disease, for caregivers of patients diagnosed at stage 4 than for caregivers of those diagnosed at stage 1, and for spousal caregivers than for other relatives and friends. Economic burden did not differ by patient age. Although not a hypothesis, the finding that workers experienced two to three times the economic burden of nonworkers reflects the importance of exploring workplace policy solutions to assist employed informal caregivers.
The total average economic burden for cancer caregivers, $14,000 after 1 year of caregiving, on average, is within the range of other studies. Hayman and colleagues used national data to examine the incremental cost of having cancer treatment in the last year on the intensity and cost of informal care [9]. They found that cancer treatment was associated with an incremental increase of 3.1 hours per week of informal care, which translated into an additional average yearly cost of $1,200 per patient. This finding is difficult to compare with our findings, because they measured the marginal effect of cancer caregiving in situations in which informal caregiving for other reasons was already taking place. We only measured cancer caregiving effort.
Other studies specifically examining the costs of adult cancer care found that total informal costs were $4,563–$7,290, on average, for a 3-month period, with the higher end of the range for caregivers of patients in the last 6 months of life [19, 20]. Our estimate of costs during the last 6 months of life—$14,234 for terminal phase patients—is at the upper range of these estimates. Regarding out-of-pocket costs, our totals (around $100–$150 per month, on average, depending on the group) are much less than the $500 a month estimated in another study of cancer caregivers in Canada [21].
There are five limitations to keep in mind when interpreting the results from this cross-sectional study. First, valuing caregiving effort for nonworkers at the minimum wage rate may not be accurate because skilled cancer-related care would correspond to a higher wage rate in the labor market [20]. Thus, this approach may have led to an underestimate of time costs for a substantial proportion of the sample (50% were nonworkers). Second, in our study, economic burden was measured for a single informal caregiver per cancer patient, so the total economic burden faced by the full network of informal caregivers per care recipient could actually be much higher [20]. Third, our study does not account for the potential health care costs to caregivers of their own health declines resulting from caregiving, despite evidence that informal care can be harmful to the physical and mental health of spousal [22–24] and adult children [25] caregivers. Fourth, the results of this study may not correspond to a nationally representative sample of cancer caregivers. The characteristics of the nonresponding caregivers are unknown, but there is considerable evidence from other studies to suggest that nonrespondents are more likely to be low income, non-white, and sicker than respondents [26, 27]. If this is true, our results may underestimate the experiences of the caregivers of the sickest cancer patients, as well as the proportion of caregivers who are poor and themselves struggling with ill health [11]. These first four limitations suggest that economic burden may have been underestimated in our study.
Fifth, however, is a concern that recall bias on the typical weekly hours of informal care provided may have led to an inaccurate estimate of the time costs of caregiving. If hours of care are reported from recent weeks instead of an average across all weeks of care, and recent weeks are higher than the average, the total accumulated time costs will be overestimated. Or, it could be that the longer-term caregivers (continuing care or terminal care) do not remember as well what their care intensity was in the initial weeks, so that their average estimates are biased versus initial caregivers. Therefore, in an effort to provide a lower bound of economic burden, we performed a sensitivity analysis to show what the total economic burden would be if care had occurred over fewer total weeks: in this case, the total economic burden would have been $8,000–$11,000, rather than around $14,000. Without follow-up data, we have no way to discern whether the typical hours provided were misreported or whether this resulted in an over- or underestimate of the time spent caregiving since diagnosis. We also cannot be sure how the countervailing effects mentioned in the previous paragraph would offset any overestimate of caregiving hours.
Our study findings indicate that informal caregivers of LC and CRC patients face significant time costs and work lost. The average total economic burden for informal caregivers, $14,000 accumulated over 1 year, on average, is equivalent to 4 or 5 months of an average worker's annual gross salary [28]. Considering the time commitment reported across the different groups, it is important to consider that, although the accumulated costs are higher for the group of continuing care caregivers, who had been providing care the longest, the immediate and short-term economic costs of caregiving are likely highest among terminal cancer caregivers, who averaged 25 hours per week of caregiving, versus 15 hours per week for initial and continuing care caregivers (Table 3). Thus, the economic burden experienced by cancer caregivers should be included in estimates of the cost of cancer care and cost-effectiveness analyses (CEAs) on cancer care across the full spectrum of a cancer caregiving episode, and especially in the terminal phase of caregiving. In any CEA, the researcher needs to decide a priori how to value a caregiver's time: at the opportunity cost of her time, like we did in this study, because it more accurately reflects the full economic cost of caregiving to the caregiver, or at a lower rate, such as the replacement cost of her time (e.g., at a typical home health aide wage rate), which may be more useful when considering policy options that would reimburse informal caregivers at going market rates. CEA researchers could also perform sensitivity analyses on the ideal quantity of informal care received, if there is evidence that the amount of care provided is below the amount indicated clinically because of time or economic constraints faced by the informal caregiver.
In addition, focusing future research and/or interventions on informal caregivers of cancer patients with a higher economic burden, as identified in the present study, spousal caregivers and employed caregivers in particular, may help to guide our efforts to reduce the associated negative health and economic outcomes among at-risk informal caregivers.
Acknowledgments
Deborah Finstad, Sean Phelan, and Michelle Sotak provided able programming and research assistance. Bob Fletcher, Joan Griffin, David Harrington, Haiden Huskamp, Michelle Martin, David Nerenz, Sara Sanders, and Jane Weeks provided very helpful comments. The views expressed represent those of the authors and not those of the National Cancer Institute, National Institutes of Health. All mistakes remain the authors' responsibility.
This work was funded by the National Cancer Institute (U01 CA93324, U01 CA93326, U01 CA93329, U01 CA93332, U01 CA93339, U01 CA93344, and U01 CA93348) and the Department of Veterans Affairs (CRS 02–164). Courtney Van Houtven was supported by the VA Health Services Research and Development Merit Review Program (MRP 05–311).
Author Contributions
Conception/Design: Courtney Harold Van Houtven, Scott D. Ramsey, Mark C. Hornbrook, Audie A. Atienza, Michelle van Ryn
Provision of study material or patients: Mark C. Hornbrook, Michelle van Ryn
Collection and/or assembly of data: Mark C. Hornbrook, Michelle van Ryn
Data analysis and interpretation: Courtney Harold Van Houtven, Scott D. Ramsey, Michelle van Ryn
Manuscript writing: Courtney Harold Van Houtven, Audie A. Atienza
Final approval of manuscript: Courtney Harold Van Houtven, Scott D. Ramsey, Mark C. Hornbrook, Audie A. Atienza, Michelle van Ryn
References
- 1.Carmichael F, Charles S. The opportunity costs of informal care: Does gender matter? J Health Econ. 2003;22:781–803. doi: 10.1016/S0167-6296(03)00044-4. [DOI] [PubMed] [Google Scholar]
- 2.Ettner SL. The impact of “parent care” on female labor supply decisions. Demography. 1995;32:63–80. [PubMed] [Google Scholar]
- 3.Heitmueller A. The chicken or the egg? Endogeneity in labour market participation of informal carers in England. J Health Econ. 2007;26:536–559. doi: 10.1016/j.jhealeco.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Wilson M, Van Houtven C, Stearns S, et al. Depression and missed work among caregivers. J Fam Econ Iss. 2007;28:684–698. [Google Scholar]
- 5.Heitmueller A, Inglis K. The earnings of informal carers: Wage differentials and opportunity costs. J Health Econ. 2007;26:821–841. doi: 10.1016/j.jhealeco.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Langa KM, Fendrick AM, Chernew ME, et al. Out-of-pocket health-care expenditures among older Americans with cancer. Value Health. 2004;7:186–194. doi: 10.1111/j.1524-4733.2004.72334.x. [DOI] [PubMed] [Google Scholar]
- 7.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Cancer Institute. Cancer Trends Progress Report – 2005 Update. [accessed July 19, 2010]. Available at http://progressreport.cancer.gov/trends-glance.asp.
- 9.Hayman JA, Langa KM, Kabeto MU, et al. Estimating the cost of informal caregiving for elderly patients with cancer. J Clin Oncol. 2001;19:3219–3225. doi: 10.1200/JCO.2001.19.13.3219. [DOI] [PubMed] [Google Scholar]
- 10.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: The Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22:2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 11.Van Ryn M, Sanders S, Kahn K, et al. Objective burden, resources, and other stressors among informal cancer caregivers. Psychooncology 2010 Mar 4 [Epub ahead of print] doi: 10.1002/pon.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Department of Labor. Minimum Wage Laws in the States: Historical Table. [accessed July 19, 2010]. Available at http://www.dol.gov/esa/minwage/america.htm.
- 13.Brown ML, Riley GF, Schussler N, et al. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care. 2002;40(8 suppl):IV-104–IV-117. doi: 10.1097/00005650-200208001-00014. [DOI] [PubMed] [Google Scholar]
- 14.Spector WD, Fleischman JA, Pezzin LE, et al. Rockville, MD: Agency for Healthcare Research and Policy; 2000. [accessed July 19, 2010]. The Characteristics of Long-Term Care Users (AHRQ Publication No. 00-0049) Available at http://www.ahrq.gov/research/ltcusers/ltcuse1.htm. [Google Scholar]
- 15.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Hays JC, Blazer DG, Gold DT. CES-D: Cutpoint or change score? J Am Geriatr Soc. 1993;41:344–345. doi: 10.1111/j.1532-5415.1993.tb06718.x. [DOI] [PubMed] [Google Scholar]
- 17.Chow G. Tests of equality between sets of coefficients in two linear regressions. Econometrica. 1960;28:591–605. [Google Scholar]
- 18.Kennedy P. Estimation with correctly interpreted dummy variables in semilogarithmic equations. Am Econ Rev. 1981;71:801. [Google Scholar]
- 19.Stommel M, Given CW, Given BA. The cost of cancer home care to families. Cancer. 1993;71:1867–1874. doi: 10.1002/1097-0142(19930301)71:5<1867::aid-cncr2820710525>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 20.Given BA, Given CW, Stommel M. Family and out-of-pocket costs for women with breast cancer. Cancer Pract. 1994;2:187–193. [PubMed] [Google Scholar]
- 21.Longo CJ, Fitch M, Deber RB, et al. Financial and family burden associated with cancer treatment in Ontario, Canada. Support Care Cancer. 2006;14:1077–1085. doi: 10.1007/s00520-006-0088-8. [DOI] [PubMed] [Google Scholar]
- 22.Schulz R, Belle SH, Czaja SJ, et al. Long-term care placement of dementia patients and caregiver health and well-being. JAMA. 2004;292:961–967. doi: 10.1001/jama.292.8.961. [DOI] [PubMed] [Google Scholar]
- 23.Schulz R, Beach SR, Lind B, et al. Involvement in caregiving and adjustment to death of a spouse: Findings from the caregiver health effects study. JAMA. 2001;285:3123–3129. doi: 10.1001/jama.285.24.3123. [DOI] [PubMed] [Google Scholar]
- 24.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 25.Coe NB, Van Houtven CH. Caring for mom and neglecting yourself? The health effects of caring for an elderly parent. Health Econ. 2009;18:991–1010. doi: 10.1002/hec.1512. [DOI] [PubMed] [Google Scholar]
- 26.Edwards P, Roberts I, Clarke M, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev. 2007;2:MR000008. doi: 10.1002/14651858.MR000008.pub3. [DOI] [PubMed] [Google Scholar]
- 27.Groves RM, Dillman DA, Eltinge J, et al. Survey Nonresponse. New York: Wiley: 2001. pp. 1–525. [Google Scholar]
- 28.BLS: Bureau of Labor Statistics. National Comparison Survey: Wages. Table 3: Civilian Full-Time Workers: Mean and Median Hourly, Weekly, and Annual Warnings and Mean Weekly and Annual Hours. [accessed July 19, 2010.]. Available at http://www.bls.gov/ncs/ocs/sp/nctb0162.pdf.