Attitudes, norms, behavioral control, and chemotherapy patients' intentions to participate in medical error prevention were examined using the theory of planned behavior.
Keywords: Chemotherapy, Patient safety, Medication errors, Theory of planned behavior, Patient-centered care
Abstract
Background.
Patients can make contributions to the safety of chemotherapy administration but little is known about their motivations to participate in safety-enhancing strategies. The theory of planned behavior was applied to analyze attitudes, norms, behavioral control, and chemotherapy patients' intentions to participate in medical error prevention.
Methods.
A quantitative, cross-sectional survey study among chemotherapy patients treated at the oncology/hematology department of a large regional hospital was conducted. Confirmatory factor analysis and structural equation modeling were used to investigate the relationship between patients' responses to measures of attitudes, norms, and behavioral control and their intentions.
Results.
Four hundred seventy-nine patients completed the survey (52% response rate). Attitudes, perceived behavioral control, and subjective norms explained 62% of the variance in intentions to engage in error monitoring and reporting. Perceived behavioral control (β = 0.476), norms relating to patients' relatives (β = 0.343), and instrumental attitudes (β = 0.281) were the strongest (direct) predictors of patients' intentions. Experiential attitudes had the smallest effect on intentions (β = 0.178). Subjective norms relating to expectations attributed to oncology staff had strong direct and indirect effects on patients' intentions (total effect, 0.382).
Conclusions.
Patients acknowledge the benefit of error monitoring and reporting and anticipate positive outcomes of involvement, but their valuations of the process of engaging in error prevention are less positive. Behavioral control and perceptions of staff approval are central for patients. Involvement of cancer patients in safety requires oncologists to address their patients' normative and control beliefs through education and proactive approval of patient engagement.
Introduction
Medical errors are a serious threat to cancer patients [1]. Gandhi et al. [2] investigated medication errors in outpatient chemotherapy in adult and pediatric ambulatory infusion units. Four percent of all chemotherapy orders in adults and 1% of chemotherapy orders in children involved errors. Walsh et al. [3] observed a medication error rate of 8.2 per 1,000 medication orders among adult cancer patients in the outpatient setting. Five medication errors per 1,000 orders had the potential to cause harm and one error per 1,000 orders resulted in injury. Research and clinical experience suggest that patients can be a valuable resource in ensuring safe care, and several cancer centers in the U.S. and Europe now try to engage cancer patients as “vigilant partners” [4–7]. For example, Weingart et al. [8] report on the “You CAN” campaign, a teamwork training program for cancer patients and their families in ambulatory oncology. At the heart of any error prevention strategy involving chemotherapy patients is that patients attentively monitor care procedures, for example, drug administration, and notify care providers if they observe any potential errors or deviations from routines. However, evidence regarding the conditions under which patients are able and willing to engage in their safety and thus the effectiveness of these approaches is still limited. It is not an uncommon experience for oncology nurses to find out retrospectively that patients were aware of errors or deviations from standards but did not communicate their observations because of a variety of reasons [9]. Prior research suggests that chemotherapy patients themselves acknowledge the importance of being proactive, asking questions, and communicating observations that may signal error [10]. In in-depth interviews, patients unequivocally agreed that patients can make contributions to safety, and many participants were prepared to get involved. However, patients also recognized their limited capabilities for error detection, that is, medical knowledge. The central importance patients attach to instruction by nurses regarding error prevention indicates that perceived social norms may be a main contributor to patient engagement. A clear understanding of the factors that determine patients' safety-related behaviors is crucial to facilitate patients' active involvement in safety and for the design of effective interventions that support patients and care providers in ensuring safe care.
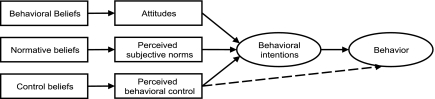
Participation in error prevention strategies can be seen as a complex case of health-promoting behavior. Thus, the theory of planned behavior (TPB) provides a useful conceptual model to explain and predict patients' behavioral intentions to engage in their safety. Transferred to the behavior of interest, namely, “monitoring care procedures and notifying staff of any potential errors,” the TPB would predict that positive emotive beliefs regarding the target behavior and a high subjective probability that the behavior positively affects safety, that is, patient preventability, are central for attitudes toward error monitoring and reporting. If patients hold normative beliefs that significant others expect them to engage in error prevention and share a high motivation to comply with these expectations, this would positively affect subjective norms and thereby intentions to participate. Finally, patients' perceptions of the presence of factors that facilitate or impede monitoring and communicating errors to staff, for example, knowledge, together with the subjective power of these factors, determine patients' self-perceived abilities to “speak up.” Attitudes, subjective norms, and perceived behavioral control would predict patients' intentions to watch for and communicate errors, and intentions would predict actual behavior (Fig. 1). Intentions have been shown to be predictive of actual behavior for a number of behaviors and settings, including patients' safety behaviors [11–13]. The TPB has been successfully applied to a variety of health-promoting behaviors, for example, physical activity and exercise, safer sex, adherence to diet, and self-examination behavior [14–17].
Figure 1.
Schematic model of the theory of planned behavior.
The primary aim of this study was to examine and empirically test the relationships between attitudes, norms, and behavioral control and chemotherapy patients' intentions to participate in error prevention. We hypothesized that perceived social norms relating to staff would play a salient role in predicting the target behavior. Chemotherapy patients often experience long and intense relations with the same medical staff, and the target behavior itself, that is, error reporting, is embedded in a complex social environment. Perceived approval of error prevention behavior by staff is likely to be of vital importance for patients because caregivers are directly affected by the target behavior. The results of the current study may have important practical implications for involving patients in error-prevention strategies.
Materials and Methods
Survey Instrument
A quantitative, cross-sectional survey study among chemotherapy patients was conducted. The development of the instrument was based on our own extensive qualitative research in chemotherapy patients and guided by the literature [7, 9, 10, 18]. We based the development of survey questions on items commonly used to assess TPB constructs and adapted them to the objective of our study. The following measures were included to assess attitudes, behavioral control, norms, and intentions.
Attitudes were measured with six items, three relating to experiential attitudes and three assessing instrumental attitudes. Experiential attitudes relate to patients' emotive beliefs and valuations of the process of engaging in error prevention whereas instrumental attitudes relate to cognitive beliefs regarding the outcomes of the behavior. Attitude items used the stem “For me, to watch for errors and notify staff of errors is …” and presented seven-point bipolar adjective response scales anchored at easy (= 7) or difficult (= 1) (ATT-E1), familiar (= 7) or unfamiliar (= 1) (ATT-E2), pleasant (= 7) or unpleasant (= 1) (ATT-E3), good (= 7) or bad (= 1) (ATT-I1), useful (= 7) or worthless (= 1) (ATT-I2), and beneficial (= 7) or harmful (= 1) (ATT-I3).
Perceived behavioral control was assessed using three items, all measured on a seven-point Likert scale ranging from completely agree (= 7) to completely disagree (= 1): “I am confident that I can watch for errors and notify staff of errors” (PBC1), “I am sure I could watch for errors and notify staff of errors if I want to” (PBC2), and “Whether I watch for errors and notify staff of errors or not is entirely up to me” (PBC3).
Subjective norms were assessed with four items, all measured on a seven-point Likert scale ranging from completely agree (= 7) to completely disagree (= 1): “People who are important to me (e.g., family) expect me to watch for errors and notify staff of errors” (N1), “People who are important to me (e.g., family) would approve of my watching for errors and notifying staff of errors” (N2), “Nurses expect me to watch for errors and notify staff of errors” (N3), and “Doctors expect me to watch for errors and notify staff of errors” (N4).
Intentions were assessed with three items, all measured on a seven-point Likert scale ranging from completely agree (= 7) to completely disagree (= 1): “Next time I go to hospital I will watch for errors and notify staff of errors” (INT1), “I intend to watch for errors and notify staff of errors next time I go to hospital” (INT2), and “Next time I go to hospital, I want to watch for errors and notify staff of errors” (INT3).
These measures were assessed within a larger survey study relating to patients' perceptions of chemotherapy safety. The term “error” was introduced at the beginning: “Errors in care can occur and manifest in multiple ways. For example, a drug can be omitted by mistake or the wrong dose can be administered. Not all errors cause harm though, for example, because they are identified and intercepted before reaching the patient.” Patients were also presented short vignettes of typical errors to make them more familiar with the variety of errors that can occur. The survey was pretested for acceptability and comprehension in 15 patients.
Sample
Patients treated at the oncology/hematology department, including the ambulatory infusion unit, of a large regional hospital in Switzerland were recruited for participation in the study. There were few inclusion criteria, namely, age >18 years, treatment with antineoplastic drugs, ability to understand German, and no information on death stored. Medical records of patients were screened for these criteria. Identified patients received the survey together with a cover letter asking for informed consent and a prepaid envelope. Forms were returned to the Swiss Patient Safety Foundation. Return of the survey was regarded as informed consent. A reminder and a copy of the survey instrument were sent 4 weeks later. No material incentives were offered for participation. Age, gender, insurance, and cancer diagnosis were extracted from medical records. The research protocol was approved by the local Ethics Committee (ref. 2008/035).
Data Analysis
Our analytical approach followed the recommended two-step procedure for structural equation modeling [19]. First, we conducted a confirmatory factor analysis (CFA) to test the measurement model and verify convergent and discriminant validity. CFA models the relations between observed variables (scores on the measurement instrument) and the underlying unobserved latent variables (e.g., TPB constructs) [20]. The modification indices and the standardized residual covariances were examined to evaluate model fit and misspecification of the measurement model and to guide model modification. In a second step, structural equation modeling (SEM) was used to define and test the hypothesized relations between the latent variables. CFA and SEM were conducted using AMOS 17 [21]. Internal consistency of the scales was assessed using Cronbach's α coefficient. Model fit was assessed using the following fit statistics: goodness-of-fit index (GFI) and adjusted goodness-of-fit index (AGFI) >0.90 as measures of absolute fit, comparative fit index (CFI) and Tucker-Lewis index (TLI) with values close to 0.95 as measures of comparative (incremental) fit, root mean square error approximation (RSMEA) <0.06 as a parsimony adjusted measure of fit, and standardized root mean square residual (SRMR) <0.08 as measure of absolute “badness-of-fit” were accepted as a “good fit” [22]. All returned surveys were screened for incomplete data. Cases with >10% missing items were excluded from analysis. Missing values in the remaining sample were imputed using full information maximum likelihood (FIML). Tests were two-sided and a p-value < .05 was considered significant.
Results
Descriptives
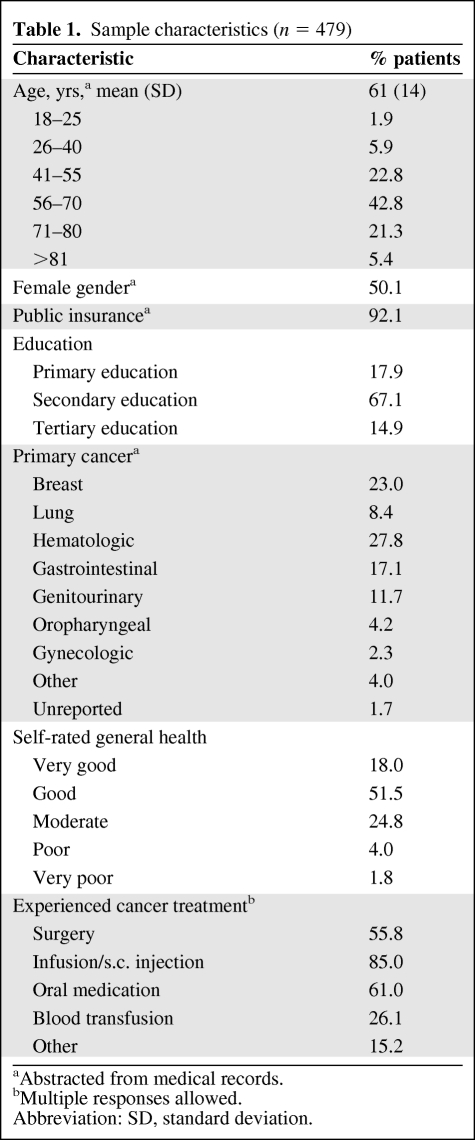
Nine hundred twenty-three patients were included in the study, of whom 479 returned the completed survey (52% response rate). Table 1 reports respondents' characteristics. There were no significant differences between responders and nonresponders in terms of mean age (61.2 years versus 60.9 years; p = .7920) and gender (50.1% female versus 45.3% female; p = .142). However, compared with nonresponders, patients who completed the survey were more likely to have private insurance (7.9% versus 4.1%; p = .014). Breast cancer (23.0% versus 16.4%; p = .01) and hematologic cancers (27.8% versus 17.1%; p < .001) were more frequent whereas lung cancer (8.4% versus 16.7%; p < .001) and genitourinary cancers (11.7% versus 17.6%; p = .011) were less frequent among responders than nonresponders. Five surveys were dropped from further analysis because of excessive missing data, leaving a sample of n = 474 for the CFA and SEM.
Table 1.
Sample characteristics (n = 479)
aAbstracted from medical records.
bMultiple responses allowed.
Abbreviation: SD, standard deviation.
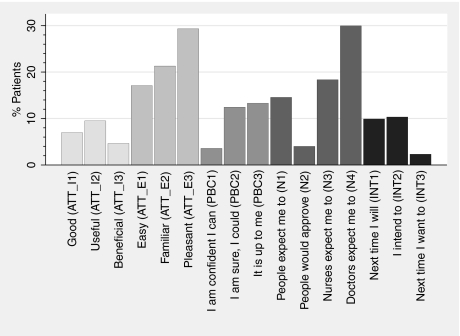
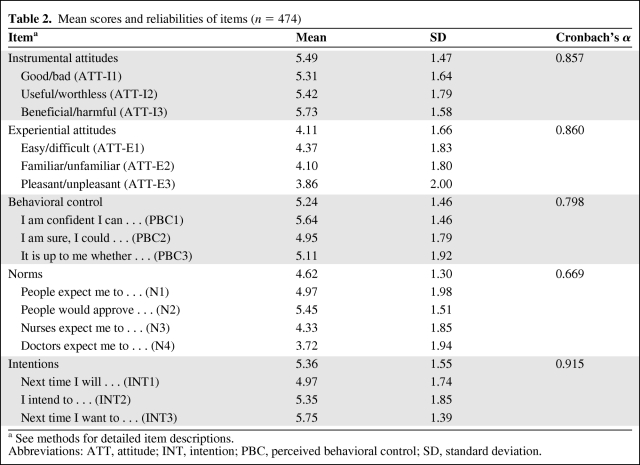
The majority of patients reported positive attitudes toward error monitoring and reporting, though a considerable fraction disagreed with positive item descriptors (5%–9% for instrumental and 17%–29% for experiential attitudes). For the PBC items, 3%–13% disagreed on having control over their error prevention behaviors and 2%–10% rejected intentions to engage in safety. Thirty percent of responders disagreed strongly that doctors expected them to watch for and report errors, whereas 18% attributed this to nurses. Figure 2 presents the fractions of patients who reported disagreement with items. Differences in patients' responses to the items of the five theoretical constructs are consistent with a priori expectations (Table 2). The mean response to instrumental attitude items was significantly higher than the mean score on experiential attitude items (5.49 versus 4.11; p < .001), indicating that patients valued the outcome expectations of error monitoring and reporting more positively than the process of performing this behavior. Perceived subjective norms associated with patients' private environment (Norms 1 and 2) were significantly higher than expectations attributed to hospital staff (Norms 3 and 4) (mean, 5.21 versus 4.02; p < .001). Norms relating to oncology nurses (Norm 3) were stronger than expectations attributed to doctors (Norm 4) (mean, 4.33 versus 3.72; p < .001). Cronbach's α indicated satisfactory internal consistency of the TPB scales, with the only exception being the Norms scale (Table 2).
Figure 2.
Fraction of patients who disagreed with theory of planned behavior items. The two bottom adjacent response categories are merged. See methods for detailed item descriptions.
Abbreviations: ATT, attitude; INT, intention; N, norm; PBC, perceived behavioral control.
Table 2.
Mean scores and reliabilities of items (n = 474)
aSee methods for detailed item descriptions.
Abbreviations: ATT, attitude; INT, intention; PBC, perceived behavioral control; SD, standard deviation.
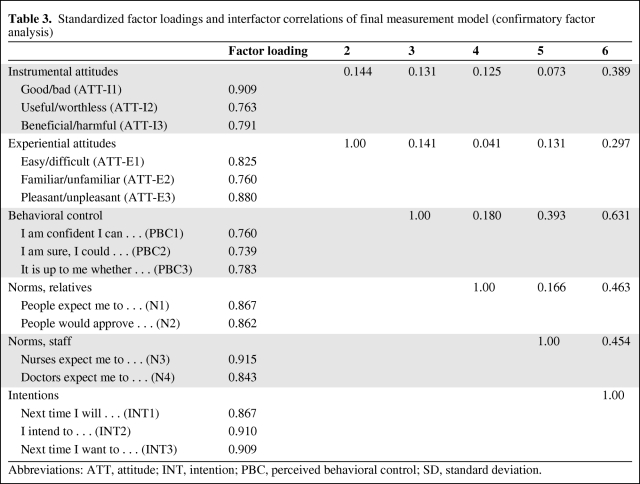
CFA
A TPB measurement model with the five factors experiential attitudes, instrumental attitudes, perceived behavioral control, norms, and intentions was estimated initially and evaluated for misspecification. Inspection of the modification indices and standardized residuals obtained by the confirmatory factory analysis of this model indicated local areas of poor fit associated with the subjective norms indicators. The model was revised to include two latent subjective norm variables (one related to hospital staff [NORM-staff] and one reflecting patients' relatives [NORM-relatives]), each measured by two items (Cronbach's α NORM-staff, 0.870; Cronbach's α NORM-relatives, 0.838). Table 3 presents the factor loadings of the latent constructs and interfactor correlations of the revised model. Standardized factor loadings were generally large (>0.7) and all were statistically significant (p < .001). The strongest relations were observed for perceived behavioral control and intentions, and norms and intentions. The goodness-of-fit indices suggest that the revised six-factor model fit the data well: χ2 (89, n = 474) = 95.7, p = .295; GFI = 0.976; AGFI = 0.964; CFI = 0.99; TLI = 0.99; RSMEA = 0.013; SRMR = 0.0196.
Table 3.
Standardized factor loadings and interfactor correlations of final measurement model (confirmatory factor analysis)
Abbreviations: ATT, attitude; INT, intention; PBC, perceived behavioral control; SD, standard deviation.
Structural Equation Model
Based on the final measurement model, a structural model was tested. In addition to the direct paths from attitudes, norms, and perceived behavioral control to intentions hypothesized by the TPB, we also found a significant path from norms relating to staff to perceived behavioral control. The final model accounted for 62% of the variance in patients' intentions. The overall fit of the model was good with χ 2 (96, n = 474) = 119.05, p = 0.056; GFI = 0.971; AGFI = 0.958; CFI = 0.99; TLI = 0.99; RSMEA = 0.023; SRMR = 0.0575. All paths are significant at the .001 level. Significant covariances were identified between the two norm constructs (covariance, 0.464; correlation, 0.169; p = .002) and the two attitude constructs (covariance, 0.272; correlation, 0.145; p = .006). presents the final model together with standardized parameters. Intentions were most strongly (directly) influenced by perceived behavioral control (β = 0.476), norms relating to relatives (β = 0.343), and instrumental attitudes (β = 0.281). Experiential attitudes had the smallest effect on intentions (β = 0.178). Norms relating to hospital staff explained 16% of the variance in perceived behavioral control. Thus, the total effect of these norms on intentions is substantial and exceeds that of norms attributed to patients' “personal environment” (standardized direct effect, 0.194; indirect effect, 0.395 × 0.476 = 0.188; total effect, 0.382).
Figure 3.
Results of structural equation modeling. Effects of norms, attitudes, and perceived behavioral control on patients' intentions to notify staff of errors. Observed manifest variables (survey items) are presented as rectangles. Latent variables are presented as ellipses. Error and residual terms are omitted from display. Standardized estimates are presented. p-values for all paths' coefficients were <.001.
Abbreviations: ATT, attitude; INT, intention; PBC, perceived behavioral control.
Discussion
This research investigated cancer patients' motivation to contribute to drug administration safety. Our study confirms the TPB as a conceptual framework in predicting chemotherapy patients' behavioral intentions to engage in medical error prevention. Perceived behavioral control, norms, and attitudes explained a large fraction of variance in intentions. As in other studies, behavioral control, that is, trust in one's own ability, was the major predictor of intending to monitor treatment safety [11]. In a recent study, self-efficacy in preventing errors, a concept closely related to behavioral control, was strongly associated with the reported likelihood of taking preventive actions [23]. Patients with high self-efficacy were more likely to engage in newer and unfamiliar actions, in particular. Luszczynska and Gunson reported behavioral control as the strongest predictor of patients' intentions to ask staff to wash their hands [13]. With respect to the target behavior in our study, behavioral control has several core dimensions that are likely to influence performance. These are, most importantly, interacting and communicating with staff about difficult issues, vigilance and reaction capabilities limited by disease and treatment, and (medical) knowledge. It is worth noting that these dimensions, for example, interacting with staff, are not, per se, important for behavioral control. Rather, behavioral control reflects patients' beliefs that a factor may facilitate or impede their error prevention activity and the perceived strength of this factor. If patients hold the belief that interaction with staff is needed for error prevention together with the perception that their potential to interact is limited because of internal or external barriers, that decreases patients' feelings of controllability and, as our results show, intentions to engage.
Our findings highlight the important role of perceptions of others' approval in predicting intentions to engage in safety, that is, subjective norms. Patients who perceive strong expectations to report errors and thus feel potential to gain approval or suffer sanctions have stronger intentions to act. The CFA also revealed that norms attributed to the “hospital environment” and norms attributed to the “private environment” reflect two distinct factors that are both important for cancer patients. Error monitoring and reporting expectations attributed to staff were significantly lower, but more influential for intentions than for expectations attributed to patients' relatives. Our previous research revealed that many chemotherapy patients have a strong motivation to comply with staff expectations [10]. In a recent survey study, patients shared affirmative attitudes about engaging in a variety of concrete safety-related behaviors, under the condition that staff would instruct them to [24]. Despite its informative and educative character, instruction by staff also symbolizes approval for patients' engagement in error prevention and can be perceived as signaling social norms. Research into oncology nurses' practices to get patients involved in safety indeed confirms that nurses intuitively choose among a set of strategies and patterns of language and switch between participative and authoritative models of education, involving different “colorings” of expectations and norms [9]. Although our findings clearly emphasize the role of perceived norms, we do not know whether expectations attributed to staff relax barriers for safety engagement, such as decreasing fears to confront staff with errors, or increasing barriers not to engage and social pressure to comply. However, the result that norms attributed to staff also indirectly affect intentions through perceived behavioral control suggests the former relation. In our study, norms attributed to staff explained about 16% of the variance in perceived behavioral control. Thus, perceived staff approval of error prevention seems to reduce social barriers, and as a consequence positively renders patients' trust in their own ability to engage in the behavior.
This study has some limitations that should be considered when interpreting its results. First, we sampled only patients from one hospital, and the generalizability of our findings is thus unclear. Second, the achieved response rate is unsatisfactory, and we cannot rule out bias from selective nonresponse. Although there were no differences between responders and nonresponders in terms of age and gender, certain types of cancer were underrepresented among responders. Unfortunately, the data available for nonparticipants are very limited. For example, we do not know whether participants and nonparticipants differed in terms of their educational and socioeconomic backgrounds. Further, we did not assess participants' income and social and economic living conditions, and did not model the influence of education on patients' responses. Education and socioeconomic background may play a major role in the ability and willingness to engage for one's own safety [24]. Finally, the main outcome measures in our model were patients' intentions rather than actual behaviors. Although the predictive value of intentions has been confirmed for many health-related behaviors, the strength of this link for safety-related activities is unclear. We thus do not know whether patients who intended to would in fact engage in error monitoring and whether changing intentions through interventions will impact changes in behavior. Webb and Sheeran concluded, from a meta-analysis of studies of intention–behavior relations, that a medium-to-large change in intention leads to a small-to-medium change in behavior. The impact of intentions on behavior is smaller for behaviors that are performed in “social context” and when there is potential for social reaction, which is certainly the case for patients' error prevention behaviors [25]. Thus, future research is needed regarding the predictive power of intentions for safety-related behaviors in socially complex environments.
Despite these limitations, the results have important implications for clinical practice and involvement of patients in error prevention. As indicated by the high scores on the instrumental attitude items, patients in our study acknowledged the utility of error monitoring and reporting and anticipated positive outcomes of involvement in safety. This is a fundamental precondition for any approaches to encourage patients. However, patients' valuations of the process of engaging in error prevention activities (experiential attitudes) were less positive. In particular, many patients felt that this process was “unfamiliar” and “unpleasant.” Future research should investigate the acceptability and comfort of different modes of communicating potential errors to providers. For example, recent studies suggest that tools for indirect communication, such as patient reminder materials [26] or electronic reporting [27], are used by patients and are perceived as helpful. Routine integration of error reporting requests in patient–provider communication during chemotherapy visits is also likely to make discussion of safety issues more familiar and pleasant for patients.
Patients themselves perceive involvement in safety issues as a learning process in which knowledge and confidence in their abilities rise with additional experiences of chemotherapy administration [10]. There are a number of ways that clinicians can support and foster this process, most profoundly by teaching what is being done and why, and by formulating simple rules of correct processes. Trust in one's own ability to identify errors is of particular importance to patients as they seek to avoid falsely attributing error and triggering additional burden for staff associated with workup of events. Clinicians thus need to address these concerns and reduce barriers by communicating that even reports of potential errors that turn out to be a “false alarm” are appreciated. Behavioral control can also be improved by providing role models of other patients who engage in error prevention. Patients report that watching other patients asking staff to wash their hands would encourage them to perform the same behavior [28, 29]. This could be accomplished by patient education material presenting other patients' reports, or by former patients serving as patient safety champions and educating other patients about error prevention [30]. However, attention should also be paid to unintended “learning effects.” Clinical staff need to be aware that nonconstructive reactions to intervening patients may not only affect involved individuals and impede the likelihood of future error preventing activities but can also render other patients' perceptions of norms and control beliefs. In particular, if care is provided at large infusion units where patients can follow staff responses to other patients' safety-related activities, adequate interaction is vital.
Engaging patients in safety is embedded in a complex professional and institutional environment and addresses the larger context of a culture of safety. Only if professionals collaborate for safety, and receive institutional and leadership support for safety, will they be able to encourage patients to engage and promote safety toward patients. There is scarce evidence on doctors' and nurses' attitudes toward involvement of patients and the relationship of these to patients' participation in safety. A recent survey among nurses about an intervention to involve patients in the prevention of adverse drug events reported positive attitudes and experiences of nurse participants [31]. Our own research suggests that nurses claim that involvement of patients needs continuous, joint, and honest efforts and must be embedded in the institution's safety culture [9]. In that qualitative study, oncology nurses argued that instruction of patients should start at the consultation with doctors and “doctors need to signal that there is room for questioning staff, that this is wanted and acknowledged.” Surprisingly, informal discussions with doctors at the same institution revealed that oncologists had little self-confidence that their instructions may have considerable impact on patients' safety behaviors. The effect of perceived subjective norms on intentions to engage in error prevention was substantial in our study. However, a considerable fraction of patients strongly disagreed that doctors, and to a lesser extent nurses, expect them to engage in error prevention. Clinicians need to be aware that their unambiguous and proactive approval may be a central force in involving their patients in safety.
Conclusion
Attitudes, behavioral control, and subjective norms explain a large portion of patients' intentions to engage in error prevention. Patients acknowledge the utility of error monitoring and reporting and anticipate positive outcomes of involvement, but their valuations of the process of engaging in error prevention are less positive. Behavioral control and perceptions of staff approval are central for patients. Involvement of cancer patients in safety requires oncologists to address their patients' normative and control beliefs through education and proactive approval of patient engagement.
Acknowledgments
We gratefully thank the patients who participated in this study and shared their experiences with us. We also thank Beatrice Brinkers, Paola Ceccarelli (both Klinische Forschung Aargau AG), and Tanja Forcellini for their continuous support in survey administration and logistics, data management, and study organization.
Financial support for this study was provided by a research grant from Oncosuisse (OCS – 02109–08-2007). The funding source had no influence on study design; in the collection, analysis, and interpretation of the data; in the writing of the manuscript; or in the decision to submit the manuscript for publication. The views expressed and any errors are the sole responsibility of the authors.
Author Contributions
Conception/Design: David L.B. Schwappach, Martin Wernli
Provision of study material or patients: David L.B. Schwappach, Martin Wernli
Collection and/or assembly of data: David L.B. Schwappach, Martin Wernli
Data analysis and interpretation: David L.B. Schwappach, Martin Wernli
Manuscript writing: David L.B. Schwappach, Martin Wernli
Final approval of manuscript: David L.B. Schwappach, Martin Wernli
References
- 1.Schulmeister L. Preventing chemotherapy errors. The Oncologist. 2006;11:463–468. doi: 10.1634/theoncologist.11-5-463. [DOI] [PubMed] [Google Scholar]
- 2.Gandhi TK, Bartel SB, Shulman LN, et al. Medication safety in the ambulatory chemotherapy setting. Cancer. 2005;104:2477–2483. doi: 10.1002/cncr.21442. [DOI] [PubMed] [Google Scholar]
- 3.Walsh KE, Dodd KS, Seetharaman K, et al. Medication errors among adults and children with cancer in the outpatient setting. J Clin Oncol. 2009;27:891–896. doi: 10.1200/JCO.2008.18.6072. [DOI] [PubMed] [Google Scholar]
- 4.Weingart SN, Price J, Duncombe D, et al. Patient-reported safety and quality of care in outpatient oncology. Jt Comm J Qual Patient Saf. 2007;33:83–94. doi: 10.1016/s1553-7250(07)33010-9. [DOI] [PubMed] [Google Scholar]
- 5.Unruh KT, Pratt W. Patients as actors: The patient's role in detecting, preventing, and recovering from medical errors. Int J Med Inform. 2006;76(suppl 1):S236–S244. doi: 10.1016/j.ijmedinf.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein JB. E-prescribing first step to improved safety. J Natl Cancer Inst. 2006;98:1763–1765. doi: 10.1093/jnci/djj519. [DOI] [PubMed] [Google Scholar]
- 7.Schwappach DL, Wernli M. Medication errors in chemotherapy: Incidence, types and involvement of patients in prevention. A review of the literature. Eur J Cancer Care (Engl) 2010;19:285–292. doi: 10.1111/j.1365-2354.2009.01127.x. [DOI] [PubMed] [Google Scholar]
- 8.Weingart SN, Simchowitz B, Eng TK, et al. The You CAN campaign: Teamwork training for patients and families in ambulatory oncology. Jt Comm J Qual Patient Saf. 2009;35:63–71. doi: 10.1016/s1553-7250(09)35009-6. [DOI] [PubMed] [Google Scholar]
- 9.Schwappach DL, Hochreutener MA, Wernli M. Oncology nurses' perceptions about involving patients in the prevention of chemotherapy administration errors. Oncol Nurs Forum. 2010;37:E84–E91. doi: 10.1188/10.ONF.E84-E91. [DOI] [PubMed] [Google Scholar]
- 10.Schwappach DL, Wernli M. Am I (un)safe here? Chemotherapy patients' perspectives towards engaging in their safety. Qual Saf Health Care 2010 Apr [Epub ahead of print] doi: 10.1136/qshc.2009.033118. [DOI] [PubMed] [Google Scholar]
- 11.Godin G, Kok G. The theory of planned behavior: A review of its applications to health-related behaviors. Am J Health Promot. 1996;11:87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- 12.Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: A meta-analytic review. Br J Soc Psychol. 2001;40:471–499. doi: 10.1348/014466601164939. [DOI] [PubMed] [Google Scholar]
- 13.Luszczynska A, Gunson KS. Predictors of asking medical personnel about handwashing: The moderating role of patients' age and MRSA infection status. Patient Educ Couns. 2007;68:79–85. doi: 10.1016/j.pec.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 14.McGilligan C, McClenahan C, Adamson G. Attitudes and intentions to performing testicular self-examination: Utilizing an extended theory of planned behavior. J Adolesc Health. 2009;44:404–406. doi: 10.1016/j.jadohealth.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Blanchard CM, Fisher J, Sparling PB, et al. Understanding adherence to 5 servings of fruits and vegetables per day: A theory of planned behavior perspective. J Nutr Educ Behav. 2009;41:3–10. doi: 10.1016/j.jneb.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mausbach BT, Semple SJ, Strathdee SA, et al. Predictors of safer sex intentions and protected sex among heterosexual HIV-negative methamphetamine users: An expanded model of the theory of planned behavior. AIDS Care. 2009;21:17–24. doi: 10.1080/09540120802017628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajzen I, Manstead ASR. Changing health-related behaviors: An approach based on the theory of planned behavior. In: van den Bos K, Hewstone M, de Wit J, et al., editors. The Scope of Social Psychology: Theory and Applications. New York: Psychology Press; 2007. pp. 43–63. [Google Scholar]
- 18.Schwappach DL. Review: Engaging patients as vigilant partners in safety: A systematic review. Med Care Res Rev. 2010;67:119–148. doi: 10.1177/1077558709342254. [DOI] [PubMed] [Google Scholar]
- 19.Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychol Bull. 1988;103:411–423. [Google Scholar]
- 20.Byrne BM. Structural Equation Modeling With AMOS. New York: Taylor & Francis; 2001. pp. 3–14. [Google Scholar]
- 21.Arbuckle J. AMOS 17.0 User's Guide. Chicago: SPSS Inc. 2008:1–602. [Google Scholar]
- 22.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 23.Hibbard JH, Peters E, Slovic P, et al. Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Rev. 2005;62:601–616. doi: 10.1177/1077558705279313. [DOI] [PubMed] [Google Scholar]
- 24.Davis RE, Koutantji M, Vincent CA. How willing are patients to question healthcare staff on issues related to the quality and safety of their healthcare? An exploratory study. Qual Saf Health Care. 2008;17:90–96. doi: 10.1136/qshc.2007.023754. [DOI] [PubMed] [Google Scholar]
- 25.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132:249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 26.McGuckin M, Waterman R, Porten L, et al. Patient education model for increasing handwashing compliance. Am J Infect Control. 1999;27:309–314. doi: 10.1016/s0196-6553(99)70049-0. [DOI] [PubMed] [Google Scholar]
- 27.Basch E, Artz D, Iasonos A, et al. Evaluation of an online platform for cancer patient self-reporting of chemotherapy toxicities. J Am Med Inform Assoc. 2007;14:264–268. doi: 10.1197/jamia.M2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duncanson V, Pearson LS. A study of the factors affecting the likelihood of patients participating in a campaign to improve staff hand hygiene. Br J Infect Control. 2005;6:26–30. [Google Scholar]
- 29.Duncan C. An exploratory study of patient's feelings about asking healthcare professionals to wash their hands. J Ren Care. 2007;33:30–34. doi: 10.1111/j.1755-6686.2007.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 30.Kovacs BK. Canadian patient safety champions: Collaborating on improving patient safety. Healthc Q. 2008;11:95–100. doi: 10.12927/hcq.2008.19657. [DOI] [PubMed] [Google Scholar]
- 31.Weingart SN, Toth M, Eneman J, et al. Lessons from a patient partnership intervention to prevent adverse drug events. Int J Qual Health Care. 2004;16:499–507. doi: 10.1093/intqhc/mzh083. [DOI] [PubMed] [Google Scholar]