Cancer-related disparities in the Appalachian region of the U.S. are described as an example of the disparities experienced by underserved predominantly white, rural populations. Appalachia Community Cancer Network activities designed to intervene on these disparities are presented.
Keywords: Disparities, Appalachia, Cancer
Abstract
There are meaningful cancer-related disparities in the Appalachian region of the U.S. To address these disparities, the Appalachia Community Cancer Network (ACCN), a collaboration of investigators and community partners in five states (Kentucky, Ohio, Pennsylvania, Virginia, and West Virginia), is involved in increasing cancer education and awareness, conducting community-based participatory research (CBPR), and creating mentorship and training opportunities. The primary objective of this paper is to describe cancer-related disparities in the Appalachian region of the U.S. as an example of the disparities experienced by underserved, predominantly white, rural populations, and to describe ACCN activities designed to intervene regarding these disparities. An ACCN overview/history and the diverse activities of ACCN-participating states are presented in an effort to suggest potential useful strategies for working to reduce health-related disparities in underserved white populations. Strengths that have emerged from the ACCN approach (e.g., innovative collaborations, long-standing established networks) and remaining challenges (e.g., difficulties with continually changing communities, scarce resources) are described. Important recommendations that have emerged from the ACCN are also presented, including the value of allowing communities to lead CBPR efforts. Characteristics of the community-based work of the ACCN provide a framework for reducing health-related disparities in Appalachia and in other underserved white and rural populations.
Introduction
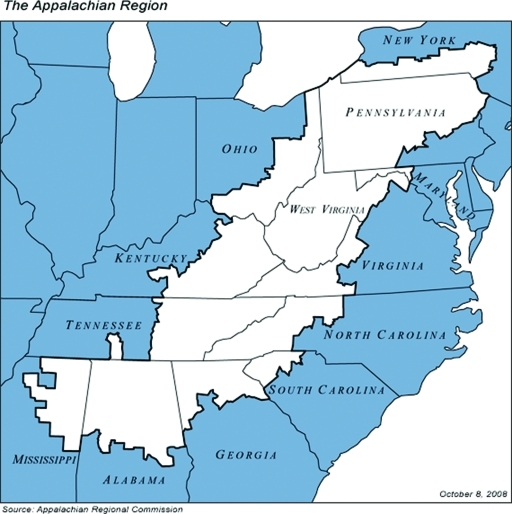
The Appalachian region of the U.S. is a federally designated 205,000 square mile region that contains 420 counties in 13 states ranging along the spine of the Appalachian Mountains from New York to Mississippi (Fig. 1). Approximately 24 million people reside in Appalachia [1] and about 42% of the region is rural [1]. Appalachia is less racially heterogeneous than the U.S. (Throughout this article, we use the term “white population” to characterize the predominant racial group in the Appalachian region. However, we acknowledge that the region is not racially homogenous. From 1990 to 2000, the percentage of minority Appalachians increased nearly 50%, amounting to 22.9 million, or 12% [2]. The central Appalachian states—those involved in the Appalachia Community Cancer Network (ACCN)—have the fewest nonwhites in Appalachia, approximately 4% or 92,000 of 2.2 million.) A relatively small proportion, about 12%, of the Appalachian population is nonwhite or Hispanic [1]. Most members of racial and ethnic minority groups residing in Appalachia live in southern Appalachia (19%), compared with 7% in northern Appalachia and 4% in central Appalachia [1]. The economy of Appalachia has diversified over the past two decades from greater reliance on a few major industries involving manufacturing into areas of government, retail, service, and tourism [1]. The Appalachian Regional Commission (ARC) considers 162 of the 420 (38.6%) Appalachia counties to be at risk or economically distressed [1]. Many additional characteristics of Appalachia affect the health of its residents and, specifically, their health as related to cancer risk, screening, treatment, and survival. Among these factors are: a greater proportion reporting no health insurance or being underinsured, greater geographic isolation, less public transportation, and fewer physicians, clinics, hospitals, and cancer centers per capita [3–9].
Figure 1.
The Appalachian region of the U.S.
This report provides information about cancer-related disparities in the Appalachian region of the U.S., as well as activities occurring in this region to address these disparities, to exemplify the experience of an underserved, largely white and rural population. Cancer-related disparities and associated activities of the ACCN were used to delineate the disparities experienced by underserved white populations, and to suggest useful strategies to improve the health of this group.
Methods
History of Appalachia
There is a distinguishable Appalachian mountain culture, and “place” is a prominent feature in that culture [10]. The historical development of Appalachia is rooted in oppression. Early settlers from England, Scotland, Ireland, and other western European countries came to the area in search of a new life. These resilient individuals sought religious freedom, ownership of land, relief from poverty, solitude, and independence. With the development of industrialization, Appalachia became characterized by control of its land and resources by large absentee companies. Settlers who had worked hard to own land fell victim to the promise of new jobs and a better economy. Instead, the ensuing growth of the coal, timber, textile, and steel industries fostered the development of chronic poverty, intimidation, and an oppressive class system. Residents of Appalachia have generally been described as responding to the adverse events of their environment by retreating, taking pride in never leaving their home or sense of “place,” maintaining a distinct dialect and colloquialisms, being hostile to outsiders, and resisting change [11]. Although these behaviors are seen as negative stereotypes, they often disguise the true strengths of the people. Appalachians tend to be resilient and action oriented; they often are community and family centered.
A common thread is woven into the fabric of being Appalachian by an overall shared system of values. These values include individualism, religion, neighborliness and hospitality, family solidarity, personalism, love of place, modesty and being oneself, sense of beauty, sense of humor, and patriotism [12]. When the history, values, and culture of Appalachia are understood and honored, it allows for the development, testing, and implementation of successful programs to reduce cancer-related disparities.
Cancer-Related Disparities in Appalachia
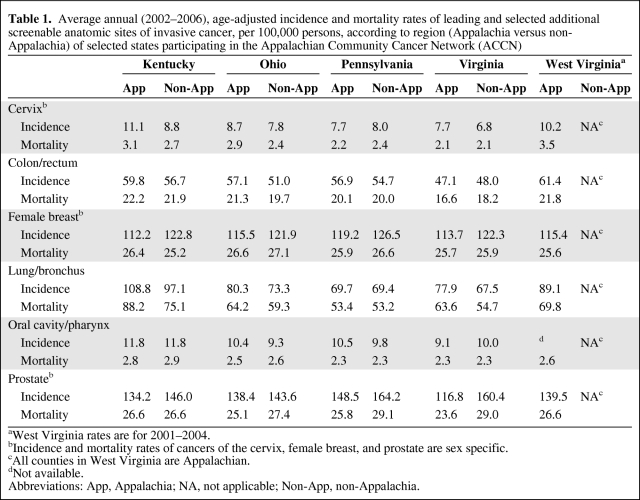
There are relatively consistent findings supporting the fact that the incidence and mortality rates for many cancers are greater in the Appalachian region than for the rest of the U.S. [13–26]. These disparities are most apparent in the central Appalachian region [26] and are strongest for cancers of the cervix, colon/rectum, and lung/bronchus. A recent report by the ACCN, summarized in Table 1, showed that the incidence and mortality rates for these same cancers were greater in the majority of the states' Appalachian areas than corresponding non-Appalachian areas [27] (Table 1). Socioeconomic differences and differences in population density may at least partially explain these disparities in cancer incidence and mortality [22, 28].
Table 1.
Average annual (2002–2006), age-adjusted incidence and mortality rates of leading and selected additional screenable anatomic sites of invasive cancer, per 100,000 persons, according to region (Appalachia versus non-Appalachia) of selected states participating in the Appalachian Community Cancer Network (ACCN)
aWest Virginia rates are for 2001–2004.
bIncidence and mortality rates of cancers of the cervix, female breast, and prostate are sex specific.
cAll counties in West Virginia are Appalachian.
dNot available.
Abbreviations: App, Appalachia; NA, not applicable; Non-App, non-Appalachia.
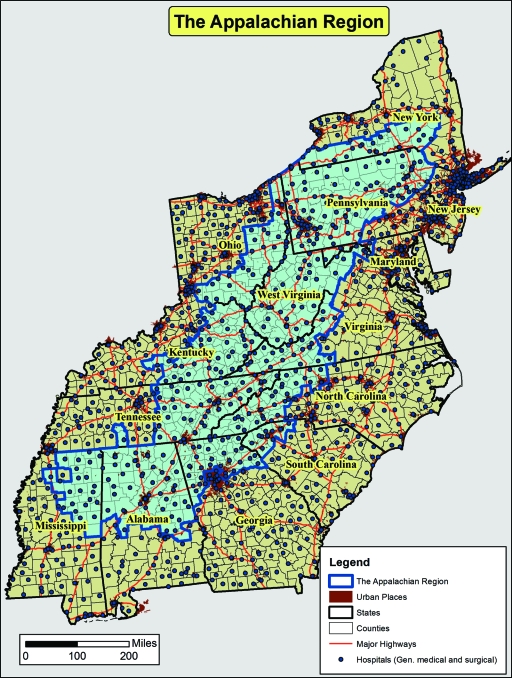
Disparities in stage at diagnosis of cancer have not been thoroughly evaluated in Appalachian areas. Limited research suggests that differences among the proportion of individuals in the Appalachian region diagnosed at a late stage with leading (lung and bronchus, colorectal, female breast, prostate) or additional screenable (cervical, oral cavity, and pharynx) cancers were not substantial; however, incidence rates for unknown stage cancer were elevated in rural Appalachian Pennsylvania, West Virginia, and Kentucky, suggesting a lack of access to cancer health care [20]. Disparities in the proportions of cancers that are reported as unknown stage may be associated with the low population density and cancer registration in small hospitals that are widely dispersed throughout Appalachia (Fig. 2). There are no known reports of possible disparities in cancer survival probability among Appalachian residents; however, data from the Surveillance, Epidemiology, and End Results program show that the 5-year cancer survival probabilities are lower in Appalachian Kentucky than in non-Appalachian Kentucky for each of the leading or screenable sites of cancer, as well as for all these sites combined (64.5% in non-Appalachian Kentucky versus 57.1% in Appalachian Kentucky).
Figure 2.
Hospitals located in states containing Appalachian counties in the U.S.
Results: The ACCN Response to Cancer-Related Disparities in Appalachia
ACCN Overview
Designed to address the cancer-related disparities that plague the Appalachian region, the National Cancer Institute (NCI)-funded ACCN emphasizes community–academic partnerships in education, research, and training. The ACCN is one of 25 NCI-designated Community Network Programs in the U.S. funded by the NCI Center to Reduce Cancer Health Disparities. With headquarters at the University of Kentucky, ACCN investigators and community partners include the central Appalachian states of Kentucky, Ohio, Pennsylvania, Virginia, and West Virginia. The network focuses on the cancers of greatest burden to the Appalachian population—cervical, colorectal, and lung cancer—with an emphasis on prevention and early detection. The focal activities include cancer education and awareness activities, community-based participatory research (CBPR) projects, and mentorship and training opportunities. CBPR strategies are especially successful and appropriate in this population because CBPR efforts include the following: (a) acknowledging the community as a unit of identity; (b) building on strengths and resources within the community; (c) facilitating a collaborative, equitable partnership in all phases of research; (d) colearning and capacity building among all partners; (e) integrating and achieving a balance between knowledge generation and intervention for the mutual benefits of all partners; (f) focusing on local relevance of public health problems; (g) partnership development that involves partners in all stages of the research process; (h) disseminating results to partners and involving them in the dissemination of results; and (i) involving a long-term process and commitment to sustainability [29].
Three forerunners to the current ACCN set the stage for these activities. In 1992–2000, under the leadership of Dr. Gilbert Friedell, The Appalachia Leadership Initiative on Cancer (ALIC) helped to develop community-based coalitions to provide local capacity to enhance cancer prevention and control [30]. The ALIC set the stage for community–academic partnerships, working closely with investigators and community leaders to enhance cancer awareness and control in Appalachia. Dr. Stephen Wyatt provided leadership to the next network program, the Appalachia Cancer Network, in 2000–2005, building on ALIC's orientations and projects, including enhancing community cancer coalitions, understanding barriers to clinical trial participation, and obtaining critical community insights to increase cancer awareness among the rural, medically underserved populations of Appalachia. In 2005, Dr. Mark Dignan took the helm of the ACCN. Consistent with the aims of preceding network programs, the ACCN continued and greatly expanded community–academic partnership through outreach, education, and training. In a competitive renewal of the ACCN awarded in 2010, this fourth-generation Appalachian cancer network program added a new component of primary prevention through the implementation of a research project focusing on energy balance that will be conducted throughout the five-state ACCN region. Below is a brief description of some ACCN projects conducted in the five states.
Kentucky-Specific Projects
In addition to participating in numerous activities across the ACCN, including training for community members through Cancer Control Planet Webinars, competitions for community education grants, and training of mentees through involvement in publications and presentations, the Kentucky ACCN has conducted several specific projects. One was a pilot project to assess the feasibility of promoting cancer screening in the emergency department (ED) of a rural, Appalachian hospital. Because rural, Appalachian populations typically experience numerous barriers to obtaining cancer screening as a result of limited access to health care, the community staff at the hospital and the local Community Advisory Board felt that this was a promising approach to screening promotion. The project was implemented by placing a trained outreach worker in the ED who provided information about cancer screening to patients and families as they waited for care. Over an 18-month period, a total of 314 individuals participated in the project. In all, it was found that ED patients were very willing and interested in obtaining cancer screening, and many scheduled a screening appointment through the project patient navigator. This project demonstrated the need for and appropriateness of reaching out to underserved populations in the ED and involving them in potential interventions designed to enhance preventive health services [31].
Kentucky ACCN investigators have leveraged their experience and interaction with the ACCN sites and partners to develop new projects. These funded projects include the following: (a) Faith Moves Mountains: A CBPR Appalachian Wellness & Cancer Prevention Program (grant no., R24 MD002757; principal investigator [PI], Nancy Schoenberg). Developed in partnership with 70 faith-based institutions in rural southeastern Kentucky, this project is designed to administer, evaluate, and disseminate a tailored wellness and cancer prevention program focused on four common prevention activities (smoking cessation and cervical, breast, and colorectal cancer [CRC] screening) [32, 33]. (b) Increasing CRC Screening in Rural Kentucky (grant no., R01 CA113932; PI, Mark Dignan). This project is designed to recruit primary health care providers, conduct a baseline assessment, and implement an intervention to increase CRC screening in primary care practices and to evaluate the effectiveness of the intervention in increasing CRC screening [34]. (c) Patient Navigation for Cervical Cancer in Appalachia (grant no., R01 CA120606; PI, Mark Dignan). This is a program of community-based patient navigator intervention in partnership with local public health departments that serve rural, Appalachian counties in Kentucky with the overall goal of increasing adherence to follow-up recommendations among women with abnormal Pap test results [35].
Ohio-Specific Projects
The Ohio ACCN is made up of a well-established network of community and academic partners that conduct CBPR in Appalachia Ohio. Six community-based coalitions collaborate to address cancer-related disparities in their communities. The Ohio ACCN has established partnerships with the faith-based community, community colleges, worksites, and health and human service agencies, as well as faculty and students from the Ohio State University (OSU). Staff members who are knowledgeable about Appalachian health disparities conduct capacity-building training and provide technical support to expand and establish membership and to assess community needs and interest in CBPR. An example of this process is the CBPR initiative to address CRC screening disparities in Appalachian Ohio, implemented by Ohio ACCN partners to address a health problem identified by residents in Meigs County—high mortality rates for CRC. A community needs assessment revealed that only 29% were within screening guidelines, although 41% reported a previous doctor recommendation for such screening. Following the community needs assessment, a media campaign entitled “Get Behind Your Health!” was developed to promote CRC screening in Meigs County, which featured a local colon cancer survivor. The results of the CRC media campaign suggested that billboards, newspapers, and posters were the preferred media outlet. This approach to increase CRC screening was included in an R24 research grant funded by the National Center on Minority Health and Health Disparities to test CRC screening interventions in 12 Appalachian Ohio counties (grant no., R24 MD002785; PI, Electra D. Paskett).
The Ohio ACCN collaboration has also helped to develop numerous funded research projects conducted by investigators at OSU such as: (a) Reducing Cervical Cancer in Appalachia, to understand why high rates of cervical cancer incidence and mortality are observed in Appalachian Ohio (grant no., P50 0CA105632; PI, Electra D. Paskett); (c) Smokeless Tobacco Marketing Approaches to Ohio Appalachian Population, to examine smokeless tobacco marketing strategies to consumers in rural Appalachian Ohio (grant no., R21 CA129907; PI, Mary Ellen Wewers); (c) Examining the Effect of Provider-Delivered Intervention Among Medicaid Smokers, with the goal of developing training materials for physicians who manage Medicaid smokers residing in Appalachian Ohio to implement evidence-based treatment (grant no., R21 CA141603; PI, Amy Ferketich); (d) A Web-Based Intervention with Adolescent Smokers of Appalachian Ohio, to evaluate a Web-based, home-based contingency management program as a smoking treatment option for rural Appalachian adolescents (grand no., RC1CA144744; PI, Brady Reynolds); and (e) Tobacco Cessation Interventions with Ohio Appalachian Smokers, with the goal of examining tobacco cessation interventions among Appalachian Ohio smokers (grant no., R01 CA129771; PI, Mary Ellen Wewers).
In addition to research-related efforts, developing the capacity and ability of each of the Ohio ACCN coalitions to directly receive financial support in their community has been a priority. ACCN staff assist the coalitions to secure and maintain a nonprofit status and to develop successful grant proposals. To date, the coalitions have directly received >$294,000 in financial support from various local and state agencies to support 26 community projects.
Pennsylvania-Specific Projects
In Appalachian Pennsylvania, the ACCN is engaged in research and associated outreach that seeks to leverage community-based resources, including 12 cancer coalitions in 17 counties, to use innovative methods to reduce the cancer burden for rural residents. One example is the development of theory-based methods among rural patients and primary care providers to test the delivery of low-cost but highly sensitive and specific techniques of screening for CRC. With funding from the NCI, a multisite, practice-based, intervention study of academic detailing was conducted in 2008–2009 to increase CRC screening in primary care practices in Appalachian Pennsylvania (grant no., U01 114622; PI, William Curry). That study found that the prevalence of having been screened in the past year increased significantly from 17% to 35% during the intervention period [36]. In a second NCI-funded study, a theory-based telephone counseling intervention to overcome patient barriers to CRC screening in Appalachian Pennsylvania was developed and tested in three rural primary care practices (grant no., U01 114662; PI, Brenda C. Kluhman). That study found that there were high levels of initial uptake of fecal immunochemical test (FIT) screening and conversion to screening after telephone counseling: 72.5% completed FIT screening as recommended and 41.8% of noncompliant patients contacted for telephone counseling converted to screening after one or two counseling sessions. In addition, working with cooperative extension, rural Pennsylvania hospitals, and a network of cancer coalitions, a 12-week, supervised physical activity intervention for rural breast cancer survivors was developed and tested in six sites in western Pennsylvania (Komen Foundation of Southwest Pennsylvania; PI, Eugene J. Lengerich). Within Appalachia, Pennsylvania is a high growth area for the Hispanic population [37]. Thus, facilitators and barriers to CRC screening among rural and urban Hispanic residents were systematically assessed through a qualitative focus group study (grant no., U01 114622; PI, Oralia Garcia Dominic) [38]. Also, the ACCN in Pennsylvania is examining the patterns of cancer patient care in Appalachia (grant no., R01CA140335; PI, Roger T. Anderson, Ph.D.).
Virginia-Specific Projects
In partnership with organizations across the Commonwealth, the ACCN in Virginia promotes cancer awareness and education activities and community-based cancer planning efforts. In addition, it provides support for broad community participation in cancer prevention and intervention activities such as the gathering of cancer data, the identification of risk factors and related risk reduction factors, and technical support for CBPR. For example, in 1992, the ALIC helped establish the first cancer control and awareness coalition in Big Stone Gap, Virginia. As a result of community forums coordinated by the Virginia ACCN, Quitline (a phone referral service to local clinics for counseling or cessation medication prescriptions) added the state Cancer Plan Action Coalition (CPAC) Cancer Screening and Education Resource Guide, which includes local smoking cessation services, to their local resources database. Storytelling is recognized as a fundamental communication method in Appalachia to communicate information about health issues, including cancer. The Virginia ACCN, in partnership with Mountain Laurel Cancer Center, has supported and facilitated the dissemination of storytelling as an effective method for community-based cancer outreach, including training for all states' project staff and community partners. In addition, together with local community cancer centers and CPAC, the Virginia ACCN assisted in the coordination and evaluation of an eight-site statewide interactive video training session about cancer clinical trials.
In partnership with CPAC, and with support from the ARC and the Centers for Disease Control (via East Tennessee State University), the Virginia ACCN coordinated a year-long project in 2010–2011 that gathered data and information about cancer navigation in the Appalachian regions of Kentucky, North Carolina, Ohio, Pennsylvania, Tennessee, Virginia, and West Virginia. As part of this project, >50 navigators, health system administrators, navigation program directors, and other key stakeholders from six states attended a day and half meeting and a 1 day follow-up meeting to complete a data matrix and share information about cancer navigation in their states. The report summarizing the findings of this effort, entitled Organizational and Financial Support of Rural Cancer Care Navigation Models in Appalachia, will be available by the end of 2011. The next phase of this project includes the establishment of a regional network, identification of community models and curriculum (reviewed by a regional advisory group), and pursuit of funding for Web-based training and continuing education.
West Virginia–Specific Projects
The ACCN at West Virginia University works with six community-based coalitions and >30 other partners to address cancer-related disparities throughout the 55 counties in West Virginia. Over the past 5 years, as a result of training and technical assistance from ACCN staff, these groups secured >$289,000 to complete educational and outreach projects far beyond their county borders. Community partners in West Virginia are committed to improving access to health screening and services for their rural residents. For example, when a local screening provider ceased offering mammogram and Pap tests through the state's breast and cervical cancer screening program, the Webster County Cancer Education Project (WCCEP) stepped in to ensure that women in this remote county were able to receive this screening. In collaboration with >30 partners, the WCCEP is providing screening events that include breast and cervical cancer screening, and also a range of other health programming, such as dental and eye exams, heart health screening, and physical activity and nutrition programs. In its inaugural year, >100 women received services at free screening events. The program continues to provide educational outreach and screening to the underserved in their community.
The West Virginia ACCN has also supported the Wetzel County Cancer Coalition, a volunteer-based coalition providing education and resources, in their community for >18 years. The Coalition's current and future activities center on the need for transportation assistance for the many cancer patients in the area who must travel outside of the county for cancer treatment. Through securing minigrant funding and other advocacy efforts, the Coalition is successfully ensuring that patients are able to get to life-saving cancer treatments and health services.
Discussion
Strengths of the ACCN Approach to Addressing Cancer-Related Disparities in Appalachia
Several notable strengths characterize the ACCN partnership. First, acknowledging that community partnership and involvement can take many forms, each state approaches community partnership in different and effective ways. For example, Pennsylvania has a long history of very active cancer coalitions that provide extensive input and outreach for community education. In Kentucky, a community advisory board model encouraged local input. Additionally, the system and structure of interaction that this network has developed over ∼20 years allows for efficient and productive involvement that capitalizes on the strengths of partnerships and interdisciplinary exchange. Another advantage of a regional network is that individuals and families dealing with complex health issues like cancer must often interact with cross-state health systems in coordinating access to the care they desire. Further, ACCN academic partners are all land-grant universities, and this fosters outreach to Appalachia through established networks.
The CBPR focus of ACCN ensures that efforts are rooted in the community, and a broad, diverse network of partners promises interdisciplinary approaches to the issues. Given limited funding, fostering collaborative and nontraditional partnerships has helped with the delivery of cancer disparity programming to reach rural and medically underserved populations. For example, the Interdisciplinary Approach to Colorectal Cancer Screening pilot project used community pharmacists to educate clients about CRC screening. The ACCN focuses its efforts to address some of the most glaring cancer-related disparities in the U.S. through flexible and diverse mechanisms, including training the next generation of academic and community members, disseminating scientific work through dozens of publications and presentations, and undertaking new and innovative research projects.
Challenges That Remain
There are numerous challenges that remain in addressing and reducing cancer-related disparities in Appalachia. First, community partnerships that are critical to the identification of health needs and the development and implementation of projects need to be nurtured. Second, communities need to be continually assessed to keep pace with adoption of new technologies, for example, the use of social media, to allow for the most dynamic and salient methods of community cancer prevention and health promotion to be disseminated. Third, the communities in which we work are constantly changing; the Appalachian population is increasingly diverse (e.g., the Hispanic population is growing throughout the region). Appalachians use many forms of technology, an increasing percentage commute to more urban jobs, and, overall, they increasingly defy easy generalizations. The dynamic nature of Appalachian communities makes it ever more important for researchers to spend time in the Appalachian region and to be receptive to the diverse voices of Appalachians in order to disseminate culturally appropriate, effective, and accessible cancer information.
Fourth, a challenge for new and junior investigators is to identify and conduct research with rural communities that are ready for cancer prevention and control research. Previous investments by federal and state agencies and academic centers to develop community-based research networks must be maintained and even enhanced if junior and new investigators are able to succeed in their chosen career of cancer prevention and control research. Fifth, it is important to consider the economic challenges that Appalachians face, including increasingly scarce individual and community resources (e.g., lower income, absence of available employment, poor/limited health resources). An ongoing challenge in Appalachia is leveraging the limited existing community resources to effectively reduce the local cancer burden. Sixth, the health care landscape is moving rapidly toward large integrated health care networks with multiple partnerships and affiliations among payers, providers, and employers. A challenge for Appalachian communities is to remain effectively integrated into this shifting health care environment that seems to push toward high patient volume. We have to question if cancer diagnosis and treatment will be a priority in small rural communities with low patient volume and if these communities will be effectively represented in these large networks.
Additional challenges include: addressing the aging of the U.S. (including Appalachian) population, especially the impact of lack of sustainability of the workforce in public health positions and coalitions/volunteerism; addressing issues related to cancer survivorship; improving the timeliness and completeness of reporting of, and quality of, cancer-related data in the region; evaluating and including proven aspects of cancer navigation across the cancer continuum; reaching, effectively and efficiently, a greater number of people living in low population density areas of rural Appalachia; increasing participation in cancer screening of all types, particularly for men and persons at high risk for cancer; increasing participation in clinical trials; and sustaining research funding for research and outreach. Finally, the cancer research community must recognize that cancer-related disparities are associated with socioeconomic status as much as, and in some instances more so than, race and ethnicity [39]. This recognition should lead to the cancer research community embracing a multilevel, transdisciplinary approach to cancer prevention and control research.
Recommendations
There are numerous opportunities for the ACCN to contribute to a reduction in cancer-related disparities in Appalachia, and these same opportunities may serve as recommendations for working with underserved white and rural populations. First, it is important to recognize the assets of communities and not merely the deficits. For example, resilience is a principal asset of Appalachian communities and this principle could be advantageous to CBPR efforts. Second, it is recommended that researchers follow the lead of the community in identifying high-priority populations and health problems, ensuring that vision extends beyond traditional designations and focuses on health inequity and needs. Further, researchers and institutions should be flexible about the approaches taken to address health inequities. For example, the ACCN has focused on energy balance, a primary prevention strategy for cancer, in addition to promoting screening. Third, the level of analysis should be expanded beyond a focus on individual behavior change to include consideration of the effects of policy-level changes. For example, policy change to reduce barriers to CRC screening, particularly in underresourced communities where gaining access to colonoscopy presents a tangible challenge to many, would go a long way in promoting screening. Fourth, outreach and research should use social media and technology. The ACCN, as a regional network, can take advantage of the investment that has been made in improving the technology infrastructure in Appalachia and the increased capacity for distance communication, conferencing, Webinars, education, and telehealth services. Fifth, greater resources for cancer-related support programs in Appalachia are needed. Specifically, more human papillomavirus programming to increase the acceptability and uptake of vaccination among age-appropriate individuals is needed, along with CRC education initiatives to increase screening in this population. Sixth, additional resources for surveillance research are needed in order to better characterize disparities, such as those for differences in the proportions of cancers reported with unknown stage. Finally, acknowledgment of place-based disparities, such as those observed in Appalachia, should be standard, and appropriate means to address resource inequity should be provided. These recommendations need not be only financial resources, but also support from all levels—for example, community members, the health care sector, researchers, and policy makers—to be implemented successfully. Without this unified commitment, reducing cancer health disparities in underserved white populations, like Appalachia, will be a continual uphill struggle.
Acknowledgments
This work was supported by National Institutes of Health/National Cancer Institute Appalachia Community Cancer Network grant U01 114622.
Author Contributions
Conception/Design: Electra D. Paskett, Eugene J. Lengerich, Nancy E. Schoenberg, Mark Dignan, Stephanie K. Kennedy, Mary Ellen Conn, Karen A. Roberto, Sharon K. Dwyer, Darla Fickle
Collection and/or assembly of data: James L. Fisher, Electra D. Paskett, Eugene J. Lengerich, Nancy E. Schoenberg, Mark Dignan, Stephanie K. Kennedy, Mary Ellen Conn, Karen A. Roberto, Sharon K. Dwyer, Darla Fickle
Data analysis and interpretation: Electra D. Paskett, Eugene J. Lengerich, Nancy E. Schoenberg, Mark Dignan, Stephanie K. Kennedy, Mary Ellen Conn, Karen A. Roberto, Sharon K. Dwyer, Darla Fickle
Manuscript writing: James L. Fisher, Electra D. Paskett, Eugene J. Lengerich, Nancy E. Schoenberg, Mark Dignan, Stephanie K. Kennedy, Mary Ellen Conn, Karen A. Roberto, Sharon K. Dwyer, Darla Fickle
Final approval of manuscript: James L. Fisher, Electra D. Paskett, Eugene J. Lengerich, Nancy E. Schoenberg, Mark Dignan, Stephanie K. Kennedy, Mary Ellen Conn, Karen A. Roberto, Sharon K. Dwyer, Darla Fickle
References
- 1.Appalachian Regional Commission. [accessed June 27, 2011]. Available at http://www.arc.gov.
- 2.Pollard KM. A New Diversity: Race and Ethnicity in the Appalachian Region Report from the Appalachian Regional Commission. [accessed June 27, 2011]. Available at http://www.arc.gov/assets/research_reports/ANewDiversityRaceandEthnicityinAppalachia.pdf.
- 3.Yabroff KR, Lawrence WF, King JC, et al. Geographic disparities in cervical cancer mortality: What are the roles of risk factor prevalence, screening, and use of recommended treatment? J Rural Health. 2005;21:149–157. doi: 10.1111/j.1748-0361.2005.tb00075.x. [DOI] [PubMed] [Google Scholar]
- 4.Katz ML, Wewers ME, Single N, et al. Key informants' perspectives prior to beginning a cervical cancer study in Ohio Appalachia. Qual Health Res. 2007;17:131–141. doi: 10.1177/1049732306296507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoenberg NE, Hopenhayn C, Christian A, et al. An in-depth and updated perspective on determinants of cervical cancer screening among central Appalachian women. Women Health. 2005;42:89–105. doi: 10.1300/j013v42n02_06. [DOI] [PubMed] [Google Scholar]
- 6.Shell R, Tudiver F. Barriers to cancer screening by rural Appalachian primary care providers. J Rural Health. 2004;20:368–373. doi: 10.1111/j.1748-0361.2004.tb00051.x. [DOI] [PubMed] [Google Scholar]
- 7.Shipp MP, Desmond R, Accortt N, et al. Population-based study of the geographic variation in colon cancer incidence in Alabama: Relationship to socioeconomic status indicators and physician density. South Med J. 2005;98:1076–1082. doi: 10.1097/01.smj.0000184844.01148.10. [DOI] [PubMed] [Google Scholar]
- 8.Tessaro I, Mangone C, Parkar I, et al. Knowledge, barriers, and predictors of colorectal cancer screening in an Appalachian church population. Prev Chronic Dis. 2006;3:A123. [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly KM, Phillips CM, Jenkins C, et al. Physician and staff perceptions of barriers to colorectal cancer screening in Appalachian Kentucky. Cancer Control. 2007;14:167–175. doi: 10.1177/107327480701400210. [DOI] [PubMed] [Google Scholar]
- 10.Behringer B, Friedell GH. Appalachia: Where place matters in health. Prev Chronic Dis. 2006;3:A113. [PMC free article] [PubMed] [Google Scholar]
- 11.Couto RA. NIH Publication No. 94-3779. Bethesda, MD: NIH; 1994. Appalachia. Sowing Seeds in the Mountains. Community-Based Coalitions for Cancer Prevention and Control; pp. 1–343. [Google Scholar]
- 12.Jones L. Ashland, KY: The Jesse Stuart Foundation; 1994. Appalachian Values; p. 9. [Google Scholar]
- 13.Armstrong LR, Thompson T, Hall HI, et al. Colorectal carcinoma mortality among Appalachian men and women, 1969–1999. Cancer. 2004;101:2851–2858. doi: 10.1002/cncr.20667. [DOI] [PubMed] [Google Scholar]
- 14.Friedell GH, Rubio A, Maretzki A, et al. Community cancer control in a rural, underserved population: The Appalachian Leadership Initiative on Cancer Project. J Health Care Poor Underserved. 2001;12:5–19. doi: 10.1353/hpu.2010.0523. [DOI] [PubMed] [Google Scholar]
- 15.Lung cancer death rates in Appalachia, 1994–1998. J Natl Cancer Inst. 2002;94:1190. [PubMed] [Google Scholar]
- 16.Hall HI, Rogers JD, Weir HK, et al. Breast and cervical carcinoma mortality among women in the Appalachian region of the U.S., 1976–1996. Cancer. 2000;89:1593–1602. doi: 10.1002/1097-0142(20001001)89:7<1593::aid-cncr25>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC) Cancer death rates–Appalachia, 1994–1998. MMWR Morb Mortal Wkly Rep. 2002;51:527–529. [PubMed] [Google Scholar]
- 18.Hopenhayn C, Bush H, Christian A, et al. Comparative analysis of invasive cervical cancer incidence rates in three Appalachian states. Prev Med. 2005;41:859–864. doi: 10.1016/j.ypmed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Hopenhayn C, Jenkins TM, Petrik J. The burden of lung cancer in Kentucky. J Ky Med Assoc. 2003;101:15–20. [PubMed] [Google Scholar]
- 20.Lengerich EJ, Tucker TC, Powell RK, et al. Cancer incidence in Kentucky, Pennsylvania, and West Virginia: Disparities in Appalachia. J Rural Health. 2005;21:39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 21.Lengerich EJ, Wyatt SW, Rubio A, et al. The Appalachia Cancer Network: Cancer control research among a rural, medically underserved population. J Rural Health. 2004;20:181–187. doi: 10.1111/j.1748-0361.2004.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 22.Singh GK, Miller BA, Hankey BF, et al. Persistent area socioeconomic disparities in U.S. incidence of cervical cancer, mortality, stage, and survival, 1975–2000. Cancer. 2004;101:1051–1057. doi: 10.1002/cncr.20467. [DOI] [PubMed] [Google Scholar]
- 23.Singh GK, Miller BA, Hankey BF, et al. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: Part I—all cancers among men. J Natl Cancer Inst. 2002;94:904–915. doi: 10.1093/jnci/94.12.904. [DOI] [PubMed] [Google Scholar]
- 24.Spitler HD, Mayo RM, Parker VG. Patterns of breast, cervical, colorectal, and prostate cancer in the Appalachian region of South Carolina. Ethn Dis. 2001;11:51–59. [PubMed] [Google Scholar]
- 25.Wyatt SW, Huang B, Tucker TC, et al. Geographic trends in cervical cancer incidence and mortality in Kentucky, 1995–2000. J Ky Med Assoc. 2004;102:11–14. [PubMed] [Google Scholar]
- 26.Wingo PA, Tucker TC, Jamison PM, et al. Cancer in Appalachia, 2001–2003. Cancer. 2008;112:181–192. doi: 10.1002/cncr.23132. [DOI] [PubMed] [Google Scholar]
- 27.Lexington, KY: Appalachia Community Cancer Network; 2009. The Cancer Burden in Appalachia 2009; pp. 1–32. [Google Scholar]
- 28.Fisher J, Engelhardt H, Stephens J, et al. Cancer-related disparities among residents of Appalachia Ohio. J Health Dispar Res Pract. 2008;2:61–74. [Google Scholar]
- 29.Israel BA, Schulz AJ, Parker EA. San Francisco: John Wiley & Sons, Inc.; 2005. Methods in Community-Based Participatory Research for Health; pp. 1–528. [Google Scholar]
- 30.Garland B, Crane M, Marino C, et al. Effect of community coalition structure and preparation on the subsequent implementation of cancer control activities. Am J Health Promot. 2004;18:424–434. doi: 10.4278/0890-1171-18.6.424. [DOI] [PubMed] [Google Scholar]
- 31.Tarasenko YN, Schoenberg NE, Bennett K. The emergency department as a potential intervention recruitment venue among vulnerable rural residents. J Prim Care Community Health. 2011;2:77–81. doi: 10.1177/2150131910391534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leach CR, Schoenberg NE, Hatcher J. Factors associated with participation in cancer prevention and control studies among rural Appalachian women. Fam Community Health. 2011;34:119–125. doi: 10.1097/FCH.0b013e31820de9bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Swanson M, Studts CR, Bardach SH, et al. Intergenerational energy balance interventions: A systematic literature review. Health Educ Behav. 2011;38:171–197. doi: 10.1177/1090198110378973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hatcher J, Dignan MB, Schoenberg NE. How do rural health care providers and patients view barriers to colorectal cancer screening? Insights from Appalachian Kentucky. Nurs Clin North Am. 2011;22:176–194. doi: 10.1016/j.cnur.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schoenberg N, Baltisberger J, Bardach S, et al. Perspectives on Pap test follow-up care among rural Appalachian women. Womens Health. 2010;50:580–597. doi: 10.1080/03630242.2010.516702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Curry WJ, Lengerich EJ, Kluhsman BC, et al. Academic detailing to increase colorectal cancer screening by primary care practices in Appalachian Pennsylvania. BMC Health Serv Res. 2011;11:112. doi: 10.1186/1472-6963-11-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barcus H. The emergence of new Hispanic settlement patterns in Appalachia. Prof Geogr. 2007;59:298–315. [Google Scholar]
- 38.Dominic OG, Lengerich EJ, Wray WA, et al. Barriers to colorectal cancer screening among Latino/Hispanic adults in urban and rural Pennsylvania: Results from the ACCN. Am J Health Behav. 2011 (in press) [Google Scholar]
- 39.Foster-Bey J, Jeffries T, Wipperman M, et al. Arlington, VA: CSR, Inc.; 2011. National Evaluation of the Community Networks Program to Reduce Cancer Health Disparities through Education, Research, and Training 2011; pp. 1–115. [Google Scholar]