The quantity, research design, and research topics of palliative oncology publications in the first 6 months of 2004 and 2009 were reviewed, and significant deficiencies were identified.
Keywords: Literature, Neoplasms, Palliative care, Research design
Abstract
The current state of the palliative oncology literature is unclear. We examined and compared the quantity, research design, and research topics of palliative oncology publications in the first 6 months of 2004 with the first 6 months of 2009. We systematically searched MEDLINE, PsychInfo, EMBASE, ISI Web of Science, and CINAHL for original studies, review articles, and systematic reviews related to “palliative care” and “cancer” during the first 6 months of 2004 and 2009. Two physicians reviewed the literature independently and coded the study characteristics with high inter-rater reliability. We found a consistent decrease in the proportion of oncology studies related to palliative care between 2004 and 2009, despite an absolute increase in the total number of palliative oncology studies. Combining the two time periods, the most common original study designs were case report/series, cross-sectional studies, and qualitative studies. Randomized controlled trials comprised 6% of all original studies. The most common topics were physical symptoms, health services research, and psychosocial issues. Communication, decision making, spirituality, education, and research methodologies all represented <5% of the literature. Comparing 2004 with 2009, we found an increase in the proportion of original studies among all palliative oncology publications but no significant difference in study design or research topic. We identified significant deficiencies in the quantity, design, and scope of the palliative oncology literature. Further effort and resources are necessary to improve the evidence base for this important field.
Introduction
Since Dr. Cicely Saunders founded the first academic hospice in the U.K. in 1967, palliative care has evolved into a discipline that places an increasing emphasis on interdisciplinary evidence-based practice. This is supported by the growing number of clinical studies in palliative care and the larger proportion of clinical trials in this field over the past few decades [1]. Despite significant developments in the palliative care literature, there remain many challenges to conducting and publishing palliative care research, including limited research funding [2], few trained personnel, difficulty in recruiting and retaining patients [3], and other methodologic issues [4, 5]. Keeping up with the palliative care literature has also been difficult because of challenges in searching the bibliographic databases [6], a lack of definitional clarity [7], and the highly heterogeneous research topics and methodologies [8, 9].
The palliative care literature is highly complex and diverse. Unlike other disciplines, the field of palliative care transects numerous domains. Whereas established disciplines predominantly focus on the diagnosis and management of specific disorders, a wide array of topics fall under palliative care, ranging from symptom management to psychosocial care, spiritual issues, communication, decision making, ethics, end-of-life care, and health services. Furthermore, the study population can vary widely, including patients at different stages of illness, caregivers, and health professionals. The interdisciplinary nature of palliative care also means that the published literature is derived from a wide range of professional disciplines, further increasing the diversity.
Despite important efforts in establishing a framework for research [10, 11], there remains no consensus on the taxonomy of the palliative care literature. This is partly a result of the difficulty in defining what constitutes the literature and the tremendous work involved in systematically classifying studies. A number of papers have examined palliative care publications in selected journals [2, 12–14] or radiation oncology meetings [15, 16]. Others have focused on palliative care qualitative studies [17, 18], observational studies [19], or bibliographic searches [1, 8, 20, 21]. However, no study to date has systematically reviewed the published literature in palliative oncology. A better understanding of the range of studies that constitute the palliative cancer care literature would help assess our progress, identify areas for research, and facilitate a systematic classification system. In this study, we examined and compared the quantity, study design, and research topics of palliative oncology publications in the first 6 months of 2004 with the first 6 months of 2009. We hypothesized that there would be an improvement in the quantity, design, and scope over time.
Methods
Literature Search
The Institutional Review Board at MD Anderson Cancer Center provided approval to proceed without the need for full committee review. Publications were included if they were (a) original studies, reviews, or systematic reviews, (b) related to both palliative care and oncology, and (c) published in the first 6 months of 2004 or 2009. These relatively short time periods were specifically chosen to provide a representative sample of the palliative oncology literature in recent years, balancing the need to retrieve searchable electronic copies of full articles and to ensure that this labor-intensive review process could be completed in a timely fashion. Non-English articles, commentaries, editorials, dissertations, conference abstracts, and letters were excluded. Our clinical librarians (S.D. and S.F.) first searched MEDLINE PubMed, PsychInfo, the Cochrane Library, EMBASE, ISI Web of Science, and CINAHL on October 28, 2009. To identify original studies or review articles related to supportive/palliative care, we used the Boolean expression (Palliat$ or hospice$ or “terminal care”). This search strategy has previously been validated to achieve a specificity of 99.97% among general medical journals [20], and has been used in several other studies [1, 8]. We then further identified studies related to cancer using the following expression (adenocarcinoma OR adenocarcinoma* OR adenosarcoma OR adenosarcoma* OR antineoplastic OR cancer OR cancer* OR carcinoid OR carcinoid* OR carcinoma OR carcinoma* OR glioblastoma OR glioblastoma* OR glioma OR glioma* OR Hodgkin OR Hodgkin* OR leukaemia OR leukaemi* OR leukemia OR leukemi* OR lymphoma OR lymphoma* OR malignan* OR melanoma OR melanoma* OR metastasis OR metasta* OR myelodysplas* OR myeloma OR myeloma* OR neoplasia OR neoplasia* OR neoplasm OR neoplasm* OR non hodgkin* OR nonseminoma* OR oncology OR osteosarcoma OR osteosarcoma* OR sarcoma OR sarcoma* OR seminoma* OR teratoma* OR tumor OR tumor* OR tumour OR tumour* OR waldenstrom*). Our librarians handpicked the articles for the correct date of publication in ISI Web of Science and the Cochrane Library because these databases could not be limited by month of publication. Duplicates were removed.
We also obtained the total number of oncology studies published during the same time period to provide a perspective for the relative change in the palliative oncology literature in MEDLINE PubMed, PsychInfo, the Cochrane Library, EMBASE, and CINAHL. This was achieved by applying the identical search strategy without the palliative care Boolean.
Identifying the Palliative Oncology Literature
A medical oncologist (D.H.) and internist (H.P.), both with palliative oncology research training, reviewed each abstract independently for relevance to palliative oncology, and rated the studies as “Yes”, “No,” or “Further review.” To qualify, studies had to be related to both cancer and palliative care based on the World Health Organization (WHO) definition: “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” [22]. The inter-rater agreement was 78% for the three categories (κ, 0.6; p < .0001). All discrepancies were discussed to come up with a final list of articles.
Study Characteristics
We obtained full electronic copies of all unique publications identified based on the above search strategy. For each publication, one author (D.H.) extracted information regarding the study type (original, systematic review, or review), year of publication, research subjects, research topic, relevance to pediatrics, country of origin of the corresponding author (or first author if corresponding author not stated), and journal type. The countries were further analyzed based on continent and also described in the text as either developed countries (i.e., United Nations Human Development Index [HDI] 2009 ≥0.8) or developing countries (HDI <0.8). The articles were classified as pediatrics if they involved subjects aged ≤18, and as therapeutic studies if they involved any specific treatment(s) (e.g., pharmacologic agents, procedures, counseling) for management of a symptom/disorder. For original studies, the research topic and study methodology (study design and prospective/retrospective nature) were decided based on the primary objective. Single-arm phase II trials were classified as prospective case series. The term “cohort studies” was used specifically for prospective studies with control group(s) and with follow-up over time for specific outcome(s). When a journal type fell under multiple categories, we used a hierarchical approach for classification. For instance, a journal focusing on palliative care issues in oncology was classified as a palliative care/symptom control journal consistently. The same process was used for classifying study topics. Because the abbreviations for journal titles were highly heterogeneous among various bibliometric databases, we reviewed all journal titles manually to ensure consistency.
To determine the accuracy of data collection, a random sample of 100 studies was selected and independently reviewed by another author (H.P.) for all the variables listed above. The inter-rater agreement was >95% for all fields (κ, 0.94–1.0; p < .001).
Statistical Analysis
We summarized the publication characteristics using frequencies, percentages, and 95% confidence intervals. We compared the study characteristics between review articles and original studies using χ2 tests and Fisher's exact test where applicable. For original articles, we also compared 2004 with 2009. A two-sided p-value <.05 was considered to be statistically significant. To determine the inter-rater agreement, we used κ statistics. STATA special edition software (version 10.0; StataCorp LP, College Station, Texas) was used for the statistical analysis.
For the purpose of analysis, we combined systematic reviews with review articles together because they are both derived from existing original studies and aim to summarize the literature.
Results
Literature Search
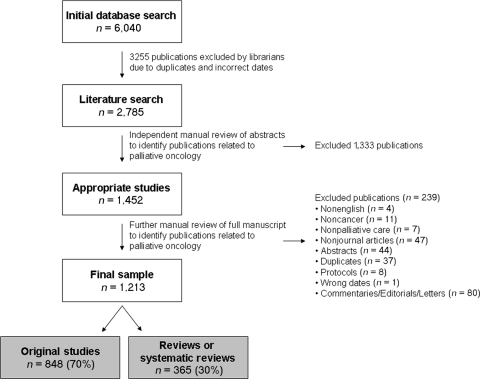
Figure 1 summarizes the palliative oncology literature search process. Among the 2,785 studies identified by our librarian in the initial search, we manually excluded 1,333 (48%) publications because they were not related to either oncology or palliative care. After further review, we excluded another 239 articles, resulting in a final sample of 1,213 publications.
Figure 1.
Study flowchart.
Quantity of Palliative Oncology Studies
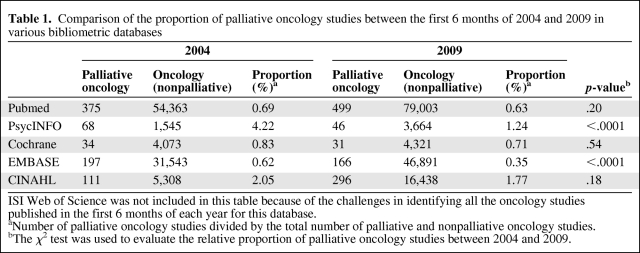
Putting the number of palliative oncology studies from multiple databases in the context of the overall oncology literature, we found a significant decrease in the proportion of oncology studies related to palliative care, despite an absolute increase in the number of palliative oncology studies (Table 1).
Table 1.
Comparison of the proportion of palliative oncology studies between the first 6 months of 2004 and 2009 in various bibliometric databases
ISI Web of Science was not included in this table because of the challenges in identifying all the oncology studies published in the first 6 months of each year for this database.
aNumber of palliative oncology studies divided by the total number of palliative and nonpalliative oncology studies.
bThe χ2 test was used to evaluate the relative proportion of palliative oncology studies between 2004 and 2009.
In the first 6 months of 2004, 344 (64%), 159 (30%), and 32 (6%) of the publications were original studies, review articles, and systematic reviews, respectively. In contrast, the breakdown was 504 (74%), 124 (18%), and 50 (8%) for the first 6 months of 2009 (p < .0001), with a higher proportion of original articles.
Palliative Oncology Literature Characteristics
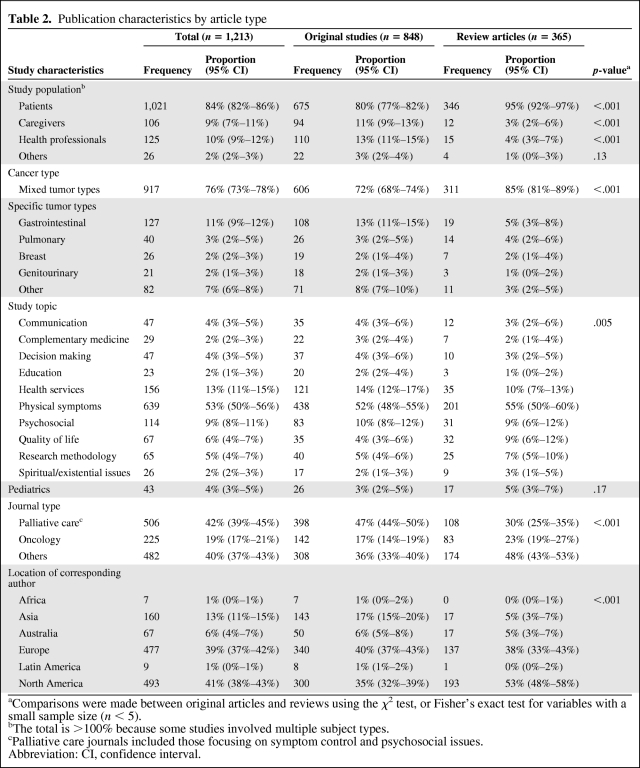
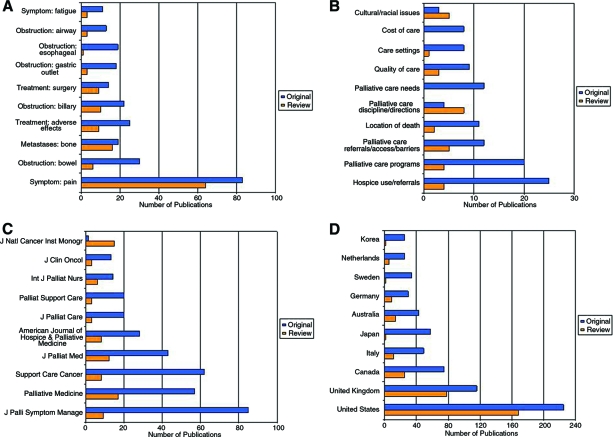
The study characteristics of the 1,213 published studies are shown in Table 2. Although a majority of study subjects were patients (84%), caregivers and health professionals were also involved in 9% and 10% of the studies, respectively. Only 296 (24%) of the studies were associated with a specific cancer type, and the remaining articles consisted of mixed tumor groups. In terms of subject area, studies on physical symptoms (n = 612) were most common, making up 50% of all articles. This was followed by studies on health services research (n = 156, 13%) and psychosocial issues (n = 114, 9%). The most common research topics under physical symptoms and health services research are shown in Figure 2A and 2B. Pediatric studies comprised only 4% of the literature.
Table 2.
Publication characteristics by article type
aComparisons were made between original articles and reviews using the χ2 test, or Fisher's exact test for variables with a small sample size (n < 5).
bThe total is >100% because some studies involved multiple subject types.
cPalliative care journals included those focusing on symptom control and psychosocial issues.
Abbreviation: CI, confidence interval.
Figure 2.
Number of publications based on research topic, journals, and countries. The number of original articles and reviews are shown for the most commonly researched topics under the domain physical symptoms (A), the most commonly researched topics under the domain health services (B), journals with the highest number of palliative oncology publications (C), and countries with the highest number of palliative oncology publications (D).
Forty-two percent of the studies were published in 46 palliative care or symptom control journals, 19% appeared in 71 oncology journals, and the remaining 39% appeared in 289 other journals (Fig. 2C). The corresponding authors were from 41 developed countries and 10 developing countries, and the numbers of studies published for the top 10 countries are shown in Figure 2D. A large majority of the palliative oncology literature was from North America (n = 493, 41%) and Europe (n = 477, 39%). Developing countries accounted for 38 of the 1,213 (3%) studies.
Table 2 highlights the differences between original studies and review articles. Compared with original studies, reviews/systematic reviews were less likely to cover subjects related to caregivers (p < .0001) and health professionals (p < .0001), more likely to have mixed tumor types (p <.0001), and more likely to be published in nonpalliative care journals (p < .0001). Furthermore, a larger proportion of review articles came from North America than from other continents (p < .0001), accounting for over half of all published reviews.
Original Study Design and Scope
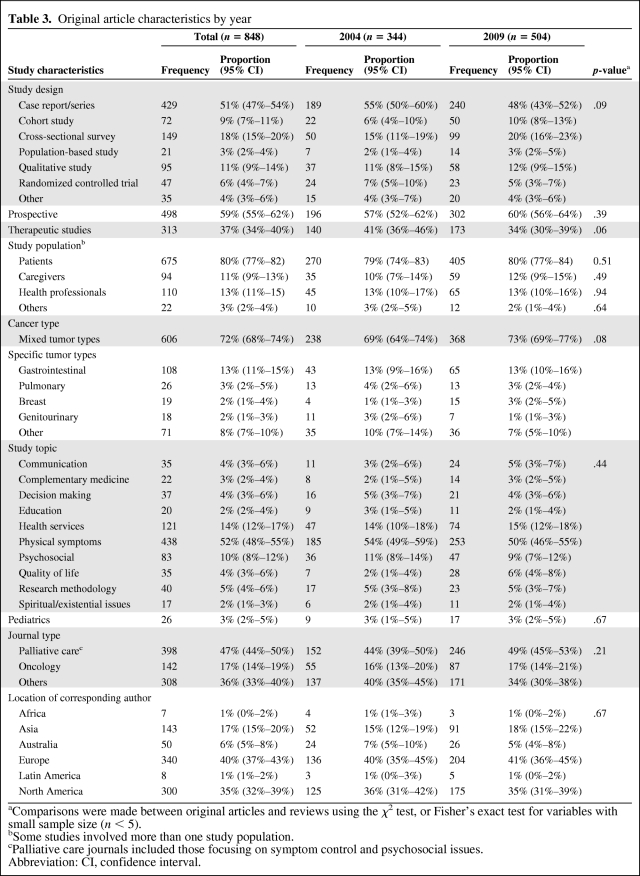
Table 3 shows the study design of the 848 original studies. Fifty-nine percent were prospective studies. The most common study design was case report/series (51%), followed by cross-sectional studies (11%), and qualitative studies (11%). Randomized controlled trials comprised 6% (n = 47) of all original studies. Thirty-seven percent were therapeutic studies. Among the case reports and case series, 164 of 429 (38%) were prospective studies.
Table 3.
Original article characteristics by year
aComparisons were made between original articles and reviews using the χ2 test, or Fisher's exact test for variables with small sample size (n < 5).
bSome studies involved more than one study population.
cPalliative care journals included those focusing on symptom control and psychosocial issues.
Abbreviation: CI, confidence interval.
There was a total of 344 original studies in 2004 and 504 original studies in 2009, representing a 47% increase over the 5 years. No statistically significant difference was noted in study design, research topics, the proportion of prospective studies, or the proportion of therapeutic studies (Table 3).
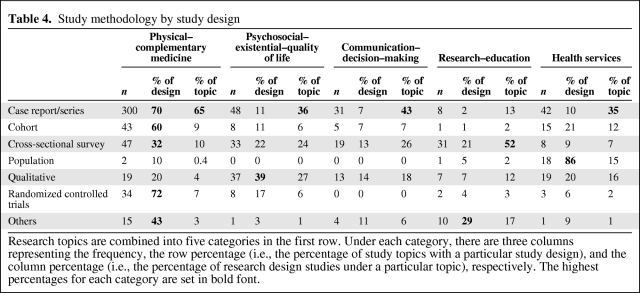
Table 4 illustrates the study design by research topic. Case report/series was the most common study design for all topics with the exception of education/research, in which 52% were cross-sectional surveys. Physical symptoms represented the most common topic for many study designs. However, population-based design was used more in health services research and qualitative study design was used to study psychosocial issues.
Table 4.
Study methodology by study design
Research topics are combined into five categories in the first row. Under each category, there are three columns representing the frequency, the row percentage (i.e., the percentage of study topics with a particular study design), and the column percentage (i.e., the percentage of research design studies under a particular topic), respectively. The highest percentages for each category are set in bold font.
Discussion
We examined >1,200 palliative oncology articles published over two 6-month periods. The proportion of oncology studies that focused on palliative care topics remained small (<1%) and in fact decreased slightly over time. The design of the literature was limited by a preponderance of case series/reports and few randomized controlled trials. Finally, we identified significant areas of deficiency, including only a small number of studies on caregivers and health professionals, and even fewer on communication, decision making, spirituality, education, and research methodologies. Given the high relevance of palliative care to oncology practice [23], further coordination and resources are necessary to improve the quantity, design, and scope of the palliative oncology literature.
Previous studies have predominantly focused on bibliometric analysis and review of selected study abstracts related to palliative care [1, 2, 8, 12–14, 18–21]. In an attempt to provide a more comprehensive and in-depth analysis, we systematically searched through multiple databases, retrieved the full article, and coded the study characteristics with high inter-rater reliability. We were surprised to find that approximately half of the articles from the initial literature search did not fit the palliative oncology profile after manual review (Fig. 1). Many of the excluded studies involved topics such as the role of palliative chemotherapy with survival as the primary endpoint, which did not clearly fit the WHO definition of palliative care. Our observation points to the low specificity of this search strategy for palliative care in bibliographic databases, and the need to manually examine studies for inclusion.
Consistent with other studies [12], the absolute quantity of oncology publications related to palliative care remained small (<1%). Teiman et al. [1] previously reviewed PubMed publications and found that the proportion of palliative care studies in the context of the overall medical literature increased over time. In this study, we specifically compared the palliative oncology literature with the greater oncology literature and found a consistent decrease across multiple databases. This observation is likely because the overall growth in palliative oncology was slower than in other areas of oncology (e.g., drug development). Another potential explanation is that palliative care research may be conducted in areas outside cancer care, suggesting a divergence between the oncology and palliative care literature as palliative care matures as a specialty.
There was, on average, one review article for every two original studies, although we were encouraged to see an increase in the proportion of original studies in 2009. Although review articles can be very useful in summarizing information, they represent subjective interpretation of the literature with a potential for bias. Systematic reviews are designed to minimize bias because they typically outline the search strategies and follow a rigid methodology during the evaluation process. Nevertheless, a recent study of Cochrane systematic reviews in palliative care found that they failed “to provide good evidence for clinical practice because the primary studies are few in number, small, clinically heterogeneous, and of poor quality and external validity” [9]. Thus, until we can improve both the quantity and quality of original studies, reviews and systematic reviews may have a limited role in consolidating the existing literature.
Our examination of study design provided an indirect measure regarding the quality of studies. Interestingly, 60% of all studies were prospective in nature, although a majority were case series. We found that >50% of the original studies were case reports/series, and did not detect an increase in the proportion of analytical studies (i.e., cohort studies and randomized controlled trials) over time. Our results are consistent with those reported by Kaasa et al. [12], raising the concern that the palliative oncology literature is flooded with descriptive studies when we urgently need more practice-changing analytical studies to advance this field. Also worrisome is the lack of progress over the 5-year period. Further studies are required to examine the quality of existing studies in detail.
In regard to research topics, physical symptoms, health services research, and psychosocial issues were the most commonly studied. On the one hand, there appeared to be an abundance of studies on pain (n = 146, 12% of all studies) and various types of obstructions (n = 144, 12%). On the other hand, there remained many “orphaned” topics even under physical symptoms, such as constipation, anorexia-cachexia, bleeding, and edema. Other aspects of palliative care, including communication, decision making/ethics, education, research methodology, and spirituality, each comprised ≤5% of all studies. Pediatric palliative care remained largely unexplored. Our study highlights important gaps in the literature and areas warranting further research.
Consistent with other studies, we found that developing countries contributed to only 3% of all studies [24]. Research output generally corresponded to the level of palliative care development worldwide [25]. Although much of the existing palliative oncology literature was derived from developed countries, we recently reported limited palliative care research infrastructure and training for research personnel among National Cancer Institute–designated cancer centers in the U.S. [26], suggesting significant room for improvement even among developed nations. A steady increase in palliative care research globally could facilitate adequately powered multicenter clinical trials.
As demonstrated in this study, the palliative oncology literature is highly diverse in terms of research methodology, research topics, and journal distribution. Nevertheless, we were able to categorize the research methodology and research topics with a high degree of inter-rater consistency, suggesting that our framework is feasible for classifying studies. The wide journal distribution (>400 titles in the search) makes it a challenge to conduct bibliographic searches and to keep up with the literature. Electronic means of summarizing and rapidly distributing the findings of high-quality studies may be helpful for busy clinicians [27].
Our study has a number of limitations. First, we focused only on oncology-related studies and cannot comment on the noncancer palliative care literature. Second, the sensitivity of our literature search was limited by the use of a specific Boolean for palliative care, and thus likely had a lower sensitivity. For instance, we found that studies in the Journal of Supportive Oncology did not show up consistently in our search. Nevertheless, this search strategy represents the most validated to date, and it has been used in multiple previous studies [1, 8]. Third, we only examined studies published during two 6-month periods. The short time frames may not provide an accurate assessment of trends over time. A more extensive review would have taken an unreasonable amount of time because the review process was labor intensive. Fourth, we did not include letters, commentaries, meeting abstracts, or grey literature. Fifth, we classified study methodologies and topics based on the primary objective of each study for consistency. However, some studies had multiple research questions and methodologies. For instance, some studies labeled as case series had a cross-sectional design examining associations among variables within the cohort. Finally, although we were able to combine the search results from multiple databases and provide the total number of unique palliative oncology publications, we were not able to do the same for the greater oncology literature because of the vast number of records.
Conclusions
To our knowledge, this is the most comprehensive attempt to review the palliative oncology literature. It provides an overview of this pleomorphic and constantly evolving entity, and highlights the need to further improve the quantity, design, and scope of palliative oncology research. Specifically, we need to develop more sensitive and specific tools for literature searches, to design adequately powered clinical trials, and to conduct more studies on caregivers, health care professionals, and nonphysical topics in palliative care. Our findings raise serious concerns about the current state of knowledge creation regarding palliative cancer care. More research is needed to identify why there are limited incentives for institutions and individuals to conduct and publish these greatly needed contributions.
Acknowledgments
Supported in part by the National Institutes of Health grants RO1NR010162-01A1, RO1CA122292-01, and RO1CA124481-01 (E.B.).
Author Contributions
Conception/Design: David Hui, Henrique A. Parsons, Shamsha Damani, Stephanie Fulton, Jun Liu, Avery Evans, Maxine De La Cruz, Eduardo Bruera
Collection and/or assembly of data: David Hui, Henrique A. Parsons, Shamsha Damani, Stephanie Fulton
Data analysis and interpretation: David Hui, Henrique A. Parsons, Jun Liu, Avery Evans, Maxine De La Cruz, Eduardo Bruera
Manuscript writing: David Hui, Eduardo Bruera
Final approval of manuscript: David Hui, Henrique A. Parsons, Shamsha Damani, Stephanie Fulton, Jun Liu, Avery Evans, Maxine De La Cruz, Eduardo Bruera
References
- 1.Tieman J, Sladek R, Currow D. Changes in the quantity and level of evidence of palliative and hospice care literature: The last century. J Clin Oncol. 2008;26:5679–5683. doi: 10.1200/JCO.2008.17.6230. [DOI] [PubMed] [Google Scholar]
- 2.Gelfman LP, Morrison RS. Research funding for palliative medicine. J Palliat Med. 2008;11:36–43. doi: 10.1089/jpm.2006.0231. [DOI] [PubMed] [Google Scholar]
- 3.Ling J, Rees E, Hardy J. What influences participation in clinical trials in palliative care in a cancer centre? Eur J Cancer. 2000;36:621–626. doi: 10.1016/s0959-8049(99)00330-5. [DOI] [PubMed] [Google Scholar]
- 4.Rinck GC, van den Bos GA, Kleijnen J, et al. Methodologic issues in effectiveness research on palliative cancer care: A systematic review. J Clin Oncol. 1997;15:1697–1707. doi: 10.1200/JCO.1997.15.4.1697. [DOI] [PubMed] [Google Scholar]
- 5.Krouse RS, Rosenfeld KE, Grant M, et al. Palliative care research: Issues and opportunities. Cancer Epidemiol Biomarkers Prev. 2004;13:337–339. [PubMed] [Google Scholar]
- 6.Tieman JJ, Abernethy A, Currow DC. Not published, not indexed: Issues in generating and finding hospice and palliative care literature. J Palliat Med. 2010;13:669–675. doi: 10.1089/jpm.2009.0273. [DOI] [PubMed] [Google Scholar]
- 7.NIH State-of-the-Science Conference Statement on improving end-of-life care. NIH Consens State Sci Statements. 2004;21:1–26. [PubMed] [Google Scholar]
- 8.Tieman JJ, Sladek RM, Currow DC. Multiple sources: Mapping the literature of palliative care. Palliat Med. 2009;23:425–431. doi: 10.1177/0269216309102727. [DOI] [PubMed] [Google Scholar]
- 9.Wee B, Hadley G, Derry S. How useful are systematic reviews for informing palliative care practice? Survey of 25 Cochrane systematic reviews. BMC Palliat Care. 2008;7:13. doi: 10.1186/1472-684X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Currow DC, Wheeler JL, Glare PA, et al. A framework for generalizability in palliative care. J Pain Symptom Manage. 2009;37:373–386. doi: 10.1016/j.jpainsymman.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 11.Payne SA, Turner JM. Research methodologies in palliative care: A bibliometric analysis. Palliat Med. 2008;22:336–342. doi: 10.1177/0269216308090072. [DOI] [PubMed] [Google Scholar]
- 12.Kaasa S, Hjermstad MJ, Loge JH. Methodological and structural challenges in palliative care research: How have we fared in the last decades? Palliat Med. 2006;20:727–734. doi: 10.1177/0269216306072620. [DOI] [PubMed] [Google Scholar]
- 13.Hermsen MA, ten Have HA. Moral problems in palliative care journals. Palliat Med. 2001;15:425–431. doi: 10.1191/026921601680419483. [DOI] [PubMed] [Google Scholar]
- 14.Puchalski CM, Kilpatrick SD, McCullough ME, et al. A systematic review of spiritual and religious variables in Palliative Medicine, American Journal of Hospice and Palliative Care, Hospice Journal, Journal of Palliative Care, and Journal of Pain and Symptom Management. Palliat Support Care. 2003;1:7–13. doi: 10.1017/s1478951503030128. [DOI] [PubMed] [Google Scholar]
- 15.Barnes EA, DeBoer G, Chow E. Symptom control and palliative care content of abstracts presented at the Canadian Association of Radiation Oncologists annual meetings. Support Care Cancer. 2004;12:91–94. doi: 10.1007/s00520-003-0564-3. [DOI] [PubMed] [Google Scholar]
- 16.Barnes EA, Palmer JL, Bruera E. Prevalence of symptom control and palliative care abstracts presented at the Annual Meeting of the American Society for Therapeutic Radiology and Oncology. Int J Radiat Oncol Biol Phys. 2002;54:211–214. doi: 10.1016/s0360-3016(02)02919-x. [DOI] [PubMed] [Google Scholar]
- 17.Bailey C, Froggatt K, Field D, et al. The nursing contribution to qualitative research in palliative care 1990–1999: A critical evaluation. J Adv Nurs. 2002;40:48–60. doi: 10.1046/j.1365-2648.2002.02339.x. [DOI] [PubMed] [Google Scholar]
- 18.Borreani C, Miccinesi G, Brunelli C, et al. An increasing number of qualitative research papers in oncology and palliative care: Does it mean a thorough development of the methodology of research? Health Qual Life Outcomes. 2004;2:7. doi: 10.1186/1477-7525-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hadley G, Derry S, Moore RA, et al. Can observational studies provide a realistic alternative to randomized controlled trials in palliative care? J Pain Palliat Care Pharmacother. 2009;23:106–113. doi: 10.1080/15360280902899921. [DOI] [PubMed] [Google Scholar]
- 20.Sladek R, Tieman J, Fazekas BS, et al. Development of a subject search filter to find information relevant to palliative care in the general medical literature. J Med Libr Assoc. 2006;94:394–401. [PMC free article] [PubMed] [Google Scholar]
- 21.Sladek RM, Tieman J, Currow DC. Improving search filter development: A study of palliative care literature. BMC Med Inform Decis Mak. 2007;7:18. doi: 10.1186/1472-6947-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. WHO Definition of Palliative Care. [accessed August 10, 2009]. Available at http://www.who.int/cancer/palliative/definition/en/
- 23.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 24.Pastrana T, Vallath N, Mastrojohn J, et al. Disparities in the contribution of low- and middle-income countries to palliative care research. J Pain Symptom Manage. 2010;39:54–68. doi: 10.1016/j.jpainsymman.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 25.Wright M, Wood J, Lynch T, et al. Mapping levels of palliative care development: A global view. J Pain Symptom Manage. 2008;35:469–485. doi: 10.1016/j.jpainsymman.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 26.Hui D, Elsayem A, De la Cruz M, et al. Availability and integration of palliative care at US cancer centers. JAMA. 2010;303:1054–1061. doi: 10.1001/jama.2010.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Academy of Hospice and Palliative Medicine. Fast Article Critical Summaries for Clinicians in Palliative Care (PC-FACS) [accessed September 15, 2010]. Available at http://www.aahpm.org/membership/default/pcfacs.html.