Abstract
Breast cancer is the most commonly diagnosed cancer in women. Insomnia is a significant problem in breast cancer patients, affecting between 20% to 70% of newly diagnosed or recently treated cancer patients. Pain, fatigue, anxiety, and depression are also common conditions in breast cancer and often co-occur with insomnia in symptom clusters, exacerbating one another, and decreasing quality of life (QOL). There have been no clinical trials of drugs for sleep in cancer. Cognitive behavioral psychotherapies on the other hand, have shown some of the most positive results in alleviating the distressing symptoms that often accompany the breast cancer experience, but even these studies have not targeted the symptom cluster. Pharmacological as well as non-pharmacological treatments need to be explored. It might be that a combined pharmacological and behavioral treatment is most efficacious. In short, substantially more research is needed to fully understand and treat the symptom cluster of insomnia, fatigue, pain, depression and anxiety in breast cancer.
Introduction
Breast cancer is the most commonly diagnosed cancer in women, accounting for approximately 32% of all new yearly cancer diagnoses among women in the U.S.[1] The prevalence rates of psychological distress among breast cancer patients are high: up to 45% of early breast cancer patients and 42% of metastatic breast cancer patients endorse a psychiatric DSM-IV diagnosis.[2] Insomnia is a significant problem in breast cancer patients, affecting between 20% to 70% of newly diagnosed or recently treated cancer patients, double that of the general population. Pain, fatigue, anxiety, and depression are also common conditions in breast cancer and often co-occur with insomnia in symptom clusters, exacerbating one another, and decreasing quality of life (QOL).
The prevalence of these symptoms in breast cancer has sparked a plethora of research studies looking at the relationships between the breast cancer experience and various medical, physical, psychological and social factors. There is still much to learn about the etiology of each symptom, the relationship among the symptoms, as well as their underlying pathophysiological mechanisms. Nevertheless, a variety of intervention studies have reported ways to reduce distress and increase QOL in breast cancer patients. Most studies have used behavioral treatments, mostly cognitive behavioral therapy (CBT) interventions, to treat one or two specific symptoms using different modalities of CBT. Few studies have looked at the effect of medications. To date, no studies have looked at a comprehensive intervention for all the symptoms in the symptom cluster.
In this paper we briefly review the prevalence and discuss the phenomenology of insomnia, fatigue, depression and pain in breast cancer and list the treatments that have been tested on these symptoms. Our manifold goals are to foster awareness of the prevalence and severity of these symptoms in breast cancer patients, encourage health care providers to offer evidence-supported treatments to alleviate these symptoms, and suggest new ideas for future research that would advance the science and practice of symptom cluster palliative care in breast cancer patients.
The Breast Cancer Symptom Cluster: Prevalence and Phenomenology
Sleep disturbance
Studies have examined sleep both objectively and subjectively and have confirmed that sleep problems are very common in breast cancer, pre-treatment, during treatment and sometimes for years after treatment.[3] Approximately 20–70% of women with breast cancer suffer from insomnia, including complaints of difficulty staying asleep, difficulty falling back to sleep at night, sleeping less overall.[3] For those patients that experienced insomnia even before their diagnosis, the majority endorse the fact that having cancer exacerbated their sleep problem.[4].
In a study of cancer survivors, 19% reported chronic insomnia (that is, difficulty falling or staying asleep), with 95% of them experiencing the insomnia for more than 6 months. Another 33% did not meet the criteria for a diagnosis of insomnia, but did report sleeping difficulties. This suggests that over half of these cancer survivors had some problem with their sleep.[4]Studies that have used objective measurements of sleep have confirmed that sleep is disturbed, finding that sleep is fragmented with low sleep efficiency (only about 76% of the time in bed spent asleep), more restlessness at night particularly during treatment, and longer sleep onset latency.[5–7]
In a study of sleep disturbances in cancer patients being followed in a pain clinic, 72% reported sleeping difficulties, 52% reported not feeling rested in the morning, 45% had difficulty staying asleep, 29% had difficulty falling asleep, and 27% woke up too early in the morning. When sleep was correlated with other symptoms, it was most often associated with complaints of fatigue or anxiety.[8] However, in another study, sleep disturbances were reported even when pain and anxiety were low suggesting that the sleep problem may be independent of these psychological and physiological factors.[9]
The risk of insomnia is high in cancer patients for various reasons. The cancer itself including tumors that increase steroid production and symptoms of tumor invasion (pain, dyspnea, fatigue, nausea, pruritis) can contribute to poor sleep. Corticosteroid treatment and hormonal fluctuations as a result of chemotherapy also put patients at greater risk for poor sleep. Medications (narcotics, chemotherapy, neuroleptics, sympathomimetics, sedative/hypnotics, steroids, caffeine/nicotine, antidepressants, diet supplements) and environmental factors (disturbing light and noise and/or temperature extremes in the bedroom) also contribute to poor sleep. And last but not least, an increase in psychological distress due to the cancer diagnosis and increased hot flashes caused by menopause, which often is induced by the breast cancer treatment, also need to be evaluated as contributors to insomnia.[10] Insomnia in these cancer patients may lead to fatigue, mood disturbances, contribute to immunosuppression, affect quality of life and might even affect the course of disease.[11]
One theory of insomnia is Speilman’s 3-P model which states that there are predisposing, precipitating and perpetuating factors of insomnia.[12] Savard and Morin hypothesized that in cancer: (1) predisposing factors which increase the individual’s general vulnerability to develop insomnia might be hyper-arousability, being female, aging, as well as a personal and familial history of insomnia; (2) precipitating factors that trigger the onset of sleep disturbances might be the cancer itself, cancer-related emotional impact and functional loss, and cancer-related treatments and pain; (3) perpetuating factors that contribute to the maintenance of sleep disturbance over time might be maladaptive sleep behaviors and faulty beliefs and attitudes about sleep that patients develop.[13]Treatments therefore, whether behavioral or pharmacological, need to target these factors.
The most likely hypothesis about the phenomenology of sleep in breast cancer patients is that the challenges faced by cancer patients may contribute to or cause insomnia, which in turn may feedback to exacerbate medical conditions comorbid with cancer, in particular pain, psychiatric comorbidities, fatigue, use of opioids (which could contribute to daytime sedation and sleep disordered breathing), stimulating or alerting drugs, napping and preexisting sleep disorders.[14] Thus a deleterious feedback loop may be created.
Fatigue
Cancer related fatigue (CRF) is one of the most debilitating, chronic symptoms in patients with cancer, characterized by extreme tiredness and inability to function due to lack of energy. CRF affects quality of life (QOL) and productivity, may lead to poor compliance with chemotherapy regimens and discontinuing treatment.[15,16] Several studies have suggested that breast cancer patients often experience fatigue before, during, and after chemotherapy. Overall in most studies the estimated prevalence of fatigue in breast cancer ranges from 30%–60%.[17]
Studies have suggested that the causes of cancer-related fatigue are multifactorial and include physiological factors (e.g., pain, anemia neuroendocrine changes, altered energy metabolism), psychological factors (e.g., depression, anxiety), socio-cultural factors (e.g., education, cognitive and behavioral response), and chronobiological factors (e.g., sleep and circadian rhythms).[18,19]
Fatigue and Circadian Rhythms
Circadian rhythms, such as alternations of hormone secretion, body temperature, and sleep-wake cycles, are 24-hour rhythms regulated by the suprachiasmatic nucleus in the hypothalamus. The synchronization of this rhythm with the solar day and night is maintained primarily through entrainment by light.
Disrupted circadian activity rhythms have been associated with mortality in cancer.[20] Yet there is little known about the links between circadian rhythms and cancer.[21]Studies have shown that breast cancer patients have more disrupted circadian activity rhythms than healthy controls,[22,23] and that disrupted activity rhythms are highly correlated with a symptom cluster of disrupted sleep, increased fatigue and depression.[24,25] Other studies suggest that cancer itself may be a result of disturbed biological rhythms.[26]
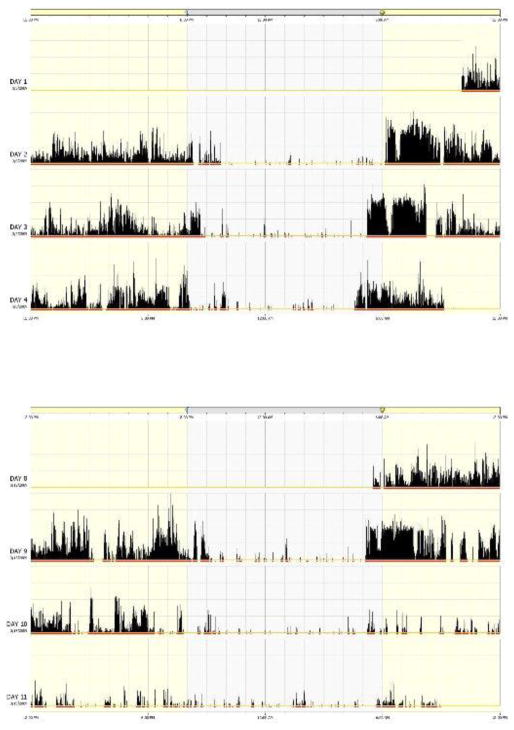
One measure of circadian activity rhythms is with actigraphy. Actigraphy measures wrist movement which can be used to reliably estimate wake and sleep as well as sleep/wake activity rhythms. Figure 1 shows an example of an actigraphic record in one breast cancer patient. Data from our laboratory suggest that the first administration of chemotherapy is associated with transient circadian disruption, while repeated administration of chemotherapy results in progressively worse and more enduring impairments in sleep-wake activity rhythms.[27]
Figure 1.
This is an actigraph record of a 57 year old woman with breast cancer, recorded for three days before and three days during the first week of chemotherapy. Each row represents 24 hours of data. Day 1 through Day 3 represent the recording conducted before the start of chemotherapy (baseline), starting at 8 am on Day 1 and ending at 9 am on the last day. Day 8 through Day 11 are the first three days of the first week of treatment (week 1), starting at 5:30 am on Day 8 and ending at 9 am on the last day. Each vertical line represents one second (called one epoch), and the height of the bar indicates the total amount of movement, or wrist activity, during that minute. The higher the bar, the more movement there is.
During the night, when the woman was asleep, there are fewer and shorter vertical bars. During the day the lines are much more dense and higher. The red horizontal bars below the vertical black bars indicate the wake time, and the rest white blank areas between the red bars indicate sleep time. At baseline, the patient went to bed at around 10 pm and woke up the next morning at around 5 to 6 am. During cycle 1 week 1, the patient went to bed at about 9 pm and got up at about 5:30 am. Compared to baseline, there was more movement during the nights of cycle 1 week 1, indicating disrupted sleep. On the other hand, compared to baseline, there was less movement during the days of week 1, especially during the third day, indicating more inactivity which might represent napping. More movement during the night and less movement during the day, indicates disturbed sleep, as well as disrupted sleep/wake circadian rhythms.
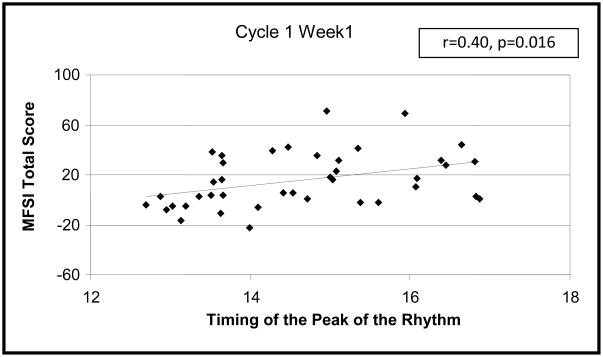
Data from our laboratory also suggest that fatigue is associated with low daytime light exposure.[28] Since decreased light is also associated with disrupted circadian rhythms, we examined whether fatigue and rest-activity circadian rhythms would also be related. The hypothesis was that women with disturbed rest-activity circadian rhythms would report more fatigue before and during the first cycle of chemotherapy. Forty women diagnosed with stage I–III breast cancer, scheduled to receive adjuvant or neoadjuvant anthracycline-based chemotherapy, were studied. Fatigue was assessed using the Short Form of Multidimensional Fatigue Symptom Inventory (MFSI-SF). Rest-activity circadian rhythms were recorded with wrist actigraphy. More fatigue was associated with more disrupted rhythms, less activity both during the day and night, and a more delayed phase (that is, falling asleep later in the night and waking up later in the morning) (see Figure 2). While causality could not be determined in this study, the data suggested that while fatigue may worsen secondary to chemotherapy, it may be mediated, in part, by desynchronized circadian rhythms.
Figure 2.
Scatterplot of total fatigue (MFSI-SF total score) and the timing of the peak of the circadian rhythm during the treatment week of cycle 1 of chemotherapy (r=0.40; p=0.016). The plot shows that the more fatigue reported by the women (that is, the higher the score on the MFSI-sf), the later the peak of their circadian activity rhythm (that is, the later they went to bed and the later the awoke in the morning).
Depression and Anxiety
Depressive symptoms are the most common mood disturbance experienced in cancer patients.[29] Women with breast cancer are not exceptions, although anxiety is also prevalent in this population. Most studies have shown that depressive disorders are common in breast cancer patients. In the DSM-IV, such disorders include major depressive disorder, dysthymic disorder, adjustment disorder with depressive mood and mixed depressive and anxious mood disorders. Other commonly encountered psychiatric disorders in breast cancer patients include anxiety disorders including generalized anxiety disorder, post-traumatic stress syndrome, and adjustment disorder with anxious mood.[2]
A study by Bardwell and colleagues reported that depressive symptoms in 2,595 breast cancer survivors were associated with stressful life events, less optimism, ambivalence over expressing negative emotions, sleep disturbance and poorer social functioning.[30] The researchers found that the depressive symptoms were not associated with any of the objective cancer related variables (e.g., stage, treatment). Notably, one study examined 24,696 older breast cancer patients and found that 1,841 were diagnosed with depression before the breast cancer diagnosis. The depressed women were more likely to receive less-than-definitive cancer treatment and had worse survival rates (that were not better explained by the differences in cancer treatment) compared to the women without depression.[31] This implies that depression and its correlates may increase the likelihood of receiving less than optimal cancer treatment by healthcare providers and/or that depressed patients may have rates of adherence and engagement in treatment that are lower than non depressed patients. Either way, the repercussions of suffering from depression while having breast cancer are serious, and may lead to mortality.
Anxiety is also quite common among breast cancer patients, with about one-third of patients being diagnosed with anxiety.[2,32] Studies have shown that both the anxiety and depression are still present one year later, after the end of treatment [32].
Pain
Pain is a common and debilitating symptom in breast cancer patients. Sources of pain in this population include post-operative pain, phantom breast pain and pain associated with the chemotherapy and radiation regimens. A study looking at prevalence reported that 52% of women with breast cancer have pain following breast surgery.[33] A reciprocal relationship is known between sleep and pain;[34] research has shown that sleep disturbance reduces pain thresholds,[35] and that shorter nighttime sleep is associated with increased pain perceptions during the following day.[36] In turn, pain increases the chances of having disrupted sleep.[34] Hence, a vicious cycle of perceiving more pain after a night of disturbed sleep, and sleeping poorly following increased pain can initiate in patients prone to both these conditions such as breast cancer patients.
Treatments
Few pharmacological studies examining the effect of sleeping pills on insomnia and other symptoms have been conducted in patients with cancer and none have looked at the treatment of the full symptom cluster. Although there are eleven drugs currently approved in the United States for the treatment of insomnia, not one has been tested for safety or efficacy in cancer patients. Consequently, no pharmacological treatments have been specifically validated for treatment of the breast cancer cluster symptoms in this population. In a cross-sectional survey of over 900 cancer patients in Israel, the use of a sleeping pill or tranquilizer was reported by 25% and was associated with poorer QOL and increased severity of symptoms, including insomnia, fatigue, pain, dyspnea and constipation. The authors concluded that causal inference was not possible given the cross-sectional design.[37] This reinforces the need to conduct well controlled clinical trials in the best pharmacological treatments for sleep in this group of patients.
There is much debate in the literature about the potential benefits of melatonin as a treatment in cancer patients. Melatonin has not been determined to be an efficacious sleep aid, although it does aid in shifting circadian rhythms. Some investigators have suggested that melatonin might be protective against certain cancer tumors.[38] Additional research is need on the effect of melatonin or other melatonin receptor agonists on sleep, fatigue and other major outcomes of cancer treatment.
Since insomnia in cancer patients may be due to a variety of causes, a multimodal treatment including both pharmacologic and non-pharmacologic therapies is most likely advantageous. A plan that combines attention to sleep hygiene and cognitive-behavioral therapy with prescription of hypnotic medications might help relieve the symptoms of insomnia in cancer patients and improve their quality of life.[10] Several studies have shown improvements in insomnia with cognitive behavioral treatment in breast cancer patients.[39–40]
While there have been no pharmaceutical trials for sleep in cancer patients, there have been several trials for fatigue. A randomized controlled study of modafinil on a group of patients with different cancers found that those with severe fatigue improved but those with mild or moderate fatigue did not.[41] In addition, a randomized controlled trial looking at the effects of the antidepressant paroxetine hydrochloride on breast cancer patients undergoing cancer treatment showed positive effects on mood but not on fatigue levels.[42]
The paucity of studies on the effects of pharmacological palliative treatments in breast cancer patients is somewhat perplexing given the breadth and severity of these symptoms. Limiting factors to this line of research might be the unwillingness of breast cancer patients to engage in more pharmacotherapy because they already feel chemically burdened by the cancer treatment drugs, the negative side effects of the palliative care drugs, and concerns of interactions with cancer treatment agents and/or adjuvant therapies. For example, a recent study reported higher risk of mortality due to breast cancer in older patients receiving adjuvant hormonal cancer treatment with tamoxifen while also using selective serotonin reuptake inhibitors.[43] In addition, that study found that longer concomitant use of these drugs was associated with even greater mortality risk.
There are many studies that looked at the effects of behavioral treatments on the symptom cluster conditions in breast cancer patients. Meta-analytic studies have shown that psychological interventions, including cognitive behavioral interventions, are effective in increasing quality of life, emotional and functional adjustment, and decreasing disease related symptoms in cancer patients.[44,45] A meta-analysis of 20 randomized controlled studies that employed cognitive (e.g., cognitive restructuring, coping skills, problem solving) and/or behavioral techniques (e.g., relaxation, visualization) for distress and/or pain in breast cancer patients revealed that cognitive behavioral treatments are effective in decreasing both pain and distress.[46]
Our laboratory conducted a small randomized controlled study looking at the effects of bright white light therapy compared to a placebo red light therapy on 40 breast cancer patients undergoing chemotherapy. While both groups were fatigued before chemotherapy, the women randomized to the red light had worse fatigue after chemotherapy compared to the women in the white light group who did not report significantly worse fatigue after chemotherapy. The bright white light therapy did not affect other symptoms such as depression or night time sleep, but did increase levels of daytime activity (paper under review). Finally, positive results on quality of life and other symptoms in breast cancer patients have been found using complementary and alternative medicine treatments such as yoga,[47] acupuncture,[48] and meditation.[49]
In summary, across the different breast cancer subpopulations and the different cancer treatments experienced, the most prevalent psychological disorders in women with breast cancer are the sleep problems, fatigue, pain, and depressive and anxiety spectrum disorders.[2] Most often breast cancer patients suffer from more than one symptom simultaneously, i.e., a symptom cluster. There have been no clinical trials of drugs for sleep in cancer. Cognitive behavioral psychotherapies on the other hand, have shown some of the most positive results in alleviating the distressing symptoms that often accompany the breast cancer experience, but even these studies have not targeted the symptom cluster. Other treatments that are promising are bright light therapy for fatigue, and a few complementary and alternative medicine therapies (e.g., yoga, meditation). Despite this array of promising treatments, we are far from having gold-standard ways of treating the distressing symptoms that often plague breast cancer patients.
To fully understand and develop safe and effective treatments, additional research is needed. In particular, mechanistic studies on sleep, fatigue, pain, depression and anxiety are needed not only to understand etiologies, but also to understand more about the relationships among these symptoms and inform new treatment studies. There is research showing that higher clinically relevant pre-treatment symptom clusters are associated with more sleep disturbances, fatigue and depressive symptoms during chemotherapy.[50] Hence, studies exploring new treatments are needed, particularly studies targeting symptom clusters. It is possible that treatments of the cluster of symptoms may be more effective than targeting individual treatments. Pharmacological as well as non-pharmacological treatments need to be explored. It might be that a combined pharmacological and behavioral treatment is most efficacious. In short, substantially more research is needed to fully understand and treat the symptom cluster of insomnia, fatigue, pain, depression and anxiety in breast cancer.
Acknowledgments
Supported by NCI CA112035, UL1RR031980, UCSD Stein Institute for Research on Aging and the Department of Veterans Affairs Center of Excellence for Stress and Mental Health (CESAMH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smigal C, Jemal A, Ward E, Cokkinides V, Smith R, Howe HL, et al. Trends in breast cancer by race and ethnicity: update 2006. CA: a Cancer Journal for Clinicians. 2006;56(3):168–183. doi: 10.3322/canjclin.56.3.168. [DOI] [PubMed] [Google Scholar]
- 2.Kissane DW, Grabsch B, Love A, Clarke DM, Bloch S, Smith GC. Psychiatric disorder in women with early stage and advanced breast cancer: a comparative analysis. Australian and New Zeland Journal of Psychiatry. 2004;38(5):320–326. doi: 10.1080/j.1440-1614.2004.01358.x. [DOI] [PubMed] [Google Scholar]
- 3.Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Medicine Reviews. 2006;10(6):419–29. doi: 10.1016/j.smrv.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savard J, Simard S, Blanchet J, Ivers H, Morin CM. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24(5):583–90. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 5.Berger AM. Patterns of fatigue and activity and rest during adjuvant breast cancer chemotherapy. Oncol Nurs Forum. 1998;25(1):51–62. [PubMed] [Google Scholar]
- 6.Silberfarb PM, Hauri PJ, Oxman TE, Schnurr P. Assessment of sleep in patients with lung cancer and breast cancer. J Clin Oncol. 1993;11(5):997–1004. doi: 10.1200/JCO.1993.11.5.997. [DOI] [PubMed] [Google Scholar]
- 7.Ancoli-Israel S, Liu L, Marler MR, Parker BA, Jones V, Sadler GR, Dimsdale J, Cohen-Zion M, Fiorentino L. Fatigue, sleep, and circadian rhythms prior tochemotherapy for breast cancer. Support Care Cancer. 2006 Mar;14(3):201–209. doi: 10.1007/s00520-005-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sela RA, Watanabe S, Nekolaichuk CL. Sleep disturbances in palliative cancerpatients attending a pain and symptom control clinic. Palliat Support Care. 2005;3(1):23–31. doi: 10.1017/s1478951505050042. [DOI] [PubMed] [Google Scholar]
- 9.Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999;22(3):185–194. doi: 10.1097/00002820-199906000-00001. [DOI] [PubMed] [Google Scholar]
- 10.O’Donnell JF. Insomnia in cancer patients. Clin Cornerstone. 2004;6(Suppl 1D):S6–14. doi: 10.1016/s1098-3597(05)80002-x. [DOI] [PubMed] [Google Scholar]
- 11.Bardwell WA, Profant J, Casden DR, Dimsdale JE, Ancoli-Israel S, Natarajan L, Rock CL, Pierce JP. The relative importance of specific risk factors for insomnia in women treated for early-stage breast cancer. Psychooncology. 2008;17(1):9–18. doi: 10.1002/pon.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Speilman AJ, Glovinsky PB. Case studies in insomnia. In: Hauri PJ, editor. The Varied Nature of Insomnia. New York: Plenum Press; 1991. pp. 1–15. [Google Scholar]
- 13.Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19:895–908. doi: 10.1200/JCO.2001.19.3.895. [DOI] [PubMed] [Google Scholar]
- 14.Fiorentino L, Ancoli-Israel S. Curr Treat Options Neurol. 2007;9(5):337–346. [PMC free article] [PubMed] [Google Scholar]
- 15.Hofman M, Ryan JL, Figueroa-Moseley CD, Jean-Pierre P, Morrow GR. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;2 (1):S4–S10. doi: 10.1634/theoncologist.12-S1-4. [DOI] [PubMed] [Google Scholar]
- 16.Winningham ML, Nail LM, Burke MB, Brophy L, Cimprich B, Jones LS, et al. Fatigue and the cancer experience; the state of the knowledge. Oncology Nursing Forum. 1994;21:23–36. [PubMed] [Google Scholar]
- 17.Bower JE. Behavioral symptoms in patients with breast cancer and survivors. Journal of Clinical Oncology. 2008;26(5):768–77. doi: 10.1200/JCO.2007.14.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ancoli-Israel S, Moore P, Jones V. The relationship between fatigue and sleep in cancer patients: A review. European Journal of Cancer Care. 2001;10:245–255. doi: 10.1046/j.1365-2354.2001.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacobsen PB, Stein K. Is Fatigue a Long-term Side Effect of Breast Cancer Treatment? Cancer Control. 1999;6(3):256–263. doi: 10.1177/107327489900600304. [DOI] [PubMed] [Google Scholar]
- 20.Mormont MC, Waterhouse J, Bleuzen P, Giacchetti S, Jami A, Bogdan A, et al. Marked 24-h rest/activity rhythms are associated with better quality of life, better response and longer survival in patients with metastatic colorectal cancer and good performance status. Clinical Cancer Research. 2000;6:3038–3045. [PubMed] [Google Scholar]
- 21.Lee K, Cho M, Miaskowski C, Dodd M. Impaired sleep and rhythms in persons with cancer. Sleep Medicine Reviews. 2004;8:199–212. doi: 10.1016/j.smrv.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Fernandes R, Stone P, Andrews P, Morgan R, Sharma S. Comparison between fatigue, sleep disturbance, and circadian rhythm in cancer inpatients and healthy volunteers: evaluation of diagnostic criteria for cancer-related fatigue. J Pain Symptom Manage. 2006;32:245–254. doi: 10.1016/j.jpainsymman.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 23.Pati AK, Parganiha A, Kar A, Soni R, Roy S, Choudhary V. Alterations of the characteristics of the circadian rest-activity rhythm of cancer in-patients. Chronobiol Int. 2007;24:1179–1197. doi: 10.1080/07420520701800868. [DOI] [PubMed] [Google Scholar]
- 24.Berger AM, Farr L. The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncology Nursing Forum. 1999;26:1663–1671. [PubMed] [Google Scholar]
- 25.Miller AH, Ancoli-Israel S, Bower JE, Capuron L, Irwin MR. Neuroendocrine-immune mechanisms of behavioral comorbidities in patients with cancer. J Clin Oncol. 2008;26:971–982. doi: 10.1200/JCO.2007.10.7805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moser M, Schaumberger K, Schernhammer E, Stevens RG. Cancer and rhythm. Cancer Causes Control. 2006;17:483–487. doi: 10.1007/s10552-006-0012-z. [DOI] [PubMed] [Google Scholar]
- 27.Savard J, Liu L, Natajaran L, Rissling M, Neikrug AB, He F, et al. Breast cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep. 2009;32:1155–1160. doi: 10.1093/sleep/32.9.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu L, Marler MR, Parker BA, Jones V, Johnson S, Cohen-Zion M, et al. Support Care Cancer, The relationship between fatigue and light exposure during chemotherapy. 2005;12:1010–7. doi: 10.1007/s00520-005-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van’t Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosomatic Medicine. 1997;59(3):280–293. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Bardwell WA, Natarajan L, Dimsdale JE, Rock CL, Mortimer JE, Hollenbach K, et al. Objective cancer-related variables are not associated with depressive symptoms in women treated for early-stage breast cancer. Journal ofClinical Oncology. 2006;24(16):2420–2427. doi: 10.1200/JCO.2005.02.0081. [DOI] [PubMed] [Google Scholar]
- 31.Goodwin JS, Zhang DD, Ostir GV. Effect of depression on diagnosis, treatment, and survival of older women with breast cancer. Journal of the American Geriatric Society. 2004;52(1):106–11. doi: 10.1111/j.1532-5415.2004.52018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montazeri A, Jarvandi S, Hagighat S, Vahdani M, Sajadian A, Ebrahimi M, et al. Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Education and Counseling. 2001;45:195–198. doi: 10.1016/s0738-3991(01)00121-5. [DOI] [PubMed] [Google Scholar]
- 33.Gärtner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–92. doi: 10.1001/jama.2009.1568. [DOI] [PubMed] [Google Scholar]
- 34.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain interrelate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Medicine Reviews. 2004;8:119–132. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 35.Tiede W, Magerl W, Baumgartner U, Durrer B, Ehlert U, Treede RD. Sleep restriction attenuates amplitudes and attentional modulation of pain-related evoked potentials, but augments pain ratings in healthy volunteers. Pain. 2010;148:36–42. doi: 10.1016/j.pain.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 36.Edwards RR, Almeida DM, Klick B, Haythornthwaite JA, Smith MT. Duration of sleep contributes to next-day pain report in the general population. Pain. 2008;137:202–207. doi: 10.1016/j.pain.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paltiel O, Marzec-Boguslawska A, Soskolne V, Massalha S, Avitzour M, Pfeffer R, Cherny N, Peretz T. Use of tranquilizers and sleeping pills among cancer patients is associated with a poorer quality of life. Quality of Life Research. 2004;13:1699–1706. doi: 10.1007/s11136-004-8745-1. [DOI] [PubMed] [Google Scholar]
- 38.Cutando A, Aneiros-Fernández J, Aneiros-Cachaza J, Arias-Santiago S. Melatonin and cancer: current knowledge and its application to oral cavity tumours. J Oral Pathol Med. 2011 Feb 2; doi: 10.1111/j.1600-0714.2010.01002.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 39.Fiorentino L, McQuaid JR, Liu L, Natarajan L, He F, Cornejo M, Lawton S, Parker BA, Sadler GR, Ancoli-Israel S. Individual cognitive behavioral therapy for insomnia in breast cancer survivors: a randomized controlled crossover pilot study. Nature and Science of Sleep. 2009;1:1–8. doi: 10.2147/NSS.S8004. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. Journal of Clinical Oncolology. 2005a;23(25):6083–96. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- 41.Jean-Pierre P, Morrow GR, Roscoe JA, Heckler C, Mohile S, Janelsins M, et al. A phase 3 randomized, placebo-controlled, double-blind, clinical trial of the effect of modafinil on cancer-related fatigue among 631 patients receiving chemotherapy: a University of Rochester Cancer Center Community Clinical Oncology Program Research base study. Cancer. 2010;116(14):3513–20. doi: 10.1002/cncr.25083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roscoe JA, Morrow GR, Hickok JT, Mustian KM, Griggs JJ, Matteson SE, Bushunow P, Qazi R, Smith B. Effect of paroxetine hydrochloride (Paxil) on fatigue and depression in breastcancer patients receiving chemotherapy. Breast Cancer Res Treat. 2005 Feb;89(3):243–9. doi: 10.1007/s10549-004-2175-1. [DOI] [PubMed] [Google Scholar]
- 43.Kelly CM, Juurlink DN, Gomes T, Duong-Hua M, Pritchard KI, Austin PC, Paszat LF. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. British Medical Journal. 2010 Feb 8;:1–8. doi: 10.1136/bmj.c693. published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rehse B, Pukrop R. Effects of psychosocial interventions on quality of life in adult cancer patients: meta analysis of 37 published controlled outcome studies. Patient Education and Counseling. 2003;50(2):179–186. doi: 10.1016/s0738-3991(02)00149-0. [DOI] [PubMed] [Google Scholar]
- 45.Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychology. 1995;14(2):101–108. doi: 10.1037//0278-6133.14.2.101. [DOI] [PubMed] [Google Scholar]
- 46.Tatrow K, Montgomery GH. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. Journal of Behavior Medicine. 2006;29(1):17–27. doi: 10.1007/s10865-005-9036-1. [DOI] [PubMed] [Google Scholar]
- 47.Vadiraja HS, Rao MR, Nagarathna R, Nagendra HR, Rekha M, Vanitha N, et al. Effects of yoga program on quality of life and affect in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Complement Ther Med. 2009;17(5–6):274–80. doi: 10.1016/j.ctim.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 48.de Valois BA, Young TE, Robinson N, McCourt C, Maher EJ. Using traditional acupuncture for breast cancer-related hot flashes and night sweats. Journalof Alternative and Complementary Medicine. 2010;16(10):1047–57. doi: 10.1089/acm.2009.0472. [DOI] [PubMed] [Google Scholar]
- 49.Nidich SI, Fields JZ, Rainforth MV, Pomerantz R, Cella D, Kristeller J, et al. A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integrative Cancer Therapy. 2009;8(3):228–34. doi: 10.1177/1534735409343000. [DOI] [PubMed] [Google Scholar]
- 50.Liu L, Fiorentino L, Natarajan L, Parker BA, Mills PJ, Sadler GR, et al. Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]