Abstract
The incidence of fungal endocarditis in premature infants is on the rise, reported in the last decade secondary to use of central venous lines, the frequent use of broad spectrum antibiotics and neonatal surgical interventions. Central line related thrombosis is a significant risk factor for persistent fungemia and end organ complications including endocarditis. We present a fatal case of progressive thrombosis of the inferior vena cava and right atrial mycetoma in a premature infant with candidemia who underwent ileostomy for bowel perforation. Renal failure occurred secondary to inferior vena cava thrombosis and right atrial mycetoma, both of which had a potential for hemodynamic compromise and embolism.
MeSH: Neonatal candidemia, Endocarditis, Venous thrombosis, Mycetoma
Background
Fungal endocarditis is a rare occurrence in premature infants with more than 50% mortality and significant morbidity regardless type of treatment.1 Candida albicans accounts for two third of fungal endocarditis. Cardiac involvement is found in 15.2% of neonates with candidemia and they usually present with hypotension, bradycardia and acute respiratory distress requiring intubation.2 Right atrial mycetoma (RAM) is reported in only 9% cases of fungal neonatal endocarditis 3 and its management is usually with prolonged use of antifungal therapy in association with surgery in a select group of patients.
Case Report
A preterm male was born at 26 weeks of gestation with a birth weight of 846g by emergency cesarean section for fetal heart rate anomalies and breech presentation.
The newborn had severe respiratory distress syndrome and metabolic acidosis at birth. He was treated with intratracheal surfactant and placed on ampicillin and gentamicin after a sepsis work up. He was treated with ibuprofen on the fifth day of life for symptomatic patent ductus arteriosus. A few hours after the administration of ibuprofen, the baby developed abdominal distension with bluish discoloration and the abdominal x ray showed evidence of intestinal perforation. Antibiotic coverage was started and peritoneal drains were placed. Blood culture grew Pseudomonas aeruginosa and Candida albicans, while peritoneal culture grew Pseudomonas aeruginosa and Enterococcus fecalis. The baby was treated with imipenam and liposomal amphotericin. An ileostomy was done. An echocardiogram performed at this time showed no evidence of endocarditis. Renal sonogram and ophthalmologic evaluation were negative. Repeat blood cultures continued to grow candida despite liposomal amphotericin administered at a dose of 7mg/kg/day.
At 10 days of life, baby began to develop persistent thrombocytopenia requiring platelet transfusions. A Broviac line was placed in the left femoral vein for intravenous antibiotics and antifungal therapy. During the next two weeks, he received a total of 7 units of fresh frozen plasma and 10 units of platelets via this line due to persistent thrombocytopenia and low grade disseminated intravascular coagulation picture. The line was removed on the 24th day of life because of a leak around the insertion site suggestive of loss of patency. Culture of the tip was negative. Caspofungin was added because of persistent fungemia.
At 28 days of life, baby developed progressively worsening oliguria and azotemia. Renal ultrasound showed bilateral abnormal renal echogenicity with reversal of blood flow in both main renal arteries during diastole. An echocardiogram revealed the cause of the renal failure, persistent fungemia and persistent thrombocytopenia. This was a massive echogenic mass in the right atrium extending from the inferior vena cava (Fig. 1).
Fig. 1.

Subcostal short axis view showing large thrombus in inferior vena cava, projecting in to right atrium over tricuspid valve.
The mass in the right atrium moved across the tricuspid valve in diastole and was also in close proximity with the atrial communication (Figs 2 and 3).
Fig. 2.

Large echodensity in right atrium (RAM) which moves across tricuspid valve in diastole.
Fig. 3.

RAM is in close proximity to atrial communication (AC).
The patient was started on heparin. Dialysis could not be done due to the baby's low weight and surgical removal was not feasible due to the low weight and the extreme critical condition of the baby. Doppler study could not demonstrate flow in the inferior vena cava, extending down below the renal veins. The baby died at 40 days of life. Limited autopsy showed a right atrial thrombus and histological staining of the thrombus revealed multiple hyphae mimicking a fungal ball (Fig. 4).
Fig. 4.
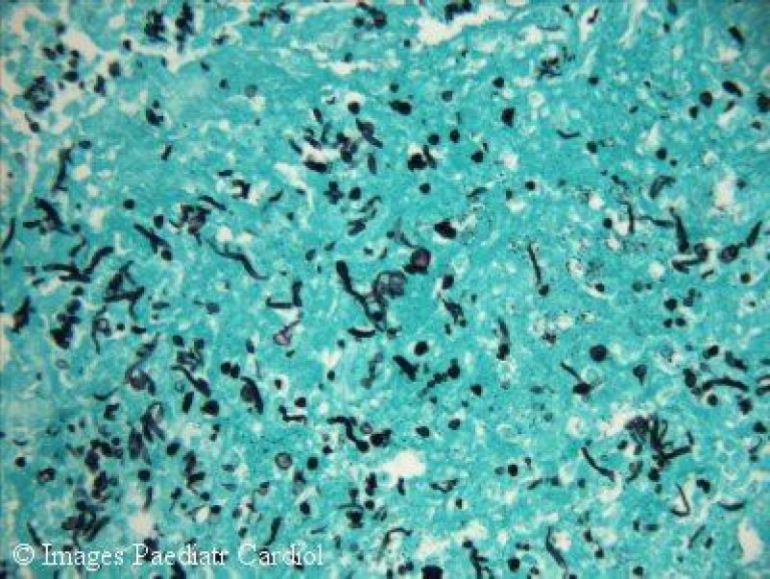
10X magnification of atrial thrombus stained with Grocott's Methenamine Silver stain (GMS) highlight numerous fungal organisms.
Discussion
The reported incidence of candida infection in neonatal intensive care units is about 1% but occurs in 4-15% of extremely low birth weight infants (BW<1kg).1 A positive Candida culture for more than five days is defined as persistent candidemia which is associated with increased risk of endocarditis but not with other complications. 2 Persistent candidemia is often invasive in low birth weight premature infants. Ophthalmologic, renal and cardiac evaluations are routinely done as baseline and should be repeated based upon the clinical course as such complications may influence therapy and outcome.1 Independent of birth weight, infants born at less than 26 weeks or who had abdominal surgery are at a significantly increased risk of candidemia.
The occurrence of fungal endocarditis is on the rise, reported in last decade in infants and children secondary to use of central venous line (CVL), prolonged use of broad spectrum antibiotics and neonatal cardiac surgery.4 CVL is frequently used in supportive care of premature infants for fluids, prolonged antimicrobial therapy and total parenteral nutrition (TPN). Several possible mechanisms by which CVL causes thrombosis include damage to vessel walls, disrupted blood flow, infusion of substances such as TPN that damage endothelial cells and thrombogenic catheter materials. An increased incidence of venous thrombosis is reported with femoral-subclavian CVL compared to brachial -jugular CVL and it does not depend on choice of type, size and duration of CVL.5 A Broviac was placed in left femoral site in our patient due to technical difficulties in the neck and upper extremity. Repeated infusion of platelets to treat persistent thrombocytopenia through this line may have led to local thrombus formation which gradually extended into the inferior vena cava affecting renal blood flow, causing progressive renal failure. Intravascular thrombus was likely seeded with fungus and led to persistent candidiasis for more than three weeks. The clot from the inferior vena cava extended in to the right atrium and became the harbinger of underlying extensive venous thrombosis.
Liposomal amphotericin is generally first line of therapy. Fluconazole is a fungistatic drug, often used in combination with amphotericin in non-neutropenic patients as well in cases of right atrial mycetoma (RAM).6 There is limited data available for the use of caspofungin in cases of fungal endocarditis. Empirical antifungal therapy is recommended in newborns aged less than 25 weeks of gestation, thrombocytopenia and exposure to third generation cephalosporins 7 days prior to blood culture due to the high incidence of mortality and morbidity in this group.7 An active effort should be made to remove CVL in the presence of persistent fungemia. Surgery has a role in a select group of neonates with RAM. Depending upon its size and location, RAM may cause hemodynamic compromise with obstruction of tricuspid inflow and potential for embolism.8 The outcome of RAM is comparable with both medical and surgical treatment. 3,6,8
Persistent candidemia in low birth weight premature infants is a risk factor for endocarditis and demands a thorough and repeated search for a nidus and end organ complications related to the heart, central nervous system and kidneys. RAM complicates the management of fungal endocarditis in the newborn. Despite advances in antifungal agents and cardiac surgical interventions, fungal endocarditis still carries high mortality and morbidity.
References
- 1.Moyola DE, Fernandez M, Moylett E, Baker C. Opthalmologic, visceral and cardiac involvement in neonates with candidemia. Clinic Infec Dis. 2001;32:1018–1023. doi: 10.1086/319601. [DOI] [PubMed] [Google Scholar]
- 2.Levy I, Shalit I, Askenzi S, Klinger G, Sirota L, Linder N. Duration and outcome of persistent candidemia in new born infants. Mycoses. 2006;49:197–201. doi: 10.1111/j.1439-0507.2006.01231.x. [DOI] [PubMed] [Google Scholar]
- 3.Levy I, Shalit I, Birk E, Sirota L, Ashkenzi S, German B, Linder N. Candida endocarditis in neonate :report of five cases and review of literature. Mycoses. 2006;49:43–48. doi: 10.1111/j.1439-0507.2005.01183.x. [DOI] [PubMed] [Google Scholar]
- 4.Tissieres P, Jaeggi ET, Beghetti M, Gervaix A. Increase of fungal endocarditis in children. Infection. 2005;33:267–272. doi: 10.1007/s15010-005-4122-4. [DOI] [PubMed] [Google Scholar]
- 5.Male C, Julian JA, Massicotle P, Gent M, Mitchell Protekt study group. Significant association with location of central venous line placement and risk of venous thrombosis in children. Thrombo Haemosta. 2005;94:516–521. doi: 10.1160/TH03-02-0091. [DOI] [PubMed] [Google Scholar]
- 6.Stripeli F, Tsolia M, Trapali C, Papaevangelou V, Vlachos E, Pasparakis D, Constantopoulos A. Successful medical treatment of candida endocarditis with liposomal amphotericin B without surgical intervention. Eur J Pediatr. 2002;167:469–470. doi: 10.1007/s00431-007-0498-8. [DOI] [PubMed] [Google Scholar]
- 7.Benjamin DK, jr, De Long ER, Steinbach WJ, Cotton CM, Walsh TJ, Clark RH. Empirical therapy for neonatal candidemia in very low birth weight infants. Pediatrics. 2003;112:543–547. doi: 10.1542/peds.112.3.543. [DOI] [PubMed] [Google Scholar]
- 8.Luchiani GB, Casali G, Viscardi F, Marcora S, Prioli MA, Mazzucco A. Tricuspid valve repair in an infant with multiple obstructive candida mycetomas. Ann Thorac Surg. 2005;80:2378–2381. doi: 10.1016/j.athoracsur.2004.07.088. [DOI] [PubMed] [Google Scholar]


