Abstract
Background/Objectives
Geographic variation in racial differences in occurrence of dementia within the US has received little attention despite its importance for generation of new etiologic hypotheses and health disparities research. We test the hypothesis that the geographic pattern of mortality with dementia coded on the death certificate varies by race and racial differences vary by geography in the US.
Design
Analysis of the US multiple cause of death files for 1999–2004.
Setting
United States of America.
Participants
Decedents with dementia coded as underlying or contributing cause of death on the death certificate.
Measurements
Age-adjusted death rates for US Census geographic divisions for blacks and whites aged 65 years and over.
Results
In 1999–2004 the US age-adjusted annual death rate per 100,000 for dementia was 628 in blacks and 647 in whites. The difference between rates in blacks and whites ranged from −130 deaths per 100,000 (−36%) in the Middle Atlantic to +55 (+8%) in the South Atlantic division. Blacks had higher rates in three divisions and whites in five. In the Middle Atlantic and US, blacks were relatively more likely to receive a diagnosis of unspecified dementia/senility (66%) than Alzheimer’s disease (30%) compared to whites (58% versus 41%).
Conclusion
Although overall rates were similar, geographic variation in racial differences in rates of death with dementia occurred among US regions. Further research is needed to assess geographic and racial variation in artifacts of certification versus biological variation as possible causes of variation to enhance utility of mortality data for disease monitoring and health disparities research.
Keywords: Blacks, Aging, Dementia, Mortality, Geography, Alzheimer's Disease
Already a major burden in affluent countries, few doubt that US demographic trends will continue to increase the burden of dementia.1,2 Dementias are projected to be among the top four causes of burden of disease in upper income countries by 2030.3 By 2006, Alzheimer’s disease had become the fifth leading cause of death for persons 65 years and over in the US.4 Many publications have detailed the geographic variation in cerebrovascular mortality in US blacks and whites.5–7 This has led to targeted prevention programs and etiologic studies in the Stroke Belt, the area in the southern US with highest mortality.8,9 However, geographic variation in occurrence of dementia within the US has received little attention despite its importance for targeting intervention, generation of new etiologic hypotheses and health services research. Lower overall dementia prevalence in sub-Saharan Africans than in North American whites or blacks has been reported.1,10–24 We test the hypothesis that the geographic pattern of mortality with dementia coded on the death certificate varies by race and racial differences vary by geography in the US.
MATERIALS AND METHODS
Study population
The resident population of the 50 US states and DC was enumerated in 2000 and estimated for other years between 1999–2004 by the US Bureau of the Census.26 This analysis was restricted to residents who identified their race as white or black/African American. Table 1 shows the average annual population for the period 1999–2004 by race and Census division (defined below).
Table 1.
Number of deaths, population and rate of death per 100,000 with underlying or contributing cause coded as dementia by division and race in persons aged 65 and over: United States 1999–2004
| Division | Race | Death n 65y+ |
Populationn 65y+ |
Crude Rate 65y+ |
Age Adjusted Rate 65y+ |
|---|---|---|---|---|---|
| New England | Black or African American | 1683 | 340854 | 494 | 574 |
| White | 77719 | 10875302 | 715 | 633 | |
| Middle Atlantic | Black or African American | 10145 | 3119034 | 325 | 362 |
| White | 15570 | 28965773 | 538 | 492 | |
| East North Central | Black or African American | 17106 | 2836888 | 603 | 671 |
| White | 21911 | 31040245 | 706 | 664 | |
| West North Central | Black or African American | 3476 | 493880 | 704 | 757 |
| White | 11593 | 14864882 | 780 | 687 | |
| South Atlantic | Black or African American | 37538 | 5553447 | 676 | 731 |
| White | 24081 | 36129123 | 667 | 676 | |
| East South Central | Black or African American | 11422 | 1798196 | 635 | 625 |
| White | 75592 | 1109330 | 681 | 721 | |
| West South Central | Black or African American | 12364 | 2158225 | 573 | 597 |
| White | 11849 | 1829368 | 648 | 676 | |
| Mountain | Black or African American | 1242 | 232688 | 534 | 688 |
| White | 78387 | 1200555 | 653 | 687 | |
| Pacific | Black or African American | 8352 | 1283968 | 650 | 725 |
| White | 18181 | 2507844 | 725 | 683 | |
| U.S. total | Black or African American | 103328 | 1779954 | 581 | 628 |
| White | 1263566 | 188249878 | 671 | 647 |
Outcome data
Data on deaths of US residents were analyzed from the US multiple cause of death files for 1999–2004.26 Each death certificate contains a single underlying cause of death, up to twenty additional multiple causes, and demographic data. The mortality data are based on records for all deaths of white or black residents of the fifty states and the District of Columbia. Deaths to foreign residents and deaths to residents who died abroad were excluded. Unfortunately, Hispanic ethnicity was not available in the version of the 1999–2004 multiple cause file used for this analysis so the analysis includes Hispanic and non-Hispanic whites and blacks.26 Deaths with Alzheimer’s Disease (International Classification of Disease 10th revision [ICD-10] codes G30.0 Alzheimer's disease with early onset; G30.1 Alzheimer's disease with late onset; G30.8 Other Alzheimer's disease; G30.9 Alzheimer's disease, unspecified G30) coded as underlying or contributing cause of death based on the death certificate were enumerated. Also enumerated were vascular dementia (F01.0 Vascular dementia of acute onset; F01.1 Multi-infarct dementia; F01.2 Subcortical vascular dementia; F01.3 Mixed cortical and subcortical vascular dementia; F01.8 Other vascular dementia; F01.9 Vascular dementia, unspecified); Unspecified dementia (F03); and senility (R54).
Geographic categories
US Census divisions, the primary predictor variable in this study, are groups of contiguous states defined by the US Bureau of the Census as shown in Appendix Table A1.26
APPENDIX Table A1.
US Census Bureau Divisions
| Division 1: New England: | Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont |
| Division 2: Middle Atlantic: | New Jersey, New York, Pennsylvania |
| Division 3: East North Central | Illinois, Indiana, Michigan, Ohio, Wisconsin |
| Division 4: West North Central | Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, South Dakota |
| Division 5: South Atlantic | Delaware, District of Columbia, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, West Virginia |
| Division 6: East South Central | Alabama, Kentucky, Mississippi, Tennessee |
| Division 7: West South Central | Arkansas, Louisiana, Oklahoma, Texas |
| Division 8: Mountain | Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming |
| Division 9: Pacific | Alaska, California, Hawaii Oregon, Washington |
Analysis and statistics
Age-adjusted death rates per 100,000 (using the 2000 US standard population) were computed by US Census division for persons aged 65 years and over using standard methods documented elsewhere.26 Rates were considered unreliable when based on fewer than 20 deaths. In order to ensure adequate numbers of deaths for blacks in every geographic unit, data were combined for six years and divisions rather than states or counties were examined. The 95% confidence intervals (CI) for rates were computed using standard methods.26 Distribution of deaths between diagnosis groups by race was assed by Chi Square test (Table 2).
Table 2.
Specific versus non-specific diagnoses of dementia by ethnicity in the US and the Mid-Atlantic Division in 1999–2004
| White | Black | |||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| US | ||||
| Specific* | 506,674 | 39 | 34,596 | 33** |
| Non-specific+ | 783,172 | 61 | 70,613 | 67 |
| Mid-Atlantic | ||||
| Specific | 59,703 | 38 | 3,149 | 31** |
| Non-specific | 98,164 | 62 | 7,137 | 69 |
ICD-10 G30, F01
ICD-10 F03, R54
P<0.01
RESULTS
In 1999–2004 the age-adjusted rate of death with dementia per 100,000 at ages 65 years and over was 628 in blacks and 647 in whites. The rate was higher in blacks than whites at age 65–74 and 75–84: 65–74y blacks 108 (95% CI = 106–110), whites 73 (95% CI = 73–74) and 75–84 y blacks 648 (95% CI = 641–654), whites 591 (95% CI = 589–593). The rate was lower in blacks age 85 and over: blacks 2,780 (95% CI = 2,757–2,803), whites 3,249 (95% CI = 3,242–3,257). The pattern of variation in rates by US Census geographic division differed between blacks and whites (Table 1). The rates for blacks were highest in the South Atlantic and West North Central divisions and lowest in New England and Middle Atlantic division, whereas rates for whites were highest in the East South Central division and lowest in New England, Middle Atlantic and East North Central divisions.
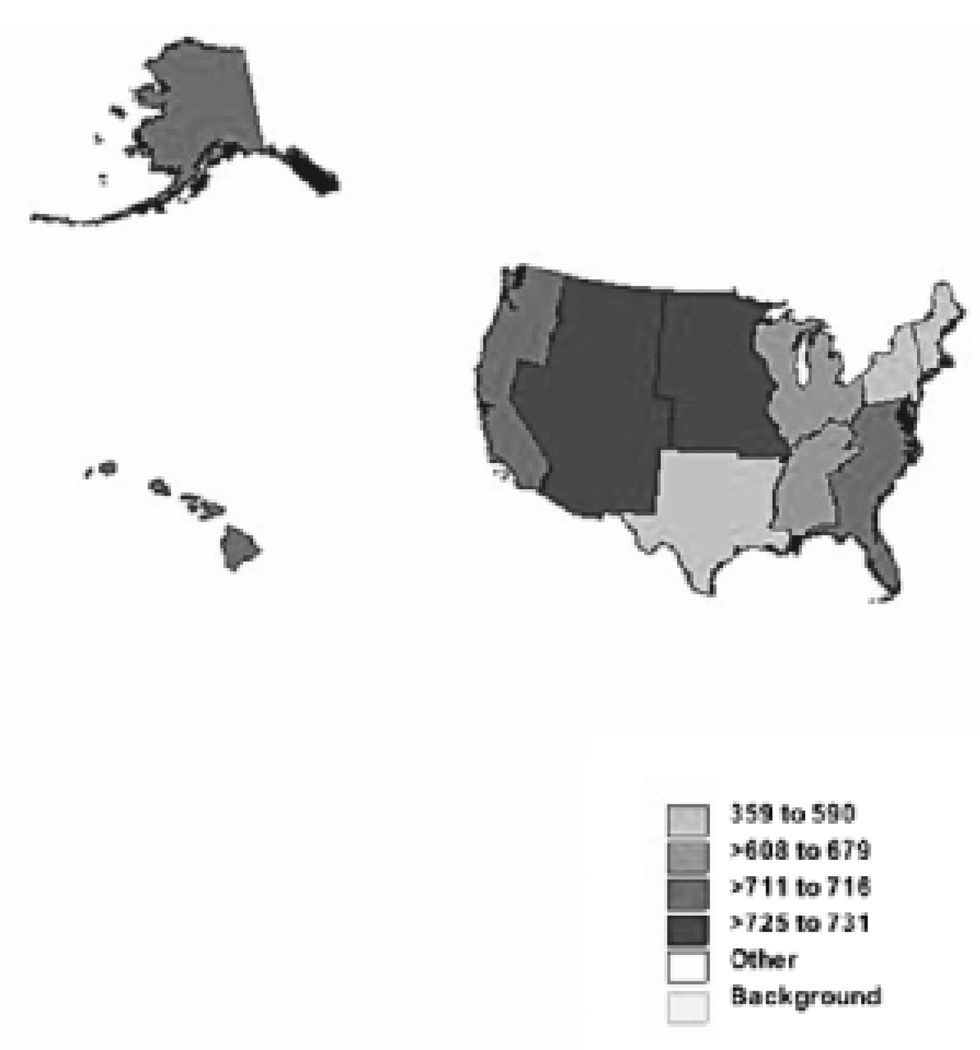
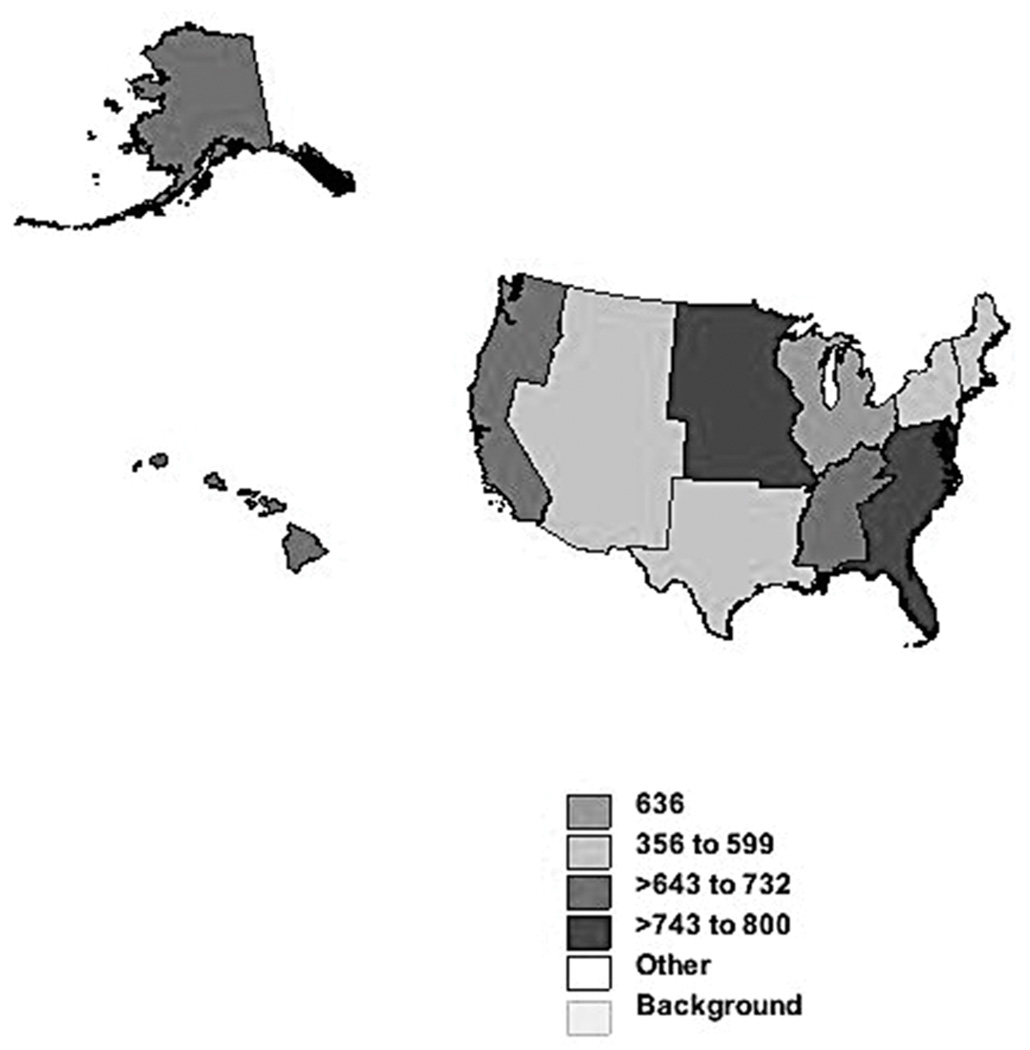
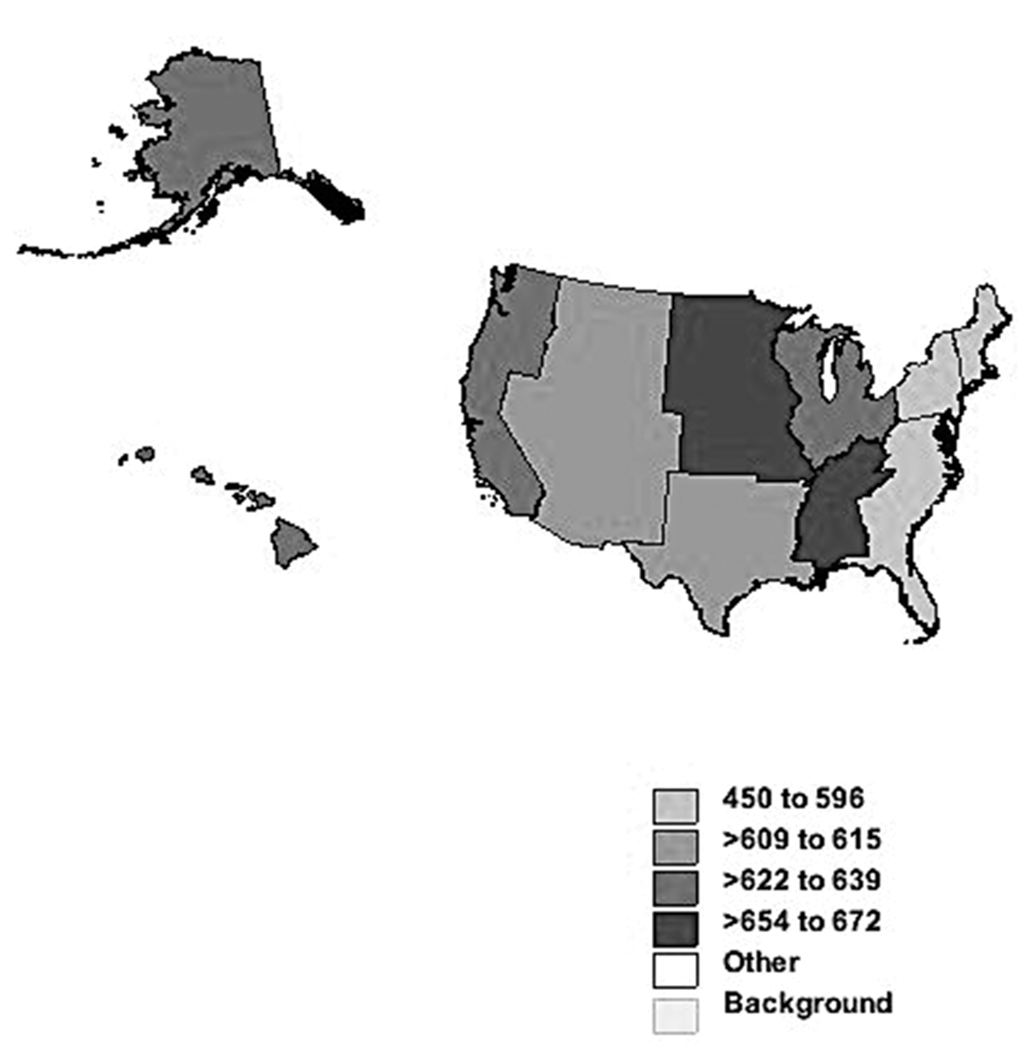
Gender-specific analyses of age-adjusted rates also were done to eliminate possible confounding by gender (Figures 1 and 2). Among black women (age-adjusted US rate 618 per 100,000), rates were highest in Mountain and West North Central divisions and lowest in West South Central, New England and Middle Atlantic divisions. Among white women (US rate 668) rates were highest in Mountain and East South Central divisions and lowest in New England, Middle Atlantic and East North Central divisions. Among black men (not shown, US rate 629), the pattern was similar to that of black women with a few exceptions; rates were highest in West North Central and South Atlantic divisions and lowest in Mountain, West South Central, New England and Middle Atlantic divisions. Among white men (not shown, US rate 593), the pattern was similar to white women; rates were highest in West North Central and East South Central divisions and lowest in New England, Middle Atlantic and South Atlantic divisions. (Maps for men are available from authors upon request).
Figure 1.
Age-adjusted rate of death per 100,000 with any mention of dementia by US Census division for black women aged 65 years and over: United States, 1999–2004. Map legend: light gray 359–590, medium light gray 608–679, medium dark gray 711–716, dark gray 725–731.
Figure 2.
Age-adjusted rate of death with any mention of dementia by US Census division for white women aged 65 years and over: United States regions, 1999–2004. Map legend: light gray 356–599, medium light gray 635–637, medium dark gray 643–732, dark gray 743–800.
As shown in Table 1, the difference in age-adjusted death rates between blacks and whites also varied by region and ranged from −130 deaths per 100,000 (−36%), i.e. higher rates in whites, in the Middle Atlantic to +55 (+8%) in the South Atlantic division, i.e. higher rates in blacks. Blacks had higher rates in three divisions and the whites in five (Table 1). Confidence intervals were narrow and generally non-overlapping. For example in women aged 75–84, whites had significantly higher rates in the Middle Atlantic division: black women 345 (95% CI = 331–359), white women 430 (95% CI = 425–435); but blacks had higher rates in the South Atlantic division: black women 708 (95% CI = 692–723), white women 625 (95% CI = 619–631).
To assess the extent to which racial variation in geographic patterns might be attributed to diagnostic practices, the numbers of deaths with codes for specific dementias (i.e. Alzheimer's disease or vascular dementia) versus nonspecific dementia were compared in the US and in the Mid-Atlantic division, where the racial difference was greatest (Table 2). In the Middle Atlantic and US compared to whites, blacks were relatively more likely to receive a diagnosis of unspecified dementia or senility than of Alzheimer’s disease or vascular dementia (p<0.01). Specific diagnoses were slightly less likely in the Middle Atlantic division than in the US for both races (p<0.01).
DISCUSSION
This analysis of data from the US multiple cause files is the first to our knowledge to establish geographic patterns by race for death with Alzheimer’s disease and other dementias. The rates for blacks were highest in the South Atlantic and West North Central divisions and lowest in New England and Middle Atlantic division, whereas rates for whites were highest in the East South Central division and lowest in New England, Middle Atlantic and East North Central divisions. Blacks had lower rates than whites in the Middle Atlantic and higher rates in the South Atlantic division; blacks had higher rates in three divisions and whites in five. In whites, women had a 13 per cent higher US rate than men whereas in blacks rates were similar. Among women the most striking racial difference was in the West South Central division while in men it was in the South Atlantic (Figures). Among blacks the most striking gender difference was in the Mountain division while in whites it was in the South Atlantic division.
Although this study could not directly address possible causes of these variations, data presented may shed light on the possible role of making and reporting diagnoses. In the Middle Atlantic and US, blacks were more likely to receive a diagnosis of unspecified dementia than Alzheimer’s disease compared to whites. This suggests that diagnostic practice varies by geographic area and by race. Possible explanations include variation in diagnostic custom and access to diagnostic technology. Since the Middle Atlantic division had the lowest death rates for either race and the lowest rates for blacks relative to whites and also had the lowest proportion of specific dementia diagnoses, one might hypothesize that death rates there may be understated compared to other divisions due to failure to record dementia on the death certificate in persons dying with dementia. Racial and geographic differences in failure by certifiers to mention chronic dementia at all on death certificates could not be addressed with vital statistics data.
Racial variation in mortality with dementia should be explained by variations in disease prevalence, a function of incidence and duration. Consistent with similar levels of mortality in blacks and whites presented here, a few studies have failed to find racial differences in unadjusted prevalence and incidence of dementia.16 But in contrast to the similar mortality rates presented here, most other reports suggest a higher prevalence and incidence in US blacks than in US whites.14, 15, 17–23. However, much of any excess incidence in blacks was explained by a protective effect of greater education among whites. Greater survival after onset of dementia in blacks than whites suggested in some studies but not others might have variable effects on relative mortality, perhaps decreasing rates in blacks at younger ages but increasing rates in blacks at older ages.25 Explanations for greater survival after diagnosis in blacks, if true, are lacking.12 A similar proportion of prevalent cases were classified as Alzheimer’s disease in US blacks and whites in several studies.14,15 However, a much higher incidence and prevalence of dementia and greater proportion attributed to Alzheimer’s disease (about three quarters) has been reported among US blacks than West Africans, likely due to environmental factors.1, 10–11
High population prevalence could result in higher death rates with dementia in east south central states (whites) or south Atlantic states such as the Carolinas (blacks) as compared to Mid-Atlantic states. This could result from more sophisticated or accessible care resulting in longer survival with the disease, higher incidence, or both in the former compared to the latter. Cardiovascular risk factors such as hypertension have been hypothesized to be risk factors for Alzheimer’s and other dementia, possibly affecting incidence.15 Interestingly, in blacks geographic patterns of stroke mortality are rather different from those for dementia in 1999–2004, with relatively low rates in the Middle Atlantic, high rates in the West South Central and high rates in the Pacific. However, in whites 1999–2004 rates were high in East South Central and low in New England and Middle Atlantic for both diagnoses. Further an analysis of trends in stroke mortality predicted that Oregon and Washington, Pacific states, would rise greatly in relative ranking consistent with dementia patterns in whites.5 Similarly, patterns of ischemic heart disease mortality differed from those of dementia in blacks; highest rates were in the East North Central and Pacific divisions and lowest in the East South Central.6 Unlike dementia, ischemic heart disease mortality in whites was high in the Middle Atlantic and West South Central, and low in New England and Mountain divisions.6 But birth in states of the Stroke Belt was associated with excess dementia mortality in a recent analysis.24 These observations are not consistent with dementia variation being explained mainly by cardiovascular risk factors or co-morbidity. However, competing mortality from cardiovascular causes may lead to lower dementia mortality in areas with high cardiovascular death rates. Further, if healthy elderly whites are more likely to move from New York to Florida than healthy blacks, migration could contribute to observed racial differences in these areas.27,28
Strengths and limitations. Strengths of this study include the lack of previous studies, the use national mortality data with their ready annual availability for divisions, states and counties, near complete coverage of the population, and enhanced diagnostic specificity with introduction of ICD-10 in 1999. Analysis of divisions rather than smaller units allowed nationwide comparisons by race and gender with adequate numbers of deaths for blacks in every geographic unit (not the case for states or counties). Limitations, stated or implied above, include diagnostic inaccuracy resulting in under-ascertainment of specific conditions at death.29 Multiple-cause data were used to reduce tendency of underlying cause data to underestimate the role of chronic conditions such as dementia on mortality due to recording only immediate causes such as pneumonia and cardiovascular disease on the death certificate. Even so, the large proportion of deaths with non-specific dementia diagnoses, many likely Alzheimer’s disease or vascular dementia, led us to aggregate deaths into one broad category for most analyses, since such misclassification would not bias such results. We did not venture to present analyses for Alzheimer’s disease or vascular dementia alone, since diagnostic misclassification would likely bias results. Unfortunately, Hispanic ethnicity was not available in the version of 1999–2004 multiple cause file that we used.26 Therefore the effect on dementia rates of including most Hispanics among whites could not be assessed. Failure by certifiers to mention chronic dementia at all on death certificates of certain groups in certain locations more than others could also contribute to geographic variation. However, this could not be assessed with available data. When death rates are computed, inaccuracies of population counts and estimates can limit the utility of data. This may affect the black more than the white population. However, every attempt is made by the U.S. Bureau of Census to understand and compensate for known problems. We did not include data here for 2005–2006 because of well-known geographic shifts of the Alabama, Louisiana, Mississippi, and Texas populations resulting from Hurricanes Katrina and Rita in 2005, which affected blacks more than others.26
CONCLUSION
Geographic variation in rates of death with dementia occurred among US regions in blacks and whites. Further research is needed to assess artifacts of certification versus biological variation as possible causes of variation to enhance utility of mortality data for disease monitoring and research. Data from multicenter studies of dementia in population-based samples of the US elderly population with validation of death-certificate diagnoses and estimation of incidence, survival and prevalence are needed to establish the magnitude and causes of racial and geographic variation in dementia mortality.
ACKNOWLEDGMENTS
Dr. Obisesan was supported by career development award # AG00980 and research award #RO1-AG031517 from the National Institute on Aging and research award #1UL1RR031975-01 from the National Center for Research Resources.
Sponsor’s Role
The funder had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest
The authors have no competing interests to declare.
Authors’ contributions
RG and TO made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data and were involved in drafting the manuscript and revising it critically for important intellectual content and have given final approval of the version to be published. Both authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Hsiung GR. Epidemiology of Alzheimer’s disease and dementia. In: Feldman HH, editor. Atlas of Alzheimer’s disease. London: Informa UK Ltd; 2007. pp. 27–40. [Google Scholar]
- 2.Dekosky ST, Lopez OL. Alzheimer’s disease. In: Growdon JH, Rossor MN, editors. The dementias 2. Philadelphia: Butterworth Heinemann/Elsevier; 2007. pp. 33–58. [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health, United States, 2009. Hyattsville, Maryland: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 5.Howard G, Howard VJ, Katholi C, et al. Decline in US stroke mortality: An analysis of temporal patterns by sex, race, and geographic region. Stroke. 2001;32:2213–2220. doi: 10.1161/hs1001.096047. [DOI] [PubMed] [Google Scholar]
- 6.Pickle LW, Gillum RF. Geographic variation in cardiovascular disease mortality in US blacks and whites. J Natl Med Assoc. 1999;91:545–556. [PMC free article] [PubMed] [Google Scholar]
- 7.Obisesan TO, Vargas CM, Gillum RF. Geographic variation in stroke risk in the United States. Region, urbanization, and hypertension in the Third National Health and Nutrition Examination Survey. Stroke. 2000;31:19–25. doi: 10.1161/01.str.31.1.19. [DOI] [PubMed] [Google Scholar]
- 8.Okwumabua JO, Martin B, Clayton-Davis J, et al. Stroke Belt initiative: The Tennessee experience. J Health Care Poor Underserved. 1997;8:292–299. doi: 10.1353/hpu.2010.0598. [DOI] [PubMed] [Google Scholar]
- 9.Howard G, Prineas R, Moy C, et al. Racial and geographic differences in awareness, treatment, and control of hypertension: The REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 10.Ferri CP, Prince M, Brayne C, et al. Alzheimer's Disease International. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogunniyi A, Hall KS, Gureje O, et al. Risk factors for incident AD in African Americans and Yoruba. Metab Brain Dis. 2006;21:235–240. doi: 10.1007/s11011-006-9017-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes LL, Wilson RS, Li Y, et al. Change in cognitive function in AD in African-American and white persons. Neuroepidemiology. 2006;26:16–22. doi: 10.1159/000089231. [DOI] [PubMed] [Google Scholar]
- 13.Obisesan TO. Hypertension and cognitive function. Clin Geriatr Med. 2009;25:259–288. doi: 10.1016/j.cger.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green RC, Cupples LA, Go R, et al. MIRAGE Study Group. Risk of dementia among white and African American relatives of patients with Alzheimer disease. JAMA. 2002;287:329–336. doi: 10.1001/jama.287.3.329. [DOI] [PubMed] [Google Scholar]
- 15.Fitzpatrick AL, Kuller LH, Ives DG, et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. J Am Geriatr Soc. 2004;52:195–204. doi: 10.1111/j.1532-5415.2004.52058.x. [DOI] [PubMed] [Google Scholar]
- 16.Fillenbaum GG, Heyman A, Huber MS, et al. The prevalence and 3-year incidence of dementia in older black and white community residents. J Clin Epidemiol. 1998;51:587–595. doi: 10.1016/s0895-4356(98)00024-9. [DOI] [PubMed] [Google Scholar]
- 17.Hendrie HC, Osuntokun BO, Hall KS, et al. Prevalence of Alzheimer's disease and dementia in two communities: Nigerian Africans and African Americans. Am J Psychiatry. 1995;152:1485–1492. doi: 10.1176/ajp.152.10.1485. [DOI] [PubMed] [Google Scholar]
- 18.Heyman A, Fillenbaum G, Prosnitz B, et al. Estimated prevalence of dementia among elderly black and white community residents. Arch Neurol. 1991;48:594–598. doi: 10.1001/archneur.1991.00530180046016. [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Bassett SS, Anthony JC, et al. Dementia: Case ascertainment in a community survey. J Gerontol. 1991;46:M132–M138. doi: 10.1093/geronj/46.4.m132. [DOI] [PubMed] [Google Scholar]
- 20.Tang MX, Cross P, Andrews H, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56:49–56. doi: 10.1212/wnl.56.1.49. [DOI] [PubMed] [Google Scholar]
- 21.Manly J, Mayeaux R. Ethnic differences in dementia and Alzheimer’s disease. In: Anderson NB, RA Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 22.Yeo G. Prevalence of dementia in different ethnic populations. In: Yeo G, Gallagher-Thompson D, editors. Ethnicity and the Dementias. 2nd Ed. Sudbury, MA: Taylor and Francis; 2006. [Google Scholar]
- 23.Shadlen MF, Siscovick D, Fitzpatrick AL, et al. Education, cognitive test scores, and black-white differences in dementia risk. J Am Geriatr Soc. 2006;54:898–905. doi: 10.1111/j.1532-5415.2006.00747.x. [DOI] [PubMed] [Google Scholar]
- 24.Glymour MM, Kosheleva A, Wadley VG, et al. Geographic distribution of dementia mortality: elevated mortality rates for Black and White Americans by Place of Birth. Alzheimer Dis Assoc Disord. 2011 Feb 2; doi: 10.1097/WAD.0b013e31820905e7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson RS, Aggarwal NT, Barnes LL, et al. Biracial population study of mortality in mild cognitive impairment and Alzheimer’s disease. Arch Neurol. 2009;66:767–772. doi: 10.1001/archneurol.2009.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death File 2005–2006. CDC WONDER On-line Database, compiled from Multiple Cause of Death File 2005–2006 Series 20 No. 2L. 2009 Accessed at http://wonder.cdc.gov/mcd-icd10.html on Nov 23, 2010 1:53:42 PM.
- 27.Conway KS, Rork JC. "Going with the flow"--a comparison of interstate elderly migration during 1970–2000 using the (I)PUMS versus full census data. J Gerontol B Psychol Sci Soc Sci. 2010;65:767–771. doi: 10.1093/geronb/gbp135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith SK, House M. Snowbirds, sunbirds, and stayers: Seasonal migration of elderly adults in Florida. J Gerontol B Psychol Sci Soc Sci. 2006;61:S232–S239. doi: 10.1093/geronb/61.5.s232. [DOI] [PubMed] [Google Scholar]
- 29.Hoyert DL. Mortality trends for Alzheimer's disease, 1979-91. Vital Health Stat 20. 1996;28:1–23. [PubMed] [Google Scholar]