Abstract
Oxidative stress is commonly associated with a number of liver diseases and is thought to play a role in the pathogenesis of chronic hepatitis C, alcoholic liver disease, nonalcoholic steatohepatitis (NASH), hemochromatosis and Wilson’s disease. Antioxidant therapy has thus been considered to have the possibility of beneficial effects in the management of these liver diseases. In spite of this promise, antioxidants have produced mixed results in a number of clinical trials of efficacy. This review summarizes the results of clinical trials of antioxidants as sole or adjuvant therapy of chronic hepatitis C, alcoholic liver disease and NASH. Overall, the most promising results to date are for vitamin E therapy of NASH but some encouraging results have been obtained with antioxidant therapy of acute alcoholic hepatitis as well. In spite of evidence for small reductions of serum ALT, there is as yet no convincing evidence that antioxidant therapy itself is beneficial to patients with chronic hepatitis C. Problems such as small sample size, short follow up duration, inadequate end points, failure to demonstrate tissue delivery and antioxidant efficacy, and heterogeneous nature of the “antioxidant” compounds used have complicated interpretation of results of the clinical studies. These limitations and their implications for future trial design are discussed.
Keywords: Antioxidants, Oxidative stress, Hepatitis C, NAFLD, NASH, Alcoholic liver disease, Vitamin E, N-acetylycysteine
INTRODUCTION
Oxidative stress is a commonly used term that refers to a state in which tissue and cellular redox balance is altered towards a more oxidizing environment (1, 2) and an ensuing adaptation of cellular functions occurs. While some of the consequences of oxidative stress result from irreversible chemical modification of proteins, lipids and nucleic acids, many more result from alterations in signaling pathways triggered by specific changes in redox sensitive trigger molecules that initiate downstream signaling pathways. Pathways controlling cell death, gene transcription, inflammation, and stellate cell activation are all under redox dependent control (3, 4). In this case, oxidative stress can be considered just one of many environmental situations for which cells have evolved complex homeostatic responses.
Oxidative stress begins with the generation of reactive oxygen species (ROS) and reactive nitrogen species (RNS) as a part of normal cellular function (1). There are multiple cellular sources of ROS generation but the most significant ones are the mitochondrial electron transport complexes I and III, P450 enzymes within the ER, membrane bound NADPH oxidase and peroxisomes. ROS production by each of these sources can be stimulated by cytokines, inflammation, viral proteins and other mechanisms. These processes initially generate superoxide which is sequentially reduced to form hydrogen peroxide, hydroxyl radical, and ultimately water. These reactive intermediates, however, interact with other molecules to form secondary reactive oxygen species, such as lipid peroxidation products, peroxynitrite, and sulfenic acid and disulfides (4). These processes are illustrated in Fig. 1.
Figure 1. Reactive oxygen and nitrogen species effect.
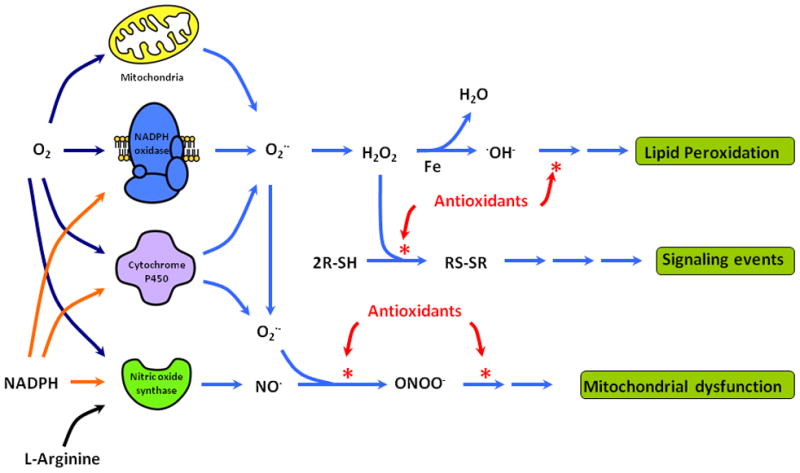
On the left the figure schematically represents the major sources of ROS and RNS production in the liver. The immediate products of these sources, superoxide and nitric oxide, undergo a series of subsequent reductions and interaction that lead to lipid peroxidation, formation of disulfides which trigger a number of singnaling events, and reduction of mitochondrial respiration with a further increase in mitochondrial ROS production. Antioxidant compounds such as vitamin C and vitamin E can act as free radical scavengers inhibiting the progression of these pathways.
The reactions that generate these compounds all result from the fact that the intracellular environment sits at a much more reducing redox potential than that of the Earth’s atmosphere. There is thus a constant and inevitable transfer of electrons from intracellular molecules to molecular oxygen. It takes 4 electrons to reduce oxygen to the stable compound, water and thus the intermediate partially reduced 1, 2 and 3 electron transfers produce the variably reactive compounds superoxide anion, hydrogen peroxide, and hydroxyl radical, respectively. These in turn can oxidize thiol groups leading to disulfide formation, react with nitric oxide to produce the strong oxidizing agent peroxynitrite, initiate self perpetuating cascades of lipid peroxidation, and cause oxidative modification of amino acid side chains in proteins and bases in nucleic acids (5). Many of these reactions, but particularly the formation of disulfides, are the triggers for specific signaling reactions such as activation of MAP kinase cascades and transcription factors. When ROS and RNS are abundant, they cause alternations in mitochondrial functions, modulate cytokine expression, alter immune responses, and activate signaling cascades resulting in hepatocellular injury, apoptosis or cell death, and liver fibrosis (1, 6, 7).
Cellular mechanisms to control oxidative stress are critical to cellular homeostasis. These include enzyme systems such as catalase, superoxide dismutases, peroxiredoxins, glutathione peroxidase and a number of thiol reductases that are ultimately linked to either NADH or NADPH as the source of reducing equivalents (8). Non-enzymatic electron receptors such as vitamin E, vitamin C, and glutathione (9) also play a major role in the cellular response to oxidative stress (1, 2).
Oxidative stress, to some extent, is seen in most diseases and certainly all inflammatory diseases. Liver disease is no exception in this case (4). Many liver diseases have high levels of ROS and RNS with substantial evidence that the magnitude of oxidative protein and lipid modifications correlates with disease severity and is also linked to disease progression (1, 4). This has led to an enthusiasm for the possibility of antioxidant therapy in liver diseases.
ANTIOXIDANT THERAPY OF LIVER DISEASES
One of the major problems in interpretation of studies attempting to show a benefit of antioxidant therapy of liver disease is the inability to know the exact mechanisms of action of specific compounds labeled “antioxidants”. Many plant derived compounds demonstrate in vitro and even in vivo antioxidant capacity but these effects may not be responsible for their biological activity. Of the various available antioxidants, strong evidence exists that several agents mediate their action primarily based on changes in ROS and redox state of the cell. These agents include vitamins E and C, N-acetylcysteine (NAC), mitoquinone (mitoq), and polyenylphosphatidylcholine (PPC). Other compounds, such as Silymaryin, S-adenosyl methionine, and betaine have additional prominent non-antioxidant effects that may be responsible for their clinical effects.
Vitamin E (tocopherol) serves as an antioxidant by complexing with unpaired electrons thus stabilizing these free radical compounds and preventing lipid peroxidation (10). Some effects observed include a decrease in production of tumor necrosis factor (TNF) in alcoholic hepatitis (11), and prevention of hepatic stellate cell (HSC) activation in chronic hepatitis C (12). Alpha tocopherol accounts for almost 90% of the total vitamin E in the human tissues. Vitamin C or ascorbic acid serves as an electron donor and thus can terminate free radical chain reactions. Similar to vitamin E, however, its ability to serve as an electron donor makes it possible for it to actually generate free radicals when at high concentrations in the presence of metal ions (13). NAC acts by increasing hepatic GSH levels, and serving as a free thiol itself. It is widely used for the treatment of acetaminophen overdose (14). As the only member of this group that is itself a reduced thiol, it has unique potential to augment GSH levels and drive protein thiol redox reactions to the reduced form. PPC, an extract of soybeans, is another compound that has been evaluated as a therapy for alcoholic liver disease. It also has lipid peroxidation chain breaking activity and may inhibit ROS generating enzymes (15, 16). Mitoquinone (MitoQ), a mitochondrially-targeted antioxidant consists of a quinone moiety linked to triphenylphosphonium by a carbon alkyl chain. Its resulting positive charge and lipophillic nature allow it to accumulate in the mitochondrial matrix and inner mitochondrial membrane. (17) This review will serve to examine the studies in which these antioxidants have been used to treat liver diseases with an aim to critically analyze and assess their current status. We will also discuss briefly those antioxidants where an antioxidant effect may be one of the mechanisms of action such as zinc, silymarin, herbal drugs, S-adenosylmethionine, and betaine. Although, oxidative stress has been shown to exist in almost every liver disease, we will limit this discussion to liver diseases for which there is maximum evidence for its participation in the disease mechanism. These include chronic hepatitis C virus infection (CHC), alcoholic liver disease, and non-alcoholic fatty liver disease with or without non-alcoholic steatohepatitis.
HEPATITIS C VIRUS INFECTION
Evidence of oxidative stress in hepatitis C
Existence of oxidative stress in chronic hepatitis C is well documented with an increase in oxidized protein and nucleic acid markers and a decrease in antioxidant levels(18–21). Oxidative stress in these patients occurs early in the disease and increases with disease severity (22). Studies have shown levels of oxidative stress markers to correlate with disease severity, HCV RNA, iron overload, and insulin sensitivity(18, 19, 23, 24). Oxidative stress has also been shown to be an early event in carcinogenesis and is a risk factor for development of HCC in patients with CHC (25). Evidence linking HCV infection itself as the cause of oxidative stress was provided by studies showing correlation of oxidative stress with response to IFN treatment and normalization of oxidative stress after viral eradication (26, 27). Existence of mitochondrial dysfunction and oxidative stress has been shown in a number of cell culture models of HCV infection. It results from a combination of viral effects on mitochondria, endoplasmic reticulum, and NADPH oxidase (28, 29). The process has been shown to be calcium dependent and can be prevented by calcium chelating agents (30). However, lack of a readily available small animal model for HCV has precluded pre-clinical assessment of antioxidants for HCV infection.
Clinical trials
Standard treatment for HCV infection is the combination of pegylated interferon and ribavirin (RBV). The aim of treatment is to achieve sustained virologic response (SVR) defined as negative HCV RNA 6 months after completion of treatment. With this regimen, SVR is reported to occur in only 40–50% of patients with genotypes 1 or 4 infections and 60–70% of genotypes 2 or 3 infections (31). Therefore, there is a need for newer drugs to supplement the standard treatment in order to improve treatment efficacy or reduce disease progression in patients who fail to achieve SVR. In this respect, antioxidants have been evaluated in CHC patients.
Agents with antioxidant effect as the main mechanism of action
Vitamin E, Vitamin C and mitoQ
A series of studies have examined the effectiveness of antioxidants in the treatment of CHC patients who have either failed or cannot be treated with interferon based therapy. In a very small open label study on 6 CHC patients refractory to IFN, vitamin E supplementation (1200 IU/d) for 8 weeks prevented the fibrogenesis cascade as reflected by decreased malonaldehyde levels and decreased activation of hepatic stellate cells. However, there was no effect on liver enzymes, HCV RNA, and liver histology (12). In another study, vitamin E supplementation (500 mg/d) for 3 months in 17 CHC patients resulted in modest reduction of serum ALT levels to 63 IU/l from baseline levels of 73 IU/l. the effect was significant only for the subgroup of patients with baseline levels > 70 IU/l (reduction from 86 to 71 IU/l). This was associated with reduction of oxidative stress with decrease in thioredoxin levels from 59 to 40 ng/ml at the end of treatment. The effect was partially maintained as the ALT returned back to 74 IU/l and thioredoxin levels to 48 ng/ml 1 month after treatment was stopped (32). Similar results were reported in another study with a prospective randomized double blind cross over design in 23 CHC patients who were refractory to IFN. Vitamin E supplementation (800 IU/d) for 12 weeks reduced serum ALT from 90 to 68 IU/l at the end of treatment. However, within a month of discontinuing vitamin E treatment, serum ALT levels returned to 91 IU/l. Re-treatment with 3 months of vitamin E supplementation of responders (decrease in ALT by at least 35%) reduced ALT again (from 93 to 50 IU/l) (33). One study using 600 mg alpha-tocopherol in 83 HCV cirrhotics showed a trend for improved hepatocellular cancer free survival at 5 years as compared to untreated patients (80% vs. 61%; P=0.07) (34).
These studies suggested a small beneficial effect of vitamin E alone but the clinical importance of these results is uncertain. Subsequently several studies examined combination of antioxidants (35–37) as primary therapy. In a phase 1 clinical trial, 50 CHC patients were prospectively treated with a cocktail of antioxidants including vitamin E for 20 weeks. At the end of treatment antioxidant treatment resulted ALT normalization in 48%, negative HCVRNA in 25%, and histological improvement in 36% with improved quality of life scores in 58% of patients (35). With these encouraging results, a larger placebo controlled RCT was performed on 100 CHC patients refractory to previous IFN treatment to study the effect of antioxidant cocktail (oral and intravenous in 50 and only oral in 50 patients). At week 24, when examined as proportion of patients improving, oral and intra-venous supplementation as compared to placebo resulted in a trend toward improvement in liver enzymes (52% vs. 20%; P=0.05), histology (48% vs. 26%; P=0.21), and HCVRNA (28% vs. 12%; P=NS). However, when quantitative values were examined even these effects were quite minimal with mean ALT changing only from 78 to 65 IU/l, mean AST change from 80 to 62 IU/l, mean histology activity index change from 8.9 to 8.1, and mean HCVRNA titers changing from 5.35 to 5.05 log/mL. Furthermore, even this modest benefit in the treated group was lost 24 weeks after discontinuing treatment or at week 48 (36). Another placebo controlled randomized study was performed in 23 CHC patients to assess beneficial effect of 6 months of combination treatment with vitamin E (945 mg), vitamin C (500 mg), and selenium (200 mcg). The study failed to show any beneficial effect on HCVRNA, ALT, or histology (37).
With mitochondrial damage being a common characteristic in the pathogenesis of CHC, MitoQ was tested as a therapeutic agent in a phase II study by Gane et al (38). Thirty patients with contraindications to PEGIFN and/or RBV were randomized to receive MitoQ (40–80 mg/d) or placebo. At the end of 28 days, compared to baseline levels 40 mg of MitoQ resulted in a decrease in ALT (153 to 110 IU/l; P=0.002) and AST (131 to 95 IU/l; P=0.003). Similar changes with 80 mg of MitoQ were 131 to 95; P=0.024 and 87 to 75 IU/l; P=0.017 respectively. However, there was no change in the HCVRNA levels (38). The above results suggest that antioxidants may produce mild decreases in ALT, but alone are not useful therapeutic agents for CHC.
Several trials examined antioxidants as adjuvants to interferon therapy in the era before ribavirin was introduced. In one study, 24 treatment naïve CHC patients were randomized to receive IFN monotherapy alone, or in combination with NAC +sodium selenite, or in combination with NAC+ sodium selenite+ vitamin E. At the end of 6 months of treatment, a higher proportion of patients treated with a regimen including vitamin E achieved negative HCVRNA as compared to IFN monotherapy or IFN+ NAC+ sodium selenite (6/8 vs. 3/8 vs. 2/8; P=0.11). Analysis between vitamin E treated (n=8) vs. non-vitamin E treated (n=16) subjects showed odds of achieving negative HCVRNA at the end of treatment was 2.4 fold higher with vitamin E (P=0.02). However, there was no beneficial effect on SVR (2/8 vs. 1/8 vs. 1/8; P=NS). Surprisingly, there was no effect on oxidative stress markers as measured by trolox equivalent antioxidant capacity (TEAC) and thibarbituric acid reactive substances (TBARS) (39). This improvement in end of treatment response was not confirmed in a placebo controlled study on 120 CHC patients with previous non-response to IFN who were randomized to receive IFN with or without NAC (1200 mg/d) + vitamin E (600 mg/d) for 6 months. ALT normalization rates were similar at the end of treatment (10.3 % vs. 9.7%; P=NS) or 6 months after completing treatment (1.3% vs. 0%; P=NS). None of the patients in either group achieved negative HCV RNA at the end of treatment (40). A similar lack of benefit of vitamin E on HCV RNA loss or SVR was seen in another RCT on 47 CHC patients (41).
In summary, vitamins E and/or C alone or in combination with anti-HCV therapy have shown some biochemical efficacy with reduction in serum ALT levels. However, there is no effect on the virological clearance or SVR which is the goal of treatment of CHC. Further, in most studies the decrease in ALT levels is marginal and is not sustained after stopping the treatment raising a question on the clinical significance of this effect. MitoQ, in one study, has shown some promise in terms of biochemical efficacy, however, it did not show any effect on viral clearance (38). However, this study is limited by small sample size, short duration of treatment, and lack of concomitant anti-HCV therapy. With the recent or upcoming introduction of viral protease inhibitors and other novel antiviral medications to the treatment regimen, it remains to be seen if antioxidants can have a beneficial effect as a component of these regimens.
N-acetylcysteine
In one open pilot study on 14 CHC patients with documented non-response to IFN, addition of NAC in a dose of 1.8 g/d to IFN showed improvement in liver enzymes with decrease in viral load (42). Based on this encouraging response, the combination of NAC and IFN was tested in better designed studies (43, 44). In a placebo controlled double blind RCT, addition of 1.8 g/d of NAC to IFN did not improve SVR rate (43). In another prospective randomized open label study, although the viral response rates were similar, the time to relapse after discontinuing treatment was longer with use of NAC (31 wks vs. 22 wks; p < 0.05). For HCV infection, as mentioned earlier the goal of treatment is to achieve SVR and a delay of 9 weeks in relapse of HCV infection is probably not of any clinical significance. (44).
Agents with antioxidant effect as one of the mechanisms of action
Zinc
Polaprezinc (combination of zinc and l-carnosine), an antioxidant, has been studied as an adjunct to IFN in the treatment of chronic HCV infection in many RCTs (150–300 mg/d orally, N=14–102)(45–51). There are a number of potential mechanisms of the beneficial effects of zinc including reduction of hepatic fibrosis, decrease in ferritin, antioxidant activity, and improvement in hepatic encephalopathy. Zinc has also been shown to negatively affect HCV replication justifying its use for treatment of HCV infection (52). Biochemical efficacy of this compound was evaluated and documented in 4 RCTs (45–48). Virological efficacy was evaluated in 6 studies(45, 46, 48–51) with 2 RCTs showing improved virological outcome (45, 48). Polaprezinc 150 mg/d as adjunct to PEGIFN+ RBV combination was superior to achieve SVR as compared to PEGIFN + RBV alone and PEGIFN + RBV + zinc 300 mg/d (53% vs. 20% vs. 11%; P< 0.05) amongst 34 patients with CHC non-responders to previous treatment (45). Another study on 75 treatment naïve CHC patients showed a trend for higher SVR with use of polaprezinc as adjunct to IFN monotherapy treatment for 6 months (41% vs. 18%; P=NS). In a logistic regression analysis, type of treatment (IFN+ zinc vs. IFN alone) was an independent predictor for achieving the SVR with OR of 5.9 (95% CI: 1.7–23.8; P< 0.007) (48).
In one placebo controlled RCT on 62 HCV cirrhotics, oral polaprezinc (150 mg twice a day) was assessed to determine if it had an impact on the occurrence of HCC. Of the 32 patients randomized to receive zinc, 15 patients had a low zinc level (< 64 mcg/dl) at baseline and 11 (73%) of these improved zinc levels to normal after therapy (zinc responders). In these zinc responders, a decreased occurrence of HCC was seen at the end of 3 years of zinc treatment as compared to placebo treated patients (0% vs. 18%; P<0.05) (53). Zinc was well tolerated by patients in all the studies. In summary, addition of zinc to IFN improves ALT normalization and may have potential to improve the SVR. In addition, zinc supplementation may decrease risk of HCC amongst patients with zinc deficiency and who appropriately respond to supplementation.
Other agents
silymarin is an active component of the milk thistle plant and has been used for treatment of liver diseases. It is a hepatoprotective agent with multifactorial mechanisms of action with reduction of oxidative stress being one of the actions(54). A total of 8 studies (4 RCTs) have evaluated treatment with silymarin as a sole agent for patients with CHC. An initial retrospective study did not show any benefit with silyamrin in a dose up to 1260 mg/d (55). Of the 3 placebo controlled RCTs assessing silymarin in CHC patients (56–58), only one study has shown biochemical efficacy (56) while none showed virological efficacy. Limitations of these studies were small sample size, short duration of 1 week and 3 months in 2 studies (56, 58), low dose of silymarin (450 mg/d) in one study (57) and lack of additional standard anti-HCV regimen in all the studies. It is important to note that there are many compounds in silymarin and high levels of the most potent ones may not be reached with oral administration (59). Limited bioavailability with customary doses of silymarin can be overcome using larger doses up to 2.1 g/d (60) or intravenous administration of silibinin, one of the most potent components of silymarin. In a prospective study, 36 CHC patients with previous non-response to treatment were studied to assess the benefit of silibinin infusion as an adjunct in achieving SVR. In the first protocol 10 mg/kg/d silibinin infusion was given in 16 patients and in the second protocol 20 patients received silibinin infusions in ascending doses of 5, 10, 15, and 20 mg/kg/d. In both the protocols infusions of silibinin were for 14 days and anti-HCV therapy (PEGIFN and RBV) was started on day 8 of silibinin infusion. Silibinin only at a dose of 15 or 20 mg/kg/d was effective in achieving negative HCVRNA in 7 of 20 cases at week 12 (61). Whether, this beneficial antiviral effect of silymarin helped achieving SVR in this difficult group of non-responders remains to be seen. Except for some gastrointestinal upset, the drug was very well tolerated. Recently, Neumann et al reported a case of post-transplantation HCV recurrence describing successful use of silibinin given as 1400 mg/d infusion for 14 days in achieving SVR (62). HCV infection in the post-OLT setting is difficult to treat and this case describing achieving SVR with use of silymarin alone is interesting. If these findings are confirmed in controlled studies on a larger sample, silymarin may have potential as adjuvant or primary therapy of CHC.
In summary, multiple trials have shown a limited ability of antioxidants to cause small reductions in ALT after chronic administration (Table 1). These are typically of the order of 10% or less and are of either uncertain or negligible clinical significance. No study has shown an improvement in outcome. In addition, no study has shown clear benefit of antioxidants as adjuvants to interferon based therapy of HCV. There is therefore no reason to conclude that antioxidants are useful therapeutic agents for chronic hepatitis C. Other agents, particularly silimaryin and its derivatives, are more encouraging, although the beneficial effects may not be strictly a consequence of antioxidant activity.
Table 1.
Randomized clinical trials of antioxidant agents in hepatitis C virus infection
| Author (Ref.) (Yr) | Sample size | Antioxidant and dose | Duration | ALT | HCVRNA | Oxidative stress markers | Histology |
|---|---|---|---|---|---|---|---|
| Antioxidants in treatment naïve patients | |||||||
| Neri (44) (2000) | 77 | IFN ± NAC (2.4 g/d) | 6 mo | NA | Time to relapse shorter with NAC (22 vs. 31 wks; P<0.05) | Decrease with NAC but not sustained | NA |
| Grant (43) (2000) | 147 | NAC 1.8 g/d | 6 mo | NA | ETR (32% vs. 28%) and SVR (5% vs. 4%) similar in 2 groups | NA | NA |
| Matsuoka(53) (2008) | 62 | Polaprezinc 150 mg bid | 3 years | Decrease in ALT with zinc | NA | NA | Lower incidence of HCC (18% vs. 0%) among zinc responders |
| Gordon (58) (2004) | 24 | Silybum marianum 600 mg or 1200 mg per day | 12 weeks | No change | NA | NA | NA |
| Antioxidants in previous non-responders to hepatitis C treatment | |||||||
| von Herbay(33) (1997) | 23 | Vitamin E 800 IU/d | 12 wks | Decrease in 46% | NA | 2 fold increase in Vitamin E levels | NA |
| Ideo (40) (1999) | 120 | IFN-alpha ± NAC 1200 mg/d + Vit. E 600 mg/d | 6 months | No difference | No difference | NA | NA |
| Gabbay (36) (2007) | 100 | Oral + IV cocktail of antioxidants | 24 weeks | Decrease (52% vs. 20%; P=0.05) | Decrease 1 log (28% vs. 12%; P=NS) | NA | Improved HAI (48% vs. 26%; P=0.21) |
| Hawke (60) (2010) | 32 | Silymarin 140, 280, 560, 700 mg every 8 hours | 7 days | No change | No change | NA | NA |
| Feld (130) (2010) | 24 | PEGIFN α-2a (180mcg weekly)+ WB RBV + SAMe 1.6 g/d | 54 wks | NA | Pre-treatment with SAMe resulted in HCVRNA –ve in 48% at 6 months | ||
| Gane (38) (2010)* | 30 | Mitoquinone 40 mg vs80 mg vs placebo | 4 weeks | Decrease in ALT, P<0.05 | No change | NA | NA |
Includes both treatment naïve and previous non-responders
CHC- chronic hepatitis C; IV: Intra-venous; ALT–Alanine aminotransferae; PEGIFN–Pegylated interferon; WB-RBV Weight based ribavirin; NAC- N-acetylcysteine; SVR–Sustained virologic response; SAMe: S-adenosyl methionine; NA: Not available; HCC: Hepatocellular carcinoma
ALCOHOLIC LIVER DISEASE
Alcohol causes three patterns of liver injury. Fatty liver is reversible in the majority of patients with alcohol abstinence whereas alcoholic hepatitis and cirrhosis are responsible for significant morbidity and mortality (63). Liver transplantation, a definitive option for end-stage liver disease may not be possible in this subset of patients due to number of social reasons (63). Hence, there is a need for development of treatment options to improve the outcome of patients with alcoholic cirrhosis and alcoholic hepatitis. Achieving alcohol abstinence is the mainstay of treatment for alcoholic liver disease but clinical improvement after abstinence is variable. Many patients such as those with advanced cirrhosis awaiting liver transplantation or patients with acute alcoholic hepatitis have high short-term mortality and could benefit greatly from therapeutic measures to improve outcome. There are therefore strong rationales for evaluating new potential therapies for alcoholic liver disease.
Clinical evidence of oxidative stress
Oxidative stress was one of the earliest described disease mechanisms in alcoholic liver disease (63–65). Urinary levels of 8-isoprostanes, a marker of oxidative stress and lipid peroxidation are elevated in subjects after alcohol intake compared to normal subjects (202 ± 26 vs. 116 ± 10 pg/mg of urinary creatinine) (66). Alcohol induced mitochondrial damage and CYP2E1 stimulation generate ROS (67). Markers of oxidative stress and lipid peroxidation are increased in patients with alcoholic liver disease (2). Lower levels of vitamin E are also seen in alcoholic liver disease patients with an inverse correlation to severity of the disease (68, 69). In addition, immune responses and antibodies against oxidative protein and DNA adducts are seen in alcoholics with advanced fibrosis/cirrhosis (70). Further, levels of inflammatory markers have been shown to be higher among those patients with alcoholic hepatitis who die compared to survivors (71, 72).
ALCOHOLIC CIRRHOSIS
Pre-clinical evidence of antioxidant efficacy
Rats and baboons fed with alcohol through the intra-gastric route or with a specific liquid Lieber DeCarli diet with ethanol supplying 30–40% of the total daily calories have been traditionally used as animal models of alcoholic liver disease (73, 74) In these models, lower levels of vitamins E and C have been observed and these correlate inversely with the presence of lipid peroxidation products (75).
Further studies in rodents by Thurman and his colleagues have very clearly and elegantly proven that antioxidants are a viable therapeutic approach for alcohol-induced liver injury. These authors showed that managanese superoxide dismutase (Mn-SOD) delivered via vector adenovirus was protective against the damaging effects of alcohol on the liver as compared to control rats given beta galactosidase (76). Pharmacological approaches in rodents have been effective as well. PPC prevents oxidative stress and development of alcoholic liver disease in rodents (15, 16). It has been particularly effective in baboons where it has been shown to decrease proliferation of hepatic stellate cells (77) and prevent alcohol induced liver fibrosis and cirrhosis when administered for 6.5 years (78). These encouraging preclinical studies would thus predict a possibility of therapeutic utility in humans.
Clinical trials
Agents with antioxidant effect as the main mechanism of action
Vitamins E and C
In a randomized double blind placebo controlled study on decompensated alcoholic cirrhotics, use of 500 mg of α tocopherol acetate for 1 year failed to improve the clinical and/or biochemical liver function, hospitalization rates, or patient survival (79). Rates of alcohol drinking were similar among treated patients and controls [17% vs. 12%; P> 0.05].
Polyenylphosphatidylcholine (PPC)
PPC (4.5 g/d given as a 1.5 g tablet three times a day orally) was tested in 789 Veterans (97% male and mean age 49 years) with biopsy proven alcoholic cirrhosis in a randomized double blind placebo controlled multicenter study (80). Average alcohol intake was comparable in the two groups with about 225 g/d for 19 years before the start of treatment and about 35 g/d during the study. The main outcome parameter was liver fibrosis and was assessed in 412 patients by repeat liver biopsy at the end of 2 years of treatment. Advancement of fibrosis by at least one stage was not different between PPC and placebo treated patients (23% vs. 20% respectively; P=0.32). However, there was a trend towards lower occurrence of ascites in the PPC group (9% vs. 14%; P< 0.057). Progression of fibrosis was more frequent amongst those with concomitant HCV infection (32% vs. 17%; P< 0.001). In this subgroup with HCV infection, treatment with PPC also resulted in improved liver function as reflected by liver enzymes and serum bilirubin (80).
In summary, limited data with use of vitamin E and PPC in patients with alcoholic cirrhosis did not provide definitive evidence of beneficial results for the main treatment outcome of fibrosis, although there appeared to be some benefit in particular subgroups such as HCV infected patients. Although, abstinence rates were similar among treated and untreated patients, lack of efficacy could be due to selection of a study population with advanced liver disease and decompensated cirrhosis. Additional studies are needed using these agents in patients with less advanced liver disease and compensated alcoholic cirrhosis.
Agents with antioxidant effect as one of the mechanisms of action
Silymarin
A total of 5 RCTs have tested the use of silymarin in the management of patients with alcoholic cirrhosis. Of these, 2 studies have shown beneficial effects. In a study on 91 patients with alcoholic cirrhosis, silymarin (520 mg/d) given on a long-term basis showed improved 4 year survival as compared to placebo treated patients (58% vs 39%; P=0.03) (81). Another study using silymarin 420 mg/d showed beneficial effects in histology and biochemical parameters but no effect on survival. However, the silymarin in this study was used only for 4 weeks (82). Three RCTs (n=60–97; dose of silymarin: 280–450 mg/d; duration: 6–24 months) were negative for any biochemical, histological, or survival benefit (83–85). This was despite a significant effect on decrease in the oxidative stress markers in one study (83). A recent meta-analysis on all the RCTs on the use of silymarin in patients with alcoholic cirrhosis has shown no beneficial effect of silymarin (86). One of the issues with this meta-analysis is that the authors were not able to control for the alcohol intake and abstinence rates amongst various studies.
ALCOHOLIC HEPATITIS
Unlike alcoholic cirrhosis in which treatment response is complicated by variable degrees of abstinence and recidivism and long-term treatment is likely to be both necessary and difficult to achieve, acute alcoholic hepatitis is a much more attractive target for therapeutic intervention due to its high short-term mortality and the controlled environment of the inpatient setting.
Clinical trials
Agents with Antioxidant Effect as the main mechanism of action
Currently available options for treatment of alcoholic hepatitis are steroids or pentoxifylline (63). Oxidative stress is a major component in the pathogenesis of alcoholic hepatitis justifying the use of antioxidants in this clinical situation. In one RCT, supplementation with 1000 mg of vitamin E on 51 patients with alcoholic hepatitis was unable to improve survival despite improvement in serum hyaluronic acid levels (87). Use of antioxidants has also been compared to steroids in 2 studies. Phillips et al. compared prednisone to a cocktail of antioxidants (treatment duration 4 weeks in both groups). Survival was better in the steroid group at 1 month but similar at 1 year (88). Recently, Ngyen-Khac and colleagues have reported beneficial effects of NAC in a randomized controlled trial in patients with alcoholic hepatitis. Both the groups were treated for 4 weeks. Compared to patients receiving steroids alone (n=85), patients randomized to receive steroids and intravenous NAC (n=89) had lower mortality at month 2 (15% vs. 33%; P=0.007) and a lower complication rate at 6 months (19% vs. 42%; P=0.001) (89). In another study, Stewart et al randomized alcoholic hepatitis patients based on 4 weeks of steroid use to receive either combination of antioxidants (including NAC) for 6 months or no treatment. The survival at 6 months was similar in the two groups and was also independent of the prior steroid use (90). However, this study included only 70 patients and used NAC for a short period of only1 week. If the encouraging results on the use of NAC are confirmed by further studies, combination of steroids and NAC may potentially improve outcome of alcoholic hepatitis patients.
In summary, antioxidants have failed to improve the outcome of patients with alcoholic cirrhosis. N-acetylcysteine as an adjuant to steroids in severe alcoholic hepatitis has shown some promise. Data require confirmation in further randomized studies prior to routine use of NAC as an adjuvant to steroids in severe alcoholic hepatitis. Some of the well designed studies evaluating various antioxidants in patients with alcoholic liver disease are highlighted in Table 2.
Table 2.
Clinical trials of antioxidant agents in alcoholic liver disease
| Author (Ref.) (Yr) | Sample size, population | Alcohol intake | Antioxidant and dose | Duration | ALT | Oxidative stress markers | Histology | Survival |
|---|---|---|---|---|---|---|---|---|
| Alcoholic cirrhosis | ||||||||
| de la Maza(79) (1995) | 74 alcoholic cirrhotics | 150 g/d × 5 yrs | Vitamin E500 mg/d | 12 months | NA | Vitamin E levels increased with treatment | NA | NA |
| Lieber(80) (2003) | 789 with biopsy proven cirrhosis | 225 g/d × 19 yrs | PPC 4.5 g/d | 24 months | No change | NA | Fibrosis progression23% vs. 20%; P=NS. | NA |
| Ferenci(81) (1989) | 91 alcoholic cirrhosis | NA | Silymarin520 mg/d | 41 months | No change | NA | NA | NA |
| Pares (85) (1998) | 200 alcoholic cirrhosis | NA | Silymarin450 mg/d | 24 months | NA | NA | NA | No benefit |
| Alcoholic hepatitis | ||||||||
| Phillips(88) (2006) | 101 with DFI ≥32 | 80g/d(M) 60 g/d(F) | Antioxidant cocktail | 4 weeks | NA | NA | NA | At 30d70% vs. 54%; P=0.05 favoring steroids |
| Stewart(90) (2007) | 70 with DFI ≥32 | NA | AO cocktail | 6 months | NA | NA | NA | 56% vs. 53%(P=0.7) |
| Ngyen- Khac(89) (2009) | 174 alcoholic hepatitis | NA | Steroids ± NAC | 4 weeks | NA | NA | NA | At 2 months(15% vs. 33%; P=0.07) favoring NAC |
| Mezey (87) (2004) | 51 mild to moderate alcoholic hepatitis | NA | Vitamin E1000 IU/d | 3 months | No change | Decrease in HA with vitamin E | NA | At 1 yr(84% vs.77%; P=NS) |
HCV–Hepatitis C virus; Se - Selenium; RCT–Randomized controlled trial; NAC–N-acetylcysteine; HA–Hyaluronic acid
NON ALCOHOLIC FATTY LIVER DISEASE AND NON-ALCOHOLIC STEATOHEPATITIS
Clinical evidence for oxidative stress
An alteration in energy metabolism and mitochondrial function is central to the pathogenesis of fatty liver disease and there is considerable evidence demonstrating that oxidative stress is present in NAFLD. Oxidation of accumulated fatty acids within the mitochondria and other mechanisms as well lead to generation of ROS and consequent oxidative stress. Lipid peroxidation and oxidative stress is a second hit and plays a significant role contributing to the progression of the disease spectrum from NAFLD to NASH (91, 92). Mitochondrial dysfunction with generation of ROS exists at multiple levels in patients with NASH (93, 94). Patients with NASH have much higher levels of markers of oxidative stress compared to NAFLD patients(95, 96). Serum markers of lipid peroxidation and oxidative stress are increased and antioxidant levels (Vitamin E, retinol, and superoxide dismutase) are decreased in NAFLD patients compared to healthy controls (20, 97–99).
Pre-clinical evidence of antioxidant efficacy
There are several useful models of NAFLD and NASH in rodents. These include feeding them with high fat diets and genetic deficiency of leptin, in the ob/ob mice (100–102). The disease induced in these animal models resembles the human phenotype with an important component of insulin resistance. Considerable evidence supports the utility of antioxidant treatment in these rodent models of NASH. Treatment with vitamin E reduced oxidative stress in young male Sprague-Dawley rats with NASH induced by feeding 100% fat diet for few weeks (101). Treatment with another antioxidant, NAC protected against NASH in Sprague Dawley rats with NAFLD induced by high fat diet. Rats treated with NAC had lower ALT elevation, fibrosis, and oxidative stress (103). In another study, SNAC (S-nitroso-N Acetylcysteine), an NO donor prevented NASH in rats when given prior to high fat diet feeding and also reversed NASH when given after 4 weeks of high fat diet and induction of NASH (104). NAC was also shown to be beneficial in a model of liver regeneration after hepatectomy and was associated with lowering of oxidative stress markers and improved antioxidant levels. The benefit was seen only in rats with NAFLD and was not seen in rats undergoing hepatectomy without NAFLD (100). In another study, however, use of NAC in Sprague-Dawley rats with NASH induced by 100% fat diet for 6 weeks did not add to the benefit observed solely by the switching of diet from high fat diet to normal diet (100). The study highlights the importance of dietary intervention in the management of NAFLD and NASH.
Clinical trials
Agents with antioxidant effect as the main mechanism of action
Vitamins E and C
Most early studies using vitamin E alone in NASH patients were not encouraging. Improved oxidative stress with a limited clinical efficacy was shown in one such study using alpha tocopherol 300 mg/d with improvement in biochemical, radiological, and histological parameters (105). In a randomized placebo controlled prospective double blind study, a statistically significant improvement (p=0.02) in fibrosis score was seen using a combination of 1000 IU of vitamin E and 1000 mg of vitamin C for 6 mo (106). No effect was seen on the biochemical profile or inflammation on liver histology (106).
More recently, encouraging data on the use of vitamin E alone was obtained from the PIVENS study (107). In this double blind placebo controlled trial, 247 non diabetic patients with biopsy proven NASH were randomized to receive pioglitazone 30 mg/d (n=80), vitamin E 800 IU/d (n=84) or placebo (n=83) (107). With two comparisons, the P value for significant results was set at 0.025 instead of 0.05. After 96 weeks of treatment, as compared to placebo, achievement of the primary end-point of treatment (biopsy documented improvement in NASH activity score with no worsening of fibrosis) was significantly higher with vitamin E (43% vs. 19%; P=0.001) but not with pioglitazone (34% vs. 19%; P=0.04). Both the drugs were effective for secondary end points of improvement in liver enzymes, and reduction in hepatic steatosis and lobular inflammation on biopsy. However, liver fibrosis did not improve with either of the agents (107). Results from this study are the first to clearly show the usefulness of vitamin E in the management of NASH patients. The main strength of this study was relatively long duration of treatment with histology improvement as the end point.
Weight loss is critical for the management of patients with NAFLD and NASH. Addition of vitamin E and/or C to management with diet and exercise has been tested in 3 studies. Nobili et al compared addition of vitamin E (600 IU/d) and vitamin C (500 mg/d) to diet and exercise with diet and exercise alone in 53 children with NAFLD. At the end of 2 years of treatment the primary end point of improvement in liver histology and improvement in secondary end points (liver enzymes, insulin sensitivity indices, and lipid profile) were similar in the two groups (Table 3) (108). Similarly, in another pilot study on 16 adults with biopsy proven NASH, supplementation with 800 IU/d of vitamin E failed to provide additional benefit on liver enzymes, insulin sensitivity, lipid profile, interlukin-6 cytokine, and plasma hyaluronic acid levels to what is achieved with diet and exercise alone (109). In another study on 28 children with pediatric NAFLD, vitamin E supplementation (400 mg/d x 2 months and then 100 mg/d x 3 months) was effective in reducing fatty liver as detected on ultrasound examination and reducing liver enzymes for children who were unable to adhere to diet control. One limitation of this study is the lack of histology before and after treatment with the diagnosis of NAFLD based on estimation of liver enzymes and ultrasound examination of the liver (110).
Table 3.
Randomized clinical trials of antioxidant agents in non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH)
| Author (Ref.) (Yr) | Population (sample size) | Antioxidant and Dose | Duration | ALT | Insulin sensitivity | Oxidative stress markers | Histology |
|---|---|---|---|---|---|---|---|
| Nobili(108) (2006) | Biopsy proven pediatric NAFLD (90) | Diet + Exercise ± Vitamin E 600 IU/d and Vitamin C 500 mg/d | 24 months | Improved with >20% weight loss | Body weight improved in both groups | Improved with >20% weight loss | NA |
| Bugianesi(112) (2005) | Non diabetic NAFLD or NASH(110) | Metformin 2 g/d vs. Vitamin E 800 IU/d vs Diet only | 12 months | Normal ALT 56% vs. 31% vs. 15% with metfromin, vitamin E, and diet+exercise | Improved with metfromin only | NA | Improved steatosis, necro- inflammation, and fibrosis with metfromin (P=0.02) |
| Harrison(106) (2003) | Biopsy proven NASH(45) | 1000 mg Vitamin E +1000 mg Vitamin C | 6 months | No change | NA | NA | Improved fibrosis with vitamin E in diabetics (P=0.002) |
| Sanyal (107) (2010) | Biopsy proven NASH(250) | Vitamin E 800 IU/D vs. Pioglitazone 30 mg/d vs. placebo | 24 months | NA | NA | NA | Improved NASH but not fibrosis with both vitamin E and pioglitazone |
| Foster (116) (2011) | NAFLD (1005) | 20 mg atorvastatin +1000 IU Vitamin E + 1 g Vitamin C vs Placebo | 42 months | NA | NAw | NA | Lower NAFLD at end of study (73% vs. 34%; P<0.0001) on CT scan |
| Pamuk (117) (2003) | Biopsy proven NASH(35) | NAC 600 mg/d | 1 month | Improved at 4 weeks with NAC(P<0.05) | NA | NA | NA |
| Abdelmalek (123) (2009) | NASH (35) | Betaine 20 mg per day | 12 months | No change | NA | No change | Improved steatosis and no effect on fibrosis |
ALT – Alanine aminotransferase; USG – Ultrasound; NAS – NASH activity score; NA: Not available
Insulin resistance plays a crucial role in the pathogenesis of NAFLD and NASH. This forms the basis for the use of insulin sensitizers in the treatment of NASH (111). Antioxidants have been compared with insulin sensitizers in a few studies. In an open label prospective study, 110 patients with non diabetic NAFLD were randomized to receive 2 g/d of metformin (n=55), vitamin E (n=28), or prescriptive weight reducing diet (n=27). All the patients at the initial screening received nutritional counseling and were advised to walk daily for at least 30 minutes. At the end of 12 months of treatment, metformin treatment was superior to vitamin E or prescriptive diet for normalization of liver enzymes (56% vs. 20%; p=0.0006) and was an independent predictor for normalization of ALT (OR 6 95% CI: 2–17; P=0.0011) (112). In another pilot study on 20 patients, the combination of vitamin E and pioglitazone was superior to vitamin E alone in improving liver biochemical and histological profile (113). Vitamin E (800 IU/d) has also been tried with in combination with ursodeoxycholic acid (UDCA) (12–15 mg/kg/d) and was superior to UDCA + placebo in improving liver enzymes and histology (114). Combination of UDCA and vitamin E (n=14) has also been shown in an randomized study to reduce hepatocyte apoptosis and restore adiponectin levels as compared to use of UDCA alone (n=14) or no treatment (n=13) (115).
Recently, use of vitamins E (1000 IU/d) and C (1 g/d) combination as an adjuvant to the lipid lowering agent atrovastatin (10 mg/d) was studied as part of the St Francis Heart Study in a double blind placebo controlled RCT on 1,005 men and women aged 50–70 years with hyperlipidemia (116). The primary end point was efficacy on reduction in the occurrence of NAFLD (as detected by liver spleen ratio on CT scan) at the end of follow up (mean 3.6 years). A total of 455 patients had pre and post treatment assessment of NAFLD on CT scan. Amongst 80 patients with NAFLD at baseline, the proportion of patients with NAFLD at the end of follow up was significantly lower amongst patients receiving combination of atorvastatin and antioxidants as compared to patients receiving atorvastatin alone (70% vs. 34%; OR 0.29; P<0.001) (116). Only 3 patients in the treatment group developed a rise of liver enzymes to > 2 x upper limit of normal. Of these, one patient had stabilization of liver enzymes and another patient normalized them by the end of the follow up. The liver enzyme levels at the end of follow up were not available for the third patient (116). These data are promising justifying use of vitamin E and/or C with statins for NAFLD patients and also confirm the safety of using statins in patients with NAFLD.
N-Acetylcysteine
NAC has been tested in two studies in patients with NASH. Use of 600 mg/d of NAC in an open label prospective randomized study for 4 wks found improvement in liver enzymes. However, histology was not assessed in this study (Table 3)(117). Another open label prospective trial was performed on 20 patients with NASH who were treated with NAC 1.2 g/d and metformin 500 mg/d for 12 months. The study showed improvement in liver enzymes, insulin resistance, body mass index, and liver histological findings including steatosis and fibrosis although no effect on ballooning or inflammation was found (118).
Agents with antioxidant effect as one of the mechanisms of action
Use of various herbal drugs as compared to diet and exercise alone in 3 studies in patients with NASH have shown improvement of biochemical and oxidative stress markers. Two of these studies are RCTs (119, 120) and one study is retrospective (121). In one study, improved NASH activity score on liver biopsy (4.4 to 0.5 vs. 4.4 to 2.2) was shown with the use of vivusid (combination of vitamin C, zinc, glycyrrhizic zcid) (119). In an open label study on 10 NASH patients, use of betaine, a methyl donor for remethylation of homocysteine showed normalization of biochemical parameters in 50% patients (mean ALT decrease from 147 before treatment to 46 and AST decrease from 94 to 29 IU/l) with improved histology at 1 year (122). Later, two RCTs evaluating this compound showed improved steatosis and biochemical markers but no effect on cytokines, oxidative stress markers, or SAMe (123, 124). Similar to SAMe, the primary mechanism of betaine is related to reconstitution of methylation by serving as a methyl donor and not as an antioxidant.
A systematic review of these studies, including two additional studies using unconventional antioxidant compounds was recently performed. In this meta analysis, no convincing evidence either supporting or refuting the use of antioxidants for fatty liver disease was determined (125). However, latest results on the encouraging effects of vitamin E alone in non-diabetic NASH patients and along with statins in NAFLD patients are promising. Further studies with long term use are needed to see whether the use of vitamin E and antioxidants is associated with improved survival.
ANTIOXIDANTS AS THERAPEUTIC AGENTS FOR LIVER DISEASE: CURRENT STATUS AND FUTURE PROSPECTS
In spite of the overwhelming evidence supporting the association of oxidative stress with liver disease (1, 2), the efficacy of antioxidant therapy has been extremely difficult to demonstrate. Despite numerous examples of efficacy of antioxidants in animal models, currently, the best clinical evidence in support of antioxidants for liver disease is the use of vitamin E for NASH. There is no convincing evidence to support use of antioxidants for Hepatitis C and there is only preliminary or equivocal evidence for alcoholic liver disease. All this is in spite of numerous examples of efficacy in animal models of these diseases. Possible reasons for this discrepancy are described below.
Factors related to study design, patient populations and clinical endpoints
Although, most clinical trials on antioxidants in liver diseases are RCTs, they are limited by small sample size (Tables 1–3). Short duration of treatment and follow up is another limiting factor as is timing of therapy in relationship to the onset of the disease process. Oxidative stress occurs early in the course of liver disease and most studies have shown increasing oxidative stress with the severity of the disease. It is thus possible that a stage is reached in the evolution of the disease process from which the injury is irreversible. Finally, the clinical endpoints used in most studies have been short-term changes in ALT or other biochemical surrogates for liver injury. The recent positive study by Sanyal et al used histology changes at 2 years as its endpoint and was able to show a significant beneficial effect of vitamin E on NASH (107). However, it may require more long-term studies using hard clinical outcomes to establish efficacy without doubt.
Factors related to methodology of measurement of oxidative stress
Failure of the antioxidant drugs to achieve desired clinical endpoints could be because oxidative stress is not a critical disease pathway or because the administered drug never actually produced an antioxidant effect in the liver. Most published studies have failed to document drug delivery and hepatic antioxidant effects. Since it is difficult to measure ROS directly, efficacy of antioxidant function generally needs to be made by measuring surrogate markers in tissue such as oxidized protein derivatives or lipid peroxidation degradation products such as 4-hydroxynoneal, malonaldehyde or isoprostanes (126, 127). Since blood measurement of oxidative stress markers may not correlate well with intrahepatic oxidative stress (95, 127), use of serial liver biopsy in protocol design would be beneficial, but clearly makes it very difficult to perform large scale trials. With the invasive nature of liver biopsy, development of better plasma markers to reflect hepatic oxidative stress is an unmet need for future research.
Variability of antioxidant type and dose
Another important factor to consider when trying to make sense of the antioxidant literature is the ill defined nature of the term “antioxidant” itself. A number of commonly used compounds such as silymarin, betaine, S-adenosylmethionine, and others have multiple biological effects in addition to their ability to function as antioxidants. One must be cautious in interpreting the effects of these agents as due solely or even primarily to the antioxidant nature of the compounds. A related problem is the nonstandard dosing of even well established antioxidant compounds. Agents such as vitamin E, vitamin C and coenzyme Q function because they are single electron acceptors. The flip side of this coin is that they can thus be single electron donors as well. At high concentrations both vitamin C and coenzyme Q can be pro-oxidants and have potential to cause liver damage (13). High dose vitamin A is also a prooxidant and vitamin C in high doses has been shown to mediate iron induced liver damage. This phenomenon may have been a factor in why doses of vitamin E of ≥ 400 IU/d caused an increase in all cause mortality in a large population based study on patients with different diseases (128). This cautionary data needs to be considered in optimal dosing of these agents.
An additional reason for lack of efficacy of vitamin E in clinical studies could be related to the use of alpha tocopherol in most studies. The term “vitamin E” is collectively used for 8 compounds with different biological effects. The antioxidant efficacy of alpha tocopherol is much weaker compared to tocotrienols (129). Secondly, most studies have used vitamin E as an oral preparation which may not always have adequate bioavailability in patients with liver disease.
In conclusion, antioxidants are a potentially attractive class of therapeutic compounds that have yet to establish a role for themselves in the treatment of liver disease. From a disease mechanism standpoint, and from the recent positive trials in NASH and alcoholic hepatitis, there is reason to hope, but many more studies need to be performed. Future studies need to be designed eliminating some of the problems of small numbers of patients and lack of documentation of antioxidant effects, that have been a problem in earlier studies. When these caveats have been followed, encouraging results have been obtained as demonstrated in the recent study reported on the use of vitamin E in NASH (107). This provides a new level of enthusiasm for the possible future of antioxidants in liver diseases.
Acknowledgments
We thank H. Jaeschke and R. Campbell for critical comments and assistance. Work in Dr. Weinman’s lab was supported by grant AA012863 from the National Institute on Alcoholism and Alcohol Abuse and a prior research grant from Cardax Pharmaceuticals. The authors have no other financial or competing interests to disclose.
References
- 1.Medina J, Moreno-Otero R. Pathophysiological basis for antioxidant therapy in chronic liver disease. Drugs. 2005;65:2445–2461. doi: 10.2165/00003495-200565170-00003. [DOI] [PubMed] [Google Scholar]
- 2.Albano E. Alcohol, oxidative stress and free radical damage. Proc Nutr Soc. 2006;65:278–290. doi: 10.1079/pns2006496. [DOI] [PubMed] [Google Scholar]
- 3.Circu ML, Aw TY. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radic Biol Med. 2010;48:749–762. doi: 10.1016/j.freeradbiomed.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muriel P. Role of free radicals in liver diseases. Hepatol Int. 2009;3:526–536. doi: 10.1007/s12072-009-9158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forman HJ, Torres M. Redox signaling in macrophages. Mol Aspects Med. 2001;22:189–216. doi: 10.1016/s0098-2997(01)00010-3. [DOI] [PubMed] [Google Scholar]
- 6.Schulze-Osthoff K, Haussinger D. Apoptosis in the liver: a matter of ion fluxes and oxidative stress: Third International Conference of the Collaborative Research Center ‘Experimental Hepatology’ (SFB-575), Dusseldorf, Germany, 13–14 October 2006. Liver Int. 2007;27:1039–1044. doi: 10.1111/j.1478-3231.2007.01525.x. [DOI] [PubMed] [Google Scholar]
- 7.Guimaraes EL, Franceschi MF, Grivicich I, Dal-Pizzol F, Moreira JC, Guaragna RM, Borojevic R, Margis R, Guma FC. Relationship between oxidative stress levels and activation state on a hepatic stellate cell line. Liver Int. 2006;26:477–485. doi: 10.1111/j.1478-3231.2006.01245.x. [DOI] [PubMed] [Google Scholar]
- 8.Mates JM. Effects of antioxidant enzymes in the molecular control of reactive oxygen species toxicology. Toxicology. 2000;153:83–104. doi: 10.1016/s0300-483x(00)00306-1. [DOI] [PubMed] [Google Scholar]
- 9.Fridovich I. Superoxide radical and superoxide dismutases. Annu Rev Biochem. 1995;64:97–112. doi: 10.1146/annurev.bi.64.070195.000525. [DOI] [PubMed] [Google Scholar]
- 10.Zingg JM. Vitamin E: an overview of major research directions. Mol Aspects Med. 2007;28:400–422. doi: 10.1016/j.mam.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Hill DB, Devalaraja R, Joshi-Barve S, Barve S, McClain CJ. Antioxidants attenuate nuclear factor-kappa B activation and tumor necrosis factor-alpha production in alcoholic hepatitis patient monocytes and rat Kupffer cells, in vitro. Clin Biochem. 1999;32:563–570. doi: 10.1016/s0009-9120(99)00056-9. [DOI] [PubMed] [Google Scholar]
- 12.Houglum K, Venkataramani A, Lyche K, Chojkier M. A pilot study of the effects of d-alpha-tocopherol on hepatic stellate cell activation in chronic hepatitis C. Gastroenterology. 1997;113:1069–1073. doi: 10.1053/gast.1997.v113.pm9322499. [DOI] [PubMed] [Google Scholar]
- 13.Abudu N, Miller JJ, Attaelmannan M, Levinson SS. Vitamins in human arteriosclerosis with emphasis on vitamin C and vitamin E. Clin Chim Acta. 2004;339:11–25. doi: 10.1016/j.cccn.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Zafarullah M, Li WQ, Sylvester J, Ahmad M. Molecular mechanisms of N-acetylcysteine actions. Cell Mol Life Sci. 2003;60:6–20. doi: 10.1007/s000180300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lieber CS, Leo MA, Aleynik SI, Aleynik MK, DeCarli LM. Polyenylphosphatidylcholine decreases alcohol-induced oxidative stress in the baboon. Alcohol Clin Exp Res. 1997;21:375–39. [PubMed] [Google Scholar]
- 16.Okiyama W, Tanaka N, Nakajima T, Tanaka E, Kiyosawa K, Gonzalez FJ, Aoyama T. Polyenephosphatidylcholine prevents alcoholic liver disease in PPARalpha-null mice through attenuation of increases in oxidative stress. J Hepatol. 2009;50:1236–1246. doi: 10.1016/j.jhep.2009.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith RA, Murphy MP. Animal and human studies with the mitochondria-targeted antioxidant MitoQ. Ann N Y Acad Sci. 2010;1201:96–103. doi: 10.1111/j.1749-6632.2010.05627.x. [DOI] [PubMed] [Google Scholar]
- 18.Yadav D, Hertan HI, Schweitzer P, Norkus EP, Pitchumoni CS. Serum and liver micronutrient antioxidants and serum oxidative stress in patients with chronic hepatitis C. Am J Gastroenterol. 2002;97:2634–2639. doi: 10.1111/j.1572-0241.2002.06041.x. [DOI] [PubMed] [Google Scholar]
- 19.Ko WS, Guo CH, Yeh MS, Lin LY, Hsu GS, Chen PC, Luo MC, Lin CY. Blood micronutrient, oxidative stress, and viral load in patients with chronic hepatitis C. World J Gastroenterol. 2005;11:4697–4702. doi: 10.3748/wjg.v11.i30.4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Konishi M, Iwasa M, Araki J, Kobayashi Y, Katsuki A, Sumida Y, Nakagawa N, Kojima Y, Watanabe S, Adachi Y, Kaito M. Increased lipid peroxidation in patients with non-alcoholic fatty liver disease and chronic hepatitis C as measured by the plasma level of 8-isoprostane. J Gastroenterol Hepatol. 2006;21:1821–1825. doi: 10.1111/j.1440-1746.2006.04420.x. [DOI] [PubMed] [Google Scholar]
- 21.Saeki T, Ichiba M, Tanabe N, Ueki M, Okamoto K, Matsunaga Y, Hosho K, Kanbe T, Tsuchiya H, Kurimasa A, Yamada S, Hirooka Y, Hisatome I, Kishimoto Y, Suou T, Murawaki Y, Kawasaki H, Yodoi J, Shiota G. Expression of oxidative stress-related molecules in circulating leukocytes and urine in patients with chronic viral hepatitis. Liver Int. 2006;26:157–165. doi: 10.1111/j.1478-3231.2005.01213.x. [DOI] [PubMed] [Google Scholar]
- 22.Jain SK, Pemberton PW, Smith A, McMahon RF, Burrows PC, Aboutwerat A, Warnes TW. Oxidative stress in chronic hepatitis C: not just a feature of late stage disease. J Hepatol. 2002;36:805–811. doi: 10.1016/s0168-8278(02)00060-0. [DOI] [PubMed] [Google Scholar]
- 23.Fujita N, Horiike S, Sugimoto R, Tanaka H, Iwasa M, Kobayashi Y, Hasegawa K, Ma N, Kawanishi S, Adachi Y, Kaito M. Hepatic oxidative DNA damage correlates with iron overload in chronic hepatitis C patients. Free Radic Biol Med. 2007;42:353–362. doi: 10.1016/j.freeradbiomed.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Mitsuyoshi H, Itoh Y, Sumida Y, Minami M, Yasui K, Nakashima T, Okanoue T. Evidence of oxidative stress as a cofactor in the development of insulin resistance in patients with chronic hepatitis C. Hepatol Res. 2008;38:348–353. doi: 10.1111/j.1872-034X.2007.00280.x. [DOI] [PubMed] [Google Scholar]
- 25.Chuma M, Hige S, Nakanishi M, Ogawa K, Natsuizaka M, Yamamoto Y, Asaka M. 8-Hydroxy-2′-deoxy-guanosine is a risk factor for development of hepatocellular carcinoma in patients with chronic hepatitis C virus infection. J Gastroenterol Hepatol. 2008;23:1431–1436. doi: 10.1111/j.1440-1746.2008.05502.x. [DOI] [PubMed] [Google Scholar]
- 26.Serejo F, Emerit I, Filipe PM, Fernandes AC, Costa MA, Freitas JP, de Moura MC. Oxidative stress in chronic hepatitis C: the effect of interferon therapy and correlation with pathological features. Can J Gastroenterol. 2003;17:644–650. doi: 10.1155/2003/710693. [DOI] [PubMed] [Google Scholar]
- 27.Levent G, Ali A, Ahmet A, Polat EC, Aytac C, Ayse E, Ahmet S. Oxidative stress and antioxidant defense in patients with chronic hepatitis C patients before and after pegylated interferon alfa-2b plus ribavirin therapy. J Transl Med. 2006;4:25. doi: 10.1186/1479-5876-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun JCG, Weinman S. Pathogenesis of liver injury in hepatitisC. In: Monga S, editor. Molecular Pathology of Liver Diseases. Vol. 5. Springer; New York: 2011. pp. 569–588. [Google Scholar]
- 29.de Mochel NS, Seronello S, Wang SH, Ito C, Zheng JX, Liang TJ, Lambeth JD, Choi J. Hepatocyte NAD(P)H oxidases as an endogenous source of reactive oxygen species during hepatitis C virus infection. Hepatology. 2010;52:47–59. doi: 10.1002/hep.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang T, Campbell RV, Yi MK, Lemon SM, Weinman SA. Role of Hepatitis C core protein in viral-induced mitochondrial dysfunction. J Viral Hepatitis. 2010;17:784–793. doi: 10.1111/j.1365-2893.2009.01238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ghany MGSD, Thomas DL, Seeff LB American Association for Study of Liver Diseases. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–1374. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahmood S, Yamada G, Niiyama G, Kawanaka M, Togawa K, Sho M, Ito T, Sasagawa T, Okita M, Nakamura H, Yodoi J. Effect of vitamin E on serum aminotransferase and thioredoxin levels in patients with viral hepatitis C. Free Radic Res. 2003;37:781–785. doi: 10.1080/1071576031000102141. [DOI] [PubMed] [Google Scholar]
- 33.von Herbay A, Stahl W, Niederau C, Sies H. Vitamin E improves the aminotransferase status of patients suffering from viral hepatitis C: a randomized, double-blind, placebo-controlled study. Free Radic Res. 1997;27:599–605. doi: 10.3109/10715769709097863. [DOI] [PubMed] [Google Scholar]
- 34.Takagi H, Kakizaki S, Sohara N, Sato K, Tsukioka G, Tago Y, Konaka K, Kabeya K, Kaneko M, Takayama H, Hashimoto Y, Yamada T, Takahashi H, Shimojo H, Nagamine T, Mori M. Pilot clinical trial of the use of alpha-tocopherol for the prevention of hepatocellular carcinoma in patients with liver cirrhosis. Int J Vitam Nutr Res. 2003;73:411–415. doi: 10.1024/0300-9831.73.6.411. [DOI] [PubMed] [Google Scholar]
- 35.Melhem A, Stern M, Shibolet O, Israeli E, Ackerman Z, Pappo O, Hemed N, Rowe M, Ohana H, Zabrecky G, Cohen R, Ilan Y. Treatment of chronic hepatitis C virus infection via antioxidants: results of a phase I clinical trial. J Clin Gastroenterol. 2005;39:737–742. doi: 10.1097/01.mcg.0000174023.73472.29. [DOI] [PubMed] [Google Scholar]
- 36.Gabbay E, Zigmond E, Pappo O, Hemed N, Rowe M, Zabrecky G, Cohen R, Ilan Y. Antioxidant therapy for chronic hepatitis C after failure of interferon: results of phase II randomized, double-blind placebo controlled clinical trial. World J Gastroenterol. 2007;13:5317–5323. doi: 10.3748/wjg.v13.i40.5317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Groenbaek K, Friis H, Hansen M, Ring-Larsen H, Krarup HB. The effect of antioxidant supplementation on hepatitis C viral load, transaminases and oxidative status: a randomized trial among chronic hepatitis C virus-infected patients. Eur J Gastroenterol Hepatol. 2006;18:985–989. doi: 10.1097/01.meg.0000231746.76136.4a. [DOI] [PubMed] [Google Scholar]
- 38.Gane EJ, Weilert F, Orr DW, Keogh GF, Gibson M, Lockhart MM, Frampton CM, Taylor KM, Smith RA, Murphy MP. The mitochondria-targeted anti-oxidant mitoquinone decreases liver damage in a phase II study of hepatitis C patients. Liver Int. 2010;30:1019–1026. doi: 10.1111/j.1478-3231.2010.02250.x. [DOI] [PubMed] [Google Scholar]
- 39.Look MP, Gerard A, Rao GS, Sudhop T, Fischer HP, Sauerbruch T, Spengler U. Interferon/antioxidant combination therapy for chronic hepatitis C--a controlled pilot trial. Antiviral Res. 1999;43:113–122. doi: 10.1016/s0166-3542(99)00041-8. [DOI] [PubMed] [Google Scholar]
- 40.Ideo G, Bellobuono A, Tempini S, Mondazzi L, Airoldi A, Benetti G, Bissoli F, Cestari C, Colombo E, Del Poggio P, Fracassetti O, Lazzaroni S, Marelli A, Paris B, Prada A, Rainer E, Roffi L. Antioxidant drugs combined with alpha-interferon in chronic hepatitis C not responsive to alpha-interferon alone: a randomized, multicentre study. Eur J Gastroenterol Hepatol. 1999;11:1203–1207. doi: 10.1097/00042737-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Saeian K, Bajaj JS, Franco J, Knox JF, Daniel J, Peine C, McKee D, Varma RR, Ho S. High-dose vitamin E supplementation does not diminish ribavirin-associated haemolysis in hepatitis C treatment with combination standard alpha-interferon and ribavirin. Aliment Pharmacol Ther. 2004;20:1189–1193. doi: 10.1111/j.1365-2036.2004.02260.x. [DOI] [PubMed] [Google Scholar]
- 42.Beloqui O, Prieto J, Suarez M, Gil B, Qian CH, Garcia N, Civeira MP. N-acetyl cysteine enhances the response to interferon-alpha in chronic hepatitis C: a pilot study. J Interferon Res. 1993;13:279–282. doi: 10.1089/jir.1993.13.279. [DOI] [PubMed] [Google Scholar]
- 43.Grant PR, Black A, Garcia N, Prieto J, Garson JA. Combination therapy with interferon-alpha plus N-acetyl cysteine for chronic hepatitis C: a placebo controlled double-blind multicentre study. J Med Virol. 2000;61:439–442. doi: 10.1002/1096-9071(200008)61:4<439::aid-jmv5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 44.Neri S, Ierna D, Antoci S, Campanile E, D’Amico RA, Noto R. Association of alpha-interferon and acetyl cysteine in patients with chronic C hepatitis. Panminerva Med. 2000;42:187–192. [PubMed] [Google Scholar]
- 45.Nagamine T, Takagi H, Takayama H, Kojima A, Kakizaki S, Mori M, Nakajima K. Preliminary study of combination therapy with interferon-alpha and zinc in chronic hepatitis C patients with genotype 1b. Biol Trace Elem Res. 2000;75:53–63. doi: 10.1385/BTER:75:1-3:53. [DOI] [PubMed] [Google Scholar]
- 46.Himoto T, Hosomi N, Nakai S, Deguchi A, Kinekawa F, Matsuki M, Yachida M, Masaki T, Kurokochi K, Watanabe S, Senda S, Kuriyama S. Efficacy of zinc administration in patients with hepatitis C virus-related chronic liver disease. Scand J Gastroenterol. 2007;42:1078–1087. doi: 10.1080/00365520701272409. [DOI] [PubMed] [Google Scholar]
- 47.Murakami Y, Koyabu T, Kawashima A, Kakibuchi N, Kawakami T, Takaguchi K, Kita K, Okita M. Zinc supplementation prevents the increase of transaminase in chronic hepatitis C patients during combination therapy with pegylated interferon alpha-2b and ribavirin. J Nutr Sci Vitaminol (Tokyo) 2007;53:213–218. doi: 10.3177/jnsv.53.213. [DOI] [PubMed] [Google Scholar]
- 48.Takagi H, Nagamine T, Abe T, Takayama H, Sato K, Otsuka T, Kakizaki S, Hashimoto Y, Matsumoto T, Kojima A, Takezawa J, Suzuki K, Sato S, Mori M. Zinc supplementation enhances the response to interferon therapy in patients with chronic hepatitis C. J Viral Hepat. 2001;8:367–371. doi: 10.1046/j.1365-2893.2001.00311.x. [DOI] [PubMed] [Google Scholar]
- 49.Ko WS, Guo CH, Hsu GS, Chiou YL, Yeh MS, Yaun SR. The effect of zinc supplementation on the treatment of chronic hepatitis C patients with interferon and ribavirin. Clin Biochem. 2005;38:614–620. doi: 10.1016/j.clinbiochem.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Suzuki H, Takagi H, Sohara N, Kanda D, Kakizaki S, Sato K, Mori M. Triple therapy of interferon and ribavirin with zinc supplementation for patients with chronic hepatitis C: a randomized controlled clinical trial. World J Gastroenterol. 2006;12:1265–1269. doi: 10.3748/wjg.v12.i8.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suzuki H, Sato K, Takagi H, Kanda D, Sohara N, Kakizaki S, Nakajima H, Otsuka T, Nagamine T, Mori M. Randomized controlled trial of consensus interferon with or without zinc for chronic hepatitis C patients with genotype 2. World J Gastroenterol. 2006;12:945–950. doi: 10.3748/wjg.v12.i6.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yuasa K, Naganuma A, Sato K, Ikeda M, Kato N, Takagi H, Mori M. Zinc is a negative regulator of hepatitis C virus RNA replication. Liver Int. 2006;26:1111–1118. doi: 10.1111/j.1478-3231.2006.01352.x. [DOI] [PubMed] [Google Scholar]
- 53.Matsuoka S, Matsumura H, Nakamura H, Oshiro S, Arakawa Y, Hayashi J, Sekine N, Nirei K, Yamagami H, Ogawa M, Nakajima N, Amaki S, Tanaka N, Moriyama M. Zinc supplementation improves the outcome of chronic hepatitis C and liver cirrhosis. J Clin Biochem Nutr. 2009;45:292–303. doi: 10.3164/jcbn.08-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagoner J, Negash A, Kane OJ, Martinez LE, Nahmias Y, Bourne N, Owen DM, Grove J, Brimacombe C, McKeating JA, Pecheur EI, Graf TN, Oberlies NH, Lohmann V, Cao F, Tavis JE, Polyak SJ. Multiple effects of silymarinon the hepatitis C virus lifecycle. Hepatology. 2010;51:1912–1921. doi: 10.1002/hep.23587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huber R, Futter I, Ludtke R. Oral silymarinfor chronic hepatitis C -a retrospectiveanalysis comparing three dose regimens. Eur J Med Res. 2005;10:68–70. [PubMed] [Google Scholar]
- 56.Buzzelli G, Moscarella S, Giusti A, Duchini A, Marena C, Lampertico M. A pilot study on the liver protective effect of silybin-phosphatidylcholine complex (IdB1016) in chronic active hepatitis. Int J Clin Pharmacol Ther Toxicol. 1993;31:456–460. [PubMed] [Google Scholar]
- 57.El-Zayadi AR, Attia M, Badran HM, El-Tawil A, Zalata K, Barakat E, Selim O, El-Nakeeb A, Saied A. Non-interferon-based therapy: an option for amelioration of necro-inflammation in hepatitis C patients who cannot afford interferon therapy. Liver Int. 2005;25:746–751. doi: 10.1111/j.1478-3231.2005.01110.x. [DOI] [PubMed] [Google Scholar]
- 58.Gordon A, Hobbs DA, Bowden DS, Bailey MJ, Mitchell J, Francis AJ, Roberts SK. Effects of Silybum marianum on serum hepatitis C virus RNA, alanine aminotransferase levels and well-being in patients with chronic hepatitis C. J Gastroenterol Hepatol. 2006;21:275–280. doi: 10.1111/j.1440-1746.2006.04138.x. [DOI] [PubMed] [Google Scholar]
- 59.Polyak SJ, Morishima C, Lohmann V, Pal S, Lee DY, Liu Y, Graf TN, Oberlies NH. Identification of hepatoprotective flavonolignans from silymarin. Proc Natl Acad Sci U S A. 2010;107:5995–5999. doi: 10.1073/pnas.0914009107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hawke RL, Schrieber SJ, Soule TA, Wen Z, Smith PC, Reddy KR, Wahed AS, Belle SH, Afdhal NH, Navarro VJ, Berman J, Liu QY, Doo E, Fried MW. Silymarin ascending multiple oral dosing phase I study in noncirrhotic patients with chronic hepatitis C. J Clin Pharmacol. 2010;50:434–449. doi: 10.1177/0091270009347475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferenci P, Scherzer TM, Kerschner H, Rutter K, Beinhardt S, Hofer H, Schoniger-Hekele M, Holzmann H, Steindl-Munda P. Silibinin is a potent antiviral agent in patients with chronic hepatitis C not responding to pegylated interferon/ribavirin therapy. Gastroenterology. 2008;135:1561–1567. doi: 10.1053/j.gastro.2008.07.072. [DOI] [PubMed] [Google Scholar]
- 62.Neumann UP, Biermer M, Eurich D, Neuhaus P, Berg T. Successful prevention of hepatitis C virus (HCV) liver graft reinfection by silibinin mono-therapy. J Hepatol. 2010;52:951–952. doi: 10.1016/j.jhep.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 63.Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N Engl J Med. 2009;360:2758–2769. doi: 10.1056/NEJMra0805786. [DOI] [PubMed] [Google Scholar]
- 64.Wu D, Cederbaum AI. Oxidative stress and alcoholic liver disease. Semin Liver Dis. 2009;29:141–154. doi: 10.1055/s-0029-1214370. [DOI] [PubMed] [Google Scholar]
- 65.Nanji AA. Role of Kupffer cells in alcoholic hepatitis. Alcohol. 2002;27:13–15. doi: 10.1016/s0741-8329(02)00207-0. [DOI] [PubMed] [Google Scholar]
- 66.Pemberton PW, Smith A, Warnes TW. Non-invasive monitoring of oxidant stress in alcoholic liver disease. Scand J Gastroenterol. 2005;40:1102–1108. doi: 10.1080/00365520510023495. [DOI] [PubMed] [Google Scholar]
- 67.Albano E. Oxidative mechanisms in the pathogenesis of alcoholic liver disease. Mol Aspects Med. 2008;29:9–16. doi: 10.1016/j.mam.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 68.Nielsen K, Kondrup J, Martinsen L, Stilling B, Wikman B. Nutritional assessment and adequacy of dietary intake in hospitalized patients with alcoholic liver cirrhosis. Br J Nutr. 1993;69:665–679. doi: 10.1079/bjn19930068. [DOI] [PubMed] [Google Scholar]
- 69.Tanner AR, Bantock I, Hinks L, Lloyd B, Turner NR, Wright R. Depressed selenium and vitamin E levels in an alcoholic population. Possible relationship to hepatic injury through increased lipid peroxidation. Dig Dis Sci. 1986;31:1307–1312. doi: 10.1007/BF01299808. [DOI] [PubMed] [Google Scholar]
- 70.Rolla R, Vay D, Mottaran E, Parodi M, Traverso N, Arico S, Sartori M, Bellomo G, Klassen LW, Thiele GM, Tuma DJ, Albano E. Detection of circulating antibodies against malondialdehyde-acetaldehyde adducts in patients with alcohol-induced liver disease. Hepatology. 2000;31:878–884. doi: 10.1053/he.2000.5373. [DOI] [PubMed] [Google Scholar]
- 71.Sheron N, Bird G, Goka J, Alexander G, Williams R. Elevated plasma interleukin-6 and increased severity and mortality in alcoholic hepatitis. Clin Exp Immunol. 1991;84:449–453. [PMC free article] [PubMed] [Google Scholar]
- 72.Ito S, Yukawa T, Uetake S, Yamauchi M. Serum intercellular adhesion molecule-1 in patients with nonalcoholic steatohepatitis: comparison with alcoholic hepatitis. Alcohol Clin Exp Res. 2007;31:S83–87. doi: 10.1111/j.1530-0277.2006.00292.x. [DOI] [PubMed] [Google Scholar]
- 73.French SW, Benson NC, Sun PS. Centrilobular liver necrosis induced by hypoxia in chronic ethanol-fed rats. Hepatology. 1984;4:912–917. doi: 10.1002/hep.1840040521. [DOI] [PubMed] [Google Scholar]
- 74.Lieber CS, DeCarli LM. The feeding of alcohol in liquid diets: two decades of applications and 1982 update. Alcohol ClinExp Res. 1982;6:523–531. doi: 10.1111/j.1530-0277.1982.tb05017.x. [DOI] [PubMed] [Google Scholar]
- 75.Jurczuk M, Brzoska MM, Moniuszko-Jakoniuk J. Hepatic and renal concentrations of vitamins E and C in lead-and ethanol-exposed rats. An assessment of their involvement in the mechanisms of peroxidative damage. Food Chem Toxicol. 2007;45:1478–1486. doi: 10.1016/j.fct.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 76.Wheeler MD, Nakagami M, Bradford BU, Uesugi T, Mason RP, Connor HD, Dikalova A, Kadiiska M, Thurman RG. Overexpression of manganese superoxide dismutase prevents alcohol-induced liver injury in the rat. J Biol Chem. 2001;276:36664–36672. doi: 10.1074/jbc.M105352200. [DOI] [PubMed] [Google Scholar]
- 77.Poniachik J, Baraona E, Zhao J, Lieber CS. Dilinoleoylphosphatidylcholine decreases hepatic stellate cell activation. J Lab Clin Med. 1999;133:342–348. doi: 10.1016/s0022-2143(99)90064-1. [DOI] [PubMed] [Google Scholar]
- 78.Lieber CS, Robins SJ, Li J, DeCarli LM, Mak KM, Fasulo JM, Leo MA. Phosphatidylcholine protects against fibrosis and cirrhosis in the baboon. Gastroenterology. 1994;106:152–159. doi: 10.1016/s0016-5085(94)95023-7. [DOI] [PubMed] [Google Scholar]
- 79.de la Maza MP, Petermann M, Bunout D, Hirsch S. Effects of long-term vitamin E supplementation in alcoholic cirrhotics. J Am Coll Nutr. 1995;14:192–196. doi: 10.1080/07315724.1995.10718493. [DOI] [PubMed] [Google Scholar]
- 80.Lieber CS, Weiss DG, Groszmann R, Paronetto F, Schenker S. II. Veterans Affairs Cooperative Study of polyenylphosphatidylcholine in alcoholic liver disease. Alcohol Clin Exp Res. 2003;27:1765–1772. doi: 10.1097/01.ALC.0000093743.03049.80. [DOI] [PubMed] [Google Scholar]
- 81.Ferenci P, Dragosics B, Dittrich H, Frank H, Benda L, Lochs H, Meryn S, Base W, Schneider B. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol. 1989;9:105–113. doi: 10.1016/0168-8278(89)90083-4. [DOI] [PubMed] [Google Scholar]
- 82.Salmi HA, Sarna S. Effect of silymarinon chemical, functional, and morphological alterations of the liver. A double-blind controlled study. Scand J Gastroenterol. 1982;17:517–521. doi: 10.3109/00365528209182242. [DOI] [PubMed] [Google Scholar]
- 83.Lucena MI, Andrade RJ, de la Cruz JP, Rodriguez-Mendizabal M, Blanco E, Sanchez de la Cuesta F. Effects of silymarinMZ-80 on oxidative stress in patients with alcoholic cirrhosis. Results of a randomized, double-blind, placebo-controlled clinical study. Int J Clin Pharmacol Ther. 2002;40:2–8. doi: 10.5414/cpp40002. [DOI] [PubMed] [Google Scholar]
- 84.Bunout D, Hirsch S, Petermann M, de la Maza MP, Silva G, Kelly M, Ugarte G, Iturriaga H. Controlled study of the effect of silymarinon alcoholic liver disease. Rev Med Chil. 1992;120:1370–1375. [PubMed] [Google Scholar]
- 85.Pares A, Planas R, Torres M, Caballeria J, Viver JM, Acero D, Panes J, Rigau J, Santos J, Rodes J. Effects of silymarinin alcoholic patients with cirrhosis of the liver: results of a controlled, double-blind, randomized and multicenter trial. J Hepatol. 1998;28:615–621. doi: 10.1016/s0168-8278(98)80285-7. [DOI] [PubMed] [Google Scholar]
- 86.Rambaldi A, Jacobs BP, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C virus liver diseases. Cochrane Database Syst Rev. 2007:CD003620. doi: 10.1002/14651858.CD003620.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mezey E, Potter JJ, Rennie-Tankersley L, Caballeria J, Pares A. A randomized placebo controlled trial of vitamin E for alcoholic hepatitis. J Hepatol. 2004;40:40–46. doi: 10.1016/s0168-8278(03)00476-8. [DOI] [PubMed] [Google Scholar]
- 88.Phillips M, Curtis H, Portmann B, Donaldson N, Bomford A, O’Grady J. Antioxidants versus corticosteroids in the treatment of severe alcoholic hepatitis--a randomised clinical trial. J Hepatol. 2006;44:784–790. doi: 10.1016/j.jhep.2005.11.039. [DOI] [PubMed] [Google Scholar]
- 89.Ngyen-Khac ETT, Piquet MA, Benferhat S, Hezam A, Goria O, et al. Treatment of severe acute alcoholic hepatitis (AAH) with cortioids plus N-acetylcysteine (C+NAC) versus corticoids alone (C): A multicenter randomized controlled trial [Abstract] Hepatology. 2009;50:346A. [Google Scholar]
- 90.Stewart S, Prince M, Bassendine M, Hudson M, James O, Jones D, Record C, Day CP. Arandomized trial of antioxidant therapy alone or with corticosteroids in acute alcoholic hepatitis. J Hepatol. 2007;47:277–283. doi: 10.1016/j.jhep.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 91.Mantena SK, King AL, Andringa KK, Eccleston HB, Bailey SM. Mitochondrial dysfunction and oxidative stress in the pathogenesis of alcohol-and obesity-induced fatty liver diseases. Free Radic Biol Med. 2008;44:1259–1272. doi: 10.1016/j.freeradbiomed.2007.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McCullough AJ. Pathophysiology of nonalcoholic steatohepatitis. J Clin Gastroenterol. 2006;40(Suppl 1):S17–29. doi: 10.1097/01.mcg.0000168645.86658.22. [DOI] [PubMed] [Google Scholar]
- 93.Sanyal AJ, Campbell-Sargent C, Mirshahi F, Rizzo WB, Contos MJ, Sterling RK, Luketic VA, Shiffman ML, Clore JN. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–1192. doi: 10.1053/gast.2001.23256. [DOI] [PubMed] [Google Scholar]
- 94.Serviddio G, Sastre J, Bellanti F, Vina J, Vendemiale G, Altomare E. Mitochondrial involvement in non-alcoholic steatohepatitis. Mol Aspects Med. 2008;29:22–35. doi: 10.1016/j.mam.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 95.Machado MV, Ravasco P, Jesus L, Marques-Vidal P, Oliveira CR, Proenca T, Baldeiras I, Camilo ME, Cortez-Pinto H. Blood oxidative stress markers in non-alcoholic steatohepatitis and how it correlates with diet. Scand J Gastroenterol. 2008;43:95–102. doi: 10.1080/00365520701559003. [DOI] [PubMed] [Google Scholar]
- 96.Musso G, Gambino R, De Michieli F, Biroli G, Premoli A, Pagano G, Bo S, Durazzo M, Cassader M. Nitrosative stress predicts the presence and severity of nonalcoholic fatty liver at different stages of the development of insulin resistance and metabolic syndrome: possible role of vitamin A intake. Am J Clin Nutr. 2007;86:661–671. doi: 10.1093/ajcn/86.3.661. [DOI] [PubMed] [Google Scholar]
- 97.Cankurtaran M, Kav T, Yavuz B, Shorbagi A, Halil M, Coskun T, Arslan S. Serum vitamin-E levels and its relation to clinical features in nonalcoholic fatty liver disease with elevated ALT levels. Acta Gastroenterol Belg. 2006;69:5–11. [PubMed] [Google Scholar]
- 98.Villaca Chaves G, Pereira SE, Saboya CJ, Ramalho A. Non-alcoholic fatty liver disease and its relationship with the nutritional status of vitamin A in individuals with class III obesity. Obes Surg. 2008;18:378–385. doi: 10.1007/s11695-007-9361-2. [DOI] [PubMed] [Google Scholar]
- 99.Koruk M, Taysi S, Savas MC, Yilmaz O, Akcay F, Karakok M. Oxidative stress and enzymatic antioxidant status in patients with nonalcoholic steatohepatitis. Ann Clin Lab Sci. 2004;34:57–62. [PubMed] [Google Scholar]
- 100.Samuhasaneeto S, Thong-Ngam D, Kulaputana O, Patumraj S, Klaikeaw N. Effects of N-acetylcysteine on oxidative stress in rats with non-alcoholic steatohepatitis. J Med Assoc Thai. 2007;90:788–797. [PubMed] [Google Scholar]
- 101.Raso GM, Esposito E, Iacono A, Pacilio M, Cuzzocrea S, Canani RB, Calignano A, Meli R. Comparative therapeutic effects of metformin and vitamin E in a model of non-alcoholic steatohepatitis in the young rat. Eur J Pharmacol. 2009;604:125–131. doi: 10.1016/j.ejphar.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 102.Brun P, Castagliuolo I, Di Leo V, Buda A, Pinzani M, Palu G, Martines D. Increased intestinal permeability in obese mice: new evidence in the pathogenesis of nonalcoholic steatohepatitis. Am J Physiol Gastrointest Liver Physiol. 2007;292:G518–525. doi: 10.1152/ajpgi.00024.2006. [DOI] [PubMed] [Google Scholar]
- 103.Baumgardner JN, Shankar K, Hennings L, Albano E, Badger TM, Ronis MJ. N-acetylcysteine attenuates progression of liver pathology in a rat model of nonalcoholic steatohepatitis. J Nutr. 2008;138:1872–1879. doi: 10.1093/jn/138.10.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.de Oliveira CP, de Lima VM, Simplicio FI, Soriano FG, de Mello ES, de Souza HP, Alves VA, Laurindo FR, Carrilho FJ, de Oliveira MG. Prevention and reversion of nonalcoholic steatohepatitis in OB/OB mice by S-nitroso-N-acetylcysteine treatment. J Am Coll Nutr. 2008;27:299–305. doi: 10.1080/07315724.2008.10719703. [DOI] [PubMed] [Google Scholar]
- 105.Kawanaka M, Mahmood S, Niiyama G, Izumi A, Kamei A, Ikeda H, Suehiro M, Togawa K, Sasagawa T, Okita M, Nakamura H, Yodoi J, Yamada G. Control of oxidative stress and reduction in biochemical markers by Vitamin E treatment in patients with nonalcoholic steatohepatitis: a pilot study. Hepatol Res. 2004;29:39–41. doi: 10.1016/j.hepres.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 106.Harrison SA, Torgerson S, Hayashi P, Ward J, Schenker S. Vitamin E and vitamin C treatment improves fibrosis inpatients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2003;98:2485–2490. doi: 10.1111/j.1572-0241.2003.08699.x. [DOI] [PubMed] [Google Scholar]
- 107.Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, Neuschwander-Tetri BA, Lavine JE, Tonascia J, Unalp A, Van Natta M, Clark J, Brunt EM, Kleiner DE, Hoofnagle JH, Robuck PR. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nobili V, Manco M, Devito R, Ciampalini P, Piemonte F, Marcellini M. Effect of vitamin E on aminotransferase levels and insulin resistance in children with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2006;24:1553–1561. doi: 10.1111/j.1365-2036.2006.03161.x. [DOI] [PubMed] [Google Scholar]
- 109.Kugelmas M, Hill DB, Vivian B, Marsano L, McClain CJ. Cytokines and NASH: a pilot study of the effects of lifestyle modification and vitamin E. Hepatology. 2003;38:413–419. doi: 10.1053/jhep.2003.50316. [DOI] [PubMed] [Google Scholar]
- 110.Vajro P, Mandato C, Franzese A, Ciccimarra E, Lucariello S, Savoia M, Capuano G, Migliaro F. Vitamin E treatment in pediatric obesity-related liver disease: a randomized study. J Pediatr Gastroenterol Nutr. 2004;38:48–55. doi: 10.1097/00005176-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 111.Stein LL, Dong MH, Loomba R. Insulin sensitizers in nonalcoholic fatty liver disease and steatohepatitis: Current status. Adv Ther. 2009;26:893–907. doi: 10.1007/s12325-009-0072-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bugianesi E, Gentilcore E, Manini R, Natale S, Vanni E, Villanova N, David E, Rizzetto M, Marchesini G. A randomized controlled trial of metformin versus vitamin E or prescriptive diet in nonalcoholic fatty liver disease. Am JGastroenterol. 2005;100:1082–1090. doi: 10.1111/j.1572-0241.2005.41583.x. [DOI] [PubMed] [Google Scholar]
- 113.Sanyal AJ, Mofrad PS, Contos MJ, Sargeant C, Luketic VA, Sterling RK, Stravitz RT, Shiffman ML, Clore J, Mills AS. A pilot study of vitamin E versus vitamin E and pioglitazone for the treatment of nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2004;2:1107–1115. doi: 10.1016/s1542-3565(04)00457-4. [DOI] [PubMed] [Google Scholar]
- 114.Dufour JF, Oneta CM, Gonvers JJ, Bihl F, Cerny A, Cereda JM, Zala JF, Helbling B, Steuerwald M, Zimmermann A. Randomized placebo-controlled trial of ursodeoxycholic acid with vitamin e in nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2006;4:1537–1543. doi: 10.1016/j.cgh.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 115.Balmer ML, Siegrist K, Zimmermann A, Dufour JF. Effects of ursodeoxycholic acid in combination with vitamin E on adipokines and apoptosis in patients with nonalcoholic steatohepatitis. Liver Int. 2009;29:1184–1188. doi: 10.1111/j.1478-3231.2009.02037.x. [DOI] [PubMed] [Google Scholar]
- 116.Foster T, Budoff MJ, Saab S, Ahmadi N, Gordon C, Guerci AD. Atorvastatin and antioxidants for the treatment of nonalcoholic fatty liver disease: the St Francis Heart Study randomized clinical trial. Am J Gastroenterol. 2011;106:71–77. doi: 10.1038/ajg.2010.299. [DOI] [PubMed] [Google Scholar]
- 117.Pamuk GE, Sonsuz A. N-acetylcysteine in the treatment of non-alcoholic steatohepatitis. J Gastroenterol Hepatol. 2003;18:1220–1221. doi: 10.1046/j.1440-1746.2003.03156.x. [DOI] [PubMed] [Google Scholar]
- 118.de Oliveira CP, Stefano JT, de Siqueira ER, Silva LS, de Campos Mazo DF, Lima VM, Furuya CK, Mello ES, Souza FG, Rabello F, Santos TE, Nogueira MA, Caldwell SH, Alves VA, Carrilho FJ. Combination of N-acetylcysteine and metformin improves histological steatosis and fibrosis in patients with non-alcoholic steatohepatitis. Hepatol Res. 2008;38:159–165. doi: 10.1111/j.1872-034X.2007.00215.x. [DOI] [PubMed] [Google Scholar]
- 119.Gomez EV, Perez YM, Sanchez HV, Forment GR, Soler EA, Bertot LC, Garcia AY, del Rosario Abreu Vazquez M, Fabian LG. Antioxidant and immunomodulatory effects of Viusid in patients with chronic hepatitis C. World J Gastroenterol. 2010;16:2638–2647. doi: 10.3748/wjg.v16.i21.2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang SJ, Chen ZX, Jiang KP, Cheng YH, Gu YL. The effect of QuYuHuaTanTongLuo Decoction on the non-alcoholic steatohepatitis. Complement Ther Med. 2008;16:192–198. doi: 10.1016/j.ctim.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 121.Fujimoto M, Tsuneyama K, Kinoshita H, Goto H, Takano Y, Selmi C, Keen CL, Gershwin ME, Shimada Y. The traditional Japanese formula keishibukuryogan reduces liver injury and inflammation in patients with nonalcoholic fatty liver disease. Ann N Y Acad Sci. 2010;1190:151–158. doi: 10.1111/j.1749-6632.2009.05265.x. [DOI] [PubMed] [Google Scholar]
- 122.Abdelmalek MF, Angulo P, Jorgensen RA, Sylvestre PB, Lindor KD. Betaine, a promising new agent for patients with nonalcoholic steatohepatitis: results of a pilot study. Am J Gastroenterol. 2001;96:2711–2717. doi: 10.1111/j.1572-0241.2001.04129.x. [DOI] [PubMed] [Google Scholar]
- 123.Abdelmalek MF, Sanderson SO, Angulo P, Soldevila-Pico C, Liu C, Peter J, Keach J, Cave M, Chen T, McClain CJ, Lindor KD. Betaine for nonalcoholic fatty liver disease: results of a randomized placebo-controlled trial. Hepatology. 2009;50:1818–1826. doi: 10.1002/hep.23239. [DOI] [PubMed] [Google Scholar]
- 124.Miglio F, Rovati LC, Santoro A, Setnikar I. Efficacy and safety of oral betaine glucuronate in non-alcoholic steatohepatitis. A double-blind, randomized, parallel-group, placebo-controlled prospective clinical study. Arzneimittelforschung. 2000;50:722–727. doi: 10.1055/s-0031-1300279. [DOI] [PubMed] [Google Scholar]
- 125.Lirussi F, Azzalini L, Orando S, Orlando R, Angelico F. Antioxidant supplements for non-alcoholic fatty liver disease and/or steatohepatitis. Cochrane Database Syst Rev. 2007:CD004996. doi: 10.1002/14651858.CD004996.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Halliwell B, Whiteman M. Measuring reactive species and oxidative damage in vivo and in cell culture: how should you do it and what do the results mean? Br J Pharmacol. 2004;142:231–255. doi: 10.1038/sj.bjp.0705776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bonnefont-Rousselot D, Ratziu V, Giral P, Charlotte F, Beucler I, Poynard T. Blood oxidative stress markers are unreliable markers of hepatic steatosis. Aliment Pharmacol Ther. 2006;23:91–98. doi: 10.1111/j.1365-2036.2006.02719.x. [DOI] [PubMed] [Google Scholar]
- 128.Miller ER, 3rd, Pastor-Barriuso R, Dalal D, Riemersma RA, Appel LJ, Guallar E. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 129.Sen CK, Khanna S, Roy S. Tocotrienols: Vitamin E beyond tocopherols. Life Sci. 2006;78:2088–2098. doi: 10.1016/j.lfs.2005.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Feld JJ, Modi AA, El-Diwany R, Rotman Y, Thomas E, Ahlenstiel G, Titerence R, Koh C, Cherepanov V, Heller T, Ghany MG, Park Y, Hoofnagle JH, Liang TJ. S-adenosyl methionine improves early viral responses and interferon-stimulated gene induction in hepatitis C nonresponders. Gastroenterology. 2011;140:830–839. doi: 10.1053/j.gastro.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


