Abstract
Little theoretical or empirical attention has been given to factors associated with better or worse outcomes in offspring of depressed fathers. Drawing from interpersonal models of intergenerational depression transmission in children of depressed mothers, the present investigation of adolescents and their families (N = 424) examined maternal warmth and hostility as moderators of the longitudinal association between paternal and adolescent depressive symptoms. Controlling for family demographic variables, previous adolescent depressive symptoms, and maternal depressive symptoms, fathers’ depressive symptoms predicted offspring depressive symptoms among adolescents experiencing low maternal warmth or high maternal hostility. Adolescent girls reporting adversity in their relationships with their mothers were the most vulnerable to risk associated with paternal depressive symptoms. These findings highlight the implications of fathers’ mental health for adolescent psychological well-being and add to the growing evidence that family relationships play a crucial role in the transmission of depression from one generation to the next.
Keywords: depressive symptoms, fathers, mother-adolescent relations, adolescent mental health
It is well established that children and adolescents of depressed parents are at increased risk for a range of psychopathology (for reviews, see Goodman & Gotlib, 2002; Hammen, 2008). Fathers have been historically underrepresented in this literature (Phares, 1997), although a fast growing body of work has associated paternal depression and depressed mood with negative outcomes in adolescents including mood disorders, substance abuse, and aggression (e.g., Low & Stocker, 2005; Ramchandani et al., 2008; Rohde, Lewinsohn, Klein, & Seeley, 2005). Over the past decade, the focus of research and theory of intergenerational depression has begun to shift from the association between parent and child disorders to the processes through which depressed parents impart risk for psychopathology to their children and to risk and protective factors in these families (see Gotlib & Goodman, 2002). One particular challenge in this area of study has been to understand the wide diversity of outcomes in offspring with depressed parents, as many of these children are able to adapt to their difficult environments (Davies & Windle, 1997).
Although not the central focus of the present study, a large body of work has investigated parenting and the family environment as predictors of adolescent adjustment. Parent – adolescent relationship difficulties and adverse family environments characterized by elevated hostility and critical interactions have both been consistently associated with adolescent maladjustment (Conger et al., 1993; Sheeber, Hops, & Davis, 2001). Research on the impact of interpersonal relations on children’s psychological well-being may be particularly relevant to the study of intergenerational depression, as families with a depressed parent are less cohesive and express less care for each other than families with nondepressed parents (Kaslow, Warner, John, & Brown, 1992). Indeed, contemporary models of intergenerational depression transmission include social aspects of the family context as moderators of the adverse effects of maternal depression on children’s functioning (e.g., Goodman, 2007; Hammen, Shih, & Brennan, 2004). Recent findings have supported these models, indicating that positive father involvement can function as a protective factor against the adverse effects of maternal depression on offspring development (Chang, Halpern, & Kaufman, 2007; Mezulis, Hyde, & Clark, 2004). Little theoretical or empirical attention has been given to factors associated with better or worse outcomes in offspring of depressed fathers (Phares, Duhig, & Watkins, 2002). The central purpose of the present study was to examine the mother-adolescent relationship as a moderator of the longitudinal association between fathers’ depressive symptoms and adolescent depressive symptoms.
Adolescent Depression
The present study focuses on the intergenerational transmission of risk for depression during adolescence. It is during early adolescence that depression and subclinical depression in children typically emerges (Georgiades, Lewinsohn, Monroe, & Seeley, 2006), and adolescence marks a particularly high-risk period for depression in terms of prevalence (Costello, Foley, & Angold, 2006) and severity of impairment (Gotlib, Lewinsohn, & Seeley, 1998). By age nineteen, 35% of adolescent females and 19% of adolescent males will experience at least one episode of clinical depression (Lewinsohn, Rohde, & Seeley, 1998), which has been associated with relationship difficulties, early pregnancy, academic difficulties, and elevated risk for a number of psychiatric problems (Gotlib et al., 1998; Harrington & Dubicka, 2001; Lewinsohn, Rohde, Klein, & Seeley, 1999). The majority of research to date on depression during adolescence has been cross– sectional (Lewinsohn & Essau, 2002) and has relied on clinical samples which may not be representative of the general population of adolescents (Costello, 1993). As a consequence, questions remain about the psychosocial antecedents of adolescent depression and about the implications of subdiagnostic levels of depression, which are experienced by a substantial proportion of adolescents (e.g., Roberts, Andrews, Lewinsohn, & Hops, 1990) and have been associated with an increased risk of functional impairment and psychiatric disorder (Broadhead, Blazer, George, & Tse, 1990; Fergusson, Horwood, Ridder, & Beautrais, 2005; Lewinsohn, Solomon, Seeley, & Zeiss, 2000).
The epidemiology of depression has consistently demonstrated that, beginning in early adolescence and continuing across the lifespan, females experience significantly more depression than males in both severity and frequency (e.g., Eaton et al., 1997; Hankin, Mermelstein, & Roesch, 2007; Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993; Nolen-Hoeksema & Hilt, 2009). However, relatively little research or theory has addressed the developmental mechanisms through which adolescent girls come to be at greater risk than boys (Peterson, Sargiani, & Kennedy, 1991). Particularly little is known about gender differences in offspring vulnerability to the adverse effects of parental depression (for review, see Sheeber, Davis, & Hops, 2002). Indeed, the majority of intergenerational depression research has focused exclusively on boys or analyzed boys and girls together (Connell & Goodman, 2002). Of the investigations which have examined offspring gender in relation to fathers’ depression and offspring outcomes, results have been equivocal. Cross –sectional findings from several studies have indicated that, relative to boys, adolescent daughters of mothers or fathers with psychopathology may be at elevated risk for depression (Bosco, Rent, Dinger, Epstein, & Phares, 2003; Davies & Windle, 1997). In contrast, Eberhart, Shih, Hammen, and Brennan (2006) found that the likelihood of adolescent girls being currently depressed was unrelated to paternal depression, whereas adolescent boys were more likely to be currently depressed if their father had a history of depression. Other research has found no gender differences in the functioning of male and female offspring as a consequence of paternal depression (e.g., Currier, Mann, Oquendo, Galfalvy, & Mann, 2006).
Psychosocial perspectives on adolescent depression suggest that interpersonal orientation and the development of gender – related role socialization during early adolescence may contribute to higher rates of depression among females, leaving them ill– equipped to cope with the stresses of adolescence (Feingold, 1994; Hops, 1996). Hill and Lynch (1983) proposed that during adolescence, girls begin to identify more strongly with stereotypically feminine stereotypes which reflect strong investment in social relationships and increased expression of depressive behaviors. Compared to males, females may invest more in their relationships and develop stronger emotional ties to their family and friends, thus strengthening their social support networks and buffering against adversity (Nolen–Hoeksema, 2000). However, interpersonal orientations may leave adolescent girls more vulnerable to the emotional consequences of interpersonal stressors when they do occur (Ge et al., 1994). Taken together, findings suggest that gender may play an important role in the associations between parental depression, intrafamilial processes, and adolescent adjustment.
Paternal Depression and Offspring Adjustment
Fathers continue to be considered relatively unimportant in research on children’s social-emotional development (Phares, Fields, Kamboukos, & Lopez, 2005), but their contribution is increasingly being addressed and understood. It is now clear, for example, that a substantial number of men experience depressive disorders (Blazer, Kessler, McGonagle, & Swartz, 1994) and that these disorders contribute to children’s psychopathology beyond that explained by maternal depression (e.g., Marchand & Hock, 1998). Two recent meta-analyses have examined the relation between depression in fathers and offspring outcomes. Connell and Goodman (2002) analyzed data from 134 independent samples and found that externalizing problems in children were equally related to psychopathology in mothers and fathers, whereas children’s internalizing problems were more closely related to maternal psychopathology. Using a sample of 40 studies of paternal depression, child psychopathology, and parent-offspring relations, meta-analytic findings from Kane and Garber (2004) indicated that paternal depression was significantly related to children’s emotional and behavioral disorders and to father-offspring conflict.
Within the extant literature on children of depressed fathers, several important gaps have been identified. First, with several notable exceptions (Goodman, Brogan, Lynch, & Fielding, 1993; Marchand & Hock, 1998; Thomas & Forehand, 1991), studies of offspring of depressed fathers have failed to statistically control for the potentially confounding effects of maternal depression. Another limitation of previous research on paternal depression is that the majority of studies have assessed concurrent relations between paternal and child functioning (Hammen, 2008), thus limiting inferences about causal sequences and direction of effect. Of the few existing longitudinal studies of paternal depression, most have not controlled for initial levels of child psychopathology (e.g., Carro, Grant, Gotlib, & Compas, 1993). Finally, and perhaps most importantly, little is known about the underlying processes of risk in offspring of depressed fathers or about individual or family factors associated with better or worse outcomes (Kane & Garber, 2004).
The Family Context and Intergenerational Depression
Family systems theories (e.g., Becvar & Becvar, 1993; Cox & Paley, 1997, 2003) focus on family relationships as opposed to individual characteristics. Given the transactional and interpersonal nature of depression in families (Kaslow, Deering, & Racusin, 1994), this emphasis on interactive processes and reciprocity has guided recent theory and research on intergenerational depression transmission. In fact, a central theme in contemporary theoretical models of intergenerational depression is the idea that parental depression occurs in an environment of adverse family factors such as cold, hostile intrafamilial relationships (e.g., Gotlib & Goodman, 2002; Hammen et al., 2004). Within these models, characteristics of family functioning have been conceptualized and studied as moderators of offspring risk. For example, family support, warmth, and approval have been shown to serve as protective factors against the adverse effects of maternal depression on children’s development (e.g., Luthar & Zigler, 1991; Pavlidis & McCauley, 2001).
Compared to maternal depression, considerably less attention has been given to the intrafamilial contexts under which fathers’ depression may have more or less of an effect on offspring functioning. When characteristics of the father have been included in models of risk in offspring of depressed parents, they have typically been considered strictly as moderators of the association between maternal depressive problems and offspring adjustment (e.g., Mezulis et al., 2004; Tannenbaum & Forehand, 1994; Teti & Gelfand, 1991). Some recent work has considered characteristics of the father-child relationship as moderators of the longitudinal association between father and child functioning (e.g., Reeb, Conger, & Wu, 2010), although, to our knowledge, no studies to date have examined whether mother-adolescent relations may modify offspring risk as a consequence of paternal depression or depressive symptoms. This issue is a central question for the present paper.
Present Study
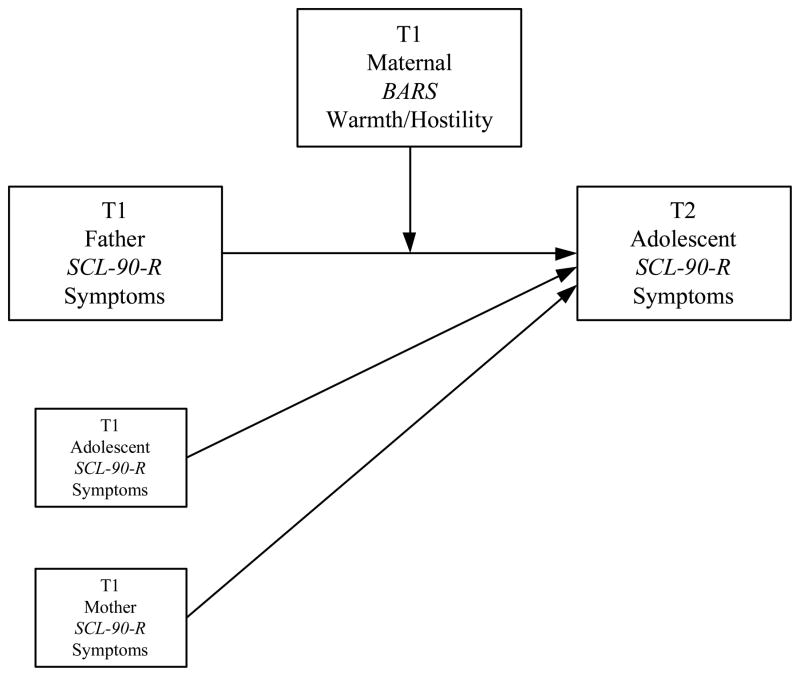
Prospective, longitudinal data from a large nonclinical sample were used to address the study goals. Controlling for maternal depressive symptoms and prior adolescent depressive symptoms, we evaluated adolescent perceptions of maternal warmth and hostility as moderators of the association between fathers’ depressive symptoms and subsequent adolescent depressive symptoms (see Figure 1). Adolescent gender was examined as a moderator of the interactive effect of paternal depressive symptoms and maternal behavior (warmth or hostility) in predicting adolescent outcomes (i.e., the three-way interaction of Paternal Depressive Symptoms × Maternal Behavior × Gender). We predicted that adolescents’ negative perceptions of mothers’ behavior would moderate the association between paternal and adolescent depressed mood such that low maternal warmth (H1) or high maternal hostility (H2) would increase adolescent risk in relation to paternal depressive symptoms. Second, we hypothesized that girls would be more depressed than boys as a function of paternal depressive symptoms when maternal warmth was low or when maternal hostility was high (H3).
Figure 1.
Conceptual model of maternal warmth and hostility as moderators of the association between Time 1 paternal depressed mood and Time 2 adolescent depressed mood.
Method
Participants and Procedures
The sample includes 451 adolescents (236 female, 215 male) from two-parent intact families in rural Iowa. The study began in 1989 (Time 1) when the adolescents were in the 7th grade and averaged 13.2 years of age. Participants were from predominately middle- and lower-middle-class families who resided on farms (34%), in non-farm rural areas (12%), or in small towns (54%). Families were eligible for the study if the 7th grader was living with both biological parents. Due to the ethnic composition of the area, all families were European-American. Of the original 451 families, approximately 95% of the sample remained in the study one year later when the adolescents were in 8th grade (Time 2). No significant differences in parents’ age, family income, or mothers’ level of education were found between participants remaining in the study (N = 424) compared to those who dropped out. Fathers not in the analyses at Time 2 averaged 12.74 years of education compared to 13.57 for those who remained in the study, a statistically significant difference (p < .05). Families not included in the analyses did not demonstrate significant differences in levels of depressive symptoms.
Measures
Depressive symptoms
Parent and adolescent depressive symptoms were assessed using the self-reported 13-item depression subscale of the Symptom Checklist-90-Revised (SCL-90-R; Derogatis, 1983), which has demonstrated reliability and validity in many studies of adults and adolescents (e.g., Essau, 2004). In our sample, internal consistencies for SCL-90-R depression were satisfactory at Time 1 (fathers α = .81; mothers α = .87; adolescents α = .88) and Time 2 (adolescents α = .94). Raw score means for fathers (M = .45, SD = .42) and mothers (M = .60, SD = .50) were somewhat higher than the mean for the normative non-patient sample (M = .36, SD = .44) reported by Derogatis (1983). Adolescent depressive symptoms at Time 1 for boys (M = .57, SD = .54) were not statistically different from those of girls (M = .67, SD = .63). At Time 2, girls’ symptoms (M = .56, SD = .48) were significantly higher than those of boys (M = .42, SD = .45); t (1) = 3.05 (p < .001). Over the course of the study, adolescents’ raw score means for the depression subscale were slightly lower than the score of 0.80 and standard deviation of 0.69 reported for the normative sample in the SCL-90-R manual (Derogatis, 1983).
Maternal hostility
Adolescent perceptions of paternal hostility were assessed at Time 1 using Conger’s (1989) Behavioral Affect Rating Scale, or BARS. This scale has demonstrated validity and reliability across multiple reporters and diverse samples (e.g., see Conger, Ebert-Wallace, Sun, Simons, McLoyd, & Brody, 2002). Each adolescent reported how often his or her mother in the study behaved in an angry or hostile fashion towards them during the previous month. On a 7-point scale, responses range from 1 (never) to 7 (always) on items such as “how often does she ignore you when you try to talk to her”, “how often does she try to make you feel guilty”, and “how often does she criticize you or your ideas”. The 12 items were averaged into a composite score; higher scores indicated higher hostility (α = .91).
Maternal warmth
Adolescent perceptions of maternal warmth were also assessed at Time 1 using the BARS (Conger, 1989). Each adolescent reported how often his or her mother in the study behaved in a warm or supportive way towards them during the previous month. Responses range from 1 (never) to 7 (always) on items such as “how often does she listen carefully to your point of view”, “how often does she let you know she really cares about you”, and “how often does she act loving and affectionate towards you”. The eight items were averaged into a composite and higher composite scores indicated higher warmth (α = .87).
Results
Correlations among the major variables used in this study are presented in Table 1. As expected, previous adolescent depressive symptoms and maternal hostility were positively associated with Time 2 adolescent depressive symptoms. Maternal warmth was negatively associated with adolescent girls’ and boys’ depressive symptoms; however, the correlation reached statistical significance only for adolescent girls at Time 2. Paternal depressive symptoms were positively correlated with adolescent girls’ subsequent depressive symptoms, whereas maternal depressive symptoms were positively associated with adolescent boys’ symptoms.
Table 1.
Correlations, Means, and Standard Deviations
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | M | SD |
|---|---|---|---|---|---|---|---|---|
| 1. T1 adolescent depressive symptoms | — | .13* | .05 | −.30** | .35** | .52** | .67 | .63 |
| 2. T1 Maternal depressive symptoms | .26** | — | .09 | −.10 | .17* | .10 | .59 | .48 |
| 3. T1 Paternal depressive symptoms | .11 | .06 | — | −.04 | .01 | .18** | .47 | .43 |
| 4. T1 Maternal warmth | −.24** | −.05 | −.03 | — | −.41** | −.14* | 5.42 | 1.04 |
| 5. T1 Maternal hostility | .41** | .13 | .02 | −.45** | — | .16* | 2.32 | .94 |
| 6. T2 Adolescent depressive symptoms | .43** | .33** | −.01 | −.14 | .23** | — | .56 | .48 |
| M | .57 | .61 | .43 | 5.21 | 2.55 | .42 | — | — |
| SD | .54 | .52 | .42 | .91 | .93 | .45 | — | — |
Note. Girls above diagonal, boys below
p < .05,
p < .01
To test for moderating effects of maternal behavior, hierarchical multiple regression analyses were conducted using PASW 18 statistical software (Allen & Bennett, 2010). This allowed us to examine the unique contribution of each independent variable to Time 2 adolescent depressive symptoms while taking into account the relationships among them. In all analyses, previous adolescent depressive symptoms, maternal depressive symptoms, and fathers’ warmth and hostility (BARS) were entered first as covariates in order to establish temporal precedence and remove spurious sources of association between father and adolescent functioning. Demographic measures including per capita family income, parental age, and parental education were also included as statistical controls in all analyses due to their potential to influence adolescent depression (Lorant et al., 2003). The demographic and paternal behavior covariates did not produce significant effects in any equations and, for the sake of brevity, are excluded from reported analyses. In all analyses, continuous independent variables were grand mean centered and gender was coded as 0 for female and 1 for male.
It could be argued that warmth and hostility are at opposite ends of a single dimension, however, we analyzed the constructs separately, as research has shown that they are distinct constructs that may have differential associations with mental health functioning (Barrera, Chassin, & Rogosch, 1993). In this sample, maternal warmth and hostility were modestly correlated (r = −.41 to −.45) indicating the expected association but not a large overlap. Furthermore, by evaluating the contributions of warmth or hostility separately, we can compare our results with previous research that has considered the role of family support and warmth (e.g., Luthar & Zigler, 1991; Pavlidis & McCauley, 2001), and also consider the risk conferred by hostility between parent and adolescent, such as that discussed by Gotlib and Goodman (2002). Nine effects were tested in each full equation: five main effects (Previous Adolescent Depressive Symptoms, Maternal Depressive Symptoms, Gender, Maternal Warmth or Hostility, and Paternal Depressive Symptoms), three two-way interactions (Paternal Depressive Symptoms × Gender, Paternal Depressive Symptoms × Maternal Warmth or Hostility, and Maternal Warmth or Hostility × Gender), and the Paternal Depressive Symptoms × Maternal Warmth or Hostility × Gender three-way interaction.
Regression parameter estimates for the maternal warmth equation are reported in Table 2. In Model 1, Time 2 adolescent depressive symptoms were regressed on Time 1 adolescent depressive symptoms and Time 1 maternal depressive symptoms. Both covariates were statistically significant and collectively explained 24.5% of the variance in Time 2 adolescent depressive symptoms. In the full model, adolescent gender, maternal warmth, and paternal depressive symptoms were entered (ΔR2 = .046*). As expected, adolescent girls reported significantly more symptoms than did boys and paternal depressive symptoms were associated with adolescent depressive symptoms. The Paternal Depressive Symptoms × Gender interaction term was significant, indicating that adolescent girls were more susceptible to the adverse effects of paternal depressive symptoms on offspring psychological well-being. The adverse effect of paternal depressive symptoms on adolescent outcome also varied as a function of maternal warmth; adolescents reporting low levels of maternal warmth were at particular risk in relation to paternal depressive symptoms.
Table 2.
Hierarchical Multiple Regression Analyses Predicting Time 2 Adolescent Depressive Symptoms from Gender, Maternal Warmth, and Paternal Depressive Symptoms
| Independent Variables | β | SE | b |
|---|---|---|---|
| Model 1 [R2= .245; F (9, 406) = 14.63***] | |||
| Control variables | |||
| Constant | .020 | .489 | |
| Previous Adolescent Depressive Symptoms | .457*** | .037 | .362 |
| Maternal Depressive Symptoms | .097* | .042 | .091 |
| Model 2 [R2= .291; F (16, 399) = 10.25***; ΔR2 = .046*] | |||
| Full equation | |||
| Constant | .028 | .524 | |
| Previous Adolescent Depressive Symptoms | .441*** | .037 | .349 |
| Maternal Depressive Symptoms | .100* | .042 | .095 |
| Gender (male = 1) | −.096* | .041 | −.090 |
| Maternal Warmth | .097 | .037 | .047 |
| Paternal Depressive Symptoms | .177** | .064 | .195 |
| Maternal Warmth × Gender | −.052 | .042 | −.040 |
| Paternal Symptoms × Gender | −.153** | .095 | −.247 |
| Paternal Symptoms × Maternal Warmth | −.185** | .065 | −.211 |
| Paternal Symptoms by × Warmth × Gender | .124* | .106 | .250 |
p < .05.
p < .01.
p < .001.
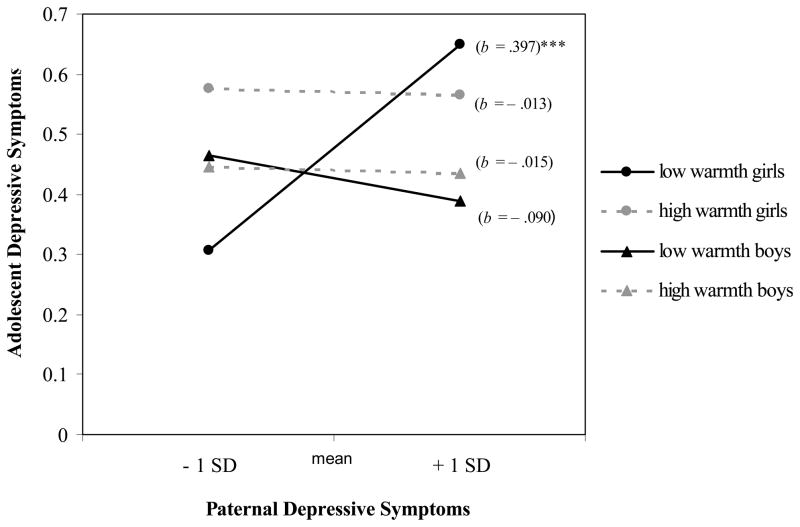
Finally, the Paternal Depressive Symptoms × Maternal Warmth × Gender three-way interaction variable was statistically significant. As suggested by Holmbeck (2002), post-hoc probing was conducted in which simple regression equations were generated, one at each of the four combinations of adolescent gender and maternal warmth at one standard deviation above and below the mean (see Figure 2). Significance tests demonstrated that only the slope for girls experiencing low maternal warmth was significantly different from zero, the direction indicating that adolescent girls’ functioning was notably more impaired as a function of paternal depressive symptoms when maternal warmth was low.
Figure 2.
Time 2 adolescent depressive symptoms as a function of paternal depressive symptoms, maternal warmth, and gender.
Note. SD = standard deviation, b = unstandardized regression coefficient.
* p < .05, ** p < .01, *** p < .001
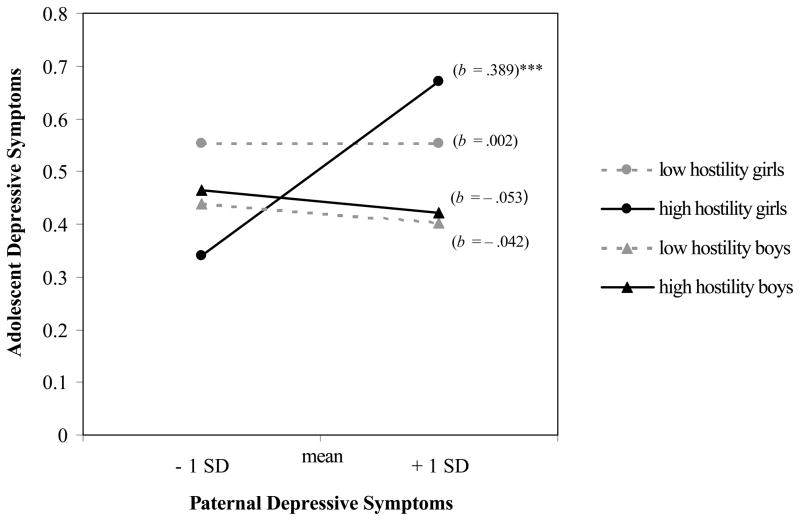
Regression models for the maternal hostility equation are reported in Table 3. In Model 1, the main effects for previous adolescent depressive symptoms and maternal depressive symptoms were both strong predictors of Time 2 adolescent depressive symptoms (R2 = .245***). Gender, paternal depressive symptoms, and maternal warmth were added in Model 2, resulting in a significant change in variance explained (ΔR2 = .042*). In this model, the main effects for gender and paternal depressive symptoms reached statistical significance. The two-way interaction between paternal depressive symptoms and adolescent gender was also significant, the direction indicating that compared to boys, adolescent girls’ experienced more depressive symptoms as a function of fathers’ depressive symptoms. The Paternal Symptoms × Maternal Hostility interaction variable also reached statistical significance; the magnitude of the adverse effect of paternal depressive symptoms on adolescent depressive was elevated among adolescents reporting high maternal hostility. The Paternal Depressive Symptoms × Maternal Hostility × Gender variable was significant. Post-hoc regression lines for each simple slope are plotted in Figure 3 and indicate a significant relation between Time 1 paternal depressive symptoms and Time 2 adolescent depressive symptoms among girls reporting high maternal hostility.
Table 3.
Hierarchical Multiple Regression Analyses Predicting Time 2 Adolescent Depressive Symptoms from Gender, Maternal Hostility, and Paternal Depressive Symptoms
| Independent Variables | β | SE | b |
|---|---|---|---|
| Model 1 [R2= .245; F (9, 406) = 14.63***] | |||
| Control variables | |||
| Constant | .020 | .489 | |
| Previous Adolescent Depressive Symptoms | .457*** | .037 | .362 |
| Maternal Depressive Symptoms | .097* | .042 | .091 |
| Model 2 [R2= .287; F (16, 399) = 10.03***; ΔR2 = .042*] | |||
| Full equation | |||
| Constant | .028 | .529 | |
| Previous Adolescent Depressive Symptoms | .433*** | .038 | .343 |
| Maternal Depressive Symptoms | .094* | .042 | .089 |
| Gender (male = 1) | − .103* | .041 | −.097 |
| Maternal Hostility | − .052 | .033 | −.026 |
| Paternal Depressive Symptoms | .179** | .065 | .196 |
| Maternal Hostility × Gender | .051 | .043 | .038 |
| Paternal Symptoms × Gender | − .150* | .095 | −.243 |
| Paternal Symptoms × Maternal Hostility | .172** | .065 | .206 |
| Paternal Symptoms by × Hostility × Gender | − .106* | .108 | −.212 |
p < .05.
p < .01.
p < .001.
Figure 3.
Time 2 adolescent depressive symptoms as a function of paternal depressive symptoms, maternal hostility, and gender.
Note. SD = standard deviation, b = unstandardized regression coefficient.
* p < .05, ** p < .01, *** p < .001
Discussion
A central theme in contemporary models of intergenerational depression transmission is that parental depression occurs in an environment of adverse contextual and family factors which may contribute to children’s risk for depression. Research to date on children of depressed parents, however, has paid relatively little attention to factors which may reduce or elevate the adverse effects of parental depression on offspring outcomes (Connell & Goodman, 2002), especially in families with depressed fathers (Phares & Compas, 1992). Using these limitations as a guide, the present study examined the mother-adolescent relationship as a moderator of adolescent risk in relation to fathers’ depressive symptoms. Several interesting findings emerged regarding family processes and the intergenerational transmission of depressive symptoms. Consistent with our hypotheses, adolescents experiencing low maternal warmth (H1) or high maternal hostility (H2) were at increased risk as a consequence of paternal depressive symptoms. These conditional effects were particularly strong for adolescent girls (H3).
Findings from the present study can be considered in relation to the Integrative Model for the Transmission of Risk to Children of Depressed Mothers (Goodman, 2007; Goodman & Gotlib, 1999), which posits that characteristics of family relationships can moderate the impact of maternal depression on offspring functioning. Consistent with Connell and Goodman’s (2002) proposition that several parameters of this developmental model can reasonably be applied to children of depressed fathers, adolescents in our data reporting low maternal warmth or high maternal hostility were particularly vulnerable to the adverse effects of paternal depressive symptoms. Some evidence has indicated that adversity in the mother-child relationship plays a key role in the intergenerational transmission of depression (see Downey & Coyne, 1990), but this work has typically failed to examine factors associated with better or worse outcomes in children of depressed fathers (Phares et al., 2005). An important task for future research will be to evaluate the processes underlying the conditional effects of paternal depressive symptoms on adolescent adjustment found in the current study.
Compared to boys, adolescent females experienced more risk in relation to paternal depressive symptoms when experiencing adversity in the mother-adolescent relationship. Adolescent girls are socialized to place more value on interpersonal relationships (Hill & Lynch, 1983) and tend to be more interpersonally oriented than are boys (for commentary, see Hops, 1996), which may contribute, in part, to this finding. Our results can also be considered in relation to Bosco et al. (2003), who reported that daughters, and not sons, exhibited higher internalizing behaviors when there was a greater negative perception of both fathers and mothers, along with higher levels of parental psychopathology. These findings were cross-sectional, however, and focused on the additive, rather than interactive effect of family relationship quality and parental depression. Overall, little is known about gender – specific risk in offspring of depressed parents (Sheeber et al., 2002).
In the current study, the main effects of parental warmth and hostility on subsequent adolescent depressive symptoms were not statistically significant. This was surprising, considering that parent – adolescent relationship difficulties and adverse family environments characterized by elevated hostility and critical interactions have been consistently associated with adolescent maladjustment (Conger et al., 1993; Sheeber, Hops, & Davis, 2001). However, despite the lack of a direct effect, adversity in the mother-adolescent relationship did have important implications for adolescent functioning among offspring whose fathers reported high levels of depressive symptoms. The significant interaction effects also qualify another interesting finding from the current study. That is, mean level depressive symptoms decreased for adolescent girls and boys over the course of the study (a one year period). It must be noted that depressive symptoms increased for a significant subset of adolescents, and, it may be that these adolescents are at increased risk for adjustment problems as they move into later adolescence.
There were important limitations to this study that should be considered in future research. First, we examined associations between adolescents’ subjective experiences within the family and self-reported depressive symptoms. Shared method variance is always a concern when a single reporter provides information for multiple constructs as moderators of risk in relation to paternal depressive symptoms. However, our results are consistent with a number of cross-sectional studies which have associated adolescents’ negative evaluations of the parent-child relationship with increased risk for depression (e.g., Plunkett, Henry, Robinson, Behnke, & Falcon, 2007; Sheeber, Davis, Leve, Hops, & Tildesley, 2007). Moreover, previous findings have demonstrated that offspring perceptions of family relations often do not correlate with parent or observer report (e.g., Cook & Goldstein, 1993) but are strongly related to their psychological adjustment (Forehand & Nousiainen, 1993) suggesting that individual perceptions contribute to our understanding of adolescent adjustment. Another task of future research will be to explore the implications of observer-rating and other family members’ perspectives in relation to paternal depression, family relationships, and adolescent functioning. Next, given the relatively low levels of symptoms reported from this rural community sample of early adolescents, the results may not generalize to urban or clinical populations or to older adolescents. Finally, only families of European decent were included. Replication of these results with more diverse samples, including single-parent, same-sex, urban, and minority families is needed.
Conclusion
The longitudinal findings reported here highlight the importance of including fathers in developmental research and add to our understanding of the psychosocial processes by which depression runs in families. Our findings indicate a complex, longitudinal association between paternal mental health, offspring gender, maternal behavior, and adolescent psychological well-being. Continued research of this type may ultimately have valuable applied implications, as research has shown that data-driven, family-level interventions for families with depressed parents are effective and available (e.g., Garber et al., 2009). It may be particularly important to help depressed fathers recognize their psychological problems and pay attention to the mother-daughter relationship as a moderator of adolescent risk. From another perspective, by increasing positive involvement or reducing conflict with their adolescent children, mothers may be able to help compensate for some of the negative consequences of paternal depressed mood.
Acknowledgments
This research is currently supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute of Mental Health (HD064687, HD051746, and MH051361). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Support for earlier years of the study also came from multiple sources, including the National Institute of Mental Health (MH00567, MH19734, MH43270, MH59355, MH62989, and MH48165), the National Institute on Drug Abuse (DA05347), the National Institute of Child Health and Human Development (HD027724, HD047573), the Bureau of Maternal and Child Health (MCJ-109572), and the MacArthur Foundation Research Network on Successful Adolescent Development Among Youth in High-Risk Settings.
References
- Allen PJ, Bennett K. PASW statistics by SPSS: Version 18.0. South Melbourne: Cengage Learning; 2010. [Google Scholar]
- Barrera M, Chassin LL, Rogosch F. Effects of social support and conflict on adolescent children of alcoholic and nonalcoholic fathers. Journal of Personality and Social Psychology. 1993;64:602–612. doi: 10.1037//0022-3514.64.4.602. [DOI] [PubMed] [Google Scholar]
- Becvar DS, Becvar RJ. Storytelling and family therapy. The American Journal of Family Therapy. 1993;21(2):145–160. [Google Scholar]
- Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: The National Comorbidity Survey. American Journal of Psychiatry. 1994;151(7):979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Bosco GL, Renk K, Dinger TM, Epstein MK, Phares V. The connections between adolescents' perceptions of parents, parental psychological symptoms, and adolescent functioning. Journal of Applied Developmental Psychology. 2003;24:179–200. [Google Scholar]
- Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiological survey. Journal of the American Medical Association. 1990;264:2524–2528. [PubMed] [Google Scholar]
- Carro MG, Grant KE, Gotlib IH, Compas BE. Postpartum depression and child development: An investigation of mothers and fathers as sources of risk and resilience. Development and Psychopathology Special Issue: Milestones in the development of resilience. 1993;5(4):567–579. [Google Scholar]
- Chang JJ, Halpern CT, Kaufman JS. Maternal Depressive Symptoms, Father's Involvement, and the Trajectories of Child Problem Behaviors in a US National Sample. Archives of Pediatric & Adolescent Medicine. 2007;161:697–703. doi: 10.1001/archpedi.161.7.697. [DOI] [PubMed] [Google Scholar]
- Conger RD. Created for Iowa Youth and Families Project. Iowa State University; Ames, Iowa: 1989. Behavioral affect rating scale: Adolescent perception of maternal hostility. [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Lorenz FO, Simons RL, Whitbeck LB. Family economic stress and adjustment of early adolescent girls. Developmental Psychology. 1993;29:206–219. [Google Scholar]
- Conger RD, Ebert-Wallace L, Sun Y, Simons RL, McLoyd VC, Brody GH. Economic pressure in African American families: A replication and extension of the Family Stress Model. Developmental Psychology. 2002;38:179–193. [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Cook WL, Goldstein MJ. Multiple perspectives on family relationships: A latent variables model. Child Development. 1993;64:1377–1388. doi: 10.1111/j.1467-8624.1993.tb02958.x. [DOI] [PubMed] [Google Scholar]
- Costello C. Psychopathology in the clinic and in the community. In: Costello C, editor. Basic issues in psychopathology. New York: Guilford Press; 1993. pp. 67–102. [Google Scholar]
- Costello EJ, Foley DL, Angold A. 10 year research update review: The epidemiology of child and adolescent psychiatric disorders II: Developmental epidemiology. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Cox MJ, Paley B. Understanding families as systems. Current Directions in Psychological Science. 2003;12(5):193–196. [Google Scholar]
- Cox MJ, Paley B. Families as systems. Annual Review of Psychology. 1997;48:243–267. doi: 10.1146/annurev.psych.48.1.243. [DOI] [PubMed] [Google Scholar]
- Currier D, Mann MJ, Oquendo MA, Galfalvy H, Mann JJ. Sex differences in the familial transmission of mood disorders. Journal of Affective Disorders. 2006;95:51–60. doi: 10.1016/j.jad.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Derogatis L. SCL-90-R administration, scoring, and procedures Manual II. Townsen, MD: Clinical Psychometric Research; 1983. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Eberhart NK, Shih JH, Hammen CL, Brennan PA. Understanding the sex difference in vulnerability to adolescent depression: An examination of child and parent characteristics. Journal of Abnormal Child Psychology. 2006;34:493–506. doi: 10.1007/s10802-006-9020-4. [DOI] [PubMed] [Google Scholar]
- Feingold A. Gender differences in personality: A meta– analysis. Psychological Bulletin. 1994;116:429–456. doi: 10.1037/0033-2909.116.3.429. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Forehand R, Nousiainen S. Maternal and paternal parenting: Critical dimensions in adolescent functioning. Journal of Family Psychology. 1993;7:213–221. [Google Scholar]
- Garber J, Clarke GN, Weersing R, Beardslee WR, Brent DA, Gladstone TRG, Iyengar S. Prevention of depression in at-risk Adolescents: A randomized controlled trial. JAMA. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgiades K, Lewinsohn PM, Monroe SM, Seeley JR. Major depressive disorder in adolescence: The role of subthreshold symptoms. Journal of American Academy of Child and Adolescent Psychiatry. 2006;45:936–944. doi: 10.1097/01.chi.0000223313.25536.47. [DOI] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Brogan D, Lynch ME, Fielding B. Social and emotional competence in children of depressed mothers. Child Development. 1993;64(2):516–531. doi: 10.1111/j.1467-8624.1993.tb02925.x. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH, editors. Children of depressed parents: Alternative pathways to risk for psychopathology. Washington, D.C: American Psychological Association; 2002. [Google Scholar]
- Gotlib IH, Goodman SH. Introduction. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. pp. 2003–2009. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Consequences of depression during adolescence: Marital status and marital functioning in early adulthood. Journal of Abnormal Psychology. 1998;107:686–690. doi: 10.1037//0021-843x.107.4.686. [DOI] [PubMed] [Google Scholar]
- Hammen CL, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hammen CL. Children of depressed parents. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford Press; 2008. pp. 275–297. [Google Scholar]
- Hankin BL, Mermelstein R, Roesch L. Sex differences in adolescent depression: Stress exposure and reactivity models. Child Development. 2007;78:279–295. doi: 10.1111/j.1467-8624.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- Harrington R, Dubicka B. Natural history of mood disorders in children and adolescents. In: Goodyer IM, editor. The depressed child and adolescent. New York: Cambridge University Press; 2001. pp. 2353–2381. [Google Scholar]
- Hill JP, Lynch ME. The intensification of gender-related role expectations during early adolescence. In: Brooks-Gunn J, Petersen A, editors. Girls at puberty. New York: Plenum Press; 1983. pp. 201–228. [Google Scholar]
- Holmbeck GM. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hops H. Intergenerational transmission of depressive symptoms: Gender and developmental considerations. In: Mundt C, Goldstein M, Hahlweg K, Fiedler P, editors. Interpersonal factors in the origin and course of affective disorders. London: Royal College of Psychiatrists; 1996. pp. 113–129. [Google Scholar]
- Kane P, Garber J. The relations among depression in fathers, children’s psychopathology, and father-child conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kaslow NJ, Deering CG, Racusin GR. Depressed children and their families. Clinical Psychology Review. 1994;14:39–59. [Google Scholar]
- Kaslow NJ, Warner V, John K, Brown R. Intra-informant agreement and family functioning in depressed and nondepressed parents and their children. American Journal of Family Therapy. 1992;20:204–217. [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Essau CA. Depression in adolescents. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford Press; 2002. pp. 2541–2559. [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review. 1998;18:765–794. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications and “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109:345–351. [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Low SM, Stocker C. Family functioning and children’s adjustment: Associations among parents’ depressed mood, marital hostility, parent –child –hostility, and children’s adjustment. Journal of Family Psychology. 2005;19:394–403. doi: 10.1037/0893-3200.19.3.394. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Zigler E. Vulnerability and competence: A review of research on resilience in childhood. American Journal of Orthopsychiatry. 1991;61:6–22. doi: 10.1037/h0079218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand JF, Hock E. The relation of problem behaviors in preschool children to depressive symptoms in mothers and fathers. Journal of Genetic Psychology. 1998;159(3):353–366. doi: 10.1080/00221329809596157. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Hyde JS, Clark R. Father involvement moderates the effect of maternal depression during a child's infancy on child behavior problems in kindergarten. Journal of Family Psychology. 2004;18:575–588. doi: 10.1037/0893-3200.18.4.575. [DOI] [PubMed] [Google Scholar]
- Nolen–Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109:504–511. [PubMed] [Google Scholar]
- Nolen Hoeksema S, Hilt LM. Gender differences in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: Guilford Press; 2009. pp. 2386–2404. [Google Scholar]
- Pavlidis K, McCauley E. Autonomy and relatedness in family interactions with depressed adolescents. Journal of Abnormal Child Psychology. 2001;29:11–21. doi: 10.1023/a:1005295328151. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Sargiani PA, Kennedy RE. Adolescent depression: Why more girls? Journal of Youth and Adolescence. 1991;20:247–271. doi: 10.1007/BF01537611. [DOI] [PubMed] [Google Scholar]
- Phares V. Psychological adjustment, maladjustment, and father-child relationships. In: Lamb M, editor. The role of the father in child development. New York: Wiley; 1997. pp. 261–283. [Google Scholar]
- Phares V, Compas BE. The role of fathers in child and adolescent psychopathology: Make room for daddy. Psychological Bulletin. 1992;111:387–412. doi: 10.1037/0033-2909.111.3.387. [DOI] [PubMed] [Google Scholar]
- Phares V, Duhig AM, Watkins MM. Family context: fathers and other supports. In: Goodman SH, Gotlib IH, editors. Children of Depressed Parents: Mechanisms of Risk and Implications for Treatment. Washington, DC: American Psychological Association; 2002. pp. 203–225. [Google Scholar]
- Phares V, Fields S, Kamboukos D, Lopez E. Still looking for poppa. American Psychologist. 2005;60:735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- Plunkett SW, Henry CS, Robinson LC, Behnke A, Falcon PC. Adolescent perceptions of parental behaviors, adolescent self-esteem, and adolescent depressed mood. Journal of Child and Family Studies. 2007;16:760–772. [Google Scholar]
- Ramchandani PG, O’Connor GO, Evans J, Heron J, Murray L, Stein A. The effects of pre- and postnatal depression in fathers: A natural experiment comparing the effects of exposure to depression on offspring. Journal of Child Psychology and Psychiatry. 2008;49:1069–1078. doi: 10.1111/j.1469-7610.2008.02000.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeb BT, Conger KJ, Wu EY. Paternal depressive symptoms and adolescent functioning: The moderating effect of gender and father hostility. Fathering: A Journal of Theory, Research, and Practice about Men as Fathers. 2010;8(1):131–142. doi: 10.3149/fth.0801.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2:122–128. [Google Scholar]
- Rohde P, Lewinsohn PM, Klein DN, Seeley JR. Association of parental depression with psychiatric course from adolescence to young adulthood among formerly depressed individuals. Journal of Abnormal Psychology. 2005;114:409–420. doi: 10.1037/0021-843X.114.3.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber LB, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. pp. 253–274. [Google Scholar]
- Sheeber LB, Davis B, Leve C, Hops H, Tildesley E. Adolescents’ relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber LB, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Tannenbaum L, Forehand R. Maternal depressive mood: The role of the father in preventing adolescent problem behaviors. Behaviour Research and Therapy. 1994;32:321–325. doi: 10.1016/0005-7967(94)90129-5. [DOI] [PubMed] [Google Scholar]
- Teti DM, Gelfand DM. Behavioral competence among mothers of infants in the first year: The mediational role of maternal self-efficacy. Child Development. 1991;62:918–929. doi: 10.1111/j.1467-8624.1991.tb01580.x. [DOI] [PubMed] [Google Scholar]
- Thomas AM, Forehand R. The relationship between paternal depressive mood and early adolescent functioning. Journal of Family Psychology. 1991;4:43–52. [Google Scholar]