Abstract
Objectives: To date, methodologies are lacking that address a holistic assessment of wellness in older adults. Technology applications may provide a platform for such an assessment, but have not been validated. We set out to demonstrate whether e-health applications could support the assessment of older adults' wellness in community-dwelling older adults. Materials and Methods: Twenty-seven residents of independent retirement community were followed over 8 weeks. Subjects engaged in the use of diverse technologies to assess cognitive performance, physiological and functional variables, as well as psychometric components of wellness. Data were integrated from various e-health sources into one study database. Correlations were assessed between different parameters, and hierarchical cluster analysis was used to explore the validity of the wellness model. Results: We found strong associations across multiple parameters of wellness within the conceptual model, including cognitive, functional, and physical. However, spirituality did not correlate with any other parameter studied in contrast to prior studies of older adults. Participants expressed overall positive attitudes toward the e-health tools and the holistic approach to the assessment of wellness, without expressing any privacy concerns. Conclusions: Parameters were highly correlated across multiple domains of wellness. Important clusters were noted to be formed across cognitive and physiological domains, giving further evidence of need for an integrated approach to the assessment of wellness. This finding warrants further replication in larger and more diverse samples of older adults to standardize and deploy these technologies across population groups.
Key words: aging, informatics, wellness, assessment
Introduction
To help older adults remain independent, clinicians' emphasis is on predicting and, if possible, minimizing progression of chronic disease and declines in overall health. Several efforts have been developed to address a single aspect of health; however, to support aging in place, a holistic approach to assessment of older adults' well-being and health is needed. To date, methodologies are lacking that address the holistic and multidimensional assessment of health and wellness. The challenge in taking this approach is to assess and integrate various data sources to provide a comprehensive assessment of older adults' health. A further challenge is then to customize such assessment based on individual healthcare needs.
Halbert Dunn originally defined wellness as “an integrated method for functioning which is oriented toward maximizing the potential of which the individual is capable. It requires that the individual maintain a continuum of balance and purposeful direction within the environment where he/she is functioning.”1 Hoyman further explored the multidimensional nature of wellness by emphasizing that the person needs to be examined in their everyday milieu and suggested that four dimensions are addressed: (1) physical well-being/fitness; (2) mental and cognitive health; (3) social well-being; and (4) spiritual well-being.2 (For full discussion, please see Demiris et al.3) Our current study was work informed by this framework of wellness as we aimed to assess wellness holistically and examine how these four dimensions interrelate.
Variables or parameters of wellness have been explored pair-wise to assess how they may interrelate. For example, decline in functional status has been found to correlate with a decline in cognition in patients with Parkinson's disease and Alzheimer's disease.4 Similarly, a structured strength and balance training program in frail, cognitive impaired elderly long-term care residents improved both functional and cognitive ability.5 Social isolation has been found to be associated with slower recovery of systolic blood pressure post-task and higher cholesterol level in response to stress.6 Spirituality may also influence blood pressure, immune function, depression, and mortality.7 These are a few examples of an extensive body of literature that examines the relationship between two distinct heath and wellness parameters; however, to date there is a dearth of literature that has taken a holistic approach to assessment of health and wellness. As older adults have different and complex needs, the emphasis needs to be on a holistic, longitudinal assessment of multiple parameters for a comprehensive examination of one's well-being and potential barriers to wellness. Therefore, it is important to explore potential correlations between all parameters of wellness (including physiological, cognitive, social, spiritual, and functional variables) and gain insight into the integrated patterns of elder wellness over time.
Technology applications have the potential to introduce tools that enable nonobtrusive monitoring of multiple parameters and their progress over time, assess relationships among parameters, and, ultimately, ways to identify patterns and trends as well as cases where an immediate intervention may be needed. Technological advances and tools are enabling us to collect, store, and analyze ever-increasing amounts of multivariable clinical data. We aimed to explore the feasibility of e-health tools to assess and monitor health and wellness for older adults and assess their perceptions of the community-based information technology (IT) platform for wellness. In the present report, we created a system that utilizes diverse and innovative existing technologies to assess the physiological, cognitive, functional, spiritual, and social wellness of older adults. Through the use of an 8-week longitudinal design, we (1) assessed the ability of e-health applications to capture physiological, functional, cognitive, social, and spiritual parameters of wellness, (2) explored correlations between various wellness parameters, and (3) explored older adults' perceptions of the system.
Materials and Methods
All procedures were approved by the Institutional Review Board of the University of Washington and the participating facility.
Subjects and Setting
The setting for our pilot study was a retirement community in Seattle, Washington, which consists of a mix of approximately 150 private apartment homes for persons 62 and older. Within this facility a community room accessible to all residents was converted into a study room where the health IT tools were installed and all study procedures took place. The room was open to study participants Monday through Friday 8 am–5 pm.
E-health Tools
In the implementation of the system, we took a hardware/software agnostic or functional approach. Specifically, we were not interested in designing our own applications, but rather wanted to use commercially available products so that our efforts were spent on data integration and analysis. Our wellness platform integrated three existing components, a telehealth kiosk (a community health kiosk that assesses physiological parameters, WebQ (a survey design interface that allows for the administration of questionnaires assessing functional, social, and spiritual well-being), and CogniFit (a software application that assesses cognitive parameters).
The telehealth kiosk was the Health Station (Healthanywhere, Inc., Ottowa, ON, Canada), which provides users secure access to an individual profile with the ability to capture relevant vital sign data into a personal health record. The kiosk comes with standard wireless medical devices, namely, a blood pressure and heart rate monitor, glucometer, pulse oximeter, and weight scale. It operates over regular phone lines, digital subscriber lines (DSL), WiFi, and broadband. Each user who is registered with the system receives a unique magnetic strip identification card that is swiped to identify the resident before any session. Thus, the kiosk can be used by multiple users from a single location and provide personalized monitoring.
All questionnaires were administered using WebQ (Catalyst Web Tools, Seattle, WA), which is a tool for creating secure, online surveys that can be administered either anonymously or confidentially. Survey data are automatically collected and compiled, and are downloadable in several formats.
The cognitive assessment was performed using the Neuropsychological Examination–CogniFit Personal Coach (N-CPC; CogniFit, Inc., Yoqneam Ilit, Israel), a brain fitness Web-based software solution. This system includes a series of steps that enable the assessment and over time the improvement of several key cognitive abilities. This software system has been tested for reliability and validity between the system's assessment and the full Cambridge Neuropsychological Test Automated Battery (CANTAB).8 The software system has been used in a wide range of populations for research purposes including older adults with insomnia, mobility deficits, and older adults at risk for cognitive decline in addition to its widespread commercial use.8–11
Procedures and Measures
Information sessions were conducted at the facility asking for interested persons to provide contact information for follow-up screening. Those individuals who met the criteria were asked to attend an initial visit, which was scheduled in the study room at the participating facility. A more detailed assessment of eligibility was undertaken at that visit and informed consent was obtained. After consent, the subject was taught about the equipment and study procedures and completed baseline measures. This included having height and grip strength assessed by study personnel and completion of physiological/functional, social, spiritual, and cognitive assessments using the IT tools described previously (see Table 1 for a list of measures obtained and relationship to conceptual framework). These parameters, with the exception of height, were obtained again at study exit (8 weeks).
Table 1.
Concepts and Measurement of Older Adults' Wellness
| MEASURE | SOURCE/INSTRUMENT | FREQUENCY | |
|---|---|---|---|
| Functional/physiological Parameters | Activities of daily living | Self-Report (WebQ) Katz Instrument of activities of daily living (ADLs) |
At baseline and exit (8 weeks) |
| Instrumental activities of daily living | Self-report (WebQ) Lawton instrumental activities of daily living (IADLs) |
At baseline and exit (8 weeks) | |
| Health-related quality of life | Centers for Disease Control and Prevention Health–related Quality of Life-4 self-report (WebQ) | Monthly | |
| Blood pressure, weight, heart rate, oxygen saturation, finger stick blood glucose | Health kiosk peripherals | Weekly | |
| Height | Assessed by staff (entered into WebQ) | At baseline | |
| Cognitive/mental parameters | Auditory working memory Awareness Divided attention Avoiding distraction Hand–eye coordination General memory Inhibition Naming Planning Response time Shifting attention Spatial perception Time estimation Visual working memory Visual perception Visual scanning Verbal auditory working memory |
Neuropsychological Examination–CogniFit Personal Coach (N-CPC) | At baseline and exit |
| Social parameters | Social support | Self-report Multidimensional Scale of Perceived Social Support (MSPSS) (WebQ) | At baseline and exit |
| Spiritual parameters | Spiritual perspectives | Self-report Spiritual Perspective Scale (SPS) (WebQ) | At baseline and exit |
During the next 8 weeks subjects visited the study room three times a week to provide cognitive assessment data; during one of these sessions each week they also provided physiological/functional data via the health kiosk (see Table 1). The parameters were chosen because they can be easily assessed in a cost-effective manner within residential settings by older adults themselves with no or minimal assistance and could serve as indicators for the underlying wellness components per the theoretical framework. Total time per week for all procedures was approximately 1 h. Participants were able to access their own vital sign data using the telehealth kiosk, but they also received monthly printed reports of all their assessments.
A research assistant trained in study protocols and the use of the equipment was available at all times during the first few weeks to assist with the equipment or any other issues that arose during the data collection sessions. This assistance was tapered off as the study progressed as the amount of assistance needed for subjects to operate the technology decreased over time. Most users became independent in very short time (approximately 1 week), requiring only occasional or no assistance thereafter even in those who identified themselves at study enrollment as computer never users. For protection of human subjects, alert thresholds were set for physiologic parameters and automated electronic alerts were sent to the principal investigator for assessment as to need for further intervention. If necessary, the facility community health nurse was consulted.
After completion of the 8-week study period, subjects participated in one of three focus groups to solicit their perceptions of the underlying conceptual framework, the instruments chosen, and the Health IT Tools used to measure wellness. We assessed their preferences and suggestions for improvement of system functionalities. Focus groups were digitally recorded and transcribed verbatim for later analysis.
Data Integration
The Health IT tools collected data separately in secure Web servers with the capability to export datasets in multiple formats including comma-separated values (CSV) and Excel files. Therefore, a challenge of this approach was to integrate the three commercially available components into one study database. This was achieved with the development of a script that imported files from different sources and converted them in the correct format of the study database. Integration of data from the different sources did require extensive programming of data conversion scripts to ensure appropriate and accurate data transfers and data integrity of the study database.
Data Analysis
We performed descriptive statistics, assessed for pair-wise correlations among parameters, and finally performed an exploratory hierarchical cluster analysis using Hoeffding's D statistics,12 which is robust against nonmonotonic relationships. We performed hierarchical cluster analysis based on the dissimilarities of the D statistics using the hclust function in R. Statistical analyses in this study were performed using SPSS 15.0 (SPSS, Inc., Chicago, IL) and R (R Foundation for Statistical Computing, Vienna, Austria) statistical computing packages.
Results
Our sample included 27 subjects (9 men and 18 women), with an average age of 88.2 years (age range 78–94 years). Responses were diverse in terms of experience with computers, with 12% of all participants being highly comfortable, 52% moderately comfortable, and 28% slightly comfortable. Two subjects (8%) reported having no experience with computers. Other baseline demographic characteristics are presented in Table 2.
Table 2.
Baseline Characteristics of Participants (n=27)
| Age | 88.2 (4.7) |
| Male (%) | 33% |
| Race (%) | |
| White | 93% |
| Other | 7% |
| Ethnicity (%) | |
| Hispanic | 11% |
| Non-Hispanic | 89% |
| Education (%) | |
| High school | 4% |
| Community, trade, or technical college | 12% |
| Baccalaureate degree | 32% |
| Graduate degree | 52% |
| Number of chronic health conditions | 4.3 (2.4) |
| Number of IADL difficulties | 0.2 (0.5) |
| Body mass index | 23.2 (1.6) |
| Blood glucose | 112.9 (21.6) |
| Blood pressure | |
| Systolic | 142.0 (21.5) |
| Diastolic | 80.1 (10.8) |
| Heart rate | 72.3 (9.9) |
| Blood oxygen (pO2%) | 96.5 (1.4) |
| CDC-HRQOL-4 | |
| Overall health rating (%) | |
| Excellent | 17% |
| Very good | 67% |
| Good | 8% |
| Fair | 4% |
| Poor | 4% |
| No. of days physical health not good | 0.6 (1.4) |
| No. of days mental health not good | 2.9 (7.3) |
| No. of days health kept from usual activity | 0.4 (1.0) |
| Self reported fatigue (%) | |
| Rarely or none of the time | 76% |
| Some or a little of the time | 8% |
| Occasionally or a moderate amount of the time | 12% |
| Most or all of the time | 4% |
| Social support (MSPSS possible range 1–7) | 5.6 (0.5) |
| Spirituality (SPS possible range 1–6) | 3.6 (1.4) |
Data are presented as mean (standard deviation) unless otherwise noted.
The number of chronic health conditions reported by participants ranged from 0 to 9 (average number 4, see Table 2). The most common health conditions reported were a history of cancer (48%), high blood pressure (44%), and cardiac arrhythmias (44%). Despite the presence of multiple chronic conditions, at baseline participants generally rated their overall health as excellent (17%) or very good (67%), on the Centers for Disease Control and Prevention Health–related Quality of Life-4 (CDC-HRQOL-4) questionnaire (Table 2). Further, participants reported that physical health in the 30 days before participation was on average “not good” and that their health interfered with their usual activities less than one full day out of the month (Table 2). However, despite this, during the 8-week study period, 15% of the sample fell and 11% experienced unplanned emergency department/hospital visits. Further, physiologic parameters measured during the study generated alerts to the study team, which led to medication adjustments for one subject and closer monitoring of blood pressure in three others.
Subjects overall reported a high level of social support on the Multidimensional Scale of Perceived Social Support (MSPSS) (range 4.8–6.4), where a score of 7 is the highest possible score. On the subscales, social support was perceived as being the highest from family (mean 5.90±0.71) and significant other (mean 5.89±0.76) followed by friends (mean 5.43±0.48). In this sample, there was a broad range of importance placed upon spirituality (mean 3.6 on 1–6 scale of spirituality using SPS; Table 2). In contrast to prior studies, we did not find social support or spirituality to be correlated to other parameters of wellness.
Overall, increased age was negatively correlated with cognitive tasks associated with divided attention (r=−0.48, p=0.029), planning (r=−0.53, p=0.013), and spatial perception (r=−0.718, p<0.0005). In assessing correlations between parameters of wellness, we found a number of significant relationships. Within the cognitive and physical/functional domain, an increased number of chronic diseases negatively correlated with planning (r=−0.52, p=0.016), and the number of instrumental activities of daily living (IADL) difficulties was correlated with inhibition (r=0.46, p=0.03). Further, better self-reported health was correlated with inhibition (r=0.493, p=0.027) and planning ability (r=0.47, p=0.037).
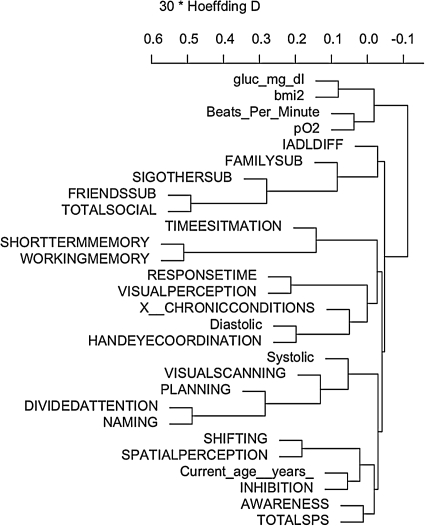
In the exploratory hierarchical cluster analysis (see Fig. 1), two primary clusters were noted within the data, one that included primarily physiological parameters (pulse oximetry, heart rate, body mass index [BMI], and glucose level) and the second with the remaining parameters. Both systolic and diastolic blood pressure clustered with cognitive parameters (Fig. 1).
Fig. 1.
Dendrogram of hierarchical cluster analysis of variables at baseline. gluc_mg_dl, glucose mg/dL; bmi, body mass index; beats_per_minute, heart rate; pO2, pulse oxygenation level; IADLDIFF, number of difficulties in instrumental activities of daily living; FAMILYSUB, family social support subscale; SIGOTHERSUB, significant other social support subscale; FRIENDSSUB, friends social support subscale; TOTALSOCIAL, total social support subscale; TOTALSPS, total spiritual perspectives scale.
Participants in the three focus group sessions expressed overall positive attitudes toward the Health IT tools and the holistic assessment of wellness. They did not express any privacy concerns. They enjoyed the community setting that was accessible to them within their building. As one respondent stated: “It was so nice to be able to do that because you don't have to have a set appointment. If you feel like you're in the mood you can do it. If you feel, oh, I don't even feel like that today you don't have to do it.” Several subjects commented on the value of receiving feedback of their assessment sessions and having the ability to monitor their own progress. One subject emphasized, “I like having the data recorded and printed out in both graphic and tabular form,” whereas another subject stated, “That was very encouraging to have those green checks.…I really enjoyed that.” Three participants commented that they would have liked to receive information about possible interventions to address potential wellness deficiencies and not only the data that present the assessment findings. Specifically, they suggested that the system should provide educational suggestions on how to improve functional, cognitive, or other parameters. Finally, two participants proposed that the system provides data that indicate one's trajectory not only in terms of previous assessments but also in comparison to other peers in the same age group.
Discussion
Our goal was to examine if wellness, informed by Hoyman's framework, could be assessed with the use of an informatics application in a sample of community-dwelling elders. Regular feedback and data access were valued by study participants. Moreover, they expressed the desire to understand their own wellness information more in depth and to understand how their information compared to peers. Prior work has indicated that access to health information, whether from the Internet or other format (e.g., print or television), provides individuals with increased ability to self-manage health.13 Participants in the current study also expressed interest in specific programmatic activities around promoting wellness, so that when a specific need or area was identified, they wanted to know what they could specifically do to improve or prevent decline an area. As healthcare providers have been previously identified as the primary source of health information,13 they can play an integral role in this process, providing context and assisting with the identification of appropriate health promotion activities.
In this study, we found that parameters were highly correlated across multiple domains of wellness. The only invasive measure, blood glucose, clustered logically with a noninvasive measure, BMI. Prior studies have shown correlations between increased body weight and metabolic risk factors.14,15 Future studies could reduce measurement to baseline only or eliminate measurement of blood glucose in those at low risk (healthy BMI or normal waist-to-hip ratio) to reduce burden. Clustering techniques with larger samples should also allow for further collapse of data elements in future studies. Important clusters were noted to be formed across cognitive and physiological domains (e.g., blood pressure and cognitive parameters), giving further evidence of need for a holistic/integrated approach to the assessment of elder wellness. This finding warrants further replication in larger and more diverse samples of older adults.
Study participants perceived value in the current conceptual approach to wellness assessment, providing the team with confirmation during the focus group sessions. When asked to identify elements important to their health or well-being that were not being considered in the current framework or study design, participants could not identify any additional areas for the team to include in future studies. However, some participants felt that spirituality was a critical component of wellness, whereas others saw a much less direct relationship and recommended that it be removed from the model. Contrary to our findings, prior studies indicated that there is a high level of spirituality among older adults in the United States.16,17 It will be important to further clarify concepts of spirituality deemed important to older adults and in which subgroups it is essential to incorporate it into measures of wellness using qualitative methods.
Multiuser Approach
In this study, the approach was that of a multiuser community wellness setting. This model has the advantages of being cost effective as it eliminates the need for monitoring equipment to be installed in individual residences as well as potential benefits of promoting social interactions among users (e.g., several new residents of the facility enrolled in the study partly to meet other participants). On the other hand, this multiuser approach bore scheduling logistical challenges for the use of hardware stations and the risk of privacy violations if personal health information is visible or otherwise accessible to others. To address these challenges, we introduced a sign up log for the equipment and careful attention was paid to the room layout to maximize privacy. During focus group discussion, participants reported that they had no privacy concerns with regard to a community approach to the assessment of wellness.18 used a community telehealth kiosk as part of a care management program to provide monthly blood pressure checks and health education in a sample of six chronically ill older adults and reported that privacy concerns were not primary focus of participants, our results echo this finding.
Adaptations
It was necessary to provide diverse tools to account for user preferences and chronic health conditions. For example, never-users and users who were more familiar with a Mac platform found use of a two-button mouse to be challenging. Other participants expressed preferences for the touchscreen kiosk over the traditional point and click systems. Finally, older adults with specific health issues (e.g., tremor and use of hearing aids) required some customization of tools or training. For example, a pediatric mouse was found to be a beneficial adaptation for participants with arthritis of the hands and some participants found improved concentration with use of headsets during cognitive training sessions while others with hearing aids preferred not to use.
Attrition
As the study required subjects to be enrolled for 2 months, attrition issues were anticipated. In the course of the study 7 participants discontinued participation before completion. Reasons for attrition varied and included death of spouse (1), illness/hospitalization (2), and other time commitments (3). The issue of attrition due to illness/hospitalization introduces the problem of missing data not at random which must be carefully addressed in future studies to avoid bias.19
Limitations
This study provides insight into the potential of IT tools for a comprehensive and ongoing assessment of older adults' wellness. The study setting was in an urban setting and residents of the retirement community had overall high educational level; therefore, findings are not generalizable to other older adult groups. Further, the small sample size did not allow us to adequately power for analysis of wellness over time, which will be important to address in future studies.
We took a community-based approach in the current pilot. With further testing of this approach to standardize and deploy these technologies across population groups, this model has potential implications for public health policy. The ability to compare uniform population health and wellness indicators across locations could enable providers determine if specific groups need additional or tailored interventions to maintain a population-level wellness state. Such an approach will allow community-level assessment of older adult wellness and development of interventions to promote and maintain wellness. Further, it will allow local health administrators to provide aggregate information regarding community wellness status to state and national policy makers for decision-making and resource allocation.
Acknowledgments
This work was supported by Grant Number 5 KL2 RR025015 from the National Center for Research Resources, a component of the National Institutes of Health.
Role of the Sponsor
The National Institute of Research Resources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the article.
Disclosure Statement
Dr. Shatil is an employee of Cognifit. The other authors report no competing financial interests.
References
- 1.Dunn HL. High-level wellness. Virginia: R. W. Beatty, Ltd.; 1961. [Google Scholar]
- 2.Hoyman HS. Rethinking an ecologic-system model of man's health, disease, aging, death. J Sch Health. 1975;45:509–518. doi: 10.1111/j.1746-1561.1975.tb04527.x. [DOI] [PubMed] [Google Scholar]
- 3.Demiris G. Thompson HJ. Reeder B. Wilamowska K. Zaslavsky O. Using informatics to capture older adults' wellness. Int J Med Inf. 2011 doi: 10.1016/j.ijmedinf.2011.03.004. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabbagh MN. Lahti T. Connor DJ. Caviness JN. Shill H. Vedders L, et al. Functional ability correlates with cognitive impairment in Parkinson's disease and Alzheimer's disease. Dement Geriatr Cogn Disord. 2007;24:327–334. doi: 10.1159/000108340. [DOI] [PubMed] [Google Scholar]
- 5.Dorner T. Kranz A. Zettl-Wiedner K. Ludwig C. Rieder A. Gisinger C. The effect of structured strength and balance training on cognitive function in frail, cognitive impaired elderly long-term care residents. Aging Clin Exp Res. 2007;19:400–405. doi: 10.1007/BF03324721. [DOI] [PubMed] [Google Scholar]
- 6.Grant N. Hamer M. Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Ann Behav Med. 2009;37:29–37. doi: 10.1007/s12160-009-9081-z. [DOI] [PubMed] [Google Scholar]
- 7.Townsend M. Kladder V. Ayele H. Mulligan T. Systematic review of clinical trials examining the effects of religion on health. South Med J. 2002;95:1429–1434. [PubMed] [Google Scholar]
- 8.Haimov I. Hanuka E. Horowitz Y. Chronic insomnia and cognitive functioning among older adults. Behav Sleep Med. 2008;6:32–54. doi: 10.1080/15402000701796080. [DOI] [PubMed] [Google Scholar]
- 9.Korczyn AD. Peretz C. Aharonson V. Giladi N. 10th International Hong Kong/Springfield Pan-Asian symposium on advances in Alzheimer therapy; Feb;2008 ; Hong Kong. 2008. [Google Scholar]
- 10.Shatil E. Korczyn AD. Peretz C. Breznitz S. Aharonson V. Giladi N. Improving cognitive performance in elderly subjects using computerized cognitive training; Alzheimer's association ICAD—International Conference on Alzheimer's Disease; Jul;2008 ; Chicago. 2008. [Google Scholar]
- 11.Verghese J. Mahoney J. Ambrose AF. Wang C. Holtzer R. Effect of cognitive remediation on gait in sedentary seniors. J Gerontol A Biol Sci Med Sci. 2010;65:1338–1343. doi: 10.1093/gerona/glq127. [DOI] [PubMed] [Google Scholar]
- 12.Hoeffding W. A non-parametric test of independence. Ann Math Stat. 1948;19:546–557. [Google Scholar]
- 13.Taha J. Sharit J. Czaja S. Use of and satisfaction with sources of health information among older Internet users and nonusers. Gerontologist. 2009;49:663–673. doi: 10.1093/geront/gnp058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biggs ML. Mukamal KJ. Luchsinger JA. Ix JH. Carnethon MR. Newman AB, et al. Association between adiposity in midlife and older age and risk of diabetes in older adults. JAMA. 2010;303:2504–2512. doi: 10.1001/jama.2010.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qin L. Corpeleijn E. Jiang C. Thomas GN. Schooling CM. Zhang W, et al. Physical activity, adiposity, and diabetes risk in middle-aged and older Chinese population: The Guangzhou Biobank Cohort Study. Diabetes Care. 2010;33:2342–2348. doi: 10.2337/dc10-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phillips LL. Paukert AL. Stanley MA. Kunik ME. Incorporating religion and spirituality to improve care for anxiety and depression in older adults. Geriatrics. 2009;64:15–18. [PubMed] [Google Scholar]
- 17.Skarupski KA. Fitchett G. Evans DA. Mendes de Leon CF. Daily spiritual experiences in a biracial, community-based population of older adults. Aging Ment Health. 2010;14:779–789. doi: 10.1080/13607861003713265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Courtney KL. Lingler JH. Mecca LP. Garlock LA. Schulz R. Dick AW, et al. Older adults' and case managers' initial impressions of community-based telehealth kiosks. Res Gerontol Nurs. 2010;3:235–239. doi: 10.3928/19404921-20100504-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rue T. Thompson HJ. Rivara FP. Mackenzie EJ. Jurkovich GJ. Managing the common problem of missing data in trauma studies. J Nurs Scholarsh. 2008;40:373–378. doi: 10.1111/j.1547-5069.2008.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]