To the Editor: I read with great interest the article on nitrofurantoin for uncomplicated urinary tract infections (UTIs) by McKinnell et al.1 Although their study primarily focused on pharmacoeconomics, comparing nitrofurantoin to trimethoprim/sulfamethoxazole (TMP-SMX) and fluoroquinolones, it has important clinical implications.
Nitrofurantoin is an underused antimicrobial for empiric therapy for community-acquired and nosocomial lower UTIs. Among susceptible uropathogens after extensive use worldwide for more than 50 years, there has been virtually no acquired resistance to nitrofurantoin.2,3 Most physicians are acquainted with the adverse effects of nitrofurantoin but are unfamiliar with its virtues. Nitrofurantoin has a unique mechanism of action by interfering with bacterial growth at 3 different locations in the Kreb’s cycle. Although approximately 25% of nitrofurantoin is excreted renally, some is eliminated via the gastrointestinal tract. Unlike “high resistance potential” antibiotics, nitrofurantoin does not predispose to resistance.4 Pharmacokinetically, nitrofurantoin reabsorption is pH dependent and at normal urinary pH (approximately 5.5 pH); nitrofurantoin is preferentially excreted into the lower urinary tract, ie, bladder urine, making it is useful to treat lower UTIs.3,5-7
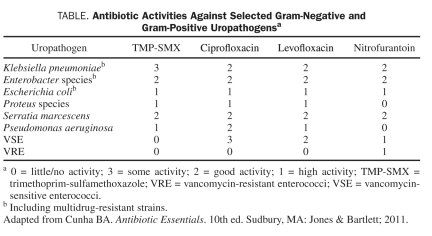
Nitrofurantoin is active against most common uropathogens, but most Proteus species, Serratia marcescens, and Pseudomonas aeruginosa are naturally resistant.4,8 Nitrofurantoin is useful against Escherichia coli and Enterococci, the most frequent causes of nosocomial lower UTIs, ie, catheter-associated bacteriuria. Nitrofurantoin is also active against most strains of multidrug-resistant gram-negative bacilli, including most extended spectrum β lactamase-producing strains.8 Nitrofurantoin is also active against vancomycin-sensitive enterococci and vancomycin-resistant enterococci.3,7,8
During the past 3 decades, I have had extensive experience with nitrofurantoin therapy for nosocomial and community-acquired lower UTIs. Nitrofurantoin, 100 mg orally every 12 hours is well tolerated. The adverse effects of nitrofurantoin are relatively uncommon and benign.4,8 Occasional nausea may occur but is uncommon with macrocrystalline formulations. In patients with intact renal function, nitrofurantoin urinary concentrations are 50 to 300 mg/mL.8 With creatinine clearances lower than 30 mL/min, therapeutic urinary concentrations are unlikely to be obtained, and therapeutic failure may result.4,8 For this reason, nitrofurantoin should be avoided in patients with a creatinine clearance lower than 30 mL/min.7,8 Acute toxicity is limited to acute/reversible migratory pulmonary infiltrates/eosinophilia. Long-term nitrofurantoin toxicity includes peripheral neuropathy, interstitial lung disease, or hepatotoxicity, which may occur in patients treated long term who have chronic renal insufficiency.6,8 Nitrofurantoin has advantages over TMP-SMX and fluoroquinolones for initial empiric therapy of community-acquired and nosocomial lower UTIs. Against gram-negative bacilli uropathogens, nitrofurantoin has a “low resistance potential” vs the “high resistance potential” of TMP-SMX and ciprofloxacin. Unlike TMP-SMX and fluoroquinolones, nitrofurantoin has activity against vancomycin-resistant enterococci3,8 (Table).
TABLE.
Antibiotic Activities Against Selected Gram-Negative and Gram-Positive Uropathogensa
In my experience-based opinion, nitrofurantoin should be the preferred empiric therapy for community-acquired and nosocomial lower UTIs. Nitrofurantoin has remained effective after more than 50 years of extensive use worldwide with essentially no resistance, and for initial empiric therapy for uncomplicated community-acquired or nosocomial UTIs, nitrofurantoin is an ideal antibiotic. If urine cultures are positive for Proteus species, S marcescens, or P aeruginosa, an alternate agent should be selected. I agree with the authors that nitrofurantoin should be the preferred antibiotic for the initial empiric treatment of community-acquired lower UTIs.
References
- 1. McKinnell JA, Stollenwerk NS, Jung CW, Miller LG. Nitrofurantoin compares favorably to recommended agents as empirical treatment of uncomplicated urinary tract infections in a decision and cost analysis. Mayo Clin Proc. 2011;86(6):480–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. McOsker CC, Fitzpatrick PM. Nitrofurantoin: mechanism of action and implications for resistance development in common uropathogens. J Antimicrob Chemother. 1994;33:23–30 [DOI] [PubMed] [Google Scholar]
- 3. Cunha BA. New uses for older antibiotics: nitrofurantoin, amikacin, colistin, polymyxin B, doxycycline, and minocycline revisited. Med Clin North Am. 2006;90:1089–1107 [DOI] [PubMed] [Google Scholar]
- 4. Brumfitt W, Hamilton-Miller MT. Efficacy and safety profile of long-term nitrofurantoin in urinary infections: 18 years’ experience. J Antimicrob Chemother. 1998;42:363–371 [DOI] [PubMed] [Google Scholar]
- 5. Woodruff MW, Malvin RI, Thompson RI. The renal transport of nitrofurantoin: effect of acid-base balance upon its excretion. JAMA. 1961;175:1132–1135 [DOI] [PubMed] [Google Scholar]
- 6. Cunha BA, Comer JB. Pharmacokinetic considerations in the treatment of urinary tract infections. Conn Med. 1979;43:347–353 [PubMed] [Google Scholar]
- 7. Cunha BA. Nitrofurantoin: current concepts. Urology. 1988;32:67–71 [DOI] [PubMed] [Google Scholar]
- 8. Grayson ML, Whitby M. Nitrofurans: nitrofurazone, furazolidone, and nitrofurantoin. In: Grayson ML, Crowe SM, McCarthy JS, et al., eds. Kucers’ The Use of Antibiotics. 6th ed. London, England: Hodder Arnold; 2010:1195–1204 [Google Scholar]