Abstract
Left ventricular (LV) dilatation may be an early sign of cardiac decompensation progressing to LV dysfunction. Determinants of LV dilatation in young asymptomatic adults are unknown. Five hundred six asymptomatic subjects (mean age 32 ± 3 years) enrolled in the Bogalusa Heart Study underwent echocardiographic examination. LV dilatation (LV end-diastolic diameter >5.5 cm) as measured by M-mode echocardiography was found in 31 subjects (6%). Subjects with LV dilatation had greater body mass indexes (32 ± 9 vs 27 ± 6 kg/m2, p <0.0001), systolic (119 ± 15 vs 112 ± 12 mm Hg, p = 0.007) and diastolic (79 ± 12 vs 75 ± 9 mm Hg, p = 0.04) blood pressures, and LV mass (230 ± 50 vs 123 ± 39 g, p <0.0001). Age, gender, race, and metabolic parameters (glucose, insulin, and lipoprotein levels) did not differ significantly between the subjects with and without LV dilatation. After correction for age, gender, and race differences, adulthood obesity (body mass index >30 kg/m2) was associated with a threefold odds ratio (2.9, 95% confidence interval 1.4 to 6.1), and hypertension (defined as per the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) was also associated with a threefold odds ratio (3.0, 95% confidence interval 1.2 to 7.1) for an increased incidence of LV dilatation. There was an incremental increase in LV end-diastolic dimension depending on the presence of hypertension or obesity, and subjects with obesity and hypertension in adulthood had the greatest degree of LV end-diastolic dimensions. In multiple regression analyses, body mass index in childhood was the only significant predictor of LV dilatation in adulthood (odds ratio 1.47, 95% confidence interval 1.03 to 2.09). In conclusion, obesity beginning in childhood and obesity and hypertension in young adulthood are predictors of LV dilatation in an otherwise healthy young adult population.
Studies of patients with coronary heart disease have confirmed the concept of left ventricular (LV) dilatation as a precursor of heart failure.1–3 Furthermore, cardiac enlargement is associated with increased morbidity and mortality in otherwise healthy middle-aged and elderly subjects.4,5 The prevalence and the risk factors for LV dilatation in young patients without symptomatic ischemic heart disease or heart failure are not known. We investigated the relation of LV end-diastolic dimensions and known cardiovascular risk factors in a group of patients free of congestive heart failure or myocardial infarction in a population study of young adults.
Methods
The Bogalusa Heart Study is a long-term epidemiologic study of the natural history of cardiovascular disease in children and young adults from the semi-rural, biracial (65% white, 35% black) community of Bogalusa, Louisiana. The population and study design of the Bogalusa Heart Study have been previously described.6,7 Five hundred six subjects (age range 20 to 38 years; 71% white, 39% men) who had echocardiographic examinations of the heart in adulthood in addition to other risk factor measurements in childhood and adulthood were included in the study.
Informed consent was obtained from all participants, and the protocols were reviewed by the institutional review board of the Tulane University Health Science Center.
All examinations essentially followed the same previously described protocols.7,8 Subjects were instructed to fast for 12 hours before screening, with compliance ascertained by interview on the morning of the examination. Height and weight were measured twice to ±0.1 cm and to ±0.1 kg, respectively, and the average values were used to calculate body mass index (BMI) as a measure of overall adiposity.
Replicate blood pressure measurements were obtained by trained observers in the right arms of the subjects in a relaxed, sitting position. Measurements of arm length and circumference were made during the examination to ensure proper cuff size. Systolic and diastolic blood pressure levels were recorded as the first and fourth (in children) or fifth (in adults) Korotkoff phases using mercury sphygmomanometers. Blood pressure levels were reported as the mean of 6 replicate readings, taken by each of 2 randomly assigned observers.
Venipuncture was performed after confirmation of a 12-hour fast. Serum total cholesterol and triglyceride levels were assayed using an enzymatic procedure on the Abbott VP instrument (Abbott Laboratories, North Chicago, Illinois). Serum lipoprotein cholesterol levels were analyzed by a combination of heparin-calcium precipitation and agar-agarose gel electrophoresis procedures.8 The laboratory was monitored by the Lipid Standardization and Surveillance Program of the Centers for Disease Control and Prevention (Atlanta, Georgia). A commercial radioimmunoassay kit was used for measuring plasma immunoreactive insulin levels (Phadebas insulin kit; Pharmacia Diagnostics, Piscataway, New Jersey). Plasma glucose levels were measured as part of a multiple chemistry profile (SMA20, Laboratory Corporation of America, Burlington, North Carolina) by a glucose oxidase method.
LV dimensions were assessed by 2-dimensional M-mode echocardiography with 2.25- and 3.5-MHz transducers according to the American Society of Echocardiography's recommendations.9 Images were recorded on standard VHS videocassette tapes by trained technicians, and repeated observations were obtained in a randomized 6% sample of subjects selected for repeat measurements 10 to 12 days apart. The measurement errors were consistent with those found in other epidemiologic studies. The coefficient of variation for inter- and intrareader variabilities for all measures of cardiac anatomy was <10%. All echocardiograms were digitized and measured on Tomtec/Freeland Cardiology Workstation digitizing systems (Tomtec/Freeland Systems, Broomfield, Colorado).
Parasternal long- and short-axis views were used for measuring LV end-diastolic and end-systolic measurements in duplicate, which were then averaged. An end-diastolic diameter of >5.5 cm was considered abnormal. LV mass was calculated on the basis of the formula recommended by Devereux.10 Diastolic function was measured using mitral inflow velocity patterns (E/A ratio), and fractional shortening was calculated.
Data analyses were performed using SAS version 8.2 (SAS Institute Inc., Cary, North Carolina). Variables were compared between the groups with normal LV end-diastolic diameters (LVEDDs) and LV dilatation using Students' t test, the chi-square test, and analysis of covariance. The difference between hypertension and/or obesity groups was tested using covariant analysis. Multiple logistic regression analysis on the basis of the maximum-likelihood method was used to calculate adjusted odds ratio with 95% confidence intervals for hypertension and/or obesity compared with no hypertension and obesity with LV dilatation. Risk factors measured at the first and last examinations were used as childhood and adulthood values, respectively.
Pearson's correlation coefficients were used to assess the relations of LVEDD with risk factors. To explore the childhood predictors of LVEDD in adulthood, multiple regression analysis was performed with LVEDD as a dependent variable and risk factors measured in childhood as the independent variables, with all the variables corrected for age, gender, and race.
Results
Among 506 subjects, 31 (6%) were found to have LV dilatation. The characteristics of young adults on the basis of the risk factor variable for cardiac dilatation are listed in Table 1. Subjects with LV dilatation had higher BMIs compared with subjects without LV dilatation. Similarly, subjects with LV dilatation had on average higher systolic and diastolic blood pressures than subjects without LV dilatation. Subjects with LV dilatation also had higher serum triglyceride and low-density lipoprotein cholesterol levels and lower high-density lipoprotein cholesterol levels, although the differences were not statistically significant. Table 2 lists the correlations between LVEDD and cardiovascular risk factors in the 31 subjects. The greatest correlations were seen among BMI, systolic blood pressure, and LVEDD.
Table 1. Characteristics of asymptomatic young adults with or without left ventricular dilatation: the Bogalusa Heart Study.
| Parameters‡ | Normal (n = 475) |
LV Dilatation* (n = 31) |
Comparison p Value† |
|---|---|---|---|
| Age (yrs) | 32.5 ± 1.8 | 32.4 ± 1.8 | NS |
| White/men | 72%/39% | 71%/52% | NS/NS |
| BMI (kg/m2) | 27.2 ± 2.5 | 32.2 ± 2.9 | <0.0001 |
| Systolic BP (mm Hg) | 112 ± 4 | 119 ± 4 | 0.007 |
| Diastolic BP (mm Hg) | 75 ± 3 | 79 ± 4 | 0.04 |
| HDL cholesterol (mg/dl) | 50 ± 4 | 46 ± 3 | NS |
| LDL cholesterol (mg/dl) | 124 ± 6 | 133 ± 6 | NS |
| Triglycerides (mg/dl) | 123 ± 10 | 128 ± 9 | NS |
| Glucose (mg/dl) | 79.5 ± 3.4 | 79.9 ± 3.1 | NS |
| Insulin (μU/ml) | 12.2 ± 3.5 | 11.7 ± 2.4 | NS |
LVEDD >5.5 cm.
BMI, BP, and metabolic parameters were adjusted for race, gender, and age when appropriate.
Raw mean ± SE for continuous variables, percentage for categorical variables.
BP = blood pressure; HDL = high-density lipoprotein; LDL = low-density lipoprotein.
Table 2. Correlation between left ventricular end diastolic diameter and cardiovascular risk factors: the Bogalusa Heart Study.
| Cardiovascular Risk Factor | Correlation Coefficient | p Value* |
|---|---|---|
| BMI (kg/m2) | 0.28 | < 0.0001 |
| Systolic BP (mm Hg) | 0.20 | < 0.0001 |
| Diastolic BP (mm Hg) | 0.15 | 0.003 |
| HDL cholesterol (mg/dl) | −0.10 | 0.04 |
| LDL cholesterol (mg/dl) | 0.12 | 0.01 |
| Triglycerides (mg/dl) | 0.06 | NS |
| Glucose (mg/dl) | 0.02 | NS |
| Insulin (μU/ml) | 0.03 | NS |
Adjusted for age.
Abbreviations as in Table 1.
After correction for age, gender, and race differences, adulthood obesity (BMI >30 kg/m2) was associated with a 2.9 odds ratio, and hypertension (defined as per the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure as 140/90 mm Hg or receiving medication) was also associated with a threefold odds ratio and increased incidence of LV dilatation (Table 3). Of the 31 patients, 8 were considered overweight (BMI 25 to 29 kg/m2) and 16 were obese (BMI ≥30 kg/m2). Seventy-two of 504 patients were hypertensive or receiving antihypertensive medications in the total sample, whereas 7 of 31 patients with LV dilatation were hypertensive or receiving antihypertensive medications. Thirteen patients were overweight or obese without having hypertension or receiving antihypertensive treatment.
Table 3. Association between left ventricular dilatation and obesity and hypertension in asymptomatic young adults: the Bogalusa Heart Study.
| Cardiovascular Risk Factor | Adjusted OR* (95% CI) |
p Value |
|---|---|---|
| Obesity (BMI ≥30 kg/m2) | 2.9 (1.4–6.1) | 0.005 |
| Hypertension (systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg or antihypertensive medication) | 3.0 (1.2–7.1) | 0.01 |
| Obesity and hypertension | 3.5 (1.1–9.3) | 0.02 |
Adjusted for race, gender, and age.
CI = confidence interval; OR = odds ratio; other abbreviations as in Table 1.
There was an incremental increase in LVEDD depending on the presence of hypertension or obesity, and subjects with obesity and hypertension in adulthood had the greatest degree of LV end-diastolic dimensions (odds ratio 3.5, 95% confidence interval 1.1 to 9.3; Figure 1). As listed in Table 4, subjects with LV dilatation had greater LV mass and also had lower diastolic indexes (E/A ratio) and fractional shortening.
Figure 1.
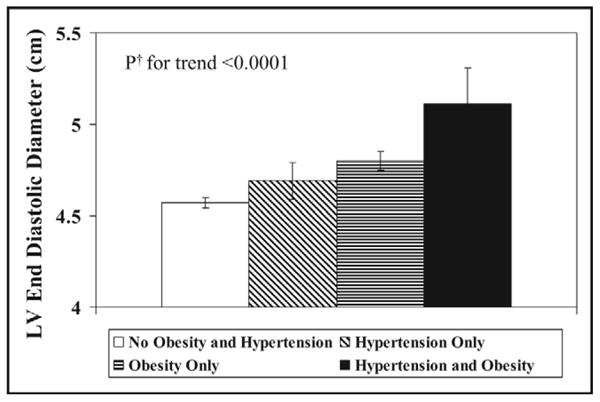
Individual and combined effects of obesity and hypertension on LVEDD (note the trend with the presence of obesity). †Adjusted for race, gender, age, and high-density lipoprotein and low-density lipoprotein cholesterol.
Table 4. Echocardiographic characteristics of asymptomatic young adults with or without left ventricular dilatation: the Bogalusa Heart Study.
| Parameters‡ | Normal (n = 475) |
LV Dilatation* (n = 31) |
Comparison p Value† |
|---|---|---|---|
| LVEDD (cm) | 4.6 ± 0.4 | 5.8 ± 0.4 | < 0.0001 |
| LV mass (g) | 123 ± 39 | 230 ± 50 | < 0.0001 |
| E/A ratio | 2.4 ±1.3 | 1.9 ± 0.7 | 0.05 |
| Fractional shortening (%) | 60.0 ± 7.0 | 56.0 ± 10.0 | 0.06 |
LVEDD >5.5 cm.
All parameters were adjusted for race, gender, and age.
Raw mean ± SD for continuous variables.
When childhood variables were analyzed for the adult subjects with LV dilatation, BMI was the only significant risk factor for LV dilatation (Table 5), indicating childhood obesity as the primary predictor of adult LV dilatation. Multiple regression analyses showed that BMI in childhood (Table 6) was the only significant predictor of LV dilatation, with systolic blood pressure in childhood of marginal significance.
Table 5. Mean ± SD of risk factor variables in childhood by dilatation status: the Bogalusa Heart Study.
| Childhood Variable | Normal (n = 475) |
LV Dilatation* (n = 31) |
Comparison p Value† |
|---|---|---|---|
| Age (yrs) | 11.0 ± 3.1 | 11.4 ± 3.9 | 0.551 |
| BMI (kg/m2) | 18.2 ± 3.6 | 20.3 ± 4.4 | 0.001 |
| Systolic BP (mm Hg) | 102 ± 10 | 107 ± 14 | 0.140 |
| LDL cholesterol (mg/dl) | 89 ± 25 | 93 ± 26 | 0.895 |
| HDL cholesterol (mg/dl) | 65 ± 21 | 62 ± 21 | 0.732 |
| Triglycerides (mg/dl) | 72 ± 40 | 83 ± 38 | 0.253 |
p Values were adjusted for covariates when appropriate.
Abbreviations as in Table 1.
Table 6. Odds ratios of childhood risk factors for having left ventricular dilatation in adulthood by multiple logistic regression analysis: the Bogalusa Heart Study.
| Variable | OR | 95% CI | p Value |
|---|---|---|---|
| BMI (kg/m2) | 1.47 | 1.03–2.09 | 0.034 |
| Systolic BP (mm Hg) | 1.46 | 0.97–2.21 | 0.069 |
| LDL cholesterol (mg/dl) | 1.01 | 0.67–1.53 | 0.962 |
| HDL cholesterol (mg/dl) | 1.08 | 0.69–1.68 | 0.742 |
| Triglycerides (mg/dl) | 1.23 | 0.81–1.86 | 0.331 |
Discussion
In the present study, obesity and hypertension emerged as 2 major independent determinants of cardiac size. The effect was even more significant when the 2 variables were concomitantly present, indicating complementary hemodynamic and potential metabolic influences on cardiac structural changes. The burden of adiposity, measured as BMI in childhood, emerged as the only significant predictor of LV dilatation. Our earlier studies also showed that obesity is the major predictor of adult increased LV mass11 and even precedes other risk factors in development of the metabolic or insulin-resistant syndrome.12
These observations emphasize the adverse effects of childhood obesity and the long-term burden of obesity. Although the relation of obesity and heart disease has long been recognized,13 a growing problem of obesity has been observed.14 Several mechanisms by which obesity can lead to LV dilatation include the excessive vascularity of adipose tissue, an increase in total blood volume, and greater cardiac output.3,13–15 In addition, fat cells generate cytokines and inflammatory factors that can enhance cardiac remodeling. Dilatation produces an increase in stress and compensatory hypertrophy. Diastolic dysfunction may ensue, and if wall stress remains high, systolic dysfunction may ultimately develop. In the present observations, an increase in LV mass and a trend toward abnormal diastolic function occurred, shown by decreased LV compliance and the E/A ratio. These changes are a reflection of LV myocardial structural changes.
Hypertension occurs in 60% of obese adults, and obesity is also known to be associated with increased blood pressure levels and other risk factors in childhood and adolescence, especially in Caucasians.16–18 The co-existence of systemic hypertension and obesity causes simultaneous increases in afterload and preload,13–15 which likely occurs beginning in childhood, at blood pressure levels much lower than recommended by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure for adults. In hypertensive obese patients, LV volume is smaller and LV wall thickness is greater than in normotensive obese subjects, suggesting a hybrid form of hypertrophy13 that could change over time, with ultimate dilatation of the LV chamber.
This study was retrospective and observational and thus subject to limitations. However, the study indicates that obesity and high blood pressure beginning at an early age can have major consequences of increased altered cardiac size and cardiac function. The long-term follow-up of subjects would be essential to study the natural course of LV dilatation leading to overt heart failure clinically. However, there is persuasive evidence that substantial weight reduction in severely obese patients as well as patients receiving antihypertensive medications has the potential to reverse LV hypertrophy, improve cardiac Doppler-derived indexes of LV diastolic dysfunction, and reduce LV systolic dysfunction.19,20 These findings need to be tested in asymptomatic subjects followed over time noting heart failure as an outcome, but more importantly, preventive cardiology should be instituted early in life.
Acknowledgments
This study was supported by National Institute of Health, Bethesda, Maryland, Grant AG-16592 from the National Institute of Aging, Bethesda, Maryland; Grant HL-38844 from the National Heart, Lung, and Blood Institute, Bethesda, Maryland; and Grant 0555168B from the American Heart Association, Dallas, Texas.
References
- 1.Nestico PF, Hakki AH, Iskandrian AS. Left ventricular dilatation. Prognostic value in severe left ventricular dysfunction secondary to coronary artery disease. Chest. 1985;88:215–220. doi: 10.1378/chest.88.2.215. [DOI] [PubMed] [Google Scholar]
- 2.Galderisi M, Lauer MS, Levy D. Echocardiographic determinants of clinical outcome in subjects with coronary artery disease (the Framingham Heart Study) Am J Cardiol. 1992;70:971–976. doi: 10.1016/0002-9149(92)90345-y. [DOI] [PubMed] [Google Scholar]
- 3.Gaudron P, Eilles C, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation. 1993;87:755–763. doi: 10.1161/01.cir.87.3.755. [DOI] [PubMed] [Google Scholar]
- 4.Lauer MS, Evans JC, Levy D. Prognostic implications of subclinical left ventricular dilatation and systolic dysfunction in men free of overt cardiovascular disease (the Framingham Heart Study) Am J Cardiol. 1992;70:1180–1184. doi: 10.1016/0002-9149(92)90052-z. [DOI] [PubMed] [Google Scholar]
- 5.Vasan RS, Larson MG, Benjamin EJ, Evans JC, Levy D. Left ventricular dilatation and the risk of congestive heart failure in people without myocardial infarction. N Engl J Med. 1997;336:1350–1355. doi: 10.1056/NEJM199705083361903. [DOI] [PubMed] [Google Scholar]
- 6.Berenson GS, McMahan CA, Voors AW, Webber LS, Srinivasan SR, Frank GC, Foster TA, Blonde CV. Cardiovascular Risk Factors in Children—The Early Natural History of Atherosclerosis and Essential Hypertension. New York, New York: Oxford University Press; 1980. [Google Scholar]
- 7.Berenson GS, editor. Causation of Cardiovascular Risk Factors in Children: Perspectives on Cardiovascular Risk in Early Life. New York, New York: Raven; 1986. p. 408. [Google Scholar]
- 8.Srinivasan SR, Berenson GS. Serum lipoproteins in children and methods for study. In: Lewis LA, editor. Handbook of Electrophoresis. Boca Raton, Florida: CRC Press; 1983. pp. 185–204. [Google Scholar]
- 9.Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978;58:1072–1083. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- 10.Devereux RB. Detection of left ventricular hypertrophy by M-mode echocardiography. Anatomic validation, standardization, and comparison to other methods. Hypertension. 1987;9:II19–II26. doi: 10.1161/01.hyp.9.2_pt_2.ii19. [DOI] [PubMed] [Google Scholar]
- 11.Li X, Li S, Ulusoy E, Chen W, Srinivasan SR, Berenson GS. Childhood adiposity as a predictor of cardiac mass in adulthood: the Bogalusa Heart Study. Circulation. 2004;110:3488–3492. doi: 10.1161/01.CIR.0000149713.48317.27. [DOI] [PubMed] [Google Scholar]
- 12.Srinivasan SR, Myers L, Berenson GS. Predictability of childhood adiposity and insulin for developing insulin resistance syndrome (syndrome X) in young adulthood: the Bogalusa Heart Study. Diabetes. 2002;51:204–209. doi: 10.2337/diabetes.51.1.204. [DOI] [PubMed] [Google Scholar]
- 13.Alpert MA, Alexander JK. The Heart and Lung in Obesity. Armonk, New York: Futura; 1998. Obesity and ventricular function in man: systolic function; pp. 77–94. [Google Scholar]
- 14.Litwin SE. The growing problem of obesity and the heart. J Am Coll Cardiol. 2006;47:617–619. doi: 10.1016/j.jacc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Messerli FH, Christie B, DeCarvalho JG, Aristimuno GG, Suarez DH, Dreslinski GR, Frohlich ED. Obesity and essential hypertension. Hemodynamics, intravascular volume, sodium excretion, and plasma renin activity. Arch Intern Med. 1981;141:81–85. doi: 10.1001/archinte.141.1.81. [DOI] [PubMed] [Google Scholar]
- 16.Berenson GS, Voors AW, Webber LS, Dalferes ER, Jr, Harsha DW. Racial differences of parameters associated with blood pressure levels in children: the Bogalusa Heart Study. Metabolism. 1979;28:1218–1228. doi: 10.1016/0026-0495(79)90134-3. [DOI] [PubMed] [Google Scholar]
- 17.Lauer RM, Clark WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1984;84:633–641. [PubMed] [Google Scholar]
- 18.Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, Berenson GS. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am J Pub Health. 1992;82:358–363. doi: 10.2105/ajph.82.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacMahon SW, Wilcken DE, Macdonald GJ. The effect of weight reduction on left ventricular mass. A randomized controlled trial in young, overweight hypertensive patients. N Engl J Med. 1986;314:334–339. doi: 10.1056/NEJM198602063140602. [DOI] [PubMed] [Google Scholar]
- 20.Schulman SP, Weiss JL, Becker LC, Gottlieb SO, Woodruff KM, Weisfeldt ML, Gerstenblith G. The effects of antihypertensive therapy on left ventricular mass in elderly patients. N Engl J Med. 1990;322:1350–1356. doi: 10.1056/NEJM199005103221904. [DOI] [PubMed] [Google Scholar]


