Abstract
Objective
To determine the association between poor sleep quality, fatigue, and self-reported safety outcomes among Emergency Medical Services (EMS) workers.
Methods
We used convenience sampling of EMS agencies and a cross-sectional survey design. We administered the 19-item Pittsburgh Sleep Quality Index (PSQI), 11-item Chalder Fatigue Questionnaire (CFQ), and 44-item EMS Safety Inventory (EMS-SI) to measure sleep quality, fatigue, and safety outcomes, respectively. We used a consensus process to develop the EMS-SI, which was designed to capture three composite measurements of EMS worker injury, medical errors and adverse events (AE), and safety compromising behaviors. We used hierarchical logistic regression to test the association between poor sleep quality, fatigue, and three composite measures of EMS worker safety outcomes.
Results
We received 547 surveys from 30 EMS agencies (a 35.6% mean agency response rate). The mean PSQI score exceeded the benchmark for poor sleep (6.9, 95%CI 6.6, 7.2). Greater than half of respondents were classified as fatigued (55%, 95%CI 50.7, 59.3). Eighteen percent of respondents reported an injury (17.8%, 95%CI 13.5, 22.1), forty-one percent a medical error or AE (41.1%, 95%CI 36.8, 45.4), and 89% (95%CI 87, 92) safety compromising behaviors. After controlling for confounding, we identified 1.9 greater odds of injury (95%CI 1.1, 3.3), 2.2 greater odds of medical error or AE (95%CI 1.4, 3.3), and 3.6 greater odds of safety compromising behavior (95%CI 1.5, 8.3) among fatigued respondents versus non-fatigued respondents.
Conclusions
In this sample of EMS workers, poor sleep quality and fatigue is common. We provide preliminary evidence of an association between sleep quality, fatigue, and safety outcomes.
Introduction
Poor sleep quality and fatigue among health care workers contributes to poor safety outcomes such as error and injury.1 Annually, medical errors and adverse events (AE) affect hundreds of thousands of patients and contribute to as much as $28 billion in additional healthcare costs.2 The World Health Organization (WHO) identified fatigue as a leading factor in medical error and injury in healthcare.3 The Accreditation Council for Graduate Medical Education has twice recommended reductions in work time for medical trainees due in part to concerns about fatigue.4 Little is known about the linkage between fatigue, sleep, and safety in Emergency Medical Services (EMS); a high-risk environment for patients and providers.
The risk of negative outcomes for the EMS worker and patient is high and different from risks from within the hospital. For example, the EMS worker makes a decision to provide medication or other treatment within minutes or even seconds of establishing a general impression of patient and condition. These decisions are made while in a fast-paced and uncertain environment where the patient and bystanders can be violent, create distractions or disrupt care delivery. Decisions are based on written protocols and radio-enabled assistance from a medical oversight physician. Care may be delivered with some assistance from a single partner, an EMT or paramedic. Most often the paramedic or EMT is in control of patient care alone in the back of an ambulance. In contrast, decisions in the in-hospital setting may involve a team of attending and resident physicians, nurses, technicians, and specialists. In-hospital decisions for care delivery may be aided by computerized patient order entry (CPOE), which can filter decisions and alert clinicians of potential errors before they occur.
EMS workers must be alert and vigilant at all times to prevent errors in protocol and injury to patients or each other. Commonly identified errors in EMS care include deviating from protocol, failure to secure a patient’s airway, dropping a patient from a stretcher, and mistakes in administration of medication.5–8 Threats to the EMS worker’s personal safety include violent patients and bystanders, high-speed ground or air-medical transports, lifting and moving patients, and exposure to hazardous materials and contaminated substances and needles.9 Rates of EMS worker injury and death while on the job exceed that of the general public.9–12 Many EMS workers hold multiple public safety jobs, routinely working 50 hours or more per week.13–16 Unlike resident physicians, the U.S. EMS worker faces few restrictions on hours worked or number of agencies employed.
A recent study determined that a high proportion of EMS workers suffer severe fatigue while at work and generally have poor sleep quality.16 There is no known research of the link between sleep, fatigue, and patient and EMS safety outcomes. The purpose of this study was to use previously tested and psychometrically sound surveys to examine the association between sleep quality, fatigue, self-reported injury, adverse events or medical errors, and safety-compromising behaviors.
Methods
Recruitment of Study Sample
We recruited EMS managers affiliated with an EMS management group with a total membership of 2,253 managers (The National EMS Management Association). The NEMSMA does not maintain a detailed repository of agency-level demographic data for the agency to which each EMS manager is affiliated. We were unable to offer a summary of the common demographic characteristics of member agencies that did not participate in our study. We distributed a standard recruitment letter and study flyer on the member email Listserv. This letter and flyer directed agencies to a designated study website (www.EMSARN.org). This site was populated with information about the research study. Agencies willing to participate contacted the study team.
Survey Sampling of EMTs
At baseline, agencies provided limited demographic data on potential EMS worker respondents employed at the agency. We used a secure online survey system developed and maintained by the University of Pittsburgh Center for Research on Health Care Data Center. Agency administrators used this system to distribute a standard email from the University of Pittsburgh to EMS workers. The email contained standardized text and information about the study and a link to the secure online survey. The EMS worker completed the survey, selected the “opt-out” option, or took no action. The survey link was available from January to June 2010. Completed survey data were stored on a secure server. We received a coded dataset with agency identification numbers linked to randomly generated survey identification numbers and survey responses at the end of the study period. We gave a $100 gift card to the agency with the highest response rate.
Survey Instruments
We measured sleep quality with the 19-item Pittsburgh Sleep Quality Index (PSQI).17 The PSQI evaluates the respondents sleep quality across seven constructs: Subjective Sleep Quality, Sleep Latency, Sleep Duration, Habitual Sleep Efficiency, Sleep Disturbances, Use of Sleeping Medications, and Daytime Dysfunction. Respondent answers to each question were weighted from 0–3 and possible scores ranged from 0–21. A score of >5 indicates poor sleep quality.17
We measured fatigue at work with the 11-item Chalder Fatigue Questionnaire (CFQ) adapted for the EMS work environment.16 The CFQ evaluates both physical and mental fatigue.18 Adapted items reference EMS work (i.e. “Do you feel weak?” was modified to, “Do you feel weak during your EMS shifts?”). Respondents recorded their answers on a 4-point Likert scale: Always, Sometimes, Rarely, or Never. We followed Chalder’s prescribed method for scoring responses as Always=1, Sometimes=1, Rarely=0, and Never=0. Respondents with scores ≥4 are classified as fatigued. Both the PSQI and CFQ have been widely used in clinical and occupational populations – including EMS workers.16
We reviewed the literature and identified limited standards for capturing safety outcomes in EMS. We developed a new 44-item survey tool to elicit safety outcomes data using self-report by EMS personnel, the EMS Safety Inventory (EMS-SI). The development process began with assembling a panel of EMS medical directors, EMTs and paramedics, and epidemiologists. This panel developed a list of draft candidate items for the EMS-SI.19 We used a Delphi-like (consensus driven) iterative process to review and eliminate or endorse each item based on content and face validity. Panelists grouped items into composite measures of safety analogous to the Patient Safety Indicator (PSI) tool developed by the Agency for Healthcare Research and Quality (AHRQ).20 Items were grouped into three composite measures of provider injury (n=2-items; i.e., “I was injured during a shift.”), medical errors or adverse events (n=25-items; i.e., “I accidentally dislodged an ET tube.”), and safety-compromising behaviors (n=17-items; “I have greatly exceeded the speed limit while responding lights and sirens.”).
We used the same consensus driven process to develop two nominal 7-point Likert scales to capture EMS-SI responses. Response options included on the first scale include: “definitely not,” “probably not,” “I’m not sure,” “probably yes,” “definitely yes,” “do not wish to answer,” or “not applicable to me.” Response options on the second scale include: “ran out of time,” “forgot to perform,” “not part of protocol,” “did not think it necessary,” “contraindicated,” “do not wish to answer,” and “not applicable to me.” The expert panel considered five responses credible indicators of negative patient or provider safety outcomes: “Probably Yes,” “Definitely Yes,” “Ran Out of Time,” “Forgot to Perform,” and “Did Not Think it was Necessary.” See Appendix A for a list of EMS-SI items and response options.
Appendix A.
The EMS Safety Inventory
| Question Number | Item Stem: In the previous 3 months | Scale | Category |
|---|---|---|---|
| 1 | ….I was injured during a shift. | A | Injury |
| 4 | …I received a needle stick injury. | A | Injury |
| 11 | …I did not establish an IV after two attempts because… | B | Error or AE |
| 12 | … I did not use a secondary treatment device when the preferred failed (e.g. IO instead of IV access, king airway instead of ET tube) because… | B | Error or AE |
| 13 | …I did not check a glucose level in a patient with altered mental status because… | B | Error or AE |
| 14 | ….I did not check a glucose level in a diabetic patient with nausea and vomiting because… | B | Error or AE |
| 15 | …I did not perform an airway intervention (e.g. BVM, Intubation, King/Combitube) on a patient with Congestive Heart Failure while enroute to the hospital because… | B | Error or AE |
| 16 | …I did not intubate a patient in respiratory arrest because… | B | Error or AE |
| 17 | …I did not place a patient on the monitor because | B | Error or AE |
| 18 | …I did not perform a 12-Lead EKG on a patient with chest pain because… | B | Error or AE |
| 19 | …I did not perform a 12-Lead EKG on a patient with STEMI because… | B | Error or AE |
| 20 | …I confirmed a STEMI but did not administer aspirin when warranted because… | B | Error or AE |
| 21 | …I administered the wrong medication by not checking the label because… | B | Error or AE |
| 22 | …I administered the wrong dose of medication by not confirming the dose because… | B | Error or AE |
| 23 | …I transferred a patient at the Emergency Department (ED) with an unrecognized esophageal intubation (ET tube placed in esophagus rather than trachea) because… | B | Error or AE |
| 24 | …I did not secure an embedded object in a wound instead of securing the object with bandages and accidently removed it because… | B | Error or AE |
| 25 | …I did not print and properly interpret a 6 inch EKG strip because… | B | Error or AE |
| 26 | …I did not properly size a piece of equipment and then used it on a patient (e.g. ET tube, C- Collar, Airway Adjunct, IV Catheter) because… | B | Error or AE |
| 27 | ….I did not transport a specialty care patient to a specialty care facility (i.e. Trauma, Stroke, Pediatric) because… | B | Error or AE |
| 28 | …I accidentally started an IO in a location outside of protocol. | A | Error or AE |
| 29 | …I made a patient with chest pain ambulate instead of using a stretcher. | A | Error or AE |
| 30 | …I did not administer the necessary treatment for a specific condition/malady. | A | Error or AE |
| 32 | …I accessed a dialysis port or other vascular device outside of protocol. | A | Error or AE |
| 33 | …I accidentally dislodged an ET tube. | A | Error or AE |
| 31 | …I placed an IV into an artery instead of into a vein. | A | Error or AE |
| 34 | …I accidentally dropped a patient while on a transportation device (i.e. stretcher, stair chair). | A | Error or AE |
| 35 | …I accidentally caused physical injury to a patient moving the patient. | A | Error or AE |
| 2 | …I was overly stressed during a shift. | A | Safety-Compromising Behavior |
| 3 | …I found myself at an unsafe scene. | A | Safety-Compromising Behavior |
| 5 | …I may have been contaminated with copious amounts of patient bodily fluids. | A | Safety-Compromising Behavior |
| 6 | …I was involved in a collision involving one of my agency’s vehicles. | A | Safety-Compromising Behavior |
| 7 | …I have reported for my shift without getting adequate rest beforehand. | A | Safety-Compromising Behavior |
| 8 | …I have reported for my shift after drinking alcohol within the previous 8 hours. | A | Safety-Compromising Behavior |
| 9 | ….I did not complete a pre-shift check of equipment and medications because… | B | Safety-Compromising Behavior |
| 10 | …I did not restock the ambulance before a call or shift because… | B | Safety-Compromising Behavior |
| 36 | …I have “fudged” information on a patient care report (i.e. vitals, chronology of events). | A | Safety-Compromising Behavior |
| 37 | …I felt vulnerable to harm due to lack of appropriate PPE (i.e. BSI, Turnout Gear, etc). | A | Safety-Compromising Behavior |
| 38 | …I felt that a patient’s safety was jeopardized because my agency did not provide me with updated equipment. | A | Safety-Compromising Behavior |
| 39 | …I felt that my safety was jeopardized because my agency did not provide me with updated equipment. | A | Safety-Compromising Behavior |
| 40 | …I felt that a patient’s safety was jeopardized because my agency did not provide me with updated protocols/policies/procedures. | A | Safety-Compromising Behavior |
| 41 | …I felt that my safety was jeopardized because my agency did not provide me with updated protocols/policies/procedures. | A | Safety-Compromising Behavior |
| 42 | …I have exceeded the speed limit while routinely driving the unit in a non-emergency mode. | A | Safety-Compromising Behavior |
| 43 | …I have greatly exceeded the speed limit while responding lights and sirens (i.e. more than 15 mph over the posted speed limit). | A | Safety-Compromising Behavior |
| 44 | …My “Chute Time” (Time from call received to rolling) was greater than 1 minute. | A | Safety-Compromising Behavior |
| Scale | Response | Negative Safety Outcome |
|---|---|---|
| A | Definitely Not | |
| Probably Not | ||
| I’m Not Sure | ||
| Probably Yes | Yes | |
| Definitely Yes | Yes | |
| Do Not Wish to Answer | ||
| Not Applicable to Me | ||
| B | Ran Out of Time | Yes |
| Forgot to Perform | Yes | |
| Not Part of Protocol | ||
| Did Not Think it was Necessary | Yes | |
| Contraindicated | ||
| Do Not Wish to Answer | ||
| Not Applicable to Me |
Respondents completed a 15-item demographic survey that included: sex, age in years, certification (EMT-Basic or EMT-Paramedic), years of EMS experience, employment status (full time, part time, volunteer only), total shifts worked last month (stratified into 3 categories based on the 25th and 75th percentiles of collected data; 0–5, 6–15, ≥16), type of shift most commonly worked (24hr, 12hr, ≤8hr), status of working at more than one EMS agency (yes, no), rating of general health (excellent, good, fair, poor), ever told by physician to have (diabetes, high blood pressure, heart problems, sleep apnea, breathing problems, arthritis, weight problems, migraines, depression), race and ethnicity, smoking status, alcohol consumption, and height and weight.
Analysis of Data
We calculated standard measures of reliability and instrument validity to evaluate the psychometric properties of the CFQ in this study sample. We calculated Cronbach’s coefficient Alpha and Pearson product moment score-total coefficients to test the internal consistency/reliability of our survey tools. Cronbach’s Alpha values above 0.70 are interpreted as a positive sign for instrument reliability.21 We used Confirmatory Factor Analysis (CFA) to test model fit and determine if the items used to measure fatigue actually measured the hypothesized constructs of mental and physical fatigue.22 We report a standard set of measures of model fit and construct validity: the Goodness of Fit Index (GFI), the Standardized Root Mean Square Residual (SRMR), Bentler’s Comparative Fit Index (CFI), the Bentler & Bonett’s Non-Normed Fit Index (NNFI), Bentler & Bonnett’s Normed Index (NFI), item-construct Pearson correlation coefficients, and Pearson construct-to-construct correlation coefficients. A SRMR less than 0.08, GFI, CFI, NNFI, and NI approaching 0.9, and item-construct Pearson correlations ≥0.40 and construct-to-construct Pearson correlation coefficients that are less than construct Cronbach’s alpha coefficients are considered acceptable indices of instrument validity and model fit.22–26 We did not perform CFA on PSQI constructs. The PSQI score calculations require use of multiple similar items across constructs. We did not perform CFA on the EMS-SI because it was not designed to measure latent constructs of safety outcomes.
We calculated frequencies and percentages to describe agency-level and individual-level demographic information. We used Wald chi-squaretests to evaluate differences between the proportions of EMS workers classified as fatigued, with poor sleep quality, injured, had committed an error, and perceived compromised safety across agency and respondent factors while accounting for within-agency clustering. We selected the Wald chi square test over the Rao-Scott chi-square because the latter test assumes random and non-complex sampling. Alpha was set at 0.05 for all comparisons. We used cluster-adjusted odds ratios to quantify the association between exposure to sleep and/or fatigue and the designated outcomes. We used cluster-adjusted (hierarchical) logistic regression to adjust for agency and respondent factors that may alter variations observed in bivarate analyses. The cluster-adjusted hierarchical logistic regression models accounts for the lack of independence that groups of respondents have with a particular agency. We followed conventional model building guidelines and included only those variables significant in bivariate analyses. We used chi-square tests to check for collinearity prior to model building. When collinearity was detected we specified a model with variables most strongly associated with fatigue, sleep, and the outcome of interest. We included the variable ‘shift length most commonly worked’ in all models because of interest in the association between extended work hours and safety outcomes in healthcare.27, 28 We included rural/urban status and a three-level categorical variable, agency call volume, in bivariate and multivariable analyses. Rural/urban status was defined based on the Rural Urban Commuting Area (RUCA) designation linked to the agency’s physical address. We stratified agency call volume into three stratums based on the variable’s non-normal characteristics and tertile distribution; ≤5,000, 5,001–15,000, >15,000. We performed all analyses with SAS Version 9.2 (Cary, North Carolina).
RESULTS
Sample Demographics
We received 556 survey responses from all four US census regions with most participating agencies and respondents located in the Midwest and Northeast (Table 1). Nine respondents selected the “opt-out” option and did not complete a survey. Thirty-six surveys were incomplete and excluded. Complete survey data was present for 511 surveys. The mean agency response rate was 35.6% (range 4.9% to 78.1%). The most common type of agency self-classification was “other” (40%) and greater than three-fourths self-identified ownership as private non-profit (83%). Three-quarters of agencies (73%) employed between 21 and 100 EMS workers. Nine of every 10 respondents (94%) self-identified as white and 74% as male (Table 2). The mean age of respondents was 37 years (SD 10.6). Greater than half of respondents were certified as an EMT-Paramedic (59.5%) and had 10 years or less of EMS experience (51.5%). The largest stratum for employment status was full-time (75%) and most respondents reported working between six and 15 shifts per month (59%). Half of respondents reported regular shift lengths of 24-hours (49%) and one-third of respondents (34%) were actively working at more than one EMS agency. Three quarters (76%) of subjects were classified as overweight or obese and more than half reported one or more health problems. Most respondents were affiliated with agencies located in the Midwest and Northwest Census regions (72.6%), a 3rd Service/Government or “other” EMS model agency (74%), agencies with 21–100 employees (81.3%), and agencies with base sites located in urban areas (74.4%; Table 1). Respondents were evenly distributed across three-levels of call volume (30.5% <5,000 dispatches; 33.9% 5,001–15,000; and 35.6% >15,000).
Table 1.
Sample Demographics
| Study Sample | Agency Level N=30 (100%) |
Individual Level N=511 (100%) |
|---|---|---|
| Census Region | ||
| Midwest | 16 (53.3%) | 176 (34.4%) |
| Northeast | 9 (30.0%) | 195 (38.2%) |
| West | 3 (10.0%) | 120 (23.5%) |
| South | 2 (6.7%) | 20 (3.9%) |
| Agency Classification | ||
| Hospital Based | 4 (13.3%) | 72 (14.1%) |
| Fire Based | 1 (3.3%) | 8 (1.6%) |
| 3rd Service/Government | 11 (36.7%) | 238 (46.6%) |
| Rescue Squad | 2 (6.7%) | 53 (10.4%) |
| Other | 12 (40.0%) | 140 (27.4%) |
| Agency Ownership | ||
| Private For-Profit | 1 (3.3%) | 9 (1.8%) |
| Private Non-Profit | 25 (83.4%) | 383 (75.0%) |
| Government Funded | 2 (6.7%) | 81 (15.9%) |
| Member Supported | 1 (3.3%) | 25 (4.9%) |
| Other | 1 (3.3%) | 13 (2.5%) |
| Number of Employees | ||
| 1–20 Employees | 5 (16.7%) | 29 (5.7%) |
| 21–50 Employees | 12 (40.0%) | 170 (33.3%) |
| 51–100 Employees | 10 (33.3%) | 245 (48.0%) |
| 101–400 Employees | 3 (10%) | 67 (13.1%) |
| Agency Call Volume | ||
| ≤5000 | 16 (53.3%) | 156 (30.5%) |
| 5001–15,000 | 8 (26.7%) | 173 (33.9%) |
| >15,000 | 6 (20.0%) | 182 (35.6%) |
| Rural/Urban Status | ||
| Rural (RUCA code ≥4) | 12 (40.0%) | 131 (25.6%) |
| Urban (RUCA code < 4) | 18 (60.0%) | 380 (74.4%) |
Table 2.
Summary of associations between respondent demographics and poor sleep, fatigue, injury, errors and adverse events, and safety compromising behaviors
| Study Sample (Respondents) n(%) | Poor Sleep n(%) | Severe Fatigue n(%) | Injury n(%) | Error or Adverse Event n(%) | Safety Compromising Behaviors n(%) | |
|---|---|---|---|---|---|---|
| N=511 100% |
N=304 59.5% |
N=281 55% |
N=91 17.8% |
N=210 41.1% |
N=458 89.6% |
|
| Age | * | |||||
| 17–25 years | 80 (15.7) | 49 (61.3) | 41 (51.3) | 10 (12.5) | 38 (47.5) | 73 (91.3) |
| 26–35 years | 163 (31.9) | 92 (56.4) | 89 (54.6) | 29 (17.8) | 74 (45.4) | 152 (93.3) |
| 36–45 years | 156 (30.5) | 93 (59.6) | 96 (61.5) | 38 (24.4) | 70 (44.9) | 138 (88.5) |
| ≥46 years | 112 (21.9) | 70 (62.5) | 55 (49.1) | 14 (12.5) | 28 (25.0) | 95 (84.8) |
| Sex | ||||||
| Male | 378 (74.0) | 216 (57.1) | 209 (55.3) | 65 (17.2) | 155 (41.0) | 338 (89.4) |
| Female | 133 (26.0) | 88 (66.2) | 72 (54.1) | 26 (19.5) | 55 (41.4) | 120 (90.2) |
| Race | * | |||||
| White | 478 (93.5) | 284 (59.4) | 263 (55.0) | 85 (17.8) | 203 (42.5) | 431 (90.2) |
| African American | 5 (1.0) | 20 (60.6) | 18 (54.5) | 6 (18.2) | 7 (21.2) | 27 (81.8) |
| Other | 28 (5.5) | |||||
| Agency Call Volume | * | |||||
| ≤5000 | 156 (30.5%) | 87 (55.8%) | 73 (46.8%) | 35 (22.4%) | 58 (37.2%) | 134 (85.9%) |
| 5000–15,000 | 173 (33.9%) | 110 (63.6%) | 111 (64.2%) | 30 (17.3%) | 69 (39.9%) | 162 (93.6%) |
| >15,000 | 182 (35.6%) | 107 (58.8%) | 97 (53.3%) | 41 (22.5%) | 83 (45.6%) | 161 (88.5%) |
| Certification | * | * | * | |||
| EMT-Paramedic | 304 (59.5) | 181 (59.4) | 178 (58.6) | 65 (21.4) | 165 (54.3) | 284 (93.4) |
| EMT-Basic | 207 (40.5) | 123 (59.5) | 103 (49.8) | 26 (12.6) | 45 (21.7) | 174 (84.1) |
| Years of EMS Experience | * | |||||
| 0–10 years | 263 (51.5) | 161 (61.2) | 131 (49.8) | 45 (17.1) | 123 (46.8) | 235 (89.4) |
| 11–20 years | 148 (29.0) | 84 (56.8) | 95 (64.2) | 31 (20.9) | 59 (39.9) | 134 (90.5) |
| ≥21 years | 100 (19.6) | 59 (59.0) | 55 (55.0) | 15 (15.0) | 28 (28.0) | 89 (89.0) |
| Employment Status | * | * | ||||
| Full-Time | 387 (75.7) | 245 (63.3) | 234 (60.5) | 79 (20.4) | 169 (43.7) | 355 (91.7) |
| Part-Time | 79 (15.5) | 39 (49.4) | 40 (50.6) | 10 (12.7) | 30 (38.0) | 69 (87.3) |
| Volunteer | 45 (8.8) | 20 (44.4) | 7 (15.6) | 2 (4.4) | 11 (24.4) | 34 (75.6) |
| Number of Shifts per Month | * | * | * | |||
| 0–5 shifts | 74 (14.5) | 36 (48.6) | 26 (35.1) | 3 (4.1) | 11 (14.9) | 54 (73.0) |
| 6–15 shifts | 301 (58.9) | 176 (58.5) | 191 (63.5) | 62 (20.6) | 140 (46.5) | 280 (93.0) |
| ≥16 shifts | 136 (26.6) | 92 (67.6) | 64 (47.1) | 26 (19.1) | 59 (43.4) | 124 (91.2) |
| Shift Most Commonly Work | * | * | * | * | ||
| 24 hours | 248 (48.5) | 153 (61.7) | 154 (62.1) | 54 (21.8) | 109 (44.0) | 228 (91.9) |
| 12 hours | 196 (38.4) | 112 (57.1) | 105 (53.6) | 31 (15.8) | 87 (44.4) | 177 (90.3) |
| ≤ 8 hours | 67 (13.1) | 39 (58.2) | 22 (32.8) | 6 (8.9) | 14 (20.9) | 53 (79.1) |
| Actively working at more than 1 EMS agency | * | * | ||||
| Yes | 175 (34.3) | 119 (68.0) | 102 (58.3) | 26 (14.9) | 86 (49.1) | 163 (93.1) |
| No | 336 (65.8) | 185 (55.1) | 179 (53.3) | 65 (19.3) | 124 (36.9) | 295 (87.8) |
| BMI | ||||||
| Normal | 112 (21.9) | 58 (51.8) | 48 (42.9) | 19 (17.0) | 46 (41.1) | 97 (86.6) |
| Overweight/Obese | 396 (77.5) | 244 (61.6) | 231 (58.3) | 72 (18.2) | 164 (41.4) | 359 (90.7) |
| Smoking Status | ||||||
| Do not smoke | 432 (84.5) | 256 (59.3) | 237 (54.9) | 79 (18.3) | 183 (42.4) | 389 (90.0) |
| Smoke | 79 (15.5) | 48 (60.8) | 44 (55.7) | 12 (15.2) | 27 (34.2) | 69 (87.3) |
| Alcoholic Drinks per Week | * | |||||
| 0 drinks | 182 (35.6) | 104 (57.1) | 90 (49.5) | 30 (16.5) | 59 (32.4) | 161 (88.5) |
| 1–3 drinks | 185 (36.2) | 111 (60) | 101 (54.6) | 36 (19.5) | 82 (44.3) | 162 (87.6) |
| 4–10 drinks | 110 (21.5) | 69 (62.7) | 69 (62.7) | 18 (16.4) | 48 (43.6) | 101 (91.8) |
| >10 drinks | 34 (6.7) | 20 (58.8) | 21 (61.8) | 7 (20.6) | 21 (61.8) | 34 (100) |
| Self-Rated General Health | * | |||||
| Excellent | 139 (27.2) | 65 (46.8) | 57 (41.0) | 18 (12.9) | 53 (38.1) | 121 (87.1) |
| Good | 325 (63.6) | 200 (61.5) | 187 (57.5) | 59 (18.2) | 137 (42.2) | 294 (90.5) |
| Fair or Poor | 47 (9.2) | 39 (83.0) | 37 (78.7) | 14 (29.8) | 20 (42.6) | 43 (91.5) |
| Ever told by a physician | ||||||
| Diabetes | 26 (5.1) | 15 (57.7) | 17 (65.4) | 5 (19.2) | 7 (26.9) | 22 (84.6) |
| Hypertension | 112 (21.9) | 71 (63.4) | 72 (64.3) | 24 (21.4) | 41 (36.6) | 99 (88.4) |
| Heart Problems | 26 (5.1) | 15 (57.7) | 17 (65.4) | 4 (15.4) | 12 (46.2) | 23 (88.5) |
| Sleep Apnea | 52 (10.2) | 32 (61.5) | 30 (57.7) | 13 (25.0) | 19 (36.5) | 45 (86.5) |
| Breathing Problems | 35 (6.8) | 24 (68.6) | 24 (68.6) | 12 (34.3) | 22 (62.8) | 31 (88.6) |
| Arthritis | 28 (5.5) | 21 (75) | 19 (67.9) | 5 (17.8) | 9 (32.1) | 24 (85.7) |
| Weight Problems | 150 (29.4) | 102 (68) | 95 (63.3) | 34 (26.7) | 68 (45.3) | 137 (91.3) |
| Migraines | 43 (8.4) | 31 (72.1) | 30 (69.8) | 11 (25.6) | 17 (39.5) | 40 (93.0) |
| Depression | 73 (14.3) | 56 (76.7) | 48 (65.8) | 18 (24.7) | 39 (53.4) | 66 (90.4) |
| Any of the above conditions | 290 (56.8) | 194 (66.9)* | 179 (61.7)* | 60 (20.7) | 129 (44.5) | 262 (90.3) |
notes:
indicates a Wald chi square test of statistical significance at p<0.05. Race African American was collapsed with the Other stratum due to low cell numbers. With exception of the study sample column all percentages appearing in parentheses represent “row percentages” and not column percentages. For example, 61.3% of subjects aged 17–25 years were classified as having poor sleep quality whereas 38.7% aged 17–25 were classified as having good sleep quality. Three (n=3) respondents were missing data required for the BMI calculation. No statistical comparisons for poor sleep, fatigue, injury, error or adverse events, or compromised safety across health conditions (i.e., diabetes, depression, etc) due to low cell frequencies (n<30) and the likelihood for unstable chi-square statistics and corresponding p-values. We focused on the composite measure “Any of the above conditions” as a more stable indicator for statistical modeling inclusive of individual health status. We did not perform tests to identify differences in sleep quality, fatigue, or safety outcomes across the following agency affiliation characteristics (Census Region, Model Classification, Agency Ownership, and Number of Employees) due to the small cell numbers for several stratums and risk of producing unstable test-statistics and corresponding p-values. We did not perform tests for differences in sleep quality, fatigue, or safety outcomes across rural/urban status because the variable was highly correlated with the variable Agency Call Volume (p<0.0001). Investigators believed that Agency Call Volume would confound any differences identified across rural/urban status. We believed Agency Call Volume was a more legitimate variable for the purposes of this study.
Sleep Quality
Psychometric tests confirmed that, in this study sample, the PSQI had positive reliability and internal consistency in this study sample (α=0.72). The component score-total Pearson correlation coefficients ranged from 0.53 (p<0.0001) for the Use of Sleeping Medications component to a high of 0.70 (p<0.0001) for the Sleep Duration component. The mean component score to total PSQI score Pearson correlation (0.61) was comparable to prior studies.17
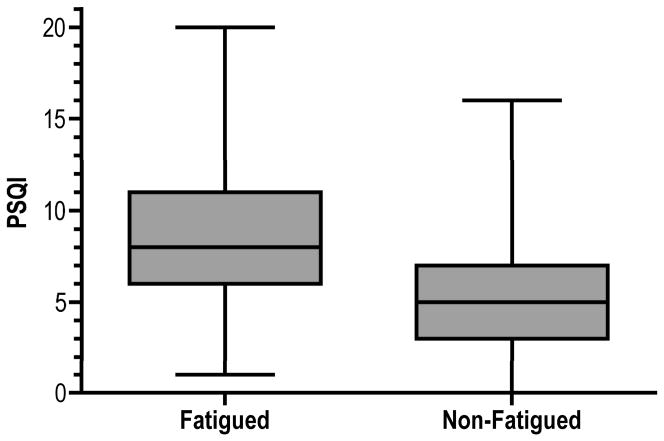
The mean PSQI score was 6.9 (95% CI 6.6, 7.2) and ranged from 0 – 20. Greater than half of all respondent PSQI scores exceeded the 6.0 benchmark for poor sleep quality (n=304, 59.5%; 95% CI 55.2–63.8%). The proportion of respondents with poor sleep scores was higher among full-time workers, respondents that commonly worked 24-hour shifts, and among those that worked at more than one EMS agency (p<0.05; Table 2). The mean sleep quality score among fatigued respondents was 3.1 points higher than the non-fatigued (p<0.0001, Figure 1).
Figure 1. Association between poor sleep quality scores and fatigue.
Notes: This box plot illustrates medians, the 25th and 75th percentiles, and range of PSQI scores stratified by fatigue status.
Fatigue
Psychometric tests confirm the CFQ had positive reliability and construct validity properties in this study sample. Cronbach’s coefficient alpha was acceptable for both physical and mental fatigue constructs (0.88 and 0.69, respectively). Component score-total Pearson correlation coefficients for physical and mental fatigue were 0.94 (p<0.001) and 0.78 (p<0.001). The CFA findings confirm the data fit the hypothesized two construct model: SRMR=0.05, GFI=0.91, CFI=0.92, NNFI=0.88, and NFI=0.91. Item-construct Pearson correlations ranged from 0.45 to 0.76 and construct-to-construct Pearson correlation was 0.53.
Greater than half of respondents were classified as fatigued while at work (n=281, 55.0%; 95% CI 50.7, 59.3%). The proportion of respondents classified as fatigued was highest among full-time workers, persons working 6–15 shifts monthly, respondents that commonly worked 24 hour shifts, and respondents with fair or poor self-rated general health (p<0.05; Table 2).
Injury
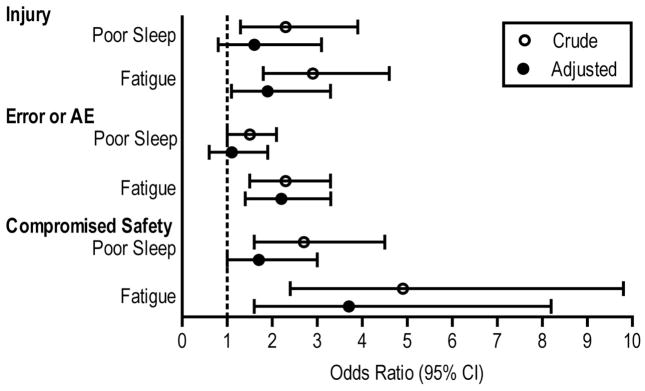
Eighteen percent of respondents reported being injured in previous three months (n=91, 17.8%, 95% CI 13.5, 22.1%; Table 2). The proportion of EMS workers injured was higher among paramedics and respondents working 6–15 shifts monthly than among respective reference groups (p<0.05; Table 2). Odds of injury were 2.3 times higher among respondents with poor sleep than respondents with good sleep (OR=2.3, 95%CI 1.3, 3.9; Table 3, Figure 2). Odds of injury were 2.9 times higher among fatigued respondents than non-fatigued (OR=2.9, 95%CI 1.8, 4.6; Table 3, Figure 2).
Table 3.
Odds of safety outcomes adjusted for confounding and clustering
| Injury Model OR (95%CI) | Error or Adverse Event Model | Compromised Safety Model | |
|---|---|---|---|
| (Unadjusted) Poor Sleep | 2.3 (1.3, 3.9) | 1.5 (1.0, 2.1) | 2.7 (1.6, 4.5) |
| (Unadjusted) Fatigue | 2.9 (1.8, 4.6) | 2.3 (1.5, 3.3) | 4.9 (2.4, 9.8) |
| (Adjusted) Poor Sleep | 1.6 (0.8, 3.1) | 1.1 (0.6, 1.9) | 1.7 (1.0, 3.1) |
| (Adjusted) Fatigue | 1.9 (1.1, 3.3)* | 2.2 (1.4, 3.3)* | 3.6 (1.5, 8.3)* |
| Age | |||
| 17–25 years | REF | ||
| 26–35 years | 0.6 (0.3, 1.2) | ||
| 36–45 years | 0.6 (0.3, 1.3) | ||
| ≥46 years | 0.4 (0.2, 1.1) | ||
| Race | * | ||
| White | REF | ||
| African American & Other | 0.4 (0.2, 0.9) | ||
| Alcohol Intake per Week | |||
| Do not drink alcohol | REF | ||
| 1–3 drinks | 1.3 (0.8, 2.1) | ||
| 4–10 drinks | 1.2 (0.7, 1.9) | ||
| >10 drinks | 2.0 (1.0, 3.8) | ||
| Self-Rated General Health | |||
| Excellent | REF | ||
| Good | 1.3 (0.8, 2.1) | ||
| Fair or Poor | 2.0 (0.7, 5.8) | ||
| Certification | * | * | |
| EMT-Basic | REF | REF | REF |
| EMT-Paramedic | 1.6 (1.0, 2.5) | 5.3 (3.1, 9.1) | 2.6 (1.5, 4.5) |
| Years Experience | * | ||
| 0–10 years | REF | ||
| 11–20 years | 0.5 (0.3, 0.9) | ||
| ≥21 years | 0.3 (0.2, 0.6) | ||
| Employment Status | |||
| Full-Time | REF | ||
| Part-Time | 1.1 (0.4, 2.5) | ||
| Volunteer | 0.7 (0.07, 7.2) | ||
| Number of Shifts per Month | * | ||
| 0–5 shifts | REF | REF | |
| 6–15 shifts | 3.8 (1.1, 12.7) | 3.2 (1.6, 6.3) | |
| ≥16 shifts | 4.0 (1.1, 14.0) | 2.9 (1.4, 6.0) | |
| Shift Most Commonly Work | |||
| ≤12 hours | REF | REF | REF |
| 24 hours | 1.4 (0.8, 2.5) | 0.8 (0.5, 1.3) | 1.1 (0.6, 1.8) |
| Agency Call Volume | |||
| ≤5,000 | REF | ||
| 5,001–15,000 | 1.7 (1.0–2.9) | ||
| >15,000 | 0.9 (0.5–1.9) |
Notes:
=indicates the variable was statistically significant at p<0.05 in the full cluster and confounding adjusted model. We assessed the fit of our logistic models by evaluating three measures of model fit and four global tests in response to eliminating non-significant variables from our full models as shown in this table. The Akaike Information Criterion (AIC) and Schwarz Criterion (SC) are commonly listed statistics of model fit for logistic regression models with smaller values of AIC and SC indicating better the model fit. We determined that the change in values of AIC and SC is insignificant for reduced models of all three outcomes indicating the full model is an adequate fit of study data. Other commonly cited model fit statistics include the Adjusted R2, Likelihood Ratio Chi-Square Test, Score Chi-Square Test, and Wald Chi-Square Test. The higher the Adjusted R2 value, the greater the proportion of variance the fitted model has explained in the data. The Likelihood Ratio Chi-Square, Score Chi-Square, and Wald Chi-Square test the null hypothesis that all variables in the model are equal to zero, with the alternative that at least one variable is not equal to zero. For all three models, the three chi-square tests were reduced but remained statistically significant following a reduction in the number of variables in the models. For all three outcomes, the Adjusted R2 statistics were reduced following a drop in the number of non-significant independent variables in the models. Taken together, these statistics suggest that while the three full fitted models shown in this table can be improved, our full (fitted) models fit the data well and a reduction in independent variables has an insignificant impact on model fit.
Figure 2. Crude and cluster/confounding-adjusted odds of safety outcomes associated with poor sleep and fatigue.
Notes: Adjusted odds ratios from Table 3. These ORs were adjusted for clustering within agencies and confounding.
Medical Error and Adverse Events
Four of every 10 respondents reported one or more medical errors or AEs in the previous three months (n=210, 41.1%, 95% CI 36.8, 45.4%; Table 2). The proportion of respondents reporting a medical error or AE was highest among the youngest age stratum (17–25 years), white respondents, certified paramedics, persons with fewer years of EMS experience, respondents working 6–15 shifts monthly, and among respondents that work longer shift hours and at more than one EMS agency (p<0.05; Table 2). Odds of reporting an error or AE in previous three months were 50% higher among respondents with poor sleep than respondents with good sleep (OR=1.5, 95%CI 1.0, 2.1; Table 3, Figure 2). Odds of error and AE were 2.3 times higher among fatigued respondents than non-fatigued respondents (OR=2.3, 95%CI 1.5, 3.3; Table 3, Figure 2).
Safety Compromising Behaviors
Ninety percent of respondents perceived that their safety or the safety of their patients was compromised during the prior three months of work (89%, 95%CI 87%, 92%; Table 2). The proportion of respondents with perceptions of compromised safety was highest among certified paramedics and among respondents that commonly worked longer shift hours (p<0.05, Table 2). Odds of perceived compromised safety were 2.7 times higher among respondents with poor sleep than respondents with good sleep (OR=2.7, 95%CI 1.6, 4.5; Table 3, Figure 2). Odds of perceived compromised safety were 4.9 times higher among fatigued respondents than the non-fatigued (OR=4.9, 95%CI 2.4, 9.8; Table 3, Figure 2).
Cluster Adjusted Multivariable Logistic Models
The odds that a respondent with poor sleep or fatigue would report an injury were attenuated after adjusting for poor sleep and fatigue simultaneously and all possible confounders (Table 3, Figure 2). The association between poor sleep and injury was reduced to non-significance while odds of injury related to fatigue remained statistically significant (OR=1.9, 95% CI 1.1, 3.3; Table 3, Figure 2). Similar to the adjusted model for injury, odds of error or AE were reduced after controlling for poor sleep, fatigue, and possible confounders. Odds of an error or AE are highest among whites, paramedics, respondents with the least years of EMS experience, and respondents that work 6–15 shifts monthly (Table 3, Figure 2). Finally, the odds that a respondent with poor sleep or fatigue perceived his or her personal or patient safety as compromised in previous three months was reduced after controlling both poor sleep and fatigue and possible confounders (Table 3, Figure 2).
DISCUSSION
In this study sample of EMS workers, we identified associations between sleep quality, fatigue, and self-reported safety outcomes. More than half of respondents had poor sleep quality or severe fatigue while at work. Fatigue was associated with all three composite measures of safety outcomes after controlling for confounding variables. Our findings are early evidence that poor sleep quality and fatigue may jeopardize patient and provider safety in the EMS setting.
In this study sample, the number of shifts worked monthly was linked to reported errors and AEs but not injury or perceptions of compromised safety. Longer shift hours (24 vs. ≤12 hours) were not associated to higher odds of negative safety outcomes. In contrast, nurses working shifts ≥ 12.5 hours commit more medical errors than those working shorter shifts.29 Medical interns experience a substantial reduction in errors when extended work shifts were eliminated and the number of weekly work hours was reduced.30 Extended-duration work shifts may contribute to fatigue and impair performance and safety.28 Long periods without rest can impair cognitive and motor performance, even to the degree of alcohol intoxication.31 Shift length for EMS workers can be long and interrupt normal circadian sleep periods resulting in detrimental effects on EMS worker performance and patient care quality.28, 32
The lack of association between shift length and safety outcomes in this study sample may be explained by an unmeasured factor in this study: varying amounts of workload during shifts measured at the individual worker level. An EMT’s workload is variable and influenced by many factors. Dispatch timing and the amount of work required for a given response are often unpredictable. Workload depends on call volume, proximity to receiving facilities, crowding in the Emergency Department, and a host of other factors. Many EMS workers may be busy the entire shift while others may have time to include a nap or rest during downtime to curb fatigue and sleepiness.
High workload during shift work is associated with higher odds of negative safety outcomes in other settings.33, 34 In a study of hospital-based nursing care, a higher rate of pneumonia and urinary tract infections was linked to increased workload and limited staffing.35 We did not capture workload at the individual level. Excluding safety-compromising behaviors, we did not detect differences in safety outcomes, sleep quality, or fatigue across three stratums of agency call volume. It may be that respondents that traditionally work 24-hour shifts rest and reduce odds of a negative outcome. Our finding higher odds of a medical error or AE among respondents that work 6–15 shifts per month is provocative and deserves further study involving an individual or team-level measure of workload.
Research subsequent to the release of the Institute of Medicine’s (IOM) 2008 report on resident hours resulted in aggressive action adopted by the Accreditation Council for Graduate Medical Education (ACGME).36 A parallel effort targeting EMS workers may lead to new studies and research to improve our understanding of the causal relationships between fatigue, sleep, shift hours, and safety outcomes. These data suggest that number of shifts and total fatigue may be important targets for intervention in EMS workers in place of shift length.
LIMITATIONS
Our findings may not generalize to all EMS workers. This study utilized a convenience sample of EMS providers that resemble EMS workers across the U.S. (Table 4). Our response rate is comparable to prior multi-agency studies of EMS workers and other survey-based research of health care professionals.37, 38 Several differences between respondents and non-respondents may impact study findings. The proportion of non-respondents certified at the EMT-Paramedic level was lower than respondents (48% vs. 59%, p<0.0001). The proportion of non-respondents that work full-time was lower than the proportion among respondents (57% vs. 76%; p<0.0001). Non-respondents had fewer median years of agency service than respondents (4 vs. 5; p<0.05).
Table 4.
Characteristics of study sample compared to other research studies of EMS workers
| Characteristic | Study Sample
|
LEADS Sample48 | High Response EMS Sample49 | NHTSA Workforce Report50** | Resuscitation Outcomes Consortium Agencies51 | Longitudinal Study of EMS Turnover52 | National Survey of EMS Safety Culture37 | |
|---|---|---|---|---|---|---|---|---|
| Respondents | Non- Respondents | |||||||
| Individual Characteristics | ||||||||
|
| ||||||||
| Sex | ||||||||
| Male | 74% | --- | 72.9% | 71.8% | 71–77% | --- | --- | 73.2% |
| Female | 26% | --- | 27.1% | 28.2% | 23–29% | --- | --- | 26.8% |
|
| ||||||||
| Certification | ||||||||
| EMT-Basic | 40.5% | 52% | 58.1% | 50.7% | #72% | 58.2% | --- | 19.4% |
| Paramedic | 59.5% | 48% | 34.6% | 49.3% | #22% | 34.2% | --- | 62.1% |
|
| ||||||||
| Mean Age in Years | 37.2 | --- | --- | --- | 35 | --- | --- | --- |
|
| ||||||||
| Race | ||||||||
| White | 93.5% | --- | --- | --- | 75–81% | --- | --- | --- |
| Non-White | 6.5% | --- | --- | --- | 19–25% | --- | --- | --- |
|
| ||||||||
| Employment Status | ||||||||
| Full-Time | 75.7% | 56.9% | --- | --- | $89% | --- | --- | 77.6% |
| Part-Time | 15.5% | 33.6% | --- | --- | $11% | --- | --- | 20.6% |
| Volunteer | 26.6% | 9.5% | --- | --- | --- | --- | 1.8% | |
|
| ||||||||
| Agency Affiliation (EMT unit of measurement) | ||||||||
| Fire-Based | 9.6% | 7.4% | 34.1% | --- | +Includes county/3rd | --- | --- | --- |
| County/3rd Service | 50% | 60% | 12.1% | --- | +30%^^ | --- | --- | --- |
| Hospital | 15% | 14% | 9.9% | --- | 20%^^ | --- | --- | --- |
| Other | 25.4% | 18.6% | 43.8% | --- | 50%^^ | --- | --- | --- |
|
| ||||||||
| Mean Years of Service at Agency | 7.1 | 6.2 | --- | --- | --- | --- | --- | --- |
|
| ||||||||
| Mean Percentage of Work devoted to Clinical Field Work (not administrative) | 61% | 69% | --- | --- | --- | --- | --- | --- |
|
| ||||||||
| Smoking Status | ||||||||
| Never/Do not smoke | 84.5% | --- | 83.0% | --- | --- | --- | --- | --- |
| Smoke | 15.5% | --- | 17.0% | --- | --- | --- | --- | --- |
|
| ||||||||
| BMI | ||||||||
| Normal weight | 21.9% | --- | 28.8% | --- | --- | --- | --- | --- |
| Overweight/Obese | 77.5% | --- | 71.2% | --- | --- | --- | --- | --- |
|
| ||||||||
| Agency Characteristics (Agency Unit of Measurement) | ||||||||
|
| ||||||||
| Agency Affiliation | ||||||||
| Fire-Based | 3.3% | --- | --- | --- | 62.5% | 10.0% | 11.5% | |
| County/3rd Service | 36.7% | --- | --- | --- | 25.7% | 22.5% | 19.7% | |
| Hospital | 13.3% | --- | --- | --- | N/A | 27.5% | 29.5% | |
| Other (i.e. private) | 46.7% | --- | --- | --- | 11.8% | 40.0% | 39.3% | |
The NHTSA Workforce report includes statistics based on data from the 2003 and 2005 Current Population Survey (CPS), the 2007 National Registry of EMTs (NREMT) registration database, the 2004–05 Edition of the Bureau of Labor Statistics Occupational Outlook Handbook.
indicates source was the 2007 NREMT database statistics cited within the NHTSA Workforce report and excludes statistics from EMT-Intermediates.
=is used to indicate data from this source does not stratify EMTs by volunteer status and automatically labels an EMT as Full-Time based on the EMT working greater than or equal to 35 hours per week.
Categories reported in the NHTSA Workforce report are not completely analogous to the stratums defined in this study. We collapsed several categories in the NHTSA Workforce report deemed similar to stratums in this study (e.g. 50% Other includes “private ambulance services and ‘other’ in the Workforce Report; and 30% County/3rd service includes all types of local government types).
The mean of medians reported in Table 2 of the Davis et al, 2007 publication.
For the ROC agency affiliation, the categories are Fire-Based, Non-fire government (county/3rd service), and Private (other).
We developed our own measure of safety outcomes given a lack of standardized measurements for safety outcomes in EMS. We used a modified Delphi consensus-driven approach and a multidisciplinary panel in light of known limitations with independent reviews and ratings of outcomes by medical oversight physicians.39, 40 The EMS-SI tool is unique to EMS, but comparable to a patient safety indicator tool developed by AHRQ and tested in prior large scale safety studies.20
The self-report nature of our safety outcome measures is a strength and weakness. We adopted a three-month period of recall in recognition that occupational epidemiologists consider the accuracy of recall to diminish several months post event.41, 42 In prior research, EMTs under report medical errors and adverse events by an estimated 4%.43–45 There is additional evidence that between 11% and 32% of occupational injuries and accidents are not voluntarily reported.46, 47 Underreporting may be attributed to an unwillingness to report, particularly in agencies where a fear of retribution may result from a poor safety culture. The EMS-SI may not provide a complete picture of error, AE, and safety compromising behaviors in EMS agencies. We believe it can provide a window into specific behaviors and actions that threaten EMS safety. The distribution of EMS-SI responses across demographic factors (i.e. certification level) deserves further study. For example, is the proportion of EMT-Paramedics answering in the affirmative for safety-compromising behaviors most often associated with on-the-job experience or some other factor? Modifications to the EMS-SI are warranted to include new items that may capture additional actions and behaviors that threaten safety. Additional research is needed to examine the association between self-report and actual reported outcomes. Managers and medical directors may wish to use this tool in an anonymous fashion as an initial step towards identifying specific threats to safety that go undocumented using existing quality assurance or reporting mechanisms.
We believe our findings do not highlight the true strength, but underestimate the association between sleep quality, fatigue, and safety outcomes. Our findings may be impacted by individual-level work-related characteristics not captured as part of our study protocol. For example, we did not include a measure of individual EMS worker workload or ask if respondents were allowed to take naps or engage in other rest behaviors during shift work. We believe that future research should include these measures to determine their association with sleep, fatigue, and safety outcomes. Our findings provide preliminary evidence that in one subset of the EMS population, sleep quality and fatigue are important indicators of safety.
CONCLUSIONS
In this sample of EMS workers, poor sleep quality and fatigue are common. We provide preliminary evidence of an association between sleep quality, fatigue, and safety outcomes.
Acknowledgments
Supported by grants from the Pittsburgh Emergency MedicineFoundation (PEMF) and North Central EMS Institute (NCEMSI). Dr. Patterson is supported by an early investigator training grant (Number KL2 RR024154) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
References
- 1.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academies of Science; 2000. [PubMed] [Google Scholar]
- 3.WHO. WHO Patient Safety Curriculum Guide for Medical Schools. Geneva: 2009. [Google Scholar]
- 4.Nasca TJ, Day SH, Amis ES, Force ADHT. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2) doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 5.Rittenberger JC, Beck PW, Paris PM. Errors of omission in the treatment of prehospital chest pain patients. Prehosp Emerg Care. 2005;9(1):2–7. doi: 10.1080/10903120590891688. [DOI] [PubMed] [Google Scholar]
- 6.Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic intubation errors: isolated events or symptoms of a larger problem? Health Aff (Millwood) 2006;25(2):501–509. doi: 10.1377/hlthaff.25.2.501. [DOI] [PubMed] [Google Scholar]
- 7.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehosp Emerg Care. 2007;11(1):80–84. doi: 10.1080/10903120601021358. [DOI] [PubMed] [Google Scholar]
- 8.Wang HE, Weaver MD, Abo BN, Kaliappan R, Fairbanks RJ. Ambulance stretcher adverse events. Qual Saf Health Care. 2009;18(3):213–216. doi: 10.1136/qshc.2007.024562. [DOI] [PubMed] [Google Scholar]
- 9.Suyama J, Rittenberger JC, Patterson PD, Hostler D. Comparison of public safety provider injury rates. Prehosp Emerg Care. 2009;13(4):451–455. doi: 10.1080/10903120903144908. [DOI] [PubMed] [Google Scholar]
- 10.Workplace Injuries and Illnesses - 2009. Washington, DC: US Department of Labor; 2010. [Google Scholar]
- 11.Reichard AA, Jackson LL. Occupational injuries among emergency responders. Am J Ind Med. 2010;53(1):1–11. doi: 10.1002/ajim.20772. [DOI] [PubMed] [Google Scholar]
- 12.Hogya PT, Ellis L. Evaluation of the injury profile of personnel in a busy urban EMS system. American Journal of Emergency Medicine. 1990;8(4):308–311. doi: 10.1016/0735-6757(90)90081-a. [DOI] [PubMed] [Google Scholar]
- 13.Patterson PD, Probst JC, Leith KH, Corwin SJ, Powell MP. Recruitment and retention of emergency medical technicians: a qualitative study. J Allied Health. 2005 Fall;34(3):153–162. [PubMed] [Google Scholar]
- 14.Brown WE, Jr, Dickison PD, Misselbeck WJ, Levine R. Longitudinal Emergency Medical Technician Attribute and Demographic Study (LEADS): an interim report. Prehosp Emerg Care. 2002 Oct–Dec;6(4):433–439. doi: 10.1080/10903120290938085. [DOI] [PubMed] [Google Scholar]
- 15.Denlinger RF, Gonzenbach K. “The Two-Hat Syndrome”: Determining Response Capabilities and Mutual Aid Limitations. Boston, MA: Harvard University the John F. Kennedy School of Government and US Department of Justice; Aug, 2002. p. 2002. [Google Scholar]
- 16.Patterson PD, Suffoletto BP, Kupas DF, Weaver MD, Hostler D. Sleep quality and fatigue among prehospital providers. Prehosp Emerg Care. 2010;14(2):187–193. doi: 10.3109/10903120903524971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989 May;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 18.Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–153. doi: 10.1016/0022-3999(93)90081-p. [DOI] [PubMed] [Google Scholar]
- 19.Patterson PD, Weaver MD, Martin-Gill C, et al. [Abstract #106] Results from the Emergency Medical Services provider and patient safety inventory tool. Prehosp Emerg Care. 2011;15(1):134. [Google Scholar]
- 20.Singer S, Lin S, Falwell A, Gaba D, Baker L. Relationship of safety climate and safety performance in hospitals. Health Serv Res. 2009 Apr;44(2 Pt 1):399–421. doi: 10.1111/j.1475-6773.2008.00918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peterson RA. A meta-analysis of cronbach/s coefficient alpha. J Consum Res. 1994;21(2):381–391. [Google Scholar]
- 22.Hatcher L. A Step-by-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling. Cary, North Carolina: SAS Institute Inc; 1994. [Google Scholar]
- 23.Lance CE, Butts MM, Michels LC. The sources of four commonly reported cutoff criteria- What did they really say? Organizational Research Methods. 2006;9(2):202–220. [Google Scholar]
- 24.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 25.Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: the effect of sample size. Psychol Bull. 1988;103(3):411–423. [Google Scholar]
- 26.Ware JE, Gandek B. Methods for Testing Data Quality, Scaling Assumptions, and Reliability: The IQOLA Project Approach. J Clin Epidemiol. 1998;51(11):945–952. doi: 10.1016/s0895-4356(98)00085-7. [DOI] [PubMed] [Google Scholar]
- 27.Lockley SW, Ayas NT, Rothschild JM, et al. Effects of health care provider work hours and sleep deprivation on safety and performance. Jt Comm J Qual Patient Saf. 2007;33(11 Suppl):7–18. doi: 10.1016/s1553-7250(07)33109-7. [DOI] [PubMed] [Google Scholar]
- 28.Lockley SW, Barger LK, Ayas NT, et al. Effects of health care provider work hours and sleep deprivation on safety and performance. Jt Comm J Qual Patient Saf. 2007;33(11 Suppl):7–18. doi: 10.1016/s1553-7250(07)33109-7. [DOI] [PubMed] [Google Scholar]
- 29.Rogers AE, Hwang WT, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff nurses and patient safety. Health Aff (Millwood) 2004 Jul–Aug;23(4):202–212. doi: 10.1377/hlthaff.23.4.202. [DOI] [PubMed] [Google Scholar]
- 30.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns/ work hours on serious medical errors in intensive care units. N Engl J Med. 2004 Oct 28;351(18):1838–1848. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 31.Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000 Oct;57(10):649–655. doi: 10.1136/oem.57.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Costa G. The impact of shift and night work on health. Appl Ergon. 1996;27(1):9–16. doi: 10.1016/0003-6870(95)00047-x. [DOI] [PubMed] [Google Scholar]
- 33.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 34.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 35.Kovner C, Gergen PJ. Nurse staffing levels and adverse events following surgery in U.S. hospitals. Image J Nurs Sch. 1998;30(4):315–321. [PubMed] [Google Scholar]
- 36.IOM (Institute of Medicine) Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 37.Patterson PD, Huang DT, Fairbanks RJ, Simeone SJ, Weaver MD, Wang HE. Variation in emergency medical services workplace safety culture. Prehosp Emerg Care. 2010;14(4):448–460. doi: 10.3109/10903127.2010.497900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 39.Patterson PD. Use of ED diagnosis to determine medical necessity of EMS transports. Prehosp Emerg Care. 2006;10(4):6. doi: 10.1080/10903120600886918. [DOI] [PubMed] [Google Scholar]
- 40.Patterson PD, Martin-Gill C, Roth RN, et al. [Abstract] Identification of Adverse Events in ground EMS by medical directors. Prehosp Emerg Care. 2010;14(Suppl 1):15. [Google Scholar]
- 41.Landren DD, Hendricks S. Effect of recall on reporting of at-work injuries. Public Health Rep. 1995;110(3):350–354. [PMC free article] [PubMed] [Google Scholar]
- 42.Jenkins P, Earle-Richardson G, Slingerland DT, May J. Time dependent memory decay. Am J Ind Med. 2002;41(2):98–101. doi: 10.1002/ajim.10035. [DOI] [PubMed] [Google Scholar]
- 43.Fairbanks RJ, Crittenden CN, O/Gara KG, et al. Emergency medical services provider perceptions of the nature of adverse events and near-misses in out-of-hospital care: an ethnographic view. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine. 2008 Jul;15(7):633–640. doi: 10.1111/j.1553-2712.2008.00147.x. [DOI] [PubMed] [Google Scholar]
- 44.Hobgood C, Bowen JB, Brice JH, Overby B, Tamayo-Sarver JH. Do EMS personnel identify, report, and disclose medical errors? Prehospital emergency care: official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2006 Jan–Mar;10(1):21–27. doi: 10.1080/10903120500366011. [DOI] [PubMed] [Google Scholar]
- 45.Vilke GM, Tornabene SV, Stepanski B, et al. Paramedic self-reported medication errors. Prehospital emergency care: official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2007 Jan-Mar;11(1):80–84. doi: 10.1080/10903120601021358. [DOI] [PubMed] [Google Scholar]
- 46.Cutter J, Jordan S. Uptake of guidelines to avoid and report exposure to blood and body fluids. Journal of advanced nursing. 2004 May;46(4):441–452. doi: 10.1111/j.1365-2648.2004.03010.x. [DOI] [PubMed] [Google Scholar]
- 47.Bjerkan AM. Health, environment, safety culture, and climate - analysing the relationships to occupational accidents. J Risk Research. 2010;13(4):445–477. [Google Scholar]
- 48.Studnek JR, Bentley M, Crawford JM, Fernandez AR. An assessment of key health indicators among emergency medical services professionals. Prehosp Emerg Care. 2010;14(1):14–20. doi: 10.3109/10903120903144957. [DOI] [PubMed] [Google Scholar]
- 49.Patterson PD, Huang DT, Fairbanks RJ, Wang HE. The emergency medical services safety attitudes questionnaire. Am J Med Qual. 2010;25(2):109–115. doi: 10.1177/1062860609352106. [DOI] [PubMed] [Google Scholar]
- 50.Chapman SA, Lindler V, Kaiser JA, Nielsen CS, Bates T, Hailer-O/Keefe L. Emergency Medical Services Workforce for the 21st Century Project. Washington, D.C: National Highway Traffic Safety Administration; 2008. [Google Scholar]
- 51.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 52.Patterson PD, Jones CB, Hubble MW, et al. The longitudinal study of turnover and the cost of turnover in emergency medical services. Prehosp Emerg Care. 2010;14(2):209–221. doi: 10.3109/10903120903564514. [DOI] [PMC free article] [PubMed] [Google Scholar]