Summary
The inflammatory milieu of the cervix may play a role in preventing intrauterine infection and subsequent preterm birth. The objectives of this study were to use exploratory factor analysis to discover the underlying structure of cytokines in the lower genital tract immunologic milieu, and evaluate the association between the cytokine factors and risk of preterm birth. Women (n=613) enrolled in a prospective pregnancy cohort study in Pittsburgh, Pennsylvania had cervical cytokine concentrations assayed at <16 weeks and were followed for data on pregnancy outcomes. Principal factor analysis identified 2 primary cytokine patterns at <16 weeks gestation: Factor 1 (proinflammatory / immunomodulatory factor), which loaded highly on interleukin (IL)-1β, IL-6, IL-8, monocyte chemotactic protein-1, and IL-10, and Factor 2 (anti-inflammatory factor), which loaded heavily on IL-4, IL-10, and IL-13. Women in the highest tertile of anti-inflammatory cytokine factor scores at <16 weeks had an increased risk of spontaneous preterm birth (confounder-adjusted odds ratio (95% CI): 2.4 (1.1, 5.7)). There was no association between pro-inflammatory cytokine factor scores and preterm birth risk. These data support the hypothesis that increased concentrations of anti-inflammatory cytokines may represent a cervical immune milieu that permits subsequent microbial invasion of the uterus during pregnancy, leading to subsequent spontaneous preterm birth.
Introduction
Preterm birth is the most important cause of illness, handicap, and mortality to newborns in the developed world.1 A major contributor to preterm birth is intrauterine infection.2 Intrauterine infection is thought to result from the ascent of vaginal bacteria into the uterus.3 The resultant infection and inflammatory cascade contribute to preterm birth and adverse neonatal outcomes. The nature of the immunologic barrier that prevents bacteria from invading the upper tract is poorly understood. We have hypothesized that the inflammatory milieu of the cervix plays a role in this process.
To characterize the immune milieu of the cervix, we have focused on cytokines. In vivo, cytokines function as part of an elaborate and complex network of molecules that mediate the innate immune response. Recognizing this, we have previously considered cytokines in functional clusters and created a measure of pro- and anti-inflammatory cytokine balance.4 In our exploration of the relationship of this functional balance with the risk of subsequent preterm birth, we defined interleukin (IL)-1α, IL-1β, IL-8, and IL-6 as representing pro-inflammatory processes and IL-4, IL-10, and IL-13 as representing anti-inflammatory processes. We categorized subjects into one of three strata: high pro-inflammatory/low anti-inflammatory; high anti-inflammatory/low pro-inflammatory; or balanced. Women in the high anti-inflammatory/low pro-inflammatory stratum had a subsequent adjusted odds ratio for preterm birth <34 weeks of 7.7 (95% confidence interval, 4.9, 9.1), which suggests that women with a relatively more anti-inflammatory cervical inflammatory milieu in early pregnancy are at higher risk of subsequent early preterm birth.
However, in these analyses, the grouping of cytokines and the uniform weighting of their contribution to preterm birth may not reflect the truest biological relationships. We had two objectives for the current study. First, we sought to use exploratory factor analysis to discover the underlying structure of cytokines in the lower genital tract immunologic milieu. We used factor analysis rather than other data reduction techniques because we believe that cervical cytokines concentrations are manifestation of larger underlying constructs (factors), which explains the high correlation patterns among them. Second, we evaluated the association between the cytokine factors and preterm birth (predictive validity).
Methods
The Study of Nutrition and Pregnancy is an ongoing prospective cohort study of pregnant women seeking care at Magee-Womens Hospital resident antepartum clinics in Pittsburgh, PA. The antepartum clinics serve a predominantly publically insured, low-income population. Women with singleton pregnancies, no known preexisting conditions, vaginal bleeding, fetal anomalies, or current or planned cervical cerclage, and who self-reported their race/ethnicity as non-Hispanic white or black were eligible. Women were enrolled at <16 weeks gestation (mean 9.5 weeks) after providing informed, written consent. The study was approved by the University of Pittsburgh Institutional Review Board.
At enrollment, women underwent a standard pelvic examination and completed an interviewer-administered questionnaire to collect data on sociodemographic characteristics; medical, reproductive, and sexual history; and maternal behaviors. They were followed up for information on pregnancy outcome, which was ascertained through medical chart abstraction. A total of 687 eligible women enrolled in the study. Of these, 613 (89%) had cervical fluid available for cytokine assay, and were therefore used to generate the cytokine factors. When we studied cytokine factors relative to preterm birth, the sample was reduced to n=497 after eliminating women who had a spontaneous or therapeutic abortion (n=67), transferred care (n=27), were lost to follow-up (n=6), delivered a stillbirth (n=6), or had not yet delivered (n=10). Women excluded from the preterm birth analysis were more likely than women included in the analysis to have less than a high-school education (21% vs. 26%). However, there were no meaningful differences between groups in terms of race/ethnicity, parity, marital status, smoking status, or age (data not shown).
During a speculum examination at enrollment, a Dacron swab was placed in the cervix and left there for 10 seconds to achieve saturation. The swab was then placed in a plastic tube containing 400 μl of PBS (final dilution of 1:5), immediately transported to the laboratory, and stored at −20°C. The buffer did not contain any other additives, including protease inhibitors. For analysis, the specimens were thawed at room temperature. The swab and the remaining diluent were centrifuged in a spin-X centrifuge filter unit (Costar, Cambridge, MA) at 12,000 rpm for 20 minutes. Concentrations of IL-1β, IL-6, IL-8, monocyte chemotactic protein (MCP)-1 IL-4, IL-10, and IL-13, were measured using the Luminex LabMAP® multiplex system and a BeadLyte bead kit (Upstate, Lake Placid, NY). Each assay was run with an intra- and inter-assay variation of <10%. For all analytes, the lower limit of sensitivity of the assay was 3.5 pg/ml. The percent of women with cytokine concentrations below the detection limit were 11% (IL-1β), 11% (IL-4), 2% (IL-6), 0% (IL-8), for 14% (IL-10), 27% (IL-13), and 0.3% (MCP-1). Women with IL-4, IL-10, and IL-13 below the detection limit (n=6) or IL-1β and IL-6 below the detection limit (n=2) were not included in the analysis because we felt that inability to detect concentration of multiple cytokines reflected an unusable sample rather than a bead assay failure. For the remaining observations with a value below the detection limit, we imputed the limit of detection divided by the square-root of 2.
Specimens obtained from the enrollment pelvic exam were also used to classify women as having sexually transmitted infections (Trichomonas vaginalis, Chlamydia trachomatis or Neisseria gonorrhoeae), using methods described previously 5. Additionally, two vaginal swabs were collected for culture and identification of vaginal flora. Bacterial vaginosis was diagnosed by vaginal pH ≥ 4.7 and a score of 7 through 10 from a Gram-stained vaginal smear 6.
Gestational age was based on best obstetrical estimate, i.e., from a reliable, self-reported estimate of last menstrual period or an ultrasound early in pregnancy. Preterm birth was defined as a delivery of a live infant occurring at 16 to <37 completed weeks gestation. Spontaneous preterm birth (sPTB) was defined as a preterm delivery occurring after preterm labor with intact membranes or pretermprelabor rupture of the fetal membranes.
At enrollment, data on race/ethnicity, education, marital status, smoking status during pregnancy, parity, household income, and employment status were self-reported as part of the interviewer-administered questionnaire. Prepregnancy body mass index was defined as pregravid weight (kg) divided by measured height (m)2.
Statistical analysis
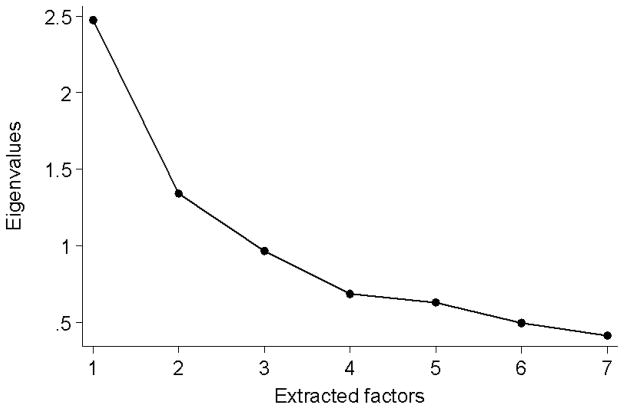
Cervical cytokine concentrations were divided into quintiles based on fifths of their distributions because the distributions were heavily skewed. An exploratory factor analysis was performed on cytokines using a principal factor method with oblique rotation (direct oblimin) on a Pearson correlation matrix.7, 8 The number of factors extracted was based on examination of eigenvalues, scree plots (Figure 1), and the interpretability of the solution. Once an initial estimate of the number of factors was made, neighboring solutions were also examined. The estimated factor scores (hereafter referred to as “factor scores”) were computed using a regression method 9 based on all 7 cytokines. All factor loading greater than or equal 0.2 were interpreted. Pair-wise Pearson correlation coefficients were generated to test the linear correlation between Factor 1 and Factor 2 scores. Factor scores were categorized based on tertiles of the distribution.
Figure 1.
Scree plot of eigenvalues of the 7 factors identified by exploratory factor analysis.
Multivariable logistic regression models were used to assess the association between the cytokine factor scores and the risk of preterm birth and sPTB. Potential confounders were race/ethnicity, smoking, age, marital status, education, income, employment, pregravid BMI, enrollment gestational age, and presence of BV or sexually transmitted infections. Our goal was to fit parsimonious regression models and removing confounders if their inclusion did not satisfy our a priori change-in-estimate criterion (>8% change in a cytokine factor odds ratio). None of these factors met our definition of confounding, but we adjusted for the presence of a sexually transmitted infection out of convention.
The presence of sexually transmitted infections may alter lower genital tract cytokine concentrations, so we ran the factor analysis and preterm birth models with and without women with any one of the sexually transmitted infections (n=70). Because the results were not meaningfully different, women with a sexually transmitted infection were included in all analysis.
Stata version 10 (StataCorp, College Station, TX) was used for analyses.
Results
The cohort was 55% non-Hispanic black and 45% non-Hispanic white. Nearly half of women smoked (46%). Study participants were predominantly 20 to 29 years old (71%), unmarried (83%), high-school educated (68%), unemployed (51%), overweight (pregravid BMI ≥ 25 kg/m2, 62%), and had a household income of <$25,000 (63%). The distribution of parity at enrollment was 0 (20%), 1 (42%), and ≥2 (38%).
Principal factor analysis identified 2 primary cytokine patterns at <16 weeks gestation. Before rotation, these factors accounted for 54% of the variance in cervical cytokine concentrations. The highest factor loadings in Factor 1 were for pro-inflammatory cytokines (IL-1β, IL-6, IL-8, and MCP-1) and IL-10, an anti-inflammatory cytokine. In this context, IL-10 likely represents a compensatory anti-inflammatory response that accompanies increased pro-inflammatory cytokine production. The cytokines that loaded most heavily on Factor 2 were anti-inflammatory cytokines (IL-4, IL-10, and IL-13). Factor 1 and Factor 2 scores were weakly correlated (r=0.21).
There were 59 cases of preterm birth (11.9%), including 42 that were sPTB cases (8.8%). There was no significant association between pro- or anti-inflammatory factor scores and preterm birth (Table 2). However, when limited to the study of sPTB, Factor 2 scores (anti-inflammatory) were significantly associated with sPTB (Table 3). Women in the highest tertile of Factor 2 scores were 2.4 times as likely as women in the lowest tertile of Factor 2 to subsequently deliver a sPTB.
Table 2.
Association between estimated cytokine factor scores and preterm birth (n=497)
| Cytokine factor | Term n (%) | Preterm n (%) | Unadjusted a preterm birth OR (95% CI) | Adjusted b preterm birth OR (95% CI) |
|---|---|---|---|---|
| Factor 1: Pro-inflammatory / immunomodulatory | ||||
| Tertile 1 (lowest) | 145 (90.6) | 15 (9.4) | 1.0 (ref) | 1.0 (ref) |
| Tertile 2 | 145 (86.3) | 23 (13.7) | 1.5 (0.7, 2.9) | 1.5 (0.7, 2.9) |
| Tertile 3 (highest) | 148 (87.6) | 21 (12.4) | 1.3 (0.6, 2.6) | 1.4 (0.6, 2.6) |
| Factor 2: Anti-inflammatory | ||||
| Tertile 1 (lowest) | 145 (91.9) | 14 (8.8) | 1.0 (ref) | 1.0 (ref) |
| Tertile 2 | 153 (87.9) | 21 (12.1) | 1.4 (0.7, 2.9) | 1.4 (0.7, 2.9) |
| Tertile 3 (highest) | 140 (85.4) | 24 (14.6) | 1.7 (0.8, 3.4) | 1.7 (0.8, 3.4) |
CI, confidence interval; OR, odds ratio
Models include only estimated Factor 1 and Factor 2 scores, without adjustment for covariates.
Models include Factor 1 scores, Factor 2 scores, and sexually transmitted infections. Adjustment for additional covariates had no meaningful impact any of the findings.
Table 3.
Association between estimated cytokine factor scores and spontaneous preterm birth (n=480)
| Cytokine factor | Term n (%) | sPTB n (%) | Unadjusted a sPTB OR (95% CI) | Adjusted b sPTB OR (95% CI) |
|---|---|---|---|---|
| Factor 1: Pro-inflammatory / immunomodulatory | ||||
| Tertile 1 (lowest) | 145 (94.2) | 9 (5.8) | 1.0 (ref) | 1.0 (ref) |
| Tertile 2 | 145 (90.1) | 16 (9.9) | 1.6 (0.7, 3.8) | 1.6 (0.7, 3.8) |
| Tertile 3 (highest) | 148 (89.7) | 17 (10.3) | 1.7 (0.7, 3.9) | 1.7 (0.7, 3.9) |
| Factor 2: Anti-inflammatory | ||||
| Tertile 1 (lowest) | 145 (94.8) | 8 (5.2) | 1.0 (ref) | 1.0 (ref) |
| Tertile 2 | 153 (91.6) | 14 (8.4) | 1.6 (0.7, 4.0) | 1.6 (0.7, 4.0) |
| Tertile 3 (highest) | 140 (87.5) | 20 (12.5) | 2.4 (1.1, 5.7) | 2.4 (1.1, 5.7) |
CI, confidence interval; OR, odds ratio; sPTB, spontaneous preterm birth
.Models include only estimated Factor 1 and Factor 2 scores, without adjustment for covariates.
Models include Factor 1 scores, Factor 2 scores, and sexually transmitted infections. Adjustment for additional covariates had no meaningful impact any of the findings.
Discussion
Using factor analysis, we identified a pro-inflammatory / immunomodulatory cytokine factor and an anti-inflammatory cytokine factor that reflect the underlying structure of the innate immune milieu of cervical fluid during pregnancy. While the pro-inflammatory cytokines all loaded together on Factor 1 and the anti-inflammatory cytokines all loaded together on Factor 2, IL-10 loaded in both factors. We speculate that IL-10 loads on Factor 1 because of the compensatory induction of IL-10 expression in the setting of increases in pro-inflammatory cytokines, as a modulator of the pro-inflammatory response.10–12 In contrast, IL-10 loads on Factor 2 along with IL-4 and IL-13 as a representation of constitutive, basal anti-inflammatory state. Importantly, the weights (factor loadings) of the cytokines are not identical. Our approach takes into account the differential contribution of cytokines to the innate immunological milieu of the lower genital tract. The factor analysis method allowed us to estimate scores that estimate the true underlying construct that drives these cytokine concentrations.
We noted a significant contribution of the anti-inflammatory factor to the risk of subsequent sPTB, but not preterm birth overall. This finding is supportive of the biologic contribution of ascending microbial invasion of the upper genital tract to preterm labor and preterm rupture of the membranes, whereas this phenomenon has not been reported to be important in the pathogenesis of indicated preterm births. These results are also consistent with our previous work on higher cervical anti-inflammatory cytokine concentrations and subsequent clinical chorioamnionitis13 and early preterm birth.4 Genc et al. suggested that an imbalance between pro- and anti-inflammatory cytokines in the lower genital tract may contribute to preterm birth related to an ascending pathway of infection. In this study, women in the midpregnancy with a disproportionate increase in IL-1β over IL-1ra and bacterial vaginosis were more likely to deliver before 37 weeks.14 Overall, these data support the notion that the immunologic milieu of the lower genital tract is an important contributor to the risk of preterm birth.
Our study was limited by a relatively small sample of preterm birth cases that prevented us from examining the interaction between anti- and pro-inflammatory factor scores on preterm birth risk, and studying these associations by etiology of preterm birth. We would expect the association between lower genital inflammatory milieu and preterm birth to be strongest with those preterm births that occur as a result of intrauterine infection/inflammation. Placental histopathology, culture, or polymerase chain reaction data would inform this issue. We are limited by the lack of availability of these data in the present work. Our study of cytokines only at <16 weeks gestation does not account for change in the lower genital tract inflammatory milieu over gestation, which may be important for subsequent preterm birth. Our imputation of cytokine concentrations below the detection limit with a uniform value has the potential to cause bias 15. Unfortunately, we could not apply newer methods for handling limits of detection 15, 16 because they cannot currently be applied to factor analysis. We are also limited by the number of markers of inflammation that we measured; our view of inflammation is defined by the lens with which we view it. Nevertheless, our consideration of multiple cytokine components of the lower genital tract innate immune response, and our data-driven approach to develop these factor scores are major strengths.
These data regarding lower genital tract immunological susceptibility to subsequent sPTB deserve ongoing study. Investigation of the maternal genetic and environmental contributors to lower genital tract immunological milieu may inform not only an understanding of the mechanisms of disease but also suggest interventions to modify susceptibility to preterm birth.
Table 1.
Rotated factor loadings a using principal factor analysis of a Spearman correlation matrix for cervical cytokine concentrations at <16 weeks gestation (n=613).
| Cytokine | Factor 1: proinflammatory / immunomodulatory | Factor 2: anti-inflammatory |
|---|---|---|
| Loading | Loading | |
| IL-6 | 0.76 | -- |
| MCP-1 | 0.75 | -- |
| IL-8 | 0.69 | -- |
| IL-1β | 0.59 | -- |
| IL-10 | 0.36 | 0.58 |
| IL-13 | -- | 0.78 |
| IL-4 | -- | 0.79 |
| Eigenvalue b | 2.5 | 1.3 |
IL, interleukin; MCP, monocyte chemotactic protein
Factor loadings are correlations between the each cytokine and the overall factor. Factor loadings are reported if their absolute value is ≥0.20.
Eigenvalues are the variances extracted by the factors.
Acknowledgments
This study was supported by NIH grants R01HD041663 and R01HD052732 to Dr. Simhan.
References
- 1.Behrman RE, Stith Butler A, editors. Preterm Birth: Causes, Consequences, and Prevention. Washington, D.C: The National Academies Press; 2007. [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hillier SL, Martius J, Krohn M, Kiviat N, Holmes KK, Eschenbach DA. A case-control study of chorioamnionic infection and histologic chorioamnionitis in prematurity. New England Journal of Medicine. 1988;319:972–978. doi: 10.1056/NEJM198810133191503. [DOI] [PubMed] [Google Scholar]
- 4.Simhan HN, Krohn MA. First-trimester cervical inflammatory milieu and subsequent early preterm birth. American Journal of Obstetrics and Gynecology. 2009;200:377 e371–374. doi: 10.1016/j.ajog.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 5.Simhan HN, Bodnar LM, Krohn MA. Paternal race and bacterial vaginosis during the first trimester of pregnancy. American Journal of Obstetrics and Gynecology. 2008;198(196):e191–194. doi: 10.1016/j.ajog.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. Journal of Clinical Microbiology. 1991;29:297–301. doi: 10.1128/jcm.29.2.297-301.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Comrey AL, Lee HB. A first course in factor analysis. 2. Hillsdale, NJ: Erlbaum Associates; 1992. [Google Scholar]
- 8.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Allyn and Bacon; 2007. [Google Scholar]
- 9.Grice JW. A comparison of factor scores under conditions of factor obliquity. Psychology Methods. 2001;6:67–83. doi: 10.1037/1082-989x.6.1.67. [DOI] [PubMed] [Google Scholar]
- 10.Cassatella MA, Meda L, Bonora S, Ceska M, Constantin G. Interleukin 10 (IL-10) inhibits the release of proinflammatory cytokines from human polymorphonuclear leukocytes. Evidence for an autocrine role of tumor necrosis factor and IL-1 beta in mediating the production of IL-8 triggered by lipopolysaccharide. Journal of Experimental Medicine. 1993;178:2207–2211. doi: 10.1084/jem.178.6.2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodwin VJ, Sato TA, Mitchell MD, Keelan JA. Anti-inflammatory effects of interleukin-4, interleukin-10, and transforming growth factor-beta on human placental cells in vitro. American Journal of Reproductive Immunology (Copenhagen) 1998;40:319–325. doi: 10.1111/j.1600-0897.1998.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 12.Moore KW, O'Garra A, de Waal Malefyt R, Vieira P, Mosmann TR. Interleukin-10. Annual Review of Immunology. 1993;11:165–190. doi: 10.1146/annurev.iy.11.040193.001121. [DOI] [PubMed] [Google Scholar]
- 13.Simhan HN, Krohn MA, Zeevi A, Daftary A, Harger G, Caritis SN. Tumor necrosis factor-alpha promoter gene polymorphism -308 and chorioamnionitis. Obstetrics & Gynecology. 2003;102:162–166. doi: 10.1016/s0029-7844(03)00406-x. [DOI] [PubMed] [Google Scholar]
- 14.Genc MR, Witkin SS, Delaney ML, Paraskevas LR, Tuomala RE, Norwitz ER, et al. A disproportionate increase in IL-1beta over IL-1ra in the cervicovaginal secretions of pregnant women with altered vaginal microflora correlates with preterm birth. American Journal of Obstetrics and Gynecology. 2004;190:1191–1197. doi: 10.1016/j.ajog.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Cole SR, Chu H, Nie L, Schisterman EF. Estimating the odds ratio when exposure has a limit of detection. International Journal of Epidemiology. 2009;38:1674–1680. doi: 10.1093/ije/dyp269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson DB, Ciampi A. Effects of exposure measurement error when an exposure variable is constrained by a lower limit. American Journal of Epidemiology. 2003;157:355–363. doi: 10.1093/aje/kwf217. [DOI] [PubMed] [Google Scholar]