Abstract
Background
In an aging society, it is increasingly important to understand how assistive devices can be used by older people to maintain quality of life despite chronic disabilities. Assistive technology is a mainstay of physical therapist practice, but the potential for device use to affect psychosocial well-being is not yet understood at the population level.
Objective
The objective of this study was to develop a parsimonious indicator that can be used in population-based surveys to represent the effect of assistive technologies on quality of life for older people, separate from personal assistance.
Design
This study was a cross-sectional survey.
Methods
The methods used in this study were psychometric scale development and structural equation modeling.
Results
The results indicated that a parsimonious, valid, and reliable scale reflecting quality of life related to assistive device use can be created from 3 questions designed to measure improvements in safety, control, and participation due to technology. The findings also suggested that assistive technology may more effectively improve quality of life for people with greater levels of functional limitations.
Limitations
The data were derived from a cross-sectional survey conducted by telephone. The use of personal assistance, on average, was low; thus, the applicability to a population with more profound care needs has yet to be confirmed.
Conclusions
Determining the broader impact of assistive technology on quality of life with population-level measures may provide insight into how best to leverage technologies to prevent dependence in aging adults.
Assistive technology facilitates myriad treatment goals for physical therapist practice. Users of assistive technology experience delays in functional decline and report greater reductions in difficulty than people relying only on personal assistance.1–3 Studies also have suggested that assistive device use may confer psychological benefits by enhancing the ability of adults to make choices about when and how they carry out activities and the extent to which they participate in daily activities.4,5 At the same time, there has been an increase in the types of technologies and supportive living environments available to help people with disabilities to live independently and participate in daily activities.6,7
These studies illustrate the great potential of assistive technology to improve the functioning and well-being of a broad range of users. Understanding the potential impact of improved access to assistive technology and determining which groups of people may benefit most from the use of assistive technology require the development of population-level measures. However, indicators that link device use to psychosocial well-being in this context have not been developed. Such indicators will be useful in developing an evidence base that informs policies regarding assistive technology access and provision.
The Consortium for Assistive Technology Outcomes Research has proposed a taxonomy of outcome measures for assistive technology to further the development of improved and better-targeted indicators of the impact of assistive technology.8 Moreover, this consortium has identified the development and study of survey-based measures of assistive technology outcomes as an important step in the evaluation of its taxonomy and the addition of new concepts.9 The consortium has proposed distinguishing the proximal and distal effects of assistive technology on physical functioning (effectiveness), on other people and society (social significance), and on quality of life (perceived well-being).
The term “quality of life” is an umbrella expression that refers to well-being across multiple domains of life.10 No consensus exists on how quality of life should be defined, especially as an outcome of rehabilitation, although domains of mastery, independence, ease/safety/comfort, and participation in valued activities commonly are cited as user priorities in studies of device use.11,12 Quality-of-life measures can be objective measures of goal attainment or subjective perceptions of users. Rehabilitation researchers who examine the use of assistive technology have long emphasized the importance of the user's subjective perspective in defining success with assistive devices.13–15
Several clinical instruments have been developed to evaluate the subjective benefits of the use of assistive technology for quality of life. The best-known instruments are the Psychosocial Impact of Assistive Devices Scale,16 the Quebec User Evaluation of Satisfaction with Assistive Technology,17 and the Assistive Technology Device Predisposition Assessment,18 all of which have been adopted broadly and validated across different devices.19,20 In addition, several device-specific measures have been developed, particularly in the area of mobility, such as those for wheelchair users.21,22
Existing clinical instruments are not easily translated to population-level (survey-based) measures because they are intended for use in clinical settings by trained providers and are often lengthy. In addition, because of their focus on person-technology fit, they are intentionally designed to assess the impact of individual devices; this design may be less useful for assessing the overall effects of assistive technology for older people, who frequently use multiple devices to meet their needs.23
Addressing the impact of assistive technology at the population level requires the development and testing of a parsimonious instrument that encompasses multiple quality-of-life dimensions and that can distinguish the impact of assistive technology from the impacts of other types of accommodations. An ideal measure also will accommodate the use of multiple devices to assist with diverse tasks across environments—the real-life conditions of device use.
In the present article, we describe the development and testing of a brief quality-of-life scale for assistive technology use that can be applied in a large-scale survey setting. In developing the Assistive Technology Quality-of-Life (ATQoL) Scale, we tested several subjective domains that link assistive technology use to independence, safety, control, participation in daily activities, pain, fatigue, and time needed to carry out activities. We hypothesized that underlying functional limitations are strongly related to both the amount of assistive technology use and the amount of personal assistance with activities of daily living (ADL) but that the ATQoL Scale represents the effect of assistive technology—separate from the effect of personal assistance—on quality of life for adults.
Method
Survey Data and Sampling
Data for this analysis came from the Pilot Study of Aging and Technology (PSAT), a study of a nationally drawn sample of Americans who were 50 years old or older and were living in the community (N=360). The purpose of the PSAT was to develop, pilot test, and disseminate a set of instruments with which national health and aging surveys can measure the use of assistive devices and the environments in which they are used. Questions from the PSAT have been used in the US Health and Retirement Survey and the forthcoming National Health and Aging Trends Study. The development of the PSAT involved an extensive review of existing measurement approaches, consultations with technical experts and stakeholders in policy and national surveys, cognitive interviews, and behavioral coding of interviews.24 Particular attention was paid to creating brief items that could be administered in a computer-assisted telephone interview.
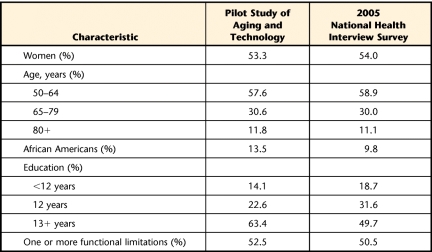
Westat, a social science research firm in Rockville, Maryland, conducted the pilot testing. Using a computer-assisted telephone instrument, trained interviewers completed 360 interviews with a racially diverse sample of adults who were 50 years of age or older and were living in the community. In the sample, which was drawn from a national marketing list, people in older age groups were oversampled so that comparisons could be made by age: 50 to 64 years (n=124), 65 to 79 years (n=124), and 80 years or older (n=112). People who were 50 to 64 years of age and were living in households with an individual reporting a disability were also oversampled (n=78), again to facilitate comparisons. The sample included people living in assisted living facilities (n=21), African Americans (n=50), and people living in rural areas (n=81). No follow-up was attempted for those who refused to participate in the study. The response rate (completed interviews/eligible candidates) was 20%, and the cooperation rate [completed interviews/(completed interviews + refusals)] was 39%. The interview length varied from 10 minutes to 1 hour; the average interview lasted 22 minutes. For the present analysis, we restricted our sample to people who reported using one or more assistive devices in the preceding 30 days (n=350). Weights were developed so that the distributions of demographic characteristics in our sample mimicked those in the National Health Interview Survey. Table 1 shows a comparison of the participants in the PSAT and the National Health Interview Survey.
Table 1.
Comparison of Participants in the Pilot Study of Aging and Technology and the 2005 National Health Interview Survey
ATQoL Scale Item Development
On the basis of the literature reporting motivators of device use and success15,25 and existing items in surveys such as the National Health Interview Survey 1994/1995 Supplement on Disability,26 we developed several items that directly assessed the link between the use of assistive technology and its impact on quality of life. Items were first evaluated at the Questionnaire Design Research Laboratory at the National Center for Health Statistics. Interviews with 28 volunteers were conducted in 3 rounds. Participants were recruited through newspaper advertisements, flyers, and word of mouth. They ranged in age from 28 to 86 years (X̅=62 years) and included both sexes and various ethnic backgrounds. All interviews were recorded. After each round of interviewing, the project team reviewed the tapes, and the Questionnaire Design Research Laboratory provided feedback regarding the performance of the questions. On the basis of this feedback, the instrument was revised for the next round of interviewing.
For the final PSAT instrument, words whose meanings were unclear or difficult to understand were eliminated from the questions, and a list of simple definitions was crafted for the questionnaire. Many of the quality-of-life concepts used in our sequence of questions (safety, independence, and participation) were explicitly mentioned by participants in a series of open-ended questions about the importance of technology in their lives. During this process, the quality-of-life questions were revised from bipolar response scales that were intended to allow respondents to evaluate assistive technology as improving or worsening their lives to unipolar scales with positive valance. The former resulted in answers that could not be coded (ie, respondents giving answers that were not in the list of possible answer categories); the adoption of unipolar scales with fewer categories remedied this problem.27
The final 7 quality-of-life questions included in the PSAT were tailored to the particular set of devices that the respondent reported using earlier in the survey. For the set of items that the respondent mentioned using, the following questions were asked:
Because you use these items, how much safer do you feel when you do your daily activities?
Because you use these items, how much more control do you have over your daily activities?
Because you use these items, how much more often do you take part in activities you enjoy?
The response categories offered for these 3 questions were: “Would you say no more, a little more, a lot more, or does that not apply to you?”
Because you use these items, how much less painful is it for you to do your daily activities?
Because you use these items, how much less tiring is it for you to do your daily activities?
Because you use these items, how much less do you rely on others in your daily activities?
Because you use these items, how much less time does it take for you to do your daily activities?
The response categories offered for these 4 questions were: “Would you say no less, a little less, a lot less, or does that not apply to you?”
Covariates
Use of assistive technology.
Although most national data on assistive technology use have been limited to measures of use versus nonuse, the PSAT allowed us to estimate the frequency of device use in the preceding 7 days, an important indicator of the successful use of assistive devices. The intensity of assistive technology use was calculated by summing across all devices used according to the following algorithm: every time=4, most times=3, sometimes=2, rarely=1, and never=0.
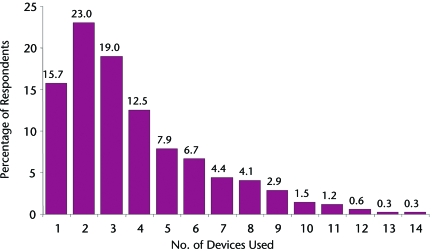
Devices included 5 bathroom features (grab bar, shower seat, grab bar around toilet, modified toilet seat, and portable commode), 6 mobility devices (cane, walker, wheelchair, scooter, crutches, and motor cart at store), 7 environmental features (ramp, elevator, stair lift, railings, raising seat, trapeze, and emergency call system), and 6 other types of assistive technology (hearing aid, vision aids other than glasses, reacher, special bed, modified clothes washer, and modified cookware). The most commonly used devices were mobility devices (∼20%) and sensory aids (12%). A total of 84.3% of respondents had used more than 1 device or feature in the preceding 30 days (Fig. 1). The maximum number used was 14 items, and the average number used was 3.8 items.
Figure 1.
Percentage distribution of the number of devices used by respondents who reported using at least 1 type of assistive technology.
Personal assistance.
To assess whether responses to the quality-of-life measures could be attributed to assistive technology use alone, we included a measure of the amount of personal assistance received. About 17% of the respondents used personal assistance in addition to devices. Like our measure of the intensity of assistive technology use, this scale reflected not only receipt of personal assistance but also how often that assistance was used. The variable was coded by summing the frequency of assistance received across 5 ADL tasks (transferring, inside mobility, leaving one's home or building, bathing, and toileting), where every time=4, most times=3, sometimes=2, rarely=1, and never=0. Personal assistance was most commonly used for transferring (10%) and leaving one's home or building (13%). Assistance was reported less often for inside mobility (6%), bathing (5%), and toileting (1%). Most people who reported the use of personal assistance with transferring, inside mobility, and toileting used help rarely or sometimes (81%, 67%, and 100%, respectively), whereas most people who used personal assistance for getting outside or bathing reported using help most of the time or every time they conducted the activity (62% and 76%, respectively). The mean value of the personal assistance scale was 0.9, and 4.9 among those who used any personal assistance.
Functional limitations.
A functional limitation score was calculated by summing the level of difficulty reported across 8 Nagi indicators, including 3 upper-body measures (reaching up, reaching out, and grasping) and 5 lower-body measures (standing, crouching, walking up 10 steps, getting up from sitting, and walking a quarter of a block). A total of 81% of respondents reported difficulty with one or more of these activities. For construction of the scale, each question was coded for the level of difficulty reported (0=none, 1=a little, 2=some, 3=a lot, and 4=unable), and scores were summed across the 8 activities. The scores ranged from 0 to 32, with a mean of 9.1, indicating mild to moderate levels of functional limitations, on average.
Analytic Methods
We first examined the frequencies for each of the quality-of-life items. Those found to have substantial numbers of “does not apply” responses were omitted from the scale construction. We treated the remaining quality-of-life items as a latent (unmeasured) variable and used structural equation modeling with SPSS AMOS software (SPSS Inc, Chicago, Illinois) to construct a scale reflecting quality-of-life outcomes and to check the congruence of the scale with other relevant constructs.
In addition, we included measures of the amount of assistive technology use, the amount of personal assistance with ADL, and functional limitations. We conservatively assumed in the structural equation model that all variables were not measured perfectly. We assessed the overall goodness of fit of the model using 3 statistics: the normed fit index and the comparative fit index, both of which are generally required to be greater than or equal to .90, and the root mean square error of approximation, which is generally required to be greater than or equal to .05. We assessed the statistical significance of both the direct and the indirect relationships by examining the significance of the standardized regression coefficient of each path. This approach allowed us to assess, within a single framework, the reliability of the ATQoL Scale and the strength of the relationships among the ATQoL Scale, use of assistive technology, underlying functioning, and use of personal assistance.
Role of the Funding Source
This research was supported by the Department of Health and Human Service's Office of the Assistant Secretary of Planning and Evaluation and by the US National Institute of Aging (R01-AG14346). Preparation of the final manuscript was supported, in part, by the Hopkins Center for Population Aging and Health (P30-AG034460).
Results
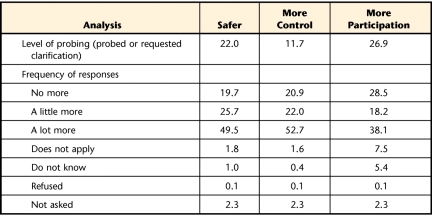
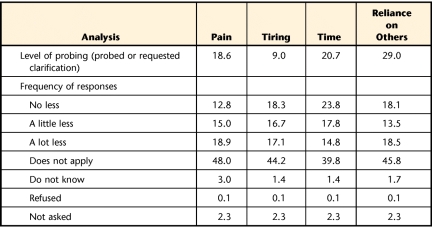
The evaluation of individual questions being considered for inclusion in the ATQoL Scale revealed similar levels of requests (9%–29%) for clarification across the items (Tabs. 2 and 3). These levels were not problematic as long as there were reasonable frequencies of responses in the final data. In this respect, questions about whether activities were less painful, tiring, or time-consuming and whether respondents were less reliant on others showed high levels of inadequate responses, being answered with “does not apply” about 40% to 48% of the time. Of the remaining 3 questions, those concerning safety and control elicited “does not apply” responses in fewer than 2% of cases, and that concerning participation did so 7.5% of the time. These 3 questions were retained for further analysis.
Table 2.
Level of Probing and Frequency of Responses to Quality-of-Life Questions With a Positive Orientationa
Data are reported as percentages.
Table 3.
Level of Probing and Frequencies of Responses to Quality-of-Life Questions With a Negative Orientationa
Data are reported as percentages.
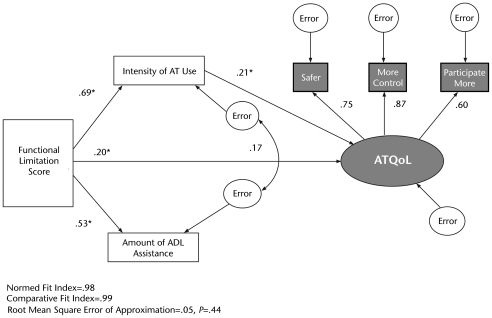
Figure 2 shows the final, best-fitting structural equation model for the ATQoL scale. This figure illustrates the relationship of the scale to the key constructs of functional limitations, intensity of assistive technology use, and amount of ADL help. Overall goodness-of-fit measures suggested that this model fit well (normed fit index=.98, comparative fit index=.99, and root mean square error of approximation=.05).
Figure 2.
Structural equation model for the Assistive Technology Quality-of-Life (ATQoL) Scale, functional limitations, intensity of assistive technology (AT) use, and amount of personal assistance with activities of daily living (ADL). Asterisks indicate values that were significant at P<.001.
The shaded oval on the right side of Figure 2 represents the latent variable (ATQoL Scale) formed from the 3 individual indicators that were retained from the survey (safer, more control, and participate more) and that are shown as shaded rectangles above the latent variable. The white ovals indicate error components for either the measured variables or the latent variable. The 3 items with a positive orientation scaled well, with factor loadings for variables indicating safety, control, and participation of .75, .87, and .60, respectively. These factor weights were all sufficient to establish the ATQoL Scale as a meaningful latent variable. The reliability of the latent variable was quite high, at .94 (data not shown).
The correlations shown on the left side of Figure 2 confirmed the anticipated relationships among the indicators for functional limitations, intensity of assistive technology use, and amount of personal assistance with ADL. Higher functional limitation scores were strongly and positively associated with both intensity of assistive technology use and amount of personal assistance with ADL. The standardized partial correlation between functional limitations and intensity of assistive technology use was high (.69) and significant, as was the standardized partial correlation between functional limitations and amount of personal assistance with ADL (.53). Consistent with previous studies of the joint use of personal assistance and assistive technology,28 the residual correlation between intensity of assistive technology use and amount of personal assistance was positive (.17).
Finally, there were significant relationships between the ATQoL Scale and these 3 variables. More intense use of assistive technology had a significant partial correlation with the ATQoL Scale of .21, indicating that the scale did measure the impact of assistive technology on quality of life. The functional limitation score was also significantly correlated with the ATQoL Scale (.20). This finding implied that assistive technology was more likely to improve the quality of life at greater levels of functional limitations. However, the amount of personal assistance with ADL had no significant correlation with the ATQoL Scale, indicating that the ATQoL Scale reflected the impact of the use of assistive technology without being confounded by the use of personal assistance. This conclusion was confirmed by an alternate specification that included a direct path between the amount of personal assistance and the ATQoL Scale; that coefficient was not statistically significant and therefore was not included in the final model.
Discussion
The relationships observed in the present study suggested that a brief ATQoL Scale that distinguishes the quality-of-life impact of assistive technology from that of personal assistance can be constructed. Our analysis suggested that a valid and reliable scale reflecting the quality-of-life impact of technology can be created from 3 questions designed to measure the role of assistive technology in increasing safety, control over daily activities, and participation in enjoyable activities. The items scaled well and were positively related to both intensity of assistive technology use and extent of underlying functional limitations. These measures appeared to perform substantially better than questions about the role of assistive technology in reducing pain, the extent to which activities were tiring, the amount of time needed to carry out activities, and reliance on other people.
One important limitation worth noting is that only 17% of people in the PSAT sample reported receiving personal assistance. It is possible that for people with more profound care needs (eg, those for whom personal assistance and devices are used together or even by a caregiver to provide assistance), the ATQoL Scale may be less successful in discriminating the benefits of assistive technology from those of personal assistance. Further research with this tool and such a sample would be beneficial.
An additional potential limitation is that the unipolar scales incorporated into the ATQoL Scale, although easier to understand than their bipolar counterparts, may have led respondents to provide more positive reports of the influence of assistive technology. This situation would be especially likely if there were a social desirability bias compounded by an interviewer's presence. Future research should explore whether substantially different findings would be obtained with an introductory neutrally worded question (eg, “Because you use [previously mentioned items], do you feel safer?”) and a follow-up question (eg, “How much safer?”) for people who responded positively and whether self-administered modes (eg, paper or Web-based) would yield different findings.
Despite these limitations, our analysis suggested that assistive technology outcome measures can be integrated into large-scale surveys and validated at the population level, allowing for larger-scale studies that will contribute to a deeper understanding of the benefits of assistive technology for independent living and aging in place, which are critical policy goals. Although clinical measures of assistive technology outcomes can explore user satisfaction and the impact of assistive technology in more depth, population-based indicators of the influence of assistive technology on quality of life meet a different need. They allow the identification of the groups of people who may benefit most from the use of assistive technology, the examination of longitudinal outcomes related to the effects of assistive technology on quality of life, and a better understanding of the tradeoffs—in terms of function and satisfaction—of the use of assistive technology versus the use of personal assistance.
Conclusions
Assistive technology is a mainstay of physical therapist practice. The use of devices to assist with daily activities is an essential component of successful interventions, particularly for older people, who respond more slowly to exercise and for whom independent functioning may mean the difference between living at home and living in a long-term–care facility. As practitioners, physical therapists believe that the effectiveness of assistive technology extends beyond the reduction of difficulties with activities and dependence to include a broader psychosocial impact on perceived quality of life. However, determining this impact and the groups of people for whom assistive technology can have the greatest impact requires population-level measures. An understanding of the extent to which assistive technology can provide unique benefits may provide insight into how best to leverage technologies to prevent dependence in aging adults.
This article has provided evidence that the impact of the use of assistive technology can be measured independently from that of the use of personal assistance in population-based surveys. Our findings also suggested that assistive technology may more effectively improve safety, control, and participation for people with greater levels of functional limitations. Capturing the unique benefits of independent functioning with assistive technology has important implications for the development of policies to improve quality of life in an aging society.
The revised agenda for research of the American Physical Therapy Association includes several items that prioritize the measurement of physical therapy effectiveness and impact.29 Specifically, the association lists several items under “Measurement Development and Validation” that are directly addressed by the research in the present study—item 1 (develop or adapt measures of effectiveness and impact of physical therapy at the community level), item 2 (develop new tools or refine existing tools to measure the impact of physical therapy on activity, participation, and quality of life), and item 7 (determine optimal measurement methods to enhance clinical decision making for specific conditions and populations). Evidence to inform all of these priorities can be developed with population-level research using the ATQoL Scale jointly with information from surveys about demographic and economic characteristics, health conditions, cognition, and home environment.
Footnotes
Both authors provided concept/idea/research design, writing, and data analysis. Dr Agree provided data collection and consultation (including review of manuscript before submission). Dr Freedman provided project management and fund procurement. The authors thank Morton Kleban for assistance in estimating the structural equation models.
This research was supported by the Department of Health and Human Service's Office of the Assistant Secretary of Planning and Evaluation and by the US National Institute of Aging (R01-AG14346). Preparation of the final manuscript was supported, in part, by the Hopkins Center for Population Aging and Health (P30-AG034460).
References
- 1. Gitlin LN, Winter L, Dennis MP, et al. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816 [DOI] [PubMed] [Google Scholar]
- 2. Mann WC, Ottenbacher KJ, Fraas L, et al. Effectiveness of assistive technology and environmental interventions in maintaining independence and reducing home care costs for the frail elderly: a randomized controlled trial. Arch Fam Med. 1999;8:210–217 [DOI] [PubMed] [Google Scholar]
- 3. Agree EM. The influence of personal care and assistive devices on the measurement of disability. Soc Sci Med. 1999;48:427–443 [DOI] [PubMed] [Google Scholar]
- 4. Pape TLB, Kim J, Weiner B. The shaping of individual meanings assigned to assistive technology: a review of personal factors. Disabil Rehabil. 2002;24:5–20 [DOI] [PubMed] [Google Scholar]
- 5. Cornman JC, Freedman VA, Agree EM. Measurement of assistive device use: implications for estimates of device use and disability in late life. Gerontologist. 2005;45:347–358 [DOI] [PubMed] [Google Scholar]
- 6. Spillman B. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Mem Fund Q. 2004;82:157–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Freedman VA, Agree EM, Martin LG, Cornman JC. Trends in the use of assistive technology and personal care for late-life disability, 1992–2001. Gerontologist. 2006;46:124–127 [DOI] [PubMed] [Google Scholar]
- 8. Fuhrer MJ, Jutai JW, Scherer MJ, Deruyter F. A framework for the conceptual modelling of assistive technology device outcomes. Disabil Rehabil. 2003;25:1243–1251 [DOI] [PubMed] [Google Scholar]
- 9. Jutai JW, Fuhrer MJ, Demers L, et al. Toward a taxonomy of assistive technology device outcomes. Am J Phys Med Rehabil. 2005;84:294–302 [DOI] [PubMed] [Google Scholar]
- 10. Andresen EM, Meyers AR. Health-related quality of life outcomes measures. Arch Phys Med Rehabil. 2000;81(suppl 2):S30–S45 [DOI] [PubMed] [Google Scholar]
- 11. Gitlin LN. Assistive technology in the home and community for older people: psychological and social considerations. In: Scherer MJ, ed. Assistive Technology: Matching Device and Consumer for Successful Rehabilitation. Washington, DC: American Psychological Association; 2002:109–122 [Google Scholar]
- 12. Pain K, Dunn M, Anderson G, et al. Quality of life: what does it mean in rehabilitation? J Rehabil. 1998;64:5–11 [Google Scholar]
- 13. Brooks NA. Users' responses to assistive devices for physical disability. Soc Sci Med. 1991;32:1417–1424 [DOI] [PubMed] [Google Scholar]
- 14. Scherer MJ. Outcomes of assistive technology use on quality of life. Disabil Rehabil. 1996;18:439–448 [DOI] [PubMed] [Google Scholar]
- 15. Heaton J, Bamford C. Assessing the outcomes of equipment and adaptations: issues and savings. Br J Occup Ther. 2001;64:346–356 [Google Scholar]
- 16. Jutai J. Quality of life impact of assistive technology. Rehabil Eng. 1999;14:2–7 [Google Scholar]
- 17. Demers L, Weiss-Lambrou R, Ska B. Development of the Quebec User Evaluation of Satisfaction With Assistive Technology (QUEST). Assist Technol. 1996;8:3–13 [DOI] [PubMed] [Google Scholar]
- 18. Scherer MJ, Cushman LA. Measuring subjective quality of life following spinal cord injury: a validation study of the Assistive Technology Device Predisposition Assessment. Disabil Rehabil. 2001;23:387–393 [DOI] [PubMed] [Google Scholar]
- 19. Brandt A. Translation, cross-cultural adaptation, and content validation of the QUEST. Technol Disabil. 2006;17:205–216 [Google Scholar]
- 20. Scherer M, Glueckauf R. Validating a measure of predisposition to and outcomes of assistive technology use. Rehabil Psychol. 2005;50:132–141 [Google Scholar]
- 21. Auger C, Demers L, Gelinas I. Reliability and validity of the telephone administration of the Wheelchair Outcome Measure (WhOM) for middle-aged and older users of power mobility devices. J Rehabil Med. 2010;42:574–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brandt A, Kreiner S, Iwarsson S. Mobility-related participation and user satisfaction: construct validity in the context of powered wheelchair use. Disabil Rehabil Assist Technol. 2010;5:305–313 [DOI] [PubMed] [Google Scholar]
- 23. Tomita MR, Mann WC, Fraas LF, Stanton KM. Predictors of the use of assistive devices that address physical impairments among community-based frail elders. J Appl Gerontol. 2004;23:141–155 [Google Scholar]
- 24. Freedman VA, Agree EM, Cornman JC. Development of an Assistive Technology and Home Environment Assessment Instrument for National Surveys: Final Report, Part I: Recommended Modules and Instrument Development Process. Washington, DC: US Department of Health and Human Service's Office of the Assistant Secretary for Planning and Evaluation; 2005 [Google Scholar]
- 25. Samuelsson K, Wressle E. User satisfaction with mobility assistive devices: an important element in the rehabilitation process. Disabil Rehabil. 2008;30:551–558 [DOI] [PubMed] [Google Scholar]
- 26. Agree EM, Freedman VA. A comparison of assistive technology and personal care in alleviating disability and unmet need. Gerontologist. 2003;43:335–344 [DOI] [PubMed] [Google Scholar]
- 27. Wilson B, Altman BE, Whitaker KR, et al. Improving person-item fit: cognitive testing questions about assistive technology and the home environment with older adults. Paper presented at: Annual Meeting of the American Association for Public Opinion Research; May 15, 2004; Phoenix, AZ [Google Scholar]
- 28. Agree EM, Freedman VA, Cornman JC, et al. Reconsidering substitution in long-term care: when does assistive technology take the place of personal care? J Gerontol B Psychol Sci Soc Sci. 2005;60:S272–S280 [DOI] [PubMed] [Google Scholar]
- 29. Goldstein MS, Scalzitti DA, Craik RL, et al. The Revised Research Agenda for Physical Therapy. Phys Ther. 2011;91:165–174 [DOI] [PMC free article] [PubMed] [Google Scholar]