Abstract
Background
The majority of interventions for knee osteoarthritis aim to reduce knee pain with the assumption that improvements in function will automatically follow. However, this assumption is not universally true, and a paradoxical decline in function is not uncommon following reduction in knee pain.
Objective
The purpose of this study was to examine what factors beyond knee pain are important for functional decline among people with reductions in knee pain.
Design
This was an observational cohort study.
Methods
The Multicenter Osteoarthritis Study (MOST) is a National Institutes of Health–funded longitudinal study of people who have or are at high risk for knee osteoarthritis. This study included individuals who had a meaningful reduction in pain in either knee over 30 months, defined as a 41% decrease in visual analog scale pain score with an absolute decrease of ≥20/100. Meaningful decline in walking speed was defined as a decrease of 0.1 m/s during a 20-m walk. To examine the association of risk factors with meaningful decline in walking speed, risk ratios were calculated and adjusted for potential confounders.
Results
Of the 465 people with a meaningful reduction in knee pain (mean [SD] age=63.3 [7.8] years, 67% female, 82% Caucasian, mean [SD] body mass index=31.3 [6.3] kg/m2), 20% had a meaningful decline in walking speed. Adjusting for confounders, participants with new comorbidity and those with widespread pain had 1.8 and 1.7 times the risk of decline compared with their counterparts with no comorbidity or widespread pain (adjusted risk ratio=1.8 [95% confidence interval=1.1–3.0] and 1.7 [95% confidence interval=1.1–2.8], respectively).
Limitations
Generalizability is limited to people with a reduction in knee pain.
Conclusions
Reductions in knee pain are not always accompanied by improvements in walking speed. Health providers should consider that the onset of new comorbidity and presence of widespread pain may increase the risk of functional decline despite a reduction in knee pain.
An estimated 7 million individuals, or 2.8% of the US population, have functional limitations attributable to arthritis, and this number is expected to increase to 11.6 million, or 3.6% of the US population, by the year 2020.1 Furthermore, knee osteoarthritis (OA) is the most common type of arthritis and the leading cause of functional limitation compared with any other chronic disease in older adults.2,3 Knee OA, therefore, represents a tremendous public health burden.
Despite the substantial functional limitation attributed to knee OA, the vast majority of interventions for OA aim at reducing knee pain rather than functional limitation, such as through the use of pharmacological and nonpharmacological modalities.4,5 This approach highlights an underlying assumption that efforts aimed at reducing knee pain will likely lead to improvements in functional limitation. Although this assumption is well supported by the fact that knee pain is strongly associated with functional limitation6,7 and that many pain-oriented interventions frequently show concordant improvements in function,4 recent studies suggest that it may not always be true. For instance, following total knee replacement, which typically is performed to relieve knee pain, residual impairments and lower-extremity functional limitations, such as quadriceps muscle weakness and slow walking speeds, are not uncommon 3 to 12 months following surgery.8 Jinks and colleagues9 reported that community-dwelling adults had only slight improvements in physical functioning following resolution of knee pain, with average follow-up scores being notably lower than in a comparison group with no knee pain followed over the same period.
Although the assumption that improvements in function will follow knee pain reduction may not be universally true, it is not clear why this may occur. Clinically, it is not uncommon for patients who report reductions in knee pain to have a seemingly paradoxical decline in function. Formally investigating this seemingly paradoxical relationship would provide insight into what factors beyond knee pain are important for function. Although previous studies have identified radiographic disease,10 comorbidity,11 knee extensor strength,12 proprioceptive acuity,12 and widespread pain13,14 as risk factors for functional decline in people with knee OA, it is not known whether these factors also may be why functional decline occurs among those who have had a reduction in knee pain. Identification of risk factors for functional decline among people with a reduction in knee pain would be helpful for clinicians in identifying patients at risk of a decline in function despite reduction in knee pain and specifically for physical therapists to target those risk factors that are modifiable for intervention. For clinical researchers, such an investigation would highlight important factors to be considered within the context of studies that investigate changes in function.
Thus, we examined risk factors for a decline in function as measured by walking speed among people with or at high risk of symptomatic knee OA who had a reduction in pain in one or both knees. We chose to measure function using walking speed, given that it is an important marker of overall health and disability in older adults.15,16
Method
Study Sample
The study sample consisted of participants from the Multicenter Osteoarthritis Study (MOST), a multicenter longitudinal cohort study of 3,026 community-dwelling adults who had or who at baseline were at high risk of developing symptomatic knee OA. A more-detailed description of recruitment and sampling for MOST has been published elsewhere.17 In brief, individuals aged 50 to 79 years were recruited from the communities in and surrounding Birmingham, Alabama, and Iowa City, Iowa. Participants were defined as being at risk of developing knee OA based on known risk factors, including older age, female sex, previous knee injury or surgery, and high body weight. At baseline only, participants had to walk without the assistance of another person. The baseline assessment took place between May 2003 and March 2005, and a follow-up assessment was conducted 30 months later.
For the current study, we limited our sample to those individuals with a meaningful reduction in pain in one or both knees from the baseline visit to the 30-month follow-up visit. We did not include people with reduction in pain in one knee but worsening of pain in the other knee. We measured knee pain using a visual analog scale (VAS), quantified as the average knee pain over the previous 30 days as measured on a horizontal line, with 0 and 100 as endpoints at both the baseline and 30-month study visits. We defined a meaningful reduction in pain according to a previously published method (ie, a 41% decrease in VAS pain score with an absolute decrease of at least 20/100).18
Outcome: Meaningful Decline in Physical Function
We used walking speed to define our outcome of meaningful decline in physical function. Walking speed has high test-retest reliability in people with knee OA19 and older adults.20 At both the baseline and 30-month study visits, participants' walking speed was calculated from the average of two 20-m walks at a usual pace. Our primary outcome was a meaningful decline in walking speed, defined as a decrease of ≥0.1 m/s from baseline to 30 months. This cutpoint is consistent with those of previously published studies of older adults21,22 and people after hip fracture.23 Participants who were able to complete the 20-m walk at baseline but not at the 30-month study visit were classified as having a meaningful decline in function.
Risk Factors
Radiographic knee osteoarthritis (ROA).
All participants underwent bilateral weight-bearing posteroanterior (PA) and lateral fixed-flexion radiographic evaluations of the knee at baseline and 30 months, as described elsewhere.17 Two experienced readers blinded to clinical data graded joint space narrowing and osteophytes using the OARSI atlas24 in both tibiofemoral (TF) and patellofemoral (PF) joints (both graded 0–3). Radiographic severity in the TF joint was graded according to Kellgren and Lawrence (KL) criteria (0–4).25 Any disagreements between readers were adjudicated by a third reader along with the first 2 readers to reach consensus. We defined ROA based on radiographic findings in either the TF or PF joint. For the TF joint, ROA was defined as a KL grade of ≥2, and for the PF joint, it was defined as an osteophyte score ≥2 or any joint space narrowing score of ≥2 with any osteophyte, sclerosis, or cyst score of ≥1 on a lateral plain-view film.25,26 The interrater reliability weighted kappa for the KL grade was .80.
A participant's ROA status was categorized into 1 of 3 groups: no ROA, incident ROA, and prevalent ROA. We defined no ROA as absence of any ROA at baseline and at 30 months. We defined incident ROA as absence of ROA at baseline and meeting the ROA criteria at 30 months. We defined prevalent ROA as ROA at baseline and at 30 months. Radiographic disease status was not classified in knees with a total knee replacement. We classified participants according to the knee that had incident disease. For instance, if a participant had no ROA in one knee and incident ROA in the other knee, he or she was classified as having incident ROA. Similarly, if a participant had prevalent ROA in one knee and incident ROA in the other knee, he or she was classified as having incident ROA. If a participant had no disease in one knee and prevalent ROA in the other knee, he or she was classified as having prevalent ROA.
Comorbidity.
Presence of comorbidity was assessed with the modified Charlson Comorbidity Index27 at baseline and 30 months. We classified participants as having no comorbidity, incident comorbidity, or prevalent comorbidity. We defined no comorbidity as absence of comorbidity at baseline and at 30 months, incident comorbidity as absence of comorbidity at baseline with at least one comorbidity at 30 months, and prevalent comorbidity as at least one comorbidity at both baseline and 30 months.
Widespread pain.
We defined the presence of widespread pain according to the American College of Rheumatology classification criteria28 using participant-marked pain patterns on a figure of the human body. In particular, we classified participants as having widespread pain if they marked pain above and below the waist, pain on the right and left sides of the body, and axial pain. We classified participants as having no widespread pain, resolution of widespread pain, incident widespread pain, or prevalent widespread pain. We defined no widespread pain as not fulfilling the criteria for widespread pain at baseline and at 30 months, resolution of widespread pain as meeting the criteria for widespread pain at baseline but not at 30 months, incident widespread pain as not fulfilling the criteria for widespread pain at baseline but fulfilling the criteria at 30 months, and prevalent widespread pain as fulfilling the criteria for widespread pain at both baseline and 30 months.
Knee strength.
Knee strength was determined from the mean of 4 isokinetic knee extensor torque repetitions at 60°/s measured in newton-meters. Knee strength was measured only at baseline using the Cybex 350 Isokinetic Test and Exercise System and HUMAC software (version 4.3.2/Cybex 300, Cybex International Inc, Medway, Massachusetts). We categorized strength of the weaker knee into sex-specific quartiles.
Proprioceptive acuity.
We assessed proprioceptive acuity of the right knee using a protocol developed by Hurley et al29 and described elsewhere.30 Measurements of proprioceptive acuity were collected only at baseline. In short, we asked blindfolded participants in a seated position with both knees dangling off a chair to slowly extend their right knee to a predetermined position, relax their knee to the starting position, and then actively reproduce that predetermined position. We defined acuity as the average difference among 10 predetermined and reproduced positions. We categorized proprioceptive acuity into quartiles.
Potential Confounders
The following baseline factors were considered as potential confounders based on existing literature linking them to function12,17,31–34: age, sex, and race; body mass index (BMI) computed from standardized weight and height assessments; and total knee replacement at baseline or at follow-up assessed from self-report or radiographic evaluation.35
Data Analysis
To examine risk factors for a meaningful decrease in walking speed in our sample with a meaningful reduction in knee pain, we performed a multivariable-adjusted regression with a log-link function and robust standard errors to obtain risk ratios.36 All analyses were mutually adjusted for the risk factors under study. We also adjusted all models for potential confounders, including age, sex (male/female), race (white, other), BMI, and total knee replacement at baseline or follow-up (yes/no).
Role of the Funding Source
This study was supported by NIH AG18820, AG18832, AG18947, AG19069, AR007598, AR47785, NIH AR47885, NIAMS K23AR055127, the Arthritis Foundation New Investigator Award, the ACR/REF Junior Career Development in Geriatric Medicine Award (T. Franklin Williams Research Scholar Award), and the Boston Claude D. Pepper Older Americans Independence Center (grant P30-AG031679).
Results
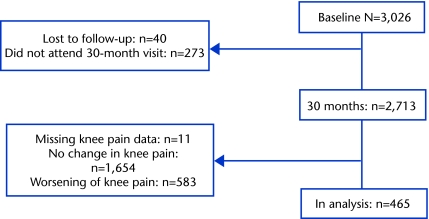
Of the 3,026 MOST participants assessed at baseline, 40 were lost to follow-up, 273 were unable to attend the 30-month study visit, and 11 had missing knee pain data. Of the remaining participants, 465 had a meaningful reduction in knee pain and were included in these analyses; the other participants either had no meaningful change in pain (n=1,654) or had a meaningful worsening of knee pain (n=583) and, therefore, were not included in this study (Figure). The characteristics of our study sample (ie, participants with a meaningful reduction in knee pain from baseline to follow-up) are listed in Table 1. The participants had a mean age of 63.3 years and a mean BMI of 31.3 kg/m2. The majority of the participants were female (67%), Caucasian (82%), and did not have depressive symptoms (84%). The frequencies of specific comorbidities from the modified Charlson Comorbidity Index are listed in Table 2.
Figure.
Flow chart of participants though baseline and 30 months.
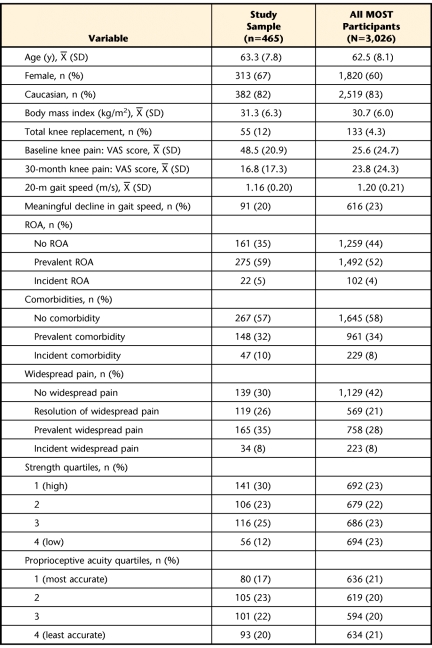
Table 1.
Summary Characteristics of the Study Samplea
MOST=Multicenter Osteoarthritis Study, VAS=visual analog scale, ROA=radiographic knee osteoarthritis.
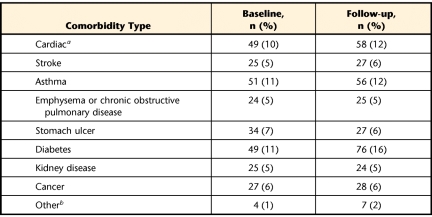
Table 2.
Frequency of Specific Comorbidities as Reported From the Modified Charlson Comorbidity Index
a Includes heart attack, bypass surgery, and heart failure.
b Includes Alzheimer disease, cirrhosis of the liver, leukemia, acquired immune deficiency disorder, and lymphoma.
Of the 465 participants with a meaningful reduction in knee pain who were included in the analyses, 20% had a meaningful decline in walking speed at 30 months (Tab. 1).
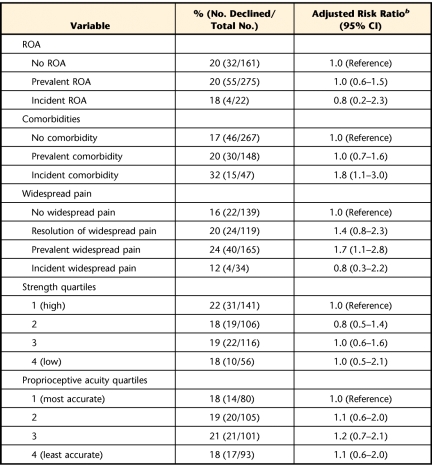
Participants with incident comorbidity and those with prevalent widespread pain had 1.8 and 1.7 times higher risk of a meaningful decline in walking speed, respectively, compared with those who had no comorbidity and those who had no widespread pain (adjusted risk ratio=1.8 [95% confidence interval=1.1–3.0] and 1.7 [95% confidence interval=1.1–2.8], respectively). There were no statistically significant associations of ROA, strength, or proprioceptive acuity with a meaningful decline in walking speed, with each of the effect estimates being close to the null. See Table 3.
Table 3.
Risk Factors for Meaningful Decline in Walking Speed Among Participants With Meaningful Reduction in Knee Paina
ROA=radiographic knee osteoarthritis, CI=confidence interval.
b Adjusted for age, sex, race, body mass index, and baseline knee pain. Risk factors were mutually adjusted for the other risk. Measurements of strength and proprioception were collected only at baseline. Higher risk ratios indicate greater risk of meaningful decline in walking speed.
Discussion
We found that 20% of the participants who had a meaningful reduction in pain in one or both knees had a meaningful decline in function as measured by walking speed. Among the participants who had a reduction in knee pain, those who had developed at least one comorbidity and who had widespread pain were more likely to have a decline in walking speed compared with their counterparts without comorbidity or widespread pain. We did not find any association between the presence of structural disease, knee extension strength, or proprioceptive acuity with a meaningful decline in walking speed.
Although higher pain severity has been shown to be strongly associated with more limitations in physical functioning,37,38 we found presence of widespread pain at baseline and 30 months to be an independent risk factor for decline in function. Previous studies also have demonstrated this association among adults with knee pain39,40 and older adults.13,14,41 Specifically, widespread pain is common among adults with knee pain and has been associated with worse knee pain and function.39,40 Among older adults, Leveille and colleagues14,41 found that widespread pain was associated with a twofold increase in the risk of developing severe difficulty with physical function 3 years later, after adjusting for potential confounders. Our study finding is consistent with previously published literature, suggesting that widespread pain is indeed an important risk factor for functional limitation.
We also found that the development of at least one comorbidity was independently associated with a meaningful decline in walking speed among participants with a reduction in knee pain. Few studies have formally examined the association of comorbidities with functional limitation, although comorbidity is frequently treated as a potential confounder in statistical analyses. Several studies have shown comorbidity to be associated with functional limitation among people following total knee replacement and people with knee OA,42,43 which supports our study findings. In the present study, the most common new comorbidities at 30 months were asthma, diabetes, and cancer. Certainly, each of these comorbidities can have multifactorial effects on walking speed as well as general physical functioning. It is noteworthy that walking speed has been found to be a marker of the effects of multiple aspects of health on an individual. In particular, Studenski and coauthors reported slower walking speed was predictive of hospital use and decline in overall health status11 and decreased survival in older adults.44
Interestingly, knee-specific factors, such as presence or worsening of structural disease, knee extensor strength, and proprioceptive acuity, did not appear to independently contribute to functional decline in this group. It may well be that those participants who had a reduction in knee pain did not have substantial impairments with these knee-specific factors. For instance, participants' proprioceptive acuity and knee extensor strength likely surpassed thresholds needed for walking at an adequate speed. The mean (SD) isokinetic knee extension strength of our sample was 61.9 (33.4) N·m, which is similar to values reported in women with preradiographic and early radiographic disease.45 Similarly, study participants likely did not have sufficiently severe structural disease to slow walking speed. Only 18% of the participants included in the study had end-stage radiographic disease at the follow-up visit. Furthermore, we were only able to measure strength and proprioceptive acuity at baseline. Thus, we were unable to assess how changes in these factors were associated with decline in walking speed.
Our study has several strengths. This study was conducted in the context of a large prospective cohort for whom high-quality data, including important potential confounders, were collected in a standardized fashion at each clinic visit. The size of the overall cohort permitted identification of an adequate number of older adults with reductions in knee pain to enable these analyses to be conducted. For our particular study sample and outcomes used, we utilized cutpoints anchored to meaningful change in pain and in function.
There are some limitations to our study. First, we used only one measure of function (ie, walking speed), primarily because walking speed has clinical health implications and is highly relevant to people with knee OA. Second, given that our study examined changes in risk factors with changes in walking speed, we cannot infer causality or directionality directly from our data. For instance, we are unable to confirm that a decline in walking speed took place after the development of comorbidity because study data were collected at baseline and 30 months. There is a possibility of reverse causality. For example, participants who walked slower could subsequently have had a reduction in knee pain. We believe this outcome is unlikely given that trials have demonstrated reductions in knee pain following intervention to increase walking speed in people with symptomatic knee OA.46–48 Third, we investigated factors associated with worse function only in participants who had a meaningful reduction in knee pain. Thus, our findings are not readily generalizable to those who have had no reduction in or worsening of their knee pain. However, for the purposes of this study, we were most interested in identifying risk factors for what is thought to be a paradoxical decline in function in the presence of reduction in knee pain. Lastly, we used a definition of meaningful change in gait speed from studies of older adults whose mean age was 77 to 78 years, which was higher than the mean age of 63 years in our sample. Despite this difference, we believe the minimum clinically important difference we used is still relevant to our young older adult sample.
In summary, we find it noteworthy that a fifth to a quarter of the participants with a meaningful reduction in knee pain had a meaningful decline in function. Our findings call into question the assumption that knee pain reduction will automatically lead to improvements in function. Our study suggests that clinicians should note outcomes in both pain and function, as both may not change concordantly. Furthermore, our findings suggest that patients who develop a new comorbidity or have widespread pain may be at risk of functional decline, highlighting the importance of patients' overall health beyond their musculoskeletal health on physical functioning. From a research perspective, comorbidity and widespread pain should be taken into account when examining longitudinal changes in function.
Footnotes
Dr White, Dr Felson, and Dr Neogi provided concept/idea/research design. Dr White, Dr Felson, Dr Nevitt, and Dr Neogi provided writing. Dr Felson, Dr Nevitt and Dr Torner provided data collection. Dr Nevitt and Dr Torner provided project management. Dr White, Dr Felson, Dr Niu, and Dr Neogi provided data analysis. Dr White, Dr Felson, Dr Nevitt, Dr Lewis, and Dr Torner provided fund procurement. Dr Lewis and Dr Torner provided participants and facilities/equipment. Dr Torner provided institutional liaisons. Dr Niu, Dr Nevitt, Dr Lewis, Dr Torner, and Dr Neogi provided consultation (including review of manuscript before submission).
The study protocol was approved by the institutional review boards at the University of Iowa, the University of California San Francisco, the University of Alabama, and Boston University Medical Center.
This study was supported by NIH AG18820, AG18832, AG18947, AG19069, AR007598, AR47785, NIH AR47885, NIAMS K23AR055127, the Arthritis Foundation New Investigator Award, the ACR/REF Junior Career Development in Geriatric Medicine Award (T. Franklin Williams Research Scholar Award), and the Boston Claude D. Pepper Older Americans Independence Center (grant P30-AG031679).
References
- 1. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799 [DOI] [PubMed] [Google Scholar]
- 2. Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights, part 1: the disease and its risk factors. Ann Intern Med. 2000;133:635–646 [DOI] [PubMed] [Google Scholar]
- 4. Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–499 [DOI] [PubMed] [Google Scholar]
- 5. Jordan KM, Arden NK, Doherty M, et al. EULAR Recommendations 2003: an evidence-based approach to the management of knee osteoarthritis. Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62:1145–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mallen CD, Peat G, Thomas E, Lacey R, Croft P. Predicting poor functional outcome in community-dwelling older adults with knee pain: prognostic value of generic indicators. Ann Rheum Dis. 2007;66:1456–4561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thomas E, Peat G, Mallen C, et al. Predicting the course of functional limitation among older adults with knee pain: do local signs, symptoms and radiographs add anything to general indicators? Ann Rheum Dis. 2008;67:1390–1398 [DOI] [PubMed] [Google Scholar]
- 8. Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon). 2008;23:320–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jinks C, Jordan K, Croft P. Osteoarthritis as a public health problem: the impact of developing knee pain on physical function in adults living in the community (KNEST 3). Rheumatology (Oxford). 2007;46:877–881 [DOI] [PubMed] [Google Scholar]
- 10. White DK, Zhang Y, Niu J, et al. Do worsening knee radiographs mean greater chances of severe functional limitation? Arthritis Care Res (Hoboken). 2010;62:1433–1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Studenski SA, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322 [DOI] [PubMed] [Google Scholar]
- 12. Sharma L, Cahue S, Song J, et al. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48:3359–3370 [DOI] [PubMed] [Google Scholar]
- 13. Eggermont LH, Bean JF, Guralnik JM, Leveille SG. Comparing pain severity versus pain location in the MOBILIZE Boston study: chronic pain and lower extremity function. J Gerontol A Biol Sci Med Sci. 2009;64:763–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leveille SG, Ling S, Hochberg MC, et al. Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med. 2001;135:1038–1046 [DOI] [PubMed] [Google Scholar]
- 15. Hardy SE, Perera S, Roumani YF, et al. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55:1727–1734 [DOI] [PubMed] [Google Scholar]
- 16. Dumurgier J, Elbaz A, Ducimetiere P, et al. Slow walking speed and cardiovascular death in well functioning older adults: prospective cohort study. BMJ. 2009;339:b4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Felson DT, Niu J, Guermazi A, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–2992 [DOI] [PubMed] [Google Scholar]
- 18. Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002;29:131–138 [PubMed] [Google Scholar]
- 19. Fransen M, Crosbie J, Edmonds J. Reliability of gait measurements in people with osteoarthritis of the knee. Phys Ther. 1997;77:944–953 [DOI] [PubMed] [Google Scholar]
- 20. Curb JD, Ceria-Ulep CD, Rodriguez BL, et al. Performance-based measures of physical function for high-function populations. J Am Geriatr Soc. 2006;54:737–742 [DOI] [PubMed] [Google Scholar]
- 21. Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743–749 [DOI] [PubMed] [Google Scholar]
- 22. Kwon S, Perera S, Pahor M, et al. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging. 2009;13:538–544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Palombaro KM, Craik RL, Mangione KK, Tomlinson JD. Determining meaningful changes in gait speed after hip fracture. Phys Ther. 2006;86:809–816 [PubMed] [Google Scholar]
- 24. Altman RD, Hochberg M, Murphy WA, Jr, et al. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(suppl A):3–70 [PubMed] [Google Scholar]
- 25. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Felson DT, McAlindon TE, Anderson JJ, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage. 1997;5:241–250 [DOI] [PubMed] [Google Scholar]
- 27. Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84 [DOI] [PubMed] [Google Scholar]
- 28. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33:160–172 [DOI] [PubMed] [Google Scholar]
- 29. Hurley MV, Rees J, Newham DJ. Quadriceps function, proprioceptive acuity and functional performance in healthy young, middle-aged and elderly subjects. Age Ageing. 1998;27:55–62 [DOI] [PubMed] [Google Scholar]
- 30. Felson DT, Gross KD, Nevitt MC, et al. The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum. 2009;61:1070–1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80:945–949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jordan J, Luta G, Renner J, et al. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol. 1997;24:1344–1349 [PubMed] [Google Scholar]
- 33. Eyler AA, Brownson RC, Bacak SJ, Housemann RA. The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc. 2003;35:1529–1536 [DOI] [PubMed] [Google Scholar]
- 34. Penninx BW, Guralnik JM, Ferrucci L, et al. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998;279:1720–1726 [DOI] [PubMed] [Google Scholar]
- 35. Escobar A, Quintana JM, Bilbao A, et al. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage. 2007;15:273–280 [DOI] [PubMed] [Google Scholar]
- 36. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706 [DOI] [PubMed] [Google Scholar]
- 37. McAlindon TE, Cooper C, Kirwan JR, Dieppe PA. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis. 1993;52:258–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dieppe PA, Cushnaghan J, Shepstone L. The Bristol “OA500” study: progression of osteoarthritis (OA) over 3 years and the relationship between clinical and radiographic changes at the knee joint. Osteoarthritis Cartilage. 1997;5:87–97 [DOI] [PubMed] [Google Scholar]
- 39. Wood LR, Peat G, Thomas E, Duncan R. The contribution of selected non-articular conditions to knee pain severity and associated disability in older adults. Osteoarthritis Cartilage. 2008;16:647–653 [DOI] [PubMed] [Google Scholar]
- 40. Jinks C, Jordan KP, Blagojevic M, Croft P. Predictors of onset and progression of knee pain in adults living in the community: a prospective study. Rheumatology (Oxford). 2008;47:368–374 [DOI] [PubMed] [Google Scholar]
- 41. Leveille SG, Bean J, Ngo L, et al. The pathway from musculoskeletal pain to mobility difficulty in older disabled women. Pain. 2007;128:69–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Singh G, Miller JD, Lee FH, et al. Prevalence of cardiovascular disease risk factors among US adults with self-reported osteoarthritis: data from the Third National Health and Nutrition Examination Survey. Am J Manag Care. 2002;8:S383–S391 [PubMed] [Google Scholar]
- 43. Reichmann WM, Katz JN, Kessler CL, et al. Determinants of self-reported health status in a population-based sample of persons with radiographic knee osteoarthritis. Arthritis Rheum. 2009;61:1046–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Studenski SA, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Diracoglu D, Baskent A, Yagci I, et al. Isokinetic strength measurements in early knee osteoarthritis. Acta Reumatol Port. 2009;34:72–77 [PubMed] [Google Scholar]
- 46. Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the Fitness Arthritis and Seniors Trial (FAST). JAMA. 1997;277:25–31 [PubMed] [Google Scholar]
- 47. Kovar PA, Allegrante JP, MacKenzie CR, et al. Supervised fitness walking in patients with osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 1992;116:529–534 [DOI] [PubMed] [Google Scholar]
- 48. Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50:1501–1510 [DOI] [PubMed] [Google Scholar]