Abstract
Magnetic resonance imaging (MRI) studies in children with maltreatment-related posttraumatic stress disorder (PTSD) have demonstrated smaller corpus callosum area, with the greatest magnitude of change in posterior portions of the corpus callosum. The purpose of this study was to measure corpus callosum area in adult female patients with childhood abuse-related PTSD and comparison subjects. MRI was used to measure the midsagittal area of the corpus callosum as well as subregions of the corpus callosum in 9 female subjects with abuse-related PTSD and 9 healthy female subjects. No differences were found in total area of the corpus callosum or in individual subregions, but the subregion/total area ratio was significantly smaller in posterior midbody in PTSD compared with the healthy subjects. These results suggest that relatively smaller areas of the posterior midbody of the corpus callosum are associated with childhood abuse related PTSD in adults; these findings are consistent with findings in children with abuse-related PTSD.
Keywords: Posttraumatic stress disorder, corpus callosum, abuse-related, magnetic resonance imaging
Posttraumatic stress disorder (PTSD), which is characterized by re-experiencing symptoms, emotional numbing, and increased arousal after exposure to a traumatic event, is a highly prevalent disorder, affecting 8% of the population by some estimates (Kessler et al., 1995). Magnetic resonance imaging (MRI) studies have demonstrated changes in brain morphology in PTSD, including smaller volume of the hippocampus (Kitayama et al., 2005) and anterior cingulate cortex (Kitayama et al., 2006; Rauch et al., 2003).
Some studies of children with PTSD showed smaller corpus callosum area in comparison to healthy subjects (De Bellis et al., 1999; De Bellis et al., 2002). Because neuronal fibers connect the left and right hemispheres of the brain and maintain a somatotopic arrangement (Innocenti et al., 1974), morphological abnormalities in specific corpus callosum areas are thought to be associated with abnormalities in corresponding cortical regions (Witelson, 1989). Findings of smaller corpus callosum size in children with PTSD related to maltreatment have led to the hypothesis that maltreatment is associated with a reduction in corpus callosum size. It is also possible that a preexistent smaller volume of the corpus callosum predisposes the individual to develop PTSD after traumatic events. There is only 1 study that showed smaller size of the corpus callosum in adults with PTSD; this study was performed in a heterogeneous sample with mixed gender and a variety of traumas (Villarreal et al., 2004). Some studies of normal human subjects have shown gender differences (Suganthy et al., 2003) whereas others have not (Luders et al., 2006). No studies have looked at corpus callosum size in adult females with PTSD related to early abuse.
The purpose of the current study was to assess size of the corpus callosum in adult female patients with abuse-related PTSD.
METHODS
MRI was used to assess the corpus callosum area in 9 female subjects with abuse-related PTSD (mean = 37.8 years, SD = 9.8) and 9 female subjects without PTSD and any other psychiatric symptoms who were matched their age (mean = 36.8 years, SD = 8.9). Women with PTSD had fewer years of education than non-PTSD (PTSD: mean = 14.4, SD = 1.0, non-PTSD: mean = 18.2, SD = 1.0; p < 0.015). The 9 subjects with PTSD met DSM-IV criteria for current PTSD, according to the Clinician Administered PTSD Scale (mean score = 75.6, SD = 30.9). Psychiatric disorder was assessed using the Structured Clinical Interview for DSM-IV (SCID). Seven of the patients had experiences of sexual abuse, 1 of physical abuse, and the other 1 witnessed adult spousal abuse in their childhood before 13 years old. Eight of the patients had a history of major depressive disorder, 2 had a current or history of panic disorder, and 3 subjects had a history of alcohol or substance abuse. No subjects had severe comorbid conditions during their participation in this study. All the healthy subjects were also interviewed with the SCID and the Early Trauma Inventory. All subjects provided written informed consent.
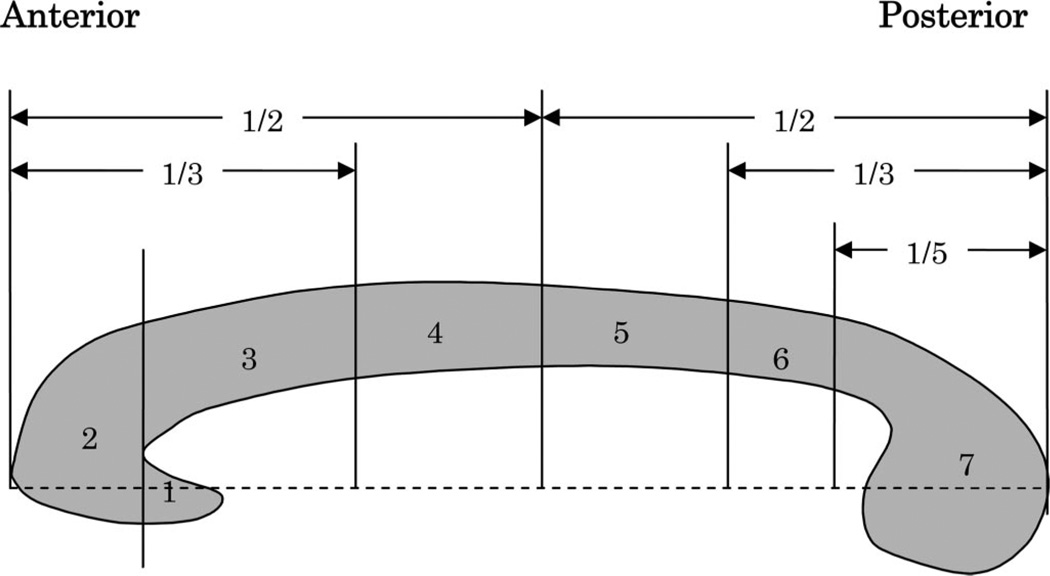
Magnetic resonance images were acquired using methods described in detail elsewhere (Vermetten et al., 2003). The MR images were analyzed using BrainWork software, developed at Emory University, on a Sun Ultra 80 workstation. A midsagittal slice, reformatted from an axial 3-dimensional volumetric T1-weighted gradient echo scan of the whole brain, in which the septum pellucidum was most clearly visualized, was chosen for the measurement. A single trained rater blinded to subject identity manually traced the edge of the corpus callosum. The BrainWork Program automatically realigned along the dominant axis of the structure and divided the corpus callosum into 7 subregions, including rostrum, genu, rostral body, anterior midbody, posterior midbody, isthmus, and splenium as previously described (Clarke et al., 1989; Witelson, 1989; Giedd et al., 1994, Fig. 1). The area of each subregion was calculated automatically by BrainWork, and the results were calculated as absolute area and the percentage of subregion/total area ratio.
FIGURE 1.
Midsagittal divisions of corpus callosum for MRI measurements. Adopted from Witelson, 1989 and Giedd et al., 1994. (1) Rostrum: Caudal/orbital prefrontal, inferior premotor region; (2) Genu: Prefrontal region; (3) Rostral body: Premotor, supplementary motor region; (4) Anterior midbody: Motor region; (5) Posterior midbody: Somatesthetic, posterior parietal region; (6) Isthmus: Superior temporal, posterior parietal region; (7) Splenium: Occipital, inferior temporal region.
The significance was defined as p < 0.05, the trend was p < 0.10, and t test was used as a statistical analysis.
RESULTS
There was no difference in total corpus callosum area between women with PTSD and healthy subjects (629.9 ± 111.0 mm2 vs. 616.0 ± 29.9 mm2, p = 0.74). As shown in Table 1, no significant differences were found between the absolute CC area of PTSD and the healthy subjects in any of the 7 subregions and total size of the corpus callosum. However, the percentage of subregion/total area ratio was significantly smaller in posterior midbody, region 5 (11.3 ± 1.3 vs. 12.9 ± 1.5, p = 0.027) in PTSD compared with the healthy subjects. There was also a trend for smaller ratio in anterior midbody, region 4 (12.6 ± 1.0 vs. 13.8 ± 1.8, p = 0.095).
TABLE 1.
Corpus Callosum Measures of Abuse-Related PTSD and Non-PTSD Controls
| Absolute Area (SD) mm2 |
Percentage of Subregion/Total Area Ratio (SD) × 100% |
|||||
|---|---|---|---|---|---|---|
| PTSD (N = 9) |
Non-PTSD (N = 9) |
PTSD (N = 9) |
Non-PTSD (N = 9) |
p |
||
| Absolute | Ratio | |||||
| Region 1 (Rostrum) | 27.6 (12.7) | 22.9 (9.7) | 4.4 (1.8) | 3.7 (1.5) | 0.39 | 0.41 |
| Region 2 (Genu) | 125.3 (29.7) | 122.6 (13.5) | 19.8 (2.9) | 20.0 (1.2) | 0.80 | 0.86 |
| Region 3 (Rostral body) | 68.4 (18.5) | 61.9 (18.5) | 10.9 (2.8) | 9.9 (2.5) | 0.47 | 0.44 |
| Region 4 (Anterior midbody) | 79.6 (15.6) | 84.9 (12.6) | 12.6 (1.0) | 13.8 (1.8) | 0.43 | 0.095 |
| Region 5 (Posterior midbody) | 72.4 (19.1) | 79.4 (9.6) | 11.3 (1.3) | 12.9 (1.5) | 0.34 | 0.027* |
| Region 6 (Isthmus) | 65.0 (12.3) | 63.7 (11.6) | 10.3 (9.5) | 10.4 (1.7) | 0.83 | 0.95 |
| Region 7 (Splenium) | 195.4 (40.2) | 180.6 (26.3) | 30.8 (1.7) | 29.3 (2.6) | 0.37 | 0.17 |
| Total area | 633.6 (117.1) | 616.0 (56.4) | — | — | 0.69 | — |
p < 0.05.
DISCUSSION
This study did not find smaller size of the absolute total corpus callosum or 7 subregions of the corpus callosum in adult women with PTSD related to early childhood abuse, but the subregion/total area ratio was significantly smaller in posterior midbody in PTSD compared with the healthy subjects, and there was also a trend for smaller ratio in anterior midbody.
De Bellis and colleagues (De Bellis et al., 1999) previously found smaller total corpus callosum size and size of subregions including posterior midbody, isthmus and splenium in boys and girls with maltreatment-related PTSD. Villarreal et al. also reported smaller corpus callosum size in male and female adult patients with PTSD, including smaller genu, midbody, isthmus, and total corpus callosum area (Villarreal et al., 2004). In the current study, there was pattern of smaller posterior midbody that was statistically significant in subregion/total area ratio; also, the magnitude of difference was as great as in the studies by De Bellis et al. (1999, 2002).
De Bellis et al. suggested that the continued development of the prefrontal cortex into the third decade of life explained the lack of smaller areas of the corpus callosum in regions 1, 2, and 3, that map onto the prefrontal cortex, in children with PTSD (De Bellis et al., 1999). The current study similarly showed preferentially smaller corpus callosum areas in the posterior part of the corpus callosum in adults with PTSD related to early childhood abuse. Therefore this study is consistent with the findings of De Bellis and colleagues. Furthermore, to the best of our knowledge, this is the first report that has demonstrated smaller areas of the posterior corpus callosum in adults with PTSD related to early childhood abuse.
Limitations of this study include the following: (a) De Bellis et al. reported that smaller corpus callosum area was more prominent in males in pediatric PTSD (De Bellis and Keshavan, 2003) although our study is in females. In comparison, Teicher et al. mentioned that sexual abuse seemed to be a strong factor associated with reduced corpus callosum size in girls (Teicher et al., 2004). Future adult studies will require further examinations to clarify the existence of sex differences in adult PTSD. (b) Relatively lower power due to the small sample size. (c) The alteration in the corpus callosum might be affected by the difference in education years and/or the comorbid major depression or a combination of comorbid disorders. (d) Other important factors which may relate to the development of the corpus callosum, such as socioeconomic status and social support, are not considered in this study. (e) The current study does not address whether these findings are related to trauma exposure or PTSD. Future studies should be performed to compare PTSD patients to abused subjects without PTSD.
In conclusion, the results of the current study are similar to previous reports in both children and adult PTSD. These findings suggest that PTSD in both adults and children is associated with alterations in brain structure. This study does not establish whether smaller area of subregions of corpus callosum is a cause or consequence of stress-related psychiatric disorder. Future prospective studies are indicated to address this question.
REFERENCES
- Clarke S, Kraftsik R, van der Loos H, Innocenti GM. Forms and measures of adult and developing human corpus callosum: Is there sexual dimorphism? J Comp Neurol. 1989;280:213–230. doi: 10.1002/cne.902800205. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Keshavan MS, Clark DB, Casey BJ, Giedd JN, Boring AM, Frustaci K, Ryan ND. Developmental traumatology. Part II: Brain development. Biol Psychiatry. 1999;45:1271–1284. doi: 10.1016/s0006-3223(99)00045-1. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Keshavan MS, Shifflett H, Iyengar S, Beers SR, Hall J, Moritz G. Brain structures in pediatric maltreatment-related posttraumatic stress disorder: A sociodemographically matched study. Biol Psychiatry. 2002;52:1066–1078. doi: 10.1016/s0006-3223(02)01459-2. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Keshavan MS. Sex differences in brain maturation in maltreatment-related pediatric posttraumatic stress disorder. Neurosci Biobehav Rev. 2003;27:103–117. doi: 10.1016/s0149-7634(03)00013-7. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Castellanos FX, Casey BJ, Kozuch P, King AC, Hamburger SD, Rapoport JL. Quantitative morphology of the corpus callosum in attention deficit hyperactivity disorder. Am J Psychiatry. 1994;151:665–669. doi: 10.1176/ajp.151.5.665. [DOI] [PubMed] [Google Scholar]
- Innocenti GM, Manzoni T, Spidalieri G. Patterns of the somesthetic messages transferred through the corpus callosum. Exp Brain Res. 1974;19:447–466. doi: 10.1007/BF00236110. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kitayama N, Vaccarino V, Kutner M, Weiss P, Bremner JD. Magnetic resonance imaging (MRI) measurement of hippocampal volume in posttraumatic stress disorder: A meta-analysis. J Affect Disord. 2005;88:79–86. doi: 10.1016/j.jad.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Kitayama N, Quinn S, Bremner JD. Smaller volume of anterior cingulate cortex in abuse-related posttraumatic stress disorder. J Affect Disord. 2006;90:171–174. doi: 10.1016/j.jad.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luders E, Narr KL, Zaidel E, Thompson PM, Toga AW. Gender effects on callosal thickness in scaled and unscaled space. Neuro Report. 2006;17:1103–1106. doi: 10.1097/01.wnr.0000227987.77304.cc. [DOI] [PubMed] [Google Scholar]
- Rauch SL, Shin LM, Segal E, Pitman RK, Carson MA, McMullin K, Whalen PJ, Makris N. Selectively reduced regional cortical volumes in post-traumatic stress disorder. Neuroreport. 2003;14:913–916. doi: 10.1097/01.wnr.0000071767.24455.10. [DOI] [PubMed] [Google Scholar]
- Suganthy J, Raghuram L, Antonisamy B, Vettivel S, Madhavi C, Koshi R. Gender- and age-related differences in the morphology of the corpus callosum. Clin Anat. 2003;16:396–403. doi: 10.1002/ca.10161. [DOI] [PubMed] [Google Scholar]
- Teicher MH, Dumont NL, Ito Y, Vaituzis C, Giedd JN, Anderson SL. Childhood neglect is associated with reduced corpus callosum area. Biol Psychiatry. 2004;56:80–85. doi: 10.1016/j.biopsych.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Vermetten E, Vythilingam M, Southwick SM, Charney DS, Bremner JD. Long-term treatment with Paroxetine increases verbal declarative memory and hippocampal volume in posttraumatic stress disorder. Biol Psychiatry. 2003;54:693–702. doi: 10.1016/s0006-3223(03)00634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal G, Hamilton DA, Graham DP, Driscoll I, Qualls C, Petropoulos H, Brooks WM. Reduced area of the corpus callosum in posttraumatic stress disorder. Psychiatry Res. 2004;131:227–235. doi: 10.1016/j.pscychresns.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Witelson SF. Hand and sex differences in the isthmus and genu of the human corpus callosum. A postmortem morphological study. Brain. 1989;112:799–835. doi: 10.1093/brain/112.3.799. [DOI] [PubMed] [Google Scholar]