Abstract
This study examined the associations between social networks, social support, social cohesion and perceived neighborhood safety among an ethnically diverse sample of 1352 residents living in 12 low-income public housing sites in Boston, Massachusetts. For males and females, social cohesion was associated with perceived safety. For males, a smaller social network was associated with greater feelings of safety. Social support was not a significant predictor of perceived safety. The findings reported here are useful in exploring a potential pathway through which social environmental factors influence health and in untangling the complex set of variables that may influence perceived safety.
Keywords: Social networks, social support, social cohesion, neighborhood safety, public housing residents
Introduction
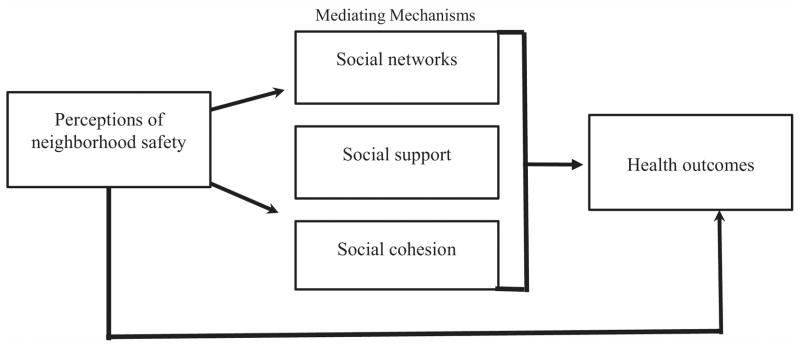
A growing body of public health research suggests that perceptions of neighborhood safety are linked to health outcomes (Macintyre & Ellaway, 2000; Chandola, 2001; Ziersch, Baum, MacDougall, & Putland, 2005; Baum, Ziersch, Zhang, & Osborne, 2009). Perceiving one’s neighborhood as unsafe has been significantly associated with anxiety (Middleton, 1998), poor health outcomes (Macintyre & Ellaway, 2000), and poor self-rated health (Chandola, 2001). Furthermore, evidence suggests that individuals’ sense of neighborhood safety is associated with the extent to which they participate in and interact with their community (Sampson, 2003; Young, Russell, & Powers, 2004; Ziersch, Putland, Palmer, MacDougall, & Baum, 2007; Lochner, Kawachi, & Kennedy, 1999; Baum et al., 2009). Empirical studies examining the role of neighborhood factors on health demonstrate that higher levels of safety are associated with higher respondent perceptions of social cohesion and better health outcomes (eg, Wen, Kandula, & Lauderdale, 2007; King, 2008). Scientific research demonstrates that “the degree to which an individual is interconnected and embedded in a community—is vital to an individual’s health and well-being…” (Berkman & Glass, 2000). This paper examines perceptions of neighborhood safety as a potential mechanism through which social environmental factors--social support, social networks, and social cohesion--may influence health (Diagram 1).
Diagram 1.
Conceptual pathway between perceptions of neighborhood safety and health
Two commonly measured characteristics of social relationships are social support and social networks (Cohen & Syme, 1985; Heaney & Israel, 1997). Social support has been broadly defined as resources (eg, emotional, instrumental, and financial support) provided in the context of a relationship (Cohen & Syme, 1985). Social networks refer to the web of social relationships that surround an individual, and provide information on the extent to which an individual is connected with others (Berkman & Syme, 1979). Another key aspect of the social environment is social cohesion which refers to the extent of connectedness and solidarity among groups (Kawachi & Berkman, 2000).
Studies exploring the interrelationships among residents of different public housing programs has resulted in mixed findings. Social network structure tends to vary by socioeconomic status (SES), and the social networks of those with lower incomes tend to be more place-based, be homogeneously low income, contain more close relationships, and contain more overlapping relations (eg, Campbell & Lee, 1992). However, several studies contradict these findings (eg, Hurlbert, Beggs, & Haines, 2001; Kleit, 2001; Chaskin & Joseph, 2010). For example, Hurlbert et al. (2001) examined poor people’s networks in a low-income neighborhood and found that those who lived in low-income neighborhoods, rather than being involved in more intense and strong relationships, instead tended to have weaker relationships than those in middle-income areas. Kleit’s (2001) study demonstrated that scattered-site and clustered public housing residents differ very little in terms of the number of neighbors they know, the degree of embeddedness of relationships within their neighborhoods, and the amount of aid received from their neighbors.
Although social support, social networks, and social cohesion factors have been found in the literature to have important implications for health (Macintyre & Ellaway, 2000; Cattell, 2001; Ziersch et al., 2005; Almedom, 2005; De Silva, McKenzie, Harpham, & Huttly, 2005; Ziersch et al., 2007), the mechanisms through which they work are not well-understood, particularly among low-income populations in urban settings. In this paper, we were interested in examining whether public housing residents’ perceptions of specific characteristics of the social environment—social support, social networks, and social cohesion—influence their perceptions of neighborhood safety as a potential pathway through which social environmental factors influence health. We hypothesized that residents with larger social networks, higher levels of social support, and higher levels of social cohesion in their neighborhood would be more likely to perceive their neighborhood as safer compared to their counterparts. Additionally, we examined whether each of these associations differed by age, ethnicity/race, health status, financial status, and employment status.
Methods
Study design and sample
This study analyzed baseline data collected in 2004–2005 from Open Doors to Health (ODH), a cluster randomized control trial of colorectal cancer (CRC) prevention targeting CRC screening, physical activity, and multi-vitamin intake. Twelve urban public housing communities in low income Boston neighborhoods were the primary sampling units and individuals within housing sites served as secondary sampling units. Ninety-two percent of housing sites approached (12 out of 13) agreed to participate. The physical properties of the sites varied, from high-rise buildings clustered around common space, to distributed sites, where buildings with subsidized units were interspersed between buildings that did not belong to that site. Unequal probability sampling across housing sites was employed due to the varying size of housing sites. In half the sites where the population was less than 300, all adult residents were sampled. In the other half of the sites where the population size was greater than 300, a random sample was drawn to obtain a 35% sample with a minimum of 250 participants per site.
An initial sample of 3688 participants was drawn. Of them, 747 (20%) were deemed ineligible for various reasons including had a cognitive or physical disability, had active cancer, were too ill to participate, or were no longer at that address, leaving an eligible sample population of 2941 individuals. Of these, 828 (28%) refused participation and 559 (19%) were never reached. Enrollment and baseline surveys were obtained on 1554 participants. This yielded an overall 53% response rate, which ranged from a low of 34% to a high of 92% across the housing sites. This response rate is comparable to that of other community-based studies (Ellison-Loschmann, Sunyer, Plana, Pearce, Zock, et al., 2007; Tan, Choo, Archibald, & Esuvaranathan, 1997). Participants provided verbal informed consent and completed an interviewer-administered survey in either English or Spanish. They received US $25 compensation for their participation. The study protocol was approved by the human subjects committee at the Harvard School of Public Health.
On the basis of the cluster design, data for all analyses were weighted up to the population size within each housing site (weighted sample size of 1980). The data reported here represent baseline data, among participants who answered questions on perceived neighborhood safety. Those missing data for this outcome variable (n=202) were dropped (n=66 due to missing data; n=136 due to completion of a short form of the baseline survey because of time and other constraints). The short form did not include perceived safety questions.
Study recruitment
Study recruitment has been described in full detail elsewhere (Bennett, McNeill, Wolin, Duncan, Puleo, & Emmons, 2007). Briefly, participant recruitment began with housing site representatives sending letters announcing the study to their eligible residents. A total of 14–16 contact attempts were made (10 phone attempts and a minimum of 4 door knocks, 6 if no phone). Eligibility criteria for the study survey included: (1) residence in one of the participating housing communities, (2) age of at least 18 years, and (3) fluency in English or Spanish.
Measures
Sociodemographic characteristics
Race/ethnicity (categorized as Hispanic, Black, White, and Other), gender, and age were assessed using standard demographic questions during the interview-administered survey. Health status was captured by asking participants whether current health problems make it difficult for them to exercise (yes/no). Household financial status was assessed on four dimensions and dichotomized as comfortable with some extras/enough but no extras versus have to cut back/can’t make ends meet. Poverty status was assessed by combining yearly household income and the number of people supported by this income. Poverty status was dichotomized as being above or below the poverty level based on the 2005 Federal Poverty Guidelines on income and household size (HHS, 2005). In addition, employment status was assessed and organized into four categories and dichotomized into work full-time/part-time versus disabled/not working. Participants’ first or native language, level of education, and immigrant status were also assessed.
Perceived social environmental factors
Social networks were measured using the Berkman-Syme Social NetworksIndex (BSSNI), a composite measure of four types of social connection: marital status, sociability, church group membership, and membershipin other community organizations (Berkman & Syme, 1979). Items included: (1) Are you married or living with a partner now? (Responses: No, Yes); (2) How many relatives, like your spouse, children, aunts, uncles, brothers, or sisters do you feel close to? (Responses: None; 1 or 2; 3–5; 6–9; 10 or more); (3) How many close friends do you have? (Responses: None; 1 or 2; 3–5; 6–9; 10 or more); and (4) Are you an active member of any of these groups or clubs? (Responses: a) Church, temple, mosque, or other religious group; b) recreation or sport league; c) civic, political, service, housing site, or other community organization; d) professional trade or labor organization; e) any other organization (write-in). The summary scores ranged from 0 to 4 reflecting the number of social network ties (Berkman & Syme, 1979). A median split of two categories was then created (< 2 ties; 3–4 ties) for these analyses, based on the distribution of responses.
Social support was assessed in three of the four domains of the Inventory of Socially Supportive Behaviors (emotional, instrumental, and financial support) (Barrera, Sandler, & Ramsey, 1981). Residents were asked: (1) Can you count on a friend or relative to give you emotional support; (2) When you need some extra help, can you count on a friend or relative to help you with daily tasks?; (3) When you need some extra money for basic needs, can you count on a friend or relative to help you?; (4) If you needed help getting to the doctor, is there someone who would help you?; and (5) When you are sick and need extra help, can you count on a friend or relative to help you? Responses included: Yes, always; Yes, sometimes; No, there isn’t anyone like that; I don’t need help; Yes, but I wouldn’t accept help. A summary score for social support ranging from 0 to 5 was created by adding the number of responses to the five questions. Due to limited variability, social support was dichotomized into high level of social support (score of 5) or lower level of social support (score of <5) for the purposes of analyses.
Social cohesion was assessed on dimensions suggested by Sampson and colleagues, examining perceptions of trust and shared values in one’s neighborhood (Sampson, Raudenbush, & Earls, 1997). Residents were asked to report their agreement (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) with five statements: (1) People around here are willing to help their neighbors; (2) This is a close-knit neighborhood; (3) People in this neighborhood can be trusted; (4) People in this neighborhood generally do not get along with each other; and (5) People in this neighborhood do not share the same values (Cronbach’s alpha= .7801). A summary score ranged from 1 to 4 with a higher score indicating higher social cohesion.
Perceptions of neighborhood safety
The outcome variable “perceived neighborhood safety,” was measured using previously tested questions (with slight modifications to accommodate literacy concerns) (Pebley & Narayan, 2003; Rountree, & Land, 1996). For both “daytime” and “night-time,” participants were asked: “…how safe do you feel walking alone in your neighborhood?” These questions are designed to capture global perceptions of neighborhood safety and as such, may reflect views on a variety of factors (eg, crime, traffic, green space, etc.). Response options included: unsafe, safe, and a little unsafe. For analysis purposes, we computed a 3-category outcome variable: (1) “unsafe” if perceived neighborhood as “not at all safe” either at night or during the day; (2) “safe” if perceived neighborhood as “safe” both at night and during the day; and (3) “a little unsafe” if any combination of day or night was reported as “a little unsafe.”
Data analysis
Frequency distributions and estimates of means and standard errors were calculated for all exposures, outcome, and covariates of interest to assess distributional assumptions and outliers. Crosstabs of demographic characteristics, organized by perceptions of neighborhood safety for males and females separately revealed gender differences, and thus gender-stratified bivariate analyses were also conducted. Based on the bivariate associations and consideration of confounders, proportional odds polytomous logistic regression models accounting for the cluster design of the dependent variable were created (McCullagh, 1980; Stokes, Davis, & Koch, 2000). In these models, odds ratios represent incremental odds between the 3 categories of the outcome variable (feeling safe vs. a little unsafe and unsafe, and, feeling a little unsafe vs. unsafe). Planned interaction analyses examining potential modifiers (eg, age, race/ethnicity, health status) in the association between social environmental factors (social networks, social support and social cohesion) and perceived safety were also conducted separately for each social factor. Only those variables that were significantly associated with neighborhood safety at the p .05 level or were found to be effect modifiers were retained in the final models. Appropriate analyses were conducted using SUDAAN 9.01 and SAS 9.1 statistical software for clustered data.
Results
Sociodemographic analyses
Table 1 presents demographics for the overall subsample of ODH participants for this study and by perceptions of neighborhood safety. The participants were largely non-white (96%), female (74%), had low levels of education (67% ≤ HS), and were either not currently working (40%) or were disabled (31%). Average age was 48 years old. Slightly more than half the participants were born in the U.S. (55%), reported English as their first language (54%), and were living below the poverty level (54%). A large percentage of the female residents (66%) and more than half of the male residents (57%) reported feeling “a little unsafe” or “unsafe” walking alone in their neighborhoods.
Table 1.
Participant characteristics overall and by perceptions of neighborhood safety (weighted N=1980**)
| Overall weighted (%) | Males weighted (%) | Females weighted (%) | |||||
|---|---|---|---|---|---|---|---|
| n (%) | Safe n (%) | A little unsafe n (%) | Unsafe n (%) | Safe n (%) | A little unsafe N (%) | Unsafe n (%) | |
| TOTAL | 1980 (100%) | 222 (44%) | 176 (35%) | 111 (22%) | 499 (34%) | 484 (33%) | 488 (33%) |
| Race/Ethnicity | |||||||
| Black | 957 (49%) | 109 (50%) | 76 (35%) | 34 (16%) | 270 (37%) | 253 (34%) | 216 (29%) |
| White | 89 (4%) | 15 (44%) | 14 (43%) | 5 (13%) | 23 (41%) | 21 (39%) | 11 (20%) |
| Hispanic | 863 (44%) | 89 (38%) | 73 (32%) | 70 (30%) | 186 (29%) | 196 (31%) | 250 (40%) |
| Other | 64 (3%) | 9 (40%) | 12 (51%) | 2 (9%) | 19 (46%) | 14 (34%) | 8 (20%) |
| Age | |||||||
| <35 | 469 (24%) | 54 (49%) | 49 (45%) | 7 (6%) | 117 (33%) | 147 (41%) | 96 (27%) |
| 35–49 | 518 (26%) | 46 (42%) | 37 (34%) | 26 (24%) | 171 (42%) | 148 (36%) | 89 (22%) |
| 50–64 | 628 (32%) | 65 (42%) | 55 (35%) | 36 (23%) | 147 (31%) | 129 (27%) | 196 (41%) |
| 65+ | 365 (18%) | 57 (43%) | 35 (26%) | 42 (31%) | 64 (28%) | 61 (26%) | 107 (46%) |
| Employment Status | |||||||
| Work full time | 459 (23%) | 60 (52%) | 38 (33%) | 17 (14%) | 139 (40%) | 131 (38%) | 74 (22%) |
| Work part time | 290 (15%) | 30 (47%) | 24 (38%) | 9 (15%) | 80 (35%) | 92 (40%) | 55 (24%) |
| Disabled | 433 (22%) | 37 (32%) | 42 (38%) | 34 (30%) | 99 (31%) | 78 (25%) | 142 (44%) |
| Not working | 799 (40%) | 95 (44%) | 71 (33%) | 51 (24%) | 181 (31%) | 183 (32%) | 216 (37%) |
| Poverty level | |||||||
| Above poverty level | 820 (46%) | 96 (42%) | 82 (36%) | 50 (22%) | 198 (33%) | 221 (37%) | 172 (29%) |
| Below poverty level | 965 (54%) | 101 (44%) | 77 (33%) | 54 (23%) | 245 (34%) | 211 (29%) | 275 (38%) |
| Education | |||||||
| Less than HS | 784 (40%) | 92 (38%) | 73 (30%) | 78 (32%) | 149 (28%) | 146 (27%) | 245 (45%) |
| Completed high school/vocational | 543 (27%) | 59 (48%) | 46 (37%) | 19 (15%) | 158 (38%) | 142 (34%) | 119 (28%) |
| At least some college | 650 (33%) | 71 (50%) | 56 (40%) | 14 (10%) | 191 (38%) | 195 (38%) | 123 (24%) |
| Immigrant | |||||||
| Born in US | 1078 (54%) | 120 (48%) | 96 (39%) | 32 (13%) | 294 (35%) | 306 (37%) | 229 (28%) |
| Born in Puerto Rico | 500 (25%) | 56 (38%) | 39 (26%) | 53 (36%) | 113 (32%) | 89 (25%) | 152 (43%) |
| Not born in US or PR | 401 (20%) | 46 (41%) | 41 (37%) | 26 (23%) | 92 (32%) | 89 (31%) | 106 (37%) |
| English 1st language | |||||||
| No | 904 (46%) | 95 (38%) | 80 (32%) | 76 (30%) | 199 (30%) | 194 (30%) | 260 (40%) |
| Yes | 1076 (54%) | 127 (49%) | 96 (37%) | 35 (14%) | 300 (37%) | 290 (35%) | 227 (28%) |
Perceptions of Neighborhood Safety for Male Residents
Bivariate analyses for male residents (Table 2) indicated that those who had completed high school (p≤.01) or at least some college (p≤.001), or who were born in the U.S. (p≤.03), or whose first language was English (p≤.03) were each significantly more likely to feel greater levels of safety compared to each of their counterparts. In addition, not having current health problems that made it difficult to exercise (p≤.001) was associated with perceptions of neighborhood safety in bivariate analyses for males.
Table 2.
Bivariate Model Predicting Neighborhood Safety (predicting greater feelings of neighborhood safety^)
| Males | Females | |||
|---|---|---|---|---|
| Weighted n | OR^ (95% CI) | Weighted n | OR^ (95% CI) | |
| Demographics | 504 | 1471 | ||
| Education | ||||
| Less than HS (Ref) | 228 | REF | 541 | REF |
| Completed HS/Voc | 122 | 1.85 (1.24, 2.76)* | 420 | 1.69 (1.20, 2.36)* |
| At least some college | 131 | 2.19 (1.37, 3.48)* | 509 | 1.82 (1.43, 2.32)* |
| Immigrant Status | ||||
| Born in US | 830 | 1.89 (1.06, 3.40)* | ||
| Born in Puerto Rico (ref) | 353 | REF | ||
| Not born in US or PR | 288 | 1.11 (0.54, 2.30) | ||
| English 1st Language | ||||
| Yes | 817 | 1.99 (1.53, 2.60)* | ||
| No (Ref) | 653 | REF | ||
| Race/Ethnicity | ||||
| Black | 739 | 1.96 (1.48, 2.60)* | ||
| Hispanic (Ref) | 631 | REF | ||
| White/Other | 97 | 1.75 (0.77, 3.95) | ||
| Age | ||||
| <35 | 109 | 1.52 (0.86, 2.69) | 359 | 1.31 (0.97, 1.77) |
| 35–49 | 109 | 1.01 (0.60, 1.70) | 408 | 1.82 (1.36, 2.44)* |
| 50+ (ref) | 290 | REF | 703 | REF |
| Employment Status | ||||
| Work full time/part time | 178 | 1.43 (0.87, 2.35) | 571 | 1.59 (1.27, 2.00)* |
| Disabled/not working (Ref) | 331 | REF | 900 | REF |
| Health problems make it difficult to exercise | ||||
| Yes (Ref) | 186 | REF | 675 | REF |
| No | 323 | 1.55 (1.21, 1.99)* | 794 | 1.38 (1.09, 1.75)* |
| Social networks | ||||
| Below median split | 216 | 1.28 (0.88, 1.86) | 581 | 1.05 (0.86, 1.28) |
| Median split or higher (Ref) | 292 | REF | 884 | REF |
| Social Support | ||||
| Has all 5 | 356 | 1.08 (0.64, 1.81) | 999 | 1.29 (1.03, 1.62)* |
| Does not have all 5 | 148 | REF | 462 | REF |
| Social cohesion | ||||
| Continuous | 482 | 1.49 (0.95, 2.35) | 1345 | 1.64 (1.32, 2.05)* |
p ≤ .05
polytomous model odds ratios represent odds for the 2 relationships: feeling safe vs. a little unsafe and unsafe, and feeling a little unsafe vs. unsafe
Table 3 displays the polytomous multivariable model of perceived neighborhood safety. As hypothesized, the overall association between social cohesion and perceptions of neighborhood safety remained significant (p≤0.03), controlling for education. We did not find a main effect of social support on perceptions of neighborhood safety as we had hypothesized. However, social networks (p≤.05) was significantly associated with perceived safety for male residents in the multivariable analyses, but in the opposite direction to our hypothesis. Men who reported having smaller social networks were more likely to perceive their neighborhoods as safer than those with larger social networks. Educational level was also a significant predictor of perceptions of neighborhood safety for male residents with higher levels of perceived safety among those with higher levels of education.
Table 3.
Multivariable Model Predicting Neighborhood Safety (predicting greater feelings of neighborhood safety^)
| Males | Females | |||
|---|---|---|---|---|
| Weighted n | OR^ (95% CI) | Weighted n | OR^ (95% CI) | |
| Demographics | 504 | 1471 | ||
| Education | ||||
| Less than HS (Ref) | 228 | REF | 483 | REF |
| Completed HS/Voc | 122 | 1.85 (1.24, 2.76)* | 386 | 1.40 (0.95, 2.04) |
| At least some college | 131 | 2.19 (1.37, 3.48)* | 476 | 1.46 (1.08, 1.97)* |
| Immigrant Status | ||||
| Born in US | ||||
| Born in Puerto Rico (ref) | ||||
| Not born in US or PR | ||||
| English 1st Language | ||||
| Yes | 760 | 1.69 (1.17, 2.45)* | ||
| No (Ref) | 585 | REF | ||
| Race/Ethnicity | ||||
| Black | ||||
| Hispanic (Ref) | ||||
| White/Other | ||||
| Age | ||||
| <35 | 331 | 1.25 (0.88, 1.77) | ||
| 35–49 | 387 | 1.85 (1.42, 2.41)* | ||
| 50+ (ref) | 627 | REF | ||
| Employment Status | ||||
| Work full time/part time | 516 | 1.28 (1.10, 1.48)* | ||
| Disabled/not working (Ref) | 829 | REF | ||
| Health problems make it difficult to exercise | ||||
| Yes (Ref) | ||||
| No | ||||
| Social networks | ||||
| Below median split | 202 | 1.61 (1.06, 2.53)* | ||
| Median split or higher (Ref) | 279 | REF | ||
| Social Support | ||||
| Has all 5 | ||||
| Does not have all 5 | ||||
| Social cohesion | ||||
| Continuous | 481 | 1.64 (1.06, 2.53)* | 1345 | 1.71 (1.39, 2.10)* |
p ≤ .05
polytomous model odds ratios represent odds for the 2 relationships: feeling safe vs. a little unsafe and unsafe, and feeling a little unsafe vs. unsafe
We also tested specific interaction effects for our hypothesized moderators (age, ethnicity/race, health status, financial status, and employment status). None of these variables were found to moderate the association between perceptions of neighborhood safety and social cohesion or social networks for male residents.
Perceptions of Neighborhood Safety for Female Residents
Bivariate analyses on primary exposures and outcomes of interest for female residents (Table 2) indicated that those who had completed high school (p≤.01) or at least some college (p≤.001), or who were born in the U.S. (p≤.03), or whose first language was English (p≤.001) were significantly more likely to have higher levels of perceived safety than their counterparts. Female residents who were Black (p≤.001), between 35 and 49 years old (p≤.001), or working were significantly more likely to have higher perceived neighborhood safety compared to their counterparts. In addition, not having current health problems that made it difficult to exercise (p≤.01), having higher levels of social support (p≤.03), and higher perceived social cohesion (p≤.001) were statistically significant predictors of perceptions of neighborhood safety among women. Having larger social networks, however, was not associated with perceptions of greater neighborhood safety for female residents.
Table 3 displays the polytomous multivariable model of perceived neighborhood safety. As hypothesized, the overall association between social cohesion and perceptions of neighborhood safety remained significant (p≤0.001), controlling for education, English as a first language, age, employment status, and health problems that make it difficult to exercise. We did not find a main effect of social network or social support on perceptions of neighborhood safety. Educational level, English as a first language, age, and employment status also remained significant predictors of neighborhood safety in the multivariable models for female residents.
We also tested specific interaction effects to examine differences in potential moderators (age, ethnicity/race, health status, financial status, and employment status) of the association between perceptions of neighborhood safety and social cohesion, social support, and social networks, respectively. None of these variables were found to moderate the association between perceptions of neighborhood safety and social cohesion for female residents.
Discussion
Although there has been a growing interest in the relationship between people’s perceptions of specific characteristics of the social environment and their perceptions of safety, very few empirical studies have examined how perceptions of the social environment might impact perceptions of perceived neighborhood safety, especially among public housing residents. Our study contributes to the scientific literature in this area by providing some insight into the association between social environmental factors—social networks, social support, and social cohesion—and perceptions of neighborhood safety among low-income public housing residents as a potential pathway through which social environmental factors influence health. As hypothesized, residents who reported higher levels of social cohesion perceived their neighborhood as safer compared to residents who reported lower levels of social cohesion. This association fits previous empirical evidence linking social cohesion to neighborhood safety (eg, Kuo, Sullivan, Coley, & Brunson, 1998; Sampson & Raudenbush, 1999; Wen et al., 2007; Baum et al., 2009).
Given the extensive literature on gender-based differences in perceptions of safety and the fear of personal and property victimization (eg, Warr, 2000; Mesch, 2000; Pain, 2001; Scott, 2003; Lane & Meeker, 2003; Schafer, Huebner, & Bynum, 2006), it is not surprising that there were divergent findings for males and females in terms of effect of social networks on perceptions of safety. Contrary to our hypothesis, male residents with smaller social networks were more likely to feel safe than those with larger social networks. It is possible that the association between social networks and perceived safety does not follow a linear dose-response curve. Another possibility is that larger social networks may be characterized by more negative social norms, influences, and interpersonal interactions which contribute to increased perceptions of being unsafe. Indeed, there is evidence that demonstrates that social networks may not always serve positive functions (Berkman & Glass, 2000; Heaney & Israel, 2002). For female residents, our findings suggest that social networks did not contribute to perceived neighborhood safety, and that sociodemographic factors (eg, employment, education, and language) were more important. Female residents who had lower levels of education, were born outside the U.S., and who reported a language other than English as their first language were more likely to feel lower levels of safety compared to each of their counterparts. Our study findings suggest that public policy and health promotion efforts need to first address female residents who are less well-educated, not born in the U.S., and whose first language is not English. Although extant research has focused on explaining differences between, rather than within the genders, there is some evidence to suggest that minority women, and women with lower educational levels and lower incomes report greater levels of fear due to residential patterns and routine activities as well as actual or perceived social and physical vulnerabilities (McGarrell, Giacomazzi, & Thurman, 1997; Goodey, 1997; Austin, Furr, & Spine, 2002). Interestingly, health status was not a significant factor for either male or female residents. However, this finding may be reflective of the fact that we had a very limited measure of health status.
Social support in this study was not significantly associated with perceived neighborhood safety. Most participants in the study actually reported fairly high levels of social support and thus, the lack of variability could, in part, explain some of these non-significant results. Our measure assessed overall social support available through all aspects of one’s life, and not just that available in one’s neighborhood. Further research examining the role of neighborhood-specific characteristics of social support on perceptions of neighborhood safety is warranted. For example, does being able to count on neighbors for emotional, instrumental, and financial support when one needs it contribute to perceptions of safety for residents?
Study strengths and limitations
To our knowledge, this study was the first to examine the role of social networks, social support, and social cohesion in influencing public housing residents’ perceptions of neighborhood safety. This research was conducted among a large, random sample of diverse racial and ethnic, low-income male and female residents. Given that this study is cross-sectional however, causal interpretations can not be made, and future studies should evaluate these associations longitudinally. Study findings are only generalizable to low income public housing residents living in the Boston metropolitan area. Another limitation was that social networks were measured solely in terms of quantity of social ties (eg, number of close friends and relatives) and not quality of social ties. Because we were specifically interested in examining individual perceptions of safety we did not use objective measures of neighborhood safety (eg, crime statistics). Further research measuring both the perceived and objective environment is needed to assess the relative contribution of each construct to specific health behaviors and health outcomes. Finally, the response rate for this study was lower than hoped, but should be considered in the context of the challenges associated with conducting research in community settings. Given the 53% response rate, the sample may be potentially skewed in terms of representativeness of safety. However, other studies confirm that our sample is generally representative of public housing populations (ie, low-income, predominately racial/ethnic minority women) (Lewis, Raczynski, Heath, Levinson, & Cutter, 1993; Brunson, Kuo, & Sullivan, 2001; Peters, Levy, Rogers, Burge, & Spengler, 2007; Manzo, Kleit, & Couch, 2008).
The findings reported here are also useful in exploring a potential pathway through which social environmental factors influence health and suggest that an examination of residents’ perceptions of social networks, social cohesion, and social support is a helpful first step in untangling the complex set of variables that underpin perceptions of neighborhood safety. This paper suggests that social cohesion, in particular, may contribute to a greater sense of safety for residents, and potentially therefore health. Interventions therefore designed to improve health and well-being for low-income residents in public housing could usefully consider ways to promote a stronger sense of cohesion amongst residents.
Acknowledgments
We would like to profoundly thank the co-investigators of this study: Gary Bennett, Sapna Syngal, Robert Mayer, and Martha Zorn. We also gratefully acknowledge the efforts of the Open Doors to Health Research Team: Elise Dietrich, Elizabeth Gonzalez Suarez, Terri Greene, Lucia Leone, Mike Massagli, Vanessa Melamede, Maribel Melendez, Tamara Parent, Lina Rincón, Claudia Viega, Monifa Watson, Caitlin Gutheil, Zoe Bendixen, Roona Ray, Aidana Baldassrre, David Wilson, Ruth Lederman. Finally, we would also like to thank the resident helpers and resident service coordinators at collaborating housing sites.
Funding
This research was supported by grants 5R01CA098864-02, 1K22CA126992-01, and K05 CA124415 from the National Cancer Institute, and support to the Dana-Farber Cancer Institute by Liberty Mutual, National Grid, the Patterson Fellowship, and the Yerby Fellowship Program.
Contributor Information
Maria De Jesus, Center for Community-Based Research, Dana-Farber Cancer Institute, Boston, MA, Department of Society, Human Development, and Health, Harvard School of Public Health, Boston, MA.
Elaine Puleo, Department of Public Health, Division of Biostatistics and Epidemiology, University of Massachusetts, Amherst, MA.
Rachel C. Shelton, Department of Oncological Sciences, Division of Cancer Prevention & Control, Mount Sinai School of Medicine, New York, NY.
Karen M. Emmons, Center for Community-Based Research, Dana-Farber Cancer Institute, Boston, MA, Department of Society, Human Development, and Health, Harvard School of Public Health, Boston, MA.
References
- 1.Almedom A. Social capital and mental health: an interdisciplinary review of primary evidence. Social Science and Medicine. 2005;61:943–964. doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 2.Austin DM, Furr LA, Spine M. The effects of neighborhood conditions on perceptions of safety. Journal of Criminal Justice. 2002;30:417–427. [Google Scholar]
- 3.Barrera M, Sandler IN, Ramsey TB. Preliminary development of a scale of social support: studies on college students. American Journal of Community Psychology. 1981;58:304–309. [Google Scholar]
- 4.Baum FE, Ziersch AM, Zhang G, Osborne K. Do perceived neighbourhood cohesion and safety contribute to neighbourhood differences in health? Health & Place. 2009;15(4):925–934. doi: 10.1016/j.healthplace.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Bennett GG, McNeill LH, Wolin KY, Duncan DT, Puleo E, Emmons KM. Safe to walk? Neighborhood safety and physical activity among public housing residents. PLoS Med. 2007;4(10):1599–1606. doi: 10.1371/journal.pmed.0040306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology. 1979;109(2):186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 7.Berkman L, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- 8.Brunson L, Kuo FE, Sullivan WC. Resident appropriation of defensible space in public housing: Implications for safety and community. Environment and Behavior. 2001;33(5):626–652. [Google Scholar]
- 9.Campbell KE, Lee BA. Sources of personal neighbor networks: Social integration, need, or time? Social Forces. 1992;70(4):1077–1100. [Google Scholar]
- 10.Cattell V. Poor people, poor places and poor health: the mediating role of social networks and social capital. Social Science and Medicine. 2001;52:1501–1516. doi: 10.1016/s0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- 11.Chandola T. The fear of crime and area differences in health. Health & Place. 2001;7:105–116. doi: 10.1016/s1353-8292(01)00002-8. [DOI] [PubMed] [Google Scholar]
- 12.Chaskin RJ, Joseph ML. Building “community” in mixed-income developments: Assumptions, approaches, and early experiences. Urban Affairs Review. 2010;45:299–307. [Google Scholar]
- 13.Cohen S, Syme SL. Issues in the application and study of social support. In: Cohen S, Syme SL, editors. Social support and health. Orlando: Academic Press; 1985. [Google Scholar]
- 14.De Silva MJ, McKenzie K, Harpham T, Huttly SRA. Social capital and mental illness: a systematic review. Journal of Epidemiology and Community Health. 2005;59:619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellison-Loschmann L, Sunyer J, Plana E, Pearce N, Zock JP, et al. Socioeconomic status, asthma and chronic bronchitis in a large community-based study. European Respiratory Journal. 2007;29:897–905. doi: 10.1183/09031936.00101606. [DOI] [PubMed] [Google Scholar]
- 16.Goodey J. Boys don’t cry: Masculinities, fear of crime and fearlessness. British Journal of Criminology. 1997;37:401–418. [Google Scholar]
- 17.Heaney CA, Israel BA. Social networks and social support in health education. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: Theory, research and practice. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 18.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research and practice. San Francisco: Jossey-Bass; 2002. pp. 185–209. [Google Scholar]
- 19.HHS. Federal Registry. 2005. Annual Update of the HHS Poverty Guidelines; pp. 8373–8375. [Google Scholar]
- 20.Hurlbert JS, Beggs JJ, Haines VA. Social networks and social capital in extreme environments. In: Lin N, Cook K, Burt RS, editors. Social capital theory: Theory and research. New Jersey: Transaction Publishers; 2001. pp. 209–232. [Google Scholar]
- 21.Kawachi I, Berkman L. Social cohesion, social capital, and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 174–190. [Google Scholar]
- 22.King D. Neighborhood and individual factors in activity in older adults: results from the neighborhood and senior health study. Journal of Aging and Physical Activity. 2008;16:144–170. doi: 10.1123/japa.16.2.144. [DOI] [PubMed] [Google Scholar]
- 23.Kleit RG. Neighborhood relations in suburban scattered-site and clustered public housing. Journal of Urban Affairs. 2001;23(3–4):409–430. [Google Scholar]
- 24.Kuo FE, Sullivan WC, Coley RL, Brunson L. Fertile ground for community: Inner-city neighborhood common spaces. American Journal of Community Psychology. 1998;26(6):823–851. [Google Scholar]
- 25.Lane J, Meeker JW. Women’s and men’s fear of gang crimes: Sexual and nonsexual assault as perceptually contempo- raneous offenses. Justice Quarterly. 2003;20:337–371. [Google Scholar]
- 26.Lewis CE, Raczynski JM, Heath GW, Levinson R, Cutter GR. Physical activity of public housing residents in Birmingham, Alabama. American Journal of Public Health. 1993;83(7):1016–1020. doi: 10.2105/ajph.83.7.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lochner K, Kawachi I, Kennedy BP. Social Capital: A guide to its measurement. Health and Place. 1999;5(4):259–70. doi: 10.1016/s1353-8292(99)00016-7. [DOI] [PubMed] [Google Scholar]
- 28.Macintyre S, Ellaway A. Ecological approaches: Rediscovering the role of the physical and social environment. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. 332–348. [Google Scholar]
- 29.Manzo LC, Kleit RG, Couch D. “Moving three times is like having your house on fire once”: The experience of place and impending displacement among public housing residents. Urban Studies. 2008;45(9):1855–1878. [Google Scholar]
- 30.McCullagh P. Regression models for ordinal data. Journal of Research Statistics Society. 1980;42:109–142. [Google Scholar]
- 31.McGarrell EF, Giacomazzi AL, Thurman QC. Neighborhood disorder, integration, and the fear of crime. Justice Quarterly. 1997;14:479–497. [Google Scholar]
- 32.Mesch GS. Perceptions of risk, lifestyle activities, and fear of crime. Deviant Behavior. 2000;21:47–62. [Google Scholar]
- 33.Middleton J. Crime is a public health problem. Medicine, Conflict and Survival. 1998;14:24–28. doi: 10.1080/13623699808409369. [DOI] [PubMed] [Google Scholar]
- 34.Pain R. Gender, race, age, and fear of the city. Urban Studies. 2001;38:899–913. [Google Scholar]
- 35.Pebley A, Narayan S. RAND Working Paper. 2003. The Los Angeles Family and Neighborhood Survey: Household Questionnaires. [Google Scholar]
- 36.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD. Determinants of Allergen Concentrations in Apartments of Asthmatic Children Living in Public Housing. Journal of Urban Health. 2007;84(2):185–197. doi: 10.1007/s11524-006-9146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rountree P, Land K. Perceived risk versus fear of crime: Empirical evidence of conceptually distinct reactions in survey data. Social Forces. 1996;74:1353–1376. [Google Scholar]
- 38.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 39.Sampson R, Raudenbush SW. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology. 1999;105:603–651. [Google Scholar]
- 40.Sampson RJ. Neighborhood-level context and health: Lessons from sociology. In: Kawachi I, Berkman LF, editors. Neighborhoods and health. New York: Oxford University Press; 2003. pp. 132–146. [Google Scholar]
- 41.Schafer JA, Huebner BM, Bynum TS. Fear of crime and criminal victimization: Gender-based contrasts. Journal of Criminal Justice. 2006;34(3):285–301. [Google Scholar]
- 42.Scott H. Stranger danger: Explaining women’s fear of crime. Western Criminology Review. 2003;4:203–214. [Google Scholar]
- 43.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. Cary: SAS Institute Inc; 2000. [Google Scholar]
- 44.Tan H, Choo W, Archibald C, Esuvaranathan K. A community-based study of prostatic symptoms in Singapore. Journal of Urology. 1997;157(3):890– 893. [PubMed] [Google Scholar]
- 45.Warr M. Fear of crime in the United States: Avenues for research and policy. In: Duffee D, editor. Criminal justice: Measurement and analysis of crime and justice. Washington, DC: National Institute of Justice; 2000. pp. 451–490. [Google Scholar]
- 46.Wen M, Kandula NR, Lauderdale DS. Walking for transportation or leisure: What difference does the neighborhood make? Journal of General Internal Medicine. 2007;22(12):1674–1680. doi: 10.1007/s11606-007-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Young AF, Russell A, Powers JR. The sense of belonging to a neighbourhood: can it be measured and is it related to health and well being in older women? Social Science and Medicine. 2004;12:2627–2637. doi: 10.1016/j.socscimed.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 48.Ziersch AM, Baum FE, MacDougall C, Putland C. Neighborhood life and social capital: The implications for health. Social Science & Medicine. 2005;60(1):71–86. doi: 10.1016/j.socscimed.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 49.Ziersch A, Putland C, Palmer C, MacDougall C, Baum F. Neighborhood life, social capital and perceptions of safety in the Western suburbs of Adelaide. Australian Journal of Social Issues. 2007;42(4):550–562. [Google Scholar]