Abstract
Self-assembling peptide amphiphile (PA) nanofibers were used to encapsulate camptothecin (CPT), a naturally occurring hydrophobic chemotherapy agent, using a solvent evaporation technique. Encapsulation by PA nanofibers was found to improve the aqueous solubility of the CPT molecule by more than 50-fold. PAs self-assembled into nanofibers in the presence of CPT as demonstrated by transmission electron microscopy. Small-angle X-ray scattering results suggest a slight increase in diameter of the nanofiber to accommodate the hydrophobic cargo. In vitro studies using human breast cancer cells show an enhancement in antitumor activity of the CPT when encapsulated by the PA nanofibers. In addition, using a mouse orthotopic model of human breast cancer, treatment with PA nanofiber encapsulated CPT inhibited tumor growth. These results highlight the potential of this model PA system to be adapted for delivery of hydrophobic therapies to treat a variety of diseases including cancer.
Keywords: Peptide amphiphile, Self-assembly, Nanofiber, Drug delivery, Camptothecin, Cancer therapy
In the field of therapeutic delivery, a variety of natural and synthetic nanomaterials1–6 have been designed to incorporate bioactive components such as small molecules,7–9 oligonucleotides,9–11 and proteins9, 12–14 through non-covalent interactions. One strategy for non-covalently introducing therapeutic molecules into a system is to promote their physical encapsulation through hydrophobic collapse. Some pharmaceutical formulations, for example, use amphiphilic excipients, comprised of hydrophobic and hydrophilic blocks, to form micelles that solubilize hydrophobic drugs in aqueous environments, thus improving their bioavailability.6, 15–20
This concept of encapsulation by hydrophobic collapse has been explored in our laboratory using a unique class of peptide amphiphile (PA) molecules, which can self-assemble into high-aspect ratio cylindrical nanofibers.21, 22 Compared to other modes of nanostructure fabrication, self-assembly has the advantage of facile generation of multiplexed nanostructures incorporating different molecular building blocks. PA molecules are composed of a sequence of amino acids linked to naturally occurring fatty acids. The self-assembly of the PA nanostructure is strongly dependent on the choice of peptide headgroup.23 Assembly of PAs into filamentous nanostructures is based on a combination of hydrophobic collapse of the alkyl tails and hydrogen bonding in the β-sheet forming region.22 Aside from the inherent benefits of biocompatibility and biodegradability, the amino acid sequence of PAs can be modified to affect both the structural properties of the resulting nanofibers and their bioactivity. For example, PA nanostructures have been reported that display epitopes for specific receptors at concentrations that are easily controlled through co-assembly with non-bioactive molecules.24, 25 PAs have also been adapted for multiple biological applications including bone mineralization,26 spinal cord regeneration,27 angiogenesis,28 cartilage regeneration,29 and cancer therapy.30
Here, we examined the use of PA nanofibers for drug delivery with potential applications in cancer therapy. These nanostructures may be advantageous as cancer treatments through passive tumor targeting due to the enhanced permeability and retention (EPR) effect,31, 32 as well due to their shape, owing to enhanced bioavailability33 and improved cellular uptake exhibited by high aspect ratio particles.34, 35 In the current work, a model PA was studied, which consisted of a hydrophobic palmitic tail linked to an A4G3E3 sequence previously shown to self-assemble into the nanofiber morphology (Fig. 1A).36, 37 The negative formal charge is included in the PA to increase solubility in water.
Figure 1. Chemical structures.
(A) Chemical structure of the model “E3 PA” peptide amphiphile used in these experiments with sequence palmitoyl-A4G3E3. (B) Camptothecin in the active lactone form.
Camptothecin (CPT) was selected as the hydrophobic drug for encapsulation within the PA nanofiber (structure shown in Fig. 1B). Discovered in 1966, CPT is a naturally occurring quinoline alkaloid originally extracted from the bark and stem of Camptotheca acuminata, a tree found in China and Tibet.38 CPT induces cancer cell death by interfering with the actions of topoisomerase I, an essential enzyme in the DNA replication process.39 Use of CPT in the clinic has been hindered by low aqueous solubility and its rapid conversion to a less active carboxylate form under physiological conditions. In this work we demonstrated the ability of PA nanofibers to encapsulate and solubilize CPT, a challenging drug to formulate, and investigated the anticancer activity of the resulting nanostructures in vitro and in vivo using a murine model.
RESULTS AND DISCUSSION
PA encapsulation of CPT
Encapsulation of CPT into PA nanofibers was achieved using a solvent evaporation technique that has been reported to yield near quantitative levels of encapsulation.40, 41 In this method, both the hydrophobic molecule and the amphiphile were mixed in a mutually dissolving solvent, which was removed by evaporation to produce a film, and then reconstituted in an aqueous medium. Aside from DMSO, which would not be a good candidate for solvent evaporation due to its high boiling point, HFIP was also found to dissolve both CPT and the E3 PA. HFIP is well known for dissolving and disaggregating proteins, peptides and synthetic polyamides, since it is a strong H-bond donor.42–44 At concentrations of 10 mM and higher of the E3 PA, dissolving in HFIP required gentle heating and sonication; however, an optically clear solution was eventually achieved. CPT was found to dissolve readily in HFIP at concentrations higher than 10 mM. We postulated that using HFIP as a mutual solvent promoted disaggregation of the individual components of the system, thereby improving mixing before water-induced hydrophobic collapse. Furthermore, the solvent evaporation proved a more rapid approach than dialysis techniques, which typically take several days to prepare encapsulated products.
Using the solvent evaporation method to encapsulate CPT in the PA nanostructures did indeed lead to high encapsulation efficiencies (Fig. 2A). Encapsulation efficiencies were calculated by dividing the final concentration of encapsulated CPT by the original concentration of CPT added. When encapsulating a 0.5 mM initial concentration of CPT, an efficiency of 72% was observed for a 10 mM E3 PA solution. This CPT encapsulation efficiency is higher than literature examples where loading efficiencies of 46–60% have been reported in block copolymer micelle systems using dialysis methods.40, 45 When using the PA to encapsulate CPT, aqueous solubility values as high as 360 μM CPT were observed, which is more than 50-fold higher than the solubility reported for CPT alone in water (7 μM).46 Moreover, a near linear dependence on initial PA concentration was observed for the solubilization of CPT. A linear regression of the data estimates a molar ratio of 1:28 CPT to PA in the solubilized nanostructures. Fluorescence spectroscopy of PA-encapsulated CPT samples also suggests that the active lactone form of CPT is stabilized in the presence of PA even after two days under aqueous conditions. The spectrum of CPT in PA is blue shifted relative to CPT alone in water (Fig. 2B), which is consistent with the expected wavelength of the lactone (λmax = 432 nm) compared to the carboxylate (λmax = 446 nm) form.47, 48 Gradual release of the majority of CPT from PA nanofibers was observed over one week (Fig. 2C). The time required for CPT release was similar to other nanoparticle constructs as previously reported.49 This slow release limits the amount of free CPT present in circulation after systemic delivery, which could both reduce off-target systemic toxicity and allow for greater accumulation of the PA-encapsulated CPT in tumor tissue.
Figure 2. Peptide amphiphile nanofiber encapsulation of camptothecin.
(A) A plot of E3 PA-encapsulated CPT prepared by the solvent evaporation method versus the initial PA concentration used. The initial concentration of CPT was held constant at 0.5 mM. (B) Fluorescence spectra (360 nm excitation) of CPT encapsulated in E3 PA nanofibers. (C) CPT-encapsulated PA (5 mM) was dialyzed in PBS over 12 days. The amount of CPT released was measured using fluorescence of the dialysate, and normalized to the initial amount of CPT encapsulated by the PA.
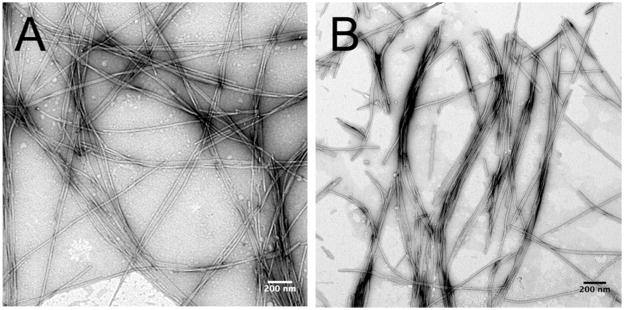
After encapsulating CPT into the PA nanofibers, we used conventional TEM to qualitatively study their individual morphology (Fig. 3). Average diameters of the fibers were measured to determine if incorporation of CPT induces swelling of the nanostructure. Average widths of 12.4 +/− 2.6 nm and 11.9 +/− 2.1 nm were observed for E3 PA alone and E3 PA with CPT, respectively. Therefore, fiber diameters did not appear to shift significantly in the presence of CPT, and the packing of the PA molecules into the cylinder shape was not hindered by the presence of the CPT molecule. A similar degree of fiber bundling was observed by TEM for both the PA alone and PA containing CPT.
Figure 3. Transmission electron microscopy.
(A) E3 PA nanofibers and (B) E3 PA-encapsulated CPT using the solvent evaporation method and reconstituted in PBS. There is no obvious change in fiber dimensions after CPT encapsulation. Bar = 200 nm.
We also studied nanofiber morphology by SAXS to characterize the shape and dimension of the nanostructures. The form factor of the 1-D scattering curve suggests the presence of long cylinders in solution, as evidenced by the -1 slope in the low-q range (Fig. 4A).50 Cross-sectional radii were determined using a modified Guinier analysis for cylindrical particles, which uses the slope of the plot of ln[qI(q)] vs. q2, where I(q) is the scattering intensity.51 The slope can be used to calculate the cross-sectional radius of gyration, RG,c, by the following equation: (RG,c)2 = −2 × slope. The value of RG,c is equal to R/21/2, where R is the actual radius of the cylinder. Slopes were determined in the linear portion of the low-q range (qRG,c < 1). The decrease in slope of the E3 PA with CPT compared to E3 PA alone showed a slight increase in radius when CPT was added to the fiber structure (Fig. 4B). From these slopes, the radius for E3 PA was calculated to be 5.1 ± 0.19 nm, and 5.5 ± 0.21 nm for E3 PA with CPT. Both microscopy and scattering confirmed that the general high aspect ratio morphology of the E3 PA nanofiber is undisturbed when loaded with drug. However, scattering experiments suggested that a small degree of swelling of the nanofibers might occur in order to accommodate a hydrophobic cargo.
Figure 4. Small angle X-ray scattering (SAXS) experiments.
(A) SAXS patterns show a cylindrical form factor, as indicated by the −1 slope at low q. Both the E3 PA and E3 PA with encapsulated CPT show a similar scattering pattern, suggesting that the CPT does not disrupt the nanostructure. (B) A modified Guinier plot shows a change in slope in the Guinier regime (qRg,c<1) after encapsulation of CPT.
In vitro activity of PA-encapsulated CPT
To investigate the antitumor activity of CPT encapsulated in E3 PA nanofibers, we treated BT-474, MCF-7, and SKBR-3 human breast cancer cells for 24 h with varying concentrations of CPT alone or loaded into E3 PA and measured cell viability using the CyQuant MTS assay (Fig. 5). E3 PA CPT was more cytotoxic than excipient CPT as reflected by lower IC50 values across all cell lines (Fig. 5). However, the increased cytotoxicity in vitro was in part due to the unexpected toxicity of the encapsulating E3 PA alone (Fig. 5). The observed cytotoxicity was surprising as a PA with the peptide sequence V3A3E3 (similar in charge to the A4G3E3 used here) has been shown to act as a nanofiber gel scaffold supporting cell adhesion and proliferation.52 We investigated the mechanism of E3 PA soluble nanofiber cytotoxicity in BT-474 cells. Treatment of BT-474 cells with 1.25 mM E3 PA did not promote apoptosis as measured by annexin V binding to externalized phosphatidylserine residues nor was cell toxicity rescued by pre-treatment of cells with the pan-caspase inhibitor Z-VAD-FMK (data not shown). To determine if the negatively charged E3 PA was membrane lytic as we have seen previously with cationic PAs,30 we performed flow cytometry-based time course experiments looking for plasma membrane permeability to the nuclear dye DAPI in response to E3 PA treatment. As opposed to 125 μM E3 PA treatment, cells exposed to 1.25 mM E3 PA rapidly become DAPI positive (Fig. 6A), leading to rapid cellular lysis (Fig. 6B), confirming the direct membrane lytic and cytotoxic action of these nanofibers at high concentrations.
Figure 5. E3 PA-encapsulated CPT is cytotoxic to breast cancer cells in vitro.
(A) BT-474, (B) MCF-7, and (C) SKBR-3 cells treated with CPT alone and CPT encapsulated in E3 PA nanofibers. Cell viability was measured by MTS assay (mean ± SEM, n=3). To compare the toxicity of E3 PA alone to the CPT encapsulated E3 PA, a CPT concentration based on a 1:62.5 molar ratio of CPT:E3 PA was used.
Figure 6. Soluble E3 PA is membrane lytic at high concentrations.
(A) BT-474 cells were treated with PBS, 20 μM or 200 μM E3 PA in the presence of DAPI. The percent of cells in the DAPI negative gate are shown over time. (B) BT-474 cellular concentration as measured as a ratio against time zero using fluorescent beads as an internal standard for each treatment group. Those cells that rapidly lose plasma membrane integrity are quickly lysed at the higher E3 PA concentration.
Collectively, these in vitro studies suggest that the CPT has enhanced antitumor potential when encapsulated in the PA. We hypothesize that these results are a combination of the effects of stabilization of the active lactone form of CPT in the hydrophobic core of the PA, and at high concentrations E3 PA contributes to toxicity as well. In future studies the unexpected in vitro toxicity of the E3 PA could be tempered with the addition of a polyethylene glycol chain to shield the negative charges, and hydrophobic cargo loading may be enhanced by using longer alkyl tails. PA nanofibers have been previously shown to become internalized by cells and metabolized through natural cellular processes,34 which may improve drug uptake in vivo. To test the in vivo behavior of encapsulated CPT we turned to a murine xenograft breast cancer model.
In vivo evaluation of antitumor activity
The antitumor activity of PA-encapsulated CPT nanostructures were investigated in vivo using a BT-474 orthotopic xenograft model of breast cancer in athymic nude mice (Fig. 7).53, 54 Four treatment groups were evaluated in the experiment, including (1) CPT encapsulated in PA; (2) a PA alone control; (3) a CPT control dissolved in a 7.5% excipient mixture in PBS v/v; and (4) a PBS vehicle control. The excipient mixture consisted of polyethylene glycol 400, propylene glycol and polysorbate 80 (40:58:2), which has been used previously in the literature to dissolve CPT for in vivo studies.55, 56 The excipient components are commonly used in oral and injectable drug-solubilizing formulations.57 Treatments were administered intravenously by tail vein injections, under the hypothesis that the EPR effect would enhance tumor uptake of the PA nanostructures. No statistically significant changes in weight of the mice were observed, suggesting that the treatments did not diminish their overall health (Fig. 7C).
Figure 7. E3 PA-encapsulated CPT inhibits breast cancer xenograft growth in vivo.
(A) Plot of BT-474 breast tumors as a function of time. (B) Tumor weights at the end of the experiment show significant decreases for mice that have been treated with CPT. (C) Relative mouse weight over time during the treatments. No significant differences were observed between groups. * p < 0.05, ** p < 0.01, *** p < 0.001.
Measurement of the tumors over three weeks of injections showed a marked reduction in tumor growth in the mice injected with CPT relative to controls (Fig. 7A). Any difference between the CPT in excipient formulation and the CPT encapsulated in PA however was difficult to discern quantitatively by tumor volumes or tumor weights (Figs. 7A and 7B). While the CPT encapsulated in PA nanofibers exhibited a significant anti-tumor effect compared to the PBS vehicle and PA alone, the result was similar to the CPT in the excipient mixture. One explanation for the similarities in anti-tumor activity between the PA and excipient mixture is the presence of polysorbate 80, a nonionic surfactant, which could potentially sequester CPT into micelles.58 Furthermore, it was also observed that nanoscale particles of CPT were observed to form in the excipient mixture, which, like the PA nanofibers, may be passively taken up in the tumors due to the EPR effect. Nonetheless, the PA nanofiber-encapsulated CPT demonstrated anti-tumor activity in vivo and shows promise for future therapies as further improvements are introduced in this platform of fully biodegradable nanostructures. One of the possibilities with these nanostructures is to integrate the therapeutic cargo with the use of PA molecules containing cytotoxic30 or pro-apoptotic peptides as well as peptides that can target tumors.
CONCLUSIONS
We have demonstrated that peptide amphiphile nanofibers can be used to encapsulate the hydrophobic drug camptothecin in its biologically active lactone form. The method described yielded high encapsulation efficiencies and would be amenable to encapsulation of other molecules. We also demonstrated high efficacy for these systems in vitro and comparable efficacy in vivo compared to a positive control. These observations suggest great therapeutic potential could be achieved with these systems compared to conventional excipients by using peptide amphiphiles that display targeting and cytotoxic or pro-apoptotic amino acid sequences. These bioactive and biodegradable constructs could increase cellular uptake and anticancer activity once the nanostructure extravasates into the tumor interstitium. These future directions are currently being explored in our laboratory.
MATERIALS AND METHODS
PA synthesis
Synthesis of the E3 PA was performed using standard Fmoc solid phase peptide synthesis protocols on a CS Bio CS136XT automated peptide synthesizer as previously described37. All fluorenylmethoxycarbonyl (Fmoc) protected amino acids, Fmoc-Glu(OtBu)-Wang resin and 2-(1H-benzotriazole-1-yl)-1,1,3,3-tetramethyluronium hexafluorophosphate (HBTU) were purchased from Novabiochem.
PA molecules were purified by reverse-phase HPLC using a Varian Prostar HPLC system and an X-bridge C-18 30×250 mm column. The mobile phase consisted of a water/acetonitrile (0.1% NH4OH) or water/methanol (0.1% NH4OH) gradient with a 25 mL/min flow rate. The desired HPLC fractions were combined, volatile organics were removed by rotary evaporation and water was removed via lyophilization. Analytical HPLC (Varian, Phenomenex column) was performed to assess purity using a similar water/acetonitrile (0.1% NH4OH) mobile phase with a flow rate of 0.7 mL/min. Electrospray ionization mass spectrometry (ESI) measurements were performed and observed masses corresponded with the desired product.
Preparation and Spectroscopic Characterization of CPT-loaded PA nanostructures
CPT was purchased from Sigma Aldrich and used without further chemical modification. Stock solutions of PA and CPT in HFIP (1,1,1,3,3,3-hexafluoro-2-propanol, 99.8+%, Sigma) were mixed together in a glass vessel and sonicated for 30 min in a 40 °C water bath. The vessel was then placed under vacuum with the cap loosened to allow evaporation of the solvent for a minimum of 2 h, which was sufficient to remove the HFIP. Aqueous media, such as purified water or PBS, was then added to the vessel and the vessel was placed in a 40 °C water bath for 30 min in order to dissolve the dried material. Then the aqueous mixture was vortexed for 1 min, transferred to a centrifuge tube and centrifuged at 1500 × g for 30 min to sediment undissolved CPT. The top 80% of the supernatant was then carefully removed and assayed for CPT concentration using a Molecular Devices microplate reader (Ex = 360 nm, Em = 450 nm). For storage, the remaining supernatant was then aliquoted, frozen in liquid nitrogen, and lyophilized. The dried material was stored at 4 °C or lower. Materials were reconstituted in aqueous media and mixed by vortex immediately prior to experiments. Assembly of nanofibers was observed by microscopy immediately after processing steps. Encapsulation efficiencies were calculated by dividing the concentration of encapsulated CPT by the initial concentration of CPT added and expressing the quotient as a percentage. CPT release studies were performed using a 1MWCO dialysis membrane (G-BioSciences). CPT-encapsulated PA (5 mM) was dissolved in PBS, added to a dialysis tube, and dialyzed in PBS over 12 days. The amount of CPT released was measured using fluorescence of the dialysate, and normalized to the initial amount of CPT encapsulated by the PA. As a control formulation for biological assays, including in vivo studies, CPT was deposited from HFIP and dried as above, then dissolved in an excipient mixture of polyethylene glycol 400, propylene glycol, and polysorbate 80 (40:58:2), as used in the literature.55, 56
Microscopy
Specimens for transmission electron microscopy (TEM) were prepared by drop-casting samples on carbon type B copper grids (Ted Pella) followed by staining with a 2% uranyl acetate aqueous solution. Images were taken using a JEOL 1230 transmission electron microscope operating at 100 keV equipped with a Hamamatsu ORCA camera.
Scattering experiments
Small angle X-ray scattering (SAXS) experiments were performed at the Advanced Photon Source, Argonne National Laboratory. The X-ray energy (15 keV) was selected using a double-crystal monochromator. The SAXS CCD camera was offset in order to achieve a wide range of scattering angles. Liquid samples were placed in 2.0 mm quartz capillary tubes. The typical incident X-ray flux on the sample was ~1×1012 photons/s with a 0.2×0.3 mm2 collimator, estimated by a He ion channel. Samples were irradiated for 5 s. The 1D scattering profiles were obtained by radial integration of the 2D patterns, with scattering from the capillaries subtracted as background. Scattering profiles were then plotted on a relative scale as a function of the scattering vector q = (4π/λ) sin(θ/2), where θ is the scattering angle.
Cell culture and reagents
The human breast cancer cell lines SKBR-3, MCF-7, and BT-474 were obtained from ATCC (Manasas, VA). Cell culture reagents were obtained from Invitrogen. SKBR-3 cells were grown in McCoy’s 5A media, supplemented with 10% fetal bovine serum and 100 IU/ml Penicillin-Streptomycin. MCF-7 cells were maintained in MEM media with Earles’ salts, 10% fetal bovine serum, 10 mM HEPES buffer, 2 mM L-glutamine, 0.1 mM non-essential amino acids, and 100 IU/ml Penicillin-Streptomycin. BT-474 cells were maintained in RPMI medium 1640 supplemented with 10% non-heat inactivated FBS, 1 mM sodium pyruvate, 10 mM HEPES buffer, 10 μg/ml insulin, 2 mM L-glutamine, 2 g/L glucose, and 100 IU/ml Penicillin-Streptomycin. All cells were grown at 37 °C in 5% CO2 atmosphere. 4′,6-Diamidino-2-phenylindole dihydrochloride (DAPI) was obtained from Sigma-Aldrich (St. Louis, MO).
Cell viability assays
Cell viability was measured using the CellTiter 96® Aqueous One Solution Cell Proliferation Assay (Promega, Madison WI). The Cell Titer Assay is a 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS)-based assay and was used as previously described according to the supplier’s instructions. For each well to be assayed in a 96-well plate containing 100 μl of media per well, 20 μl of the CellTiter96® Aqueous One Solution was added. The plate was incubated for 1–3 h at 37 °C, and absorbance was read using a Molecular Devices microplate reader (490 nm).
Flow cytometry assays
Either E3 PA or vehicle alone was added to BT-474 cells in suspension in the presence of 10 μg/mL DAPI. A time course of plasma membrane permeability and total cell concentration was determined by measuring fluorescence intensity at 25º C using a DakoCyomation CyAn.
Mouse orthotopic xenograft experiments
1 × 106 BT-474 human breast carcinoma cells were implanted subcutaneously (s.c.) into the 4th mammary fat pads of 4–5-week old female athymic nude mice (Harlan Sprague-Dawley, Madison, WI) to establish orthotopic xenograft tumors. Mice were additionally supplemented with 17β-estradiol applied s.c. in a 60-day release biodegradable carrier-binder (1.7 mg of estradiol per pellet) to promote xenograft tumor growth (Innovative Research of America). Four weeks after tumor implantation, mice were randomized into treatment groups (8 mice per group) and given 3 weeks of either PBS vehicle (Sigma-Aldrich), CPT 1.5 mg/kg/dose in an excipient formulation, CPT 1.5 mg/kg/dose encapsulated in 10 mM E3 PA, and a 10 mM E3 PA control by tail vein injection twice per week for six total injections. Tumors were measured after each injection with Vernier calipers, and tumor volume was calculated using the equation: tumor volume (mm3) = (length × width2) × π/6 as previously described.54
Acknowledgments
This work was supported by an NCI Center for Cancer Nanotechnology Excellence grant 1U54CA119341 (SIS and VLC); the Breast Cancer Research Foundation (VLC); Dixon Translational Research grant (VLC and SIS); Department of Defense Breast Cancer Research Program grant W81XWH-10-1-0503 (DJT); NIH grants 5F32GM080021 (SMS) and T32DK007169 (DJT); and a Graduate Research Fellowship from the National Science Foundation (TJM). Additional support was provided by the Northwestern University Flow Cytometry Facility and a Robert H. Lurie Comprehensive Cancer Center Support Grant (NCI CA060553). Transmission electron microscopy images were taken in the Biological Imaging Facility at Northwestern University. SAXS experiments were performed using the Advanced Photon Source DND-CAT beamline at Argonne National Laboratory. Use of the Advanced Photon Source at Argonne National Laboratory was supported by the U.S. Department of Energy under Contract No. DE-AC02-06CH11357. We thank Dr. Ronit Bitton, Dr. Honggang Cui, and Liam Palmer for helpful discussions.
References
- 1.Allen TM, Cullis PR. Drug Delivery Systems: Entering the Mainstream. Science. 2004;303:1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 2.Langer R. Biomaterials in Drug Delivery and Tissue Engineering: One Laboratory’s Experience. Acc Chem Res. 2000;33:94–101. doi: 10.1021/ar9800993. [DOI] [PubMed] [Google Scholar]
- 3.LaVan DA, Lynn DM, Langer R. Moving Smaller in Drug Discovery and Delivery. Nat Rev Drug Discovery. 2002;1:77–84. doi: 10.1038/nrd707. [DOI] [PubMed] [Google Scholar]
- 4.Lboutounne H, Faivre V, Falson F, Pirot F. Characterization of Transport of Chlorhexidine-Loaded Nanocapsules Through Hairless and Wistar Rat Skin. Skin Pharmacol Physiol. 2004;17:176–182. doi: 10.1159/000078820. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald MP, Spalding GC, Dholakia K. Microfluidic Sorting in an Optical Lattice. Nature. 2003;426:421–424. doi: 10.1038/nature02144. [DOI] [PubMed] [Google Scholar]
- 6.Pillai O, Panchagnula R. Polymers in Drug Delivery. Curr Opin Chem Biol. 2001;5:447–451. doi: 10.1016/s1367-5931(00)00227-1. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J, Ellsworth K, Ma PX. Hydrophobic Pharmaceuticals Mediated Self-Assembly of Beta-Cyclodextrin Containing Hydrophilic Copolymers: Novel Chemical Responsive Nano-Vehicles for Drug Delivery. J Control Release. 2010;145:116–123. doi: 10.1016/j.jconrel.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang W, Rong J, Wang Q, He X. The Encapsulation and Intracellular Delivery of Trehalose Using a Thermally Responsive Nanocapsule. Nanotechnology. 2009;20:275101. doi: 10.1088/0957-4484/20/27/275101. [DOI] [PubMed] [Google Scholar]
- 9.Rolland JP, Maynor BW, Euliss LE, Exner AE, Denison GM, DeSimone JM. Direct Fabrication and Harvesting of Monodisperse, Shape-Specific Nanobiomaterials. J Am Chem Soc. 2005;127:10096–10100. doi: 10.1021/ja051977c. [DOI] [PubMed] [Google Scholar]
- 10.Vinogradov SV, Batrakova EV, Kabanov AV. Nanogels for Oligonucleotide Delivery to the Brain. Bioconjugate Chem. 2004;15:50–60. doi: 10.1021/bc034164r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goh SL, Murthy N, Xu M, Fréchet JM. Cross-Linked Microparticles As Carriers For The Delivery of Plasmid DNA for Vaccine Development. Bioconjugate Chem. 2004;15:467–474. doi: 10.1021/bc034159n. [DOI] [PubMed] [Google Scholar]
- 12.Liu SQ, Yang YY, Liu XM, Tong YW. Preparation and Characterization of Temperature-Sensitive poly(N-isopropylacrylamide)-b-poly(d, l-lactide) Microspheres for Protein Delivery. Biomacromolecules. 2003;4:1784–1793. doi: 10.1021/bm034189t. [DOI] [PubMed] [Google Scholar]
- 13.Pongjanyakul T, Medlicott NJ, Tucker IG. Melted Glyceryl Palmitostearate (GPS) Pellets for Protein Delivery. Int J Pharm. 2004;271:53–62. doi: 10.1016/j.ijpharm.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 14.Vila A, Sanchez A, Janes K, Behrens I, Kissel T, Vila Jato JL, Alonso MJ. Low Molecular Weight Chitosan Nanoparticles as New Carriers for Nasal Vaccine Delivery in Mice. Eur J Pharm Biopharm. 2004;57:123–131. doi: 10.1016/j.ejpb.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Gupta U, Agashe HB, Asthana A, Jain NK. Dendrimers: Novel Polymeric Nanoarchitectures For Solubility Enhancement. Biomacromolecules. 2006;7:649–658. doi: 10.1021/bm050802s. [DOI] [PubMed] [Google Scholar]
- 16.Lee CC, MacKay JA, Frechet JM, Szoka FC. Designing Dendrimers for Biological Applications. Nat Biotechnol. 2005;23:1517–1526. doi: 10.1038/nbt1171. [DOI] [PubMed] [Google Scholar]
- 17.Liu XM, Pramoda KP, Yang YY, Chow SY, He C. Cholesteryl-Grafted Functional Amphiphilic Poly(N-isopropylacrylamide-co-N-hydroxylmethylacrylamide): Synthesis, Temperature-Sensitivity, Self-Assembly And Encapsulation of a Hydrophobic Agent. Biomaterials. 2004;25:2619–2628. doi: 10.1016/j.biomaterials.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 18.Morgan MT, Carnahan MA, Immoos CE, Ribeiro AA, Finkelstein S, Lee SJ, Grinstaff MW. Dendritic Molecular Capsules for Hydrophobic Compounds. J Am Chem Soc. 2003;125:15485–15489. doi: 10.1021/ja0347383. [DOI] [PubMed] [Google Scholar]
- 19.Rosler A, Vandermeulen GW, Klok HA. Advanced Drug Delivery Devices via Self-Assembly of Amphiphilic Block Copolymers. Adv Drug Delivery Rev. 2001;53:95–108. doi: 10.1016/s0169-409x(01)00222-8. [DOI] [PubMed] [Google Scholar]
- 20.Zupon MA, Fang SM, Christensen JM, Petersen RV. In Vivo Release of Norethindrone Coupled to a Biodegradable poly(alpha-amino acid) Drug Delivery System. J Pharm Sci. 1983;72:1323–1326. doi: 10.1002/jps.2600721121. [DOI] [PubMed] [Google Scholar]
- 21.Hartgerink JD, Beniash E, Stupp SI. Peptide-Amphiphile Nanofibers: A Versatile Scaffold for the Preparation of Self-Assembling Materials. Proc Natl Acad Sci U S A. 2002;99:5133–5138. doi: 10.1073/pnas.072699999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartgerink JD, Beniash E, Stupp SI. Self-Assembly and Mineralization of Peptide-Amphiphile Nanofibers. Science. 2001;294:1684–1688. doi: 10.1126/science.1063187. [DOI] [PubMed] [Google Scholar]
- 23.Trent A, Marullo R, Lin B, Black M, Tirrell M. Structural Properties of Soluble Peptide Amphiphile Micelles. Soft Matter. 2011;7:9572–9582. [Google Scholar]
- 24.Storrie H, Guler MO, Abu-Amara SN, Volberg T, Rao M, Geiger B, Stupp SI. Supramolecular Crafting of Cell Adhesion. Biomaterials. 2007;28:4608–4618. doi: 10.1016/j.biomaterials.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 25.Guler MO, Hsu L, Soukasene S, Harrington DA, Hulvat JF, Stupp SI. Presentation of RGDS Epitopes on Self-Assembled Nanofibers of Branched Peptide Amphiphiles. Biomacromolecules. 2006;7:1855–1863. doi: 10.1021/bm060161g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mata A, Geng Y, Henrikson KJ, Aparicio C, Stock SR, Satcher RL, Stupp SI. Bone Regeneration Mediated by Biomimetic Mineralization of a Nanofiber Matrix. Biomaterials. 2010;31:6004–6012. doi: 10.1016/j.biomaterials.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tysseling-Mattiace VM, Sahni V, Niece KL, Birch D, Czeisler C, Fehlings MG, Stupp SI, Kessler JA. Self-Assembling Nanofibers Inhibit Glial Scar Formation and Promote Axon Elongation After Spinal Cord Injury. J Neurosci. 2008;28:3814–3823. doi: 10.1523/JNEUROSCI.0143-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajangam K, Behanna HA, Hui MJ, Han X, Hulvat JF, Lomasney JW, Stupp SI. Heparin Binding Nanostructures to Promote Growth of Blood Vessels. Nano Lett. 2006;6:2086–2090. doi: 10.1021/nl0613555. [DOI] [PubMed] [Google Scholar]
- 29.Shah RN, Shah NA, Del Rosario Lim MM, Hsieh C, Nuber G, Stupp SI. Supramolecular Design of Self-Assembling Nanofibers for Cartilage Regeneration. Proc Natl Acad Sci U S A. 2010;107:3293–3298. doi: 10.1073/pnas.0906501107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Standley SM, Toft DJ, Cheng H, Soukasene S, Chen J, Raja SM, Band V, Band H, Cryns VL, Stupp SI. Induction of Cancer Cell Death by Self-Assembling Nanostructures Incorporating a Cytotoxic Peptide. Cancer Res. 2010;70:3020–3026. doi: 10.1158/0008-5472.CAN-09-3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matsumura Y, Maeda H. A New Concept for Macromolecular Therapeutics in Cancer Chemotherapy: Mechanism of Tumoritropic Accumulation of Proteins and the Antitumor Agent Smancs. Cancer Research. 1986;46:6387–6392. [PubMed] [Google Scholar]
- 32.Duncan R. The Dawning Era of Polymer Therapeutics. Nat Rev Drug Discovery. 2003;2:347–360. doi: 10.1038/nrd1088. [DOI] [PubMed] [Google Scholar]
- 33.Geng Y, Dalhaimer P, Cai S, Tsai R, Tewari M, Minko T, Discher DE. Shape Effects of Filaments Versus Spherical Particles in Flow and Drug Delivery. Nat Nanotechnol. 2007;2:249–255. doi: 10.1038/nnano.2007.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Beniash E, Hartgerink JD, Storrie H, Stendahl JC, Stupp SI. Self-Assembling Peptide Amphiphile Nanofiber Matrices for Cell Entrapment. Acta Biomater. 2005;1:387–397. doi: 10.1016/j.actbio.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 35.Gratton SE, Ropp PA, Pohlhaus PD, Luft JC, Madden VJ, Napier ME, DeSimone JM. The Effect of Particle Design on Cellular Internalization Pathways. Proc Natl Acad Sci U S A. 2008;105:11613–11618. doi: 10.1073/pnas.0801763105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee HK, Soukasene S, Jiang H, Zhang S, Feng W, Stupp SI. Light-Induced Self-Assembly of Nanofibers Inside Liposomes. Soft Matter. 2008;4:962–964. doi: 10.1039/b719486b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Niece KL, Czeisler C, Sahni V, Tysseling-Mattiace V, Pashuck ET, Kessler JA, Stupp SI. Modification of Gelation Kinetics in Bioactive Peptide Amphiphiles. Biomaterials. 2008;29:4501–4509. doi: 10.1016/j.biomaterials.2008.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wall ME, Wani MC, Cook CE, Palmer KH, Mephail AT, Sim GA. Plant antitumor agents. 1. The Isolation and Structure of Camptothecin, a Novel Alkaloidal Leukemia and Tumor Inhibitor from Camptotheca Acuminata. J Am Chem Soc. 1966;88:3888–3890. [Google Scholar]
- 39.Hsiang YH, Hertzberg R, Hecht S, Liu LF. Camptothecin Induces Protein-Linked DNA Breaks via Mammalian DNA Topoisomerase I. J Biol Chem. 1985;260:14873–14878. [PubMed] [Google Scholar]
- 40.Yokoyama M, Opanasopit P, Okano T, Kawano K, Maitani Y. Polymer Design and Incorporation Methods for Polymeric Micelle Carrier System Containing Water-Insoluble Anti-Cancer Agent Camptothecin. J Drug Target. 2004;12:373–384. doi: 10.1080/10611860412331285251. [DOI] [PubMed] [Google Scholar]
- 41.Lavasanifar A, Samuel J, Kwon GS. Micelles Self-Assembled from poly(ethylene oxide)-block-poly(N-hexyl stearate L-aspartamide) by a Solvent Evaporation Method: Effect on the Solubilization and Haemolytic Activity of Amphotericin B. J Control Release. 2001;77:155–160. doi: 10.1016/s0168-3659(01)00477-1. [DOI] [PubMed] [Google Scholar]
- 42.Crisma M, Saviano M, Moretto A, Broxterman QB, Kaptein B, Toniolo C. Peptide alpha/3(10)-Helix Dimorphism in the Crystal State. J Am Chem Soc. 2007;129:15471–15473. doi: 10.1021/ja076656a. [DOI] [PubMed] [Google Scholar]
- 43.Ha SW, Asakura T, Kishore R. Distinctive Influence of Two Hexafluoro Solvents on the Structural Stabilization of Bombyx Mori Silk Fibroin Protein and its Derived Peptides: 13C NMR and CD Studies. Biomacromolecules. 2006;7:18–23. doi: 10.1021/bm050783m. [DOI] [PubMed] [Google Scholar]
- 44.Sirangelo I, Dal Piaz F, Malmo C, Casillo M, Birolo L, Pucci P, Marino G, Irace G. Hexafluoroisopropanol and Acid Destabilized Forms of Apomyoglobin Exhibit Structural Differences. Biochemistry. 2003;42:312–319. doi: 10.1021/bi020447f. [DOI] [PubMed] [Google Scholar]
- 45.Opanasopit P, Yokoyama M, Watanabe M, Kawano K, Maitani Y, Okano T. Block Copolymer Design for Camptothecin Incorporation into Polymeric Micelles for Passive Tumor Targeting. Pharm Res. 2004;21:2001–2008. doi: 10.1023/b:pham.0000048190.53439.eb. [DOI] [PubMed] [Google Scholar]
- 46.Greenwald RB, Choe YH, McGuire J, Conover CD. Effective Drug Delivery by PEGylated Drug Conjugates. Adv Drug Delivery Rev. 2003;55:217–250. doi: 10.1016/s0169-409x(02)00180-1. [DOI] [PubMed] [Google Scholar]
- 47.Dey J, Warner IM. Spectroscopic and Photophysical Studies of the Anticancer Drug: Camptothecin. J Lumin. 1997;71:105–114. [Google Scholar]
- 48.Chourpa I, Millot JM, Sockalingum GD, Riou JF, Manfait M. Kinetics of Lactone Hydrolysis in Antitumor Drugs of Camptothecin Series as Studied by Fluorescence Spectroscopy. Biochim Biophys Acta, Gen Subj. 1998;1379:353–366. doi: 10.1016/s0304-4165(97)00115-3. [DOI] [PubMed] [Google Scholar]
- 49.Liu J, Jiang Z, Zhang S, Saltzman WM. Poly(œâ-pentadecalactone-co-butylene-co-succinate) Nanoparticles as Biodegradable Carriers for Camptothecin Delivery. Biomaterials. 2009;30:5707–5719. doi: 10.1016/j.biomaterials.2009.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glatter O, Kratky O. In: Small Angle X-Ray Scattering. Glatter O, Kratky O, editors. London ; New York: Academic Press; 1982. [Google Scholar]
- 51.Burkoth TS, Benzinger TLS, Urban V, Lynn DG, Meredith SC, Thiyagarajan P. COMMUNICATIONS TO THE EDITOR - Self-Assembly of Ab(10–35)-PEG Block Copolymer Fibrils. J Am Chem Soc. 1999;121:2. [Google Scholar]
- 52.Webber MJ, Tongers J, Renault MA, Roncalli JG, Losordo DW, Stupp SI. Development of Bioactive Peptide Amphiphiles for Therapeutic Cell Delivery. Acta Biomater. 2010;6:3–11. doi: 10.1016/j.actbio.2009.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kamradt MC, Lu M, Werner ME, Kwan T, Chen F, Strohecker A, Oshita S, Wilkinson JC, Yu C, Oliver PG, Duckett CS, Buchsbaum DJ, LoBuglio AF, Jordan VC, Cryns VL. The Small Heat Shock Protein Alpha B-Crystallin is a Novel Inhibitor of TRAIL-Induced Apoptosis that Suppresses the Activation of Caspase-3. J Biol Chem. 2005;280:11059–11066. doi: 10.1074/jbc.M413382200. [DOI] [PubMed] [Google Scholar]
- 54.Lu M, Kwan T, Yu C, Chen F, Freedman B, Schafer JM, Lee EJ, Jameson JL, Jordan VC, Cryns VL. Peroxisome Proliferator-Activated Receptor Gamma Agonists Promote TRAIL-Induced Apoptosis by Reducing Survivin Levels via Cyclin D3 Repression and Cell Cycle Arrest. J Biol Chem. 2005;280:6742–6751. doi: 10.1074/jbc.M411519200. [DOI] [PubMed] [Google Scholar]
- 55.Watanabe M, Kawano K, Toma K, Hattori Y, Maitani Y. In Vivo Antitumor Activity of Camptothecin Incorporated in Liposomes Formulated with an Artificial Lipid and Human Serum Albumin. J Control Release. 2008;127:231–238. doi: 10.1016/j.jconrel.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 56.Yang SC, Lu LF, Cai Y, Zhu JB, Liang BW, Yang CZ. Body Distribution in Mice of Intravenously Injected Camptothecin Solid Lipid Nanoparticles and Targeting Effect on Brain. J Control Release. 1999;59:299–307. doi: 10.1016/s0168-3659(99)00007-3. [DOI] [PubMed] [Google Scholar]
- 57.Katdare A, Chaubal MV. Excipient Development for Pharmaceutical, Biotechnology, and Drug Delivery Systems. Informa Healthcare; 2006. [Google Scholar]
- 58.Aizawa H. Morphology of Polysorbate 80 (Tween 80) Micelles in Aqueous 1,4-dioxane Solutions. J Appl Crystallogr. 2009;42:592–596. doi: 10.1107/S002188981000779X. [DOI] [PMC free article] [PubMed] [Google Scholar]