Abstract
Ozone is known to add across and cleave carbon–carbon double bonds. Ozonolysis is widely used for the preparation of pharmaceuticals, for bleaching substances and for killing microorganisms in air and water sources. Some polysaccharides and oligosaccharides, such as those prepared using chemical or enzymatic β-elimination, contain a site of unsaturation. We examined ozonolysis of low-molecular-weight heparins (LMWHs), enoxaparin and logiparin, and heparosan oligo- and polysaccharide for the removal of the nonreducing terminal unsaturated uronate residue. 1D 1H NMR showed that these ozone-treated polysaccharides retained the same structure as the starting polysaccharide, except that the C4–C5 double bond in the nonreducing end unsaturated uronate had been removed. The anticoagulant activity of the resulting product from enoxaparin and logiparin was comparable to that of the starting material. These results demonstrate that ozonolysis is an important tool for the removal of unsaturated uronate residues from LMWHs and heparosan without modification of the core polysaccharide structure or diminution of anticoagulant activity. This reaction also has potential applications in the chemoenzymatic synthesis of bioengineered heparin from Escherichia coli-derived K5 heparosan.
Keywords: heparosan, low-molecular-weight heparin, ozone, beta elimination, unsaturated uronic acid
1. Introduction
Heparin is a glycosaminoglycan composed of O-sulfo and N-acetyl or N-sulfo (1→4)- linked glucosamine and uronic acid residues. While heparin exhibits undesirable side effects such as hemorrhagic complications and heparin-induced thrombocytopenia, it is still in widespread clinical use.1,2,3 Low-molecular-weight heparins (LMWHs) have been introduced as heparin substitutes with reduced side effects, more predictable pharmacological action, sustained antithrombotic activity, and better bioavailability.3,4,5 LMWH is prepared from heparin by one of the following methods: treatment with nitrous acid, cleavage with enzyme heparinase, oxidative cleavage with hydrogen peroxide, or benzylation followed by alkaline depolymerization.6,7,8,9,10 The resulting LMWHs often have modified saccharide residues, such as a C4–C5 double bond in the uronate residue at the nonreducing end (cleavage with heparin lyase I or benzylation followed by alkaline depolymerization) or anhydromannose at the reducing end (nitrous acid depolymerization).6,9,10,11
Escherichia coli-derived K5 heparosan is a capsular polysaccharide, comprised of a [→4)β-D-glucuronic acid (GlcA) (1 →4) N-acetyl-α-D-glucosamine (GlcNAc) (1 →].12 K5 heparosan is a bacterial capsular polysaccharide that acts as a molecular camouflage muting immune response because of its structural similarity to heparosan, the biosynthetic precursor of heparin and heparan sulfate.13 Portions of the heparosan polysaccharide can be shed from E. coli K5 through the action of K5 heparosan lyase, an enzyme originating from bacterial phage that cleaves the heparosan chain through a β-elimination mechanism.14 In response to the heparin contamination crisis of 2008,15 we have begun to chemoenzymatically synthesize a bioengineered heparin by following the heparin biosynthetic pathway using recombinant biosynthetic enzymes.16 Starting from E. coli K5 heparosan, two chemical steps and four enzymatic steps led our group to prepare a bioengineered heparin.17 However, the resulting heparin contained a double bond in the C4 and C5 position of the uronic acid (ΔUA) moiety in the nonreducing end associated with the action of K5 lyase on the heparosan starting material. In the current study, ozonolysis is examined as a method to remove ΔUA residues from heparosan and LMWHs. Ozone also offers an added advantage of decolorizing or bleaching the sample and removing endotoxins. Mercuric acetate treatment is currently used to remove the ΔUA nonreducing residue from polysaccharides after treatment with polysaccharide lyases.18 Unfortunately, mercuric salts are highly toxic and are generally not used in the preparation of pharmaceutical products.
Ozonolysis is the cleavage of an alkene or alkyne with ozone to form organic compounds in which the multiple carbon–carbon has been replaced by a double bond to oxygen. Ozonolysis is widely used for the preparation of pharmaceuticals, and many other commercially useful organic compounds where it is used to sever carbon–carbon double bonds.19 Hyaluronic acid oligosaccharides prepared using polysaccharide lyase were treated with ozone to confirm the presence of a double bond in the C4 and C5 position of the uronic acid moiety.20 However, this paper failed to characterize the resulting oligosaccharide product, making it unclear whether ozone had damaged other saccharide units in addition to the ΔUA residue. Moreover, it was also unclear whether ozonolysis would be effective in the case of a sulfated polysaccharide or result in the loss of N-sulfo or O-sulfo groups from the treated polysaccharide or oligosaccharide. Thus, we examined ozonolysis for the removal of unsaturated modified sugar residues. As a model compound, an unsaturated heparosan hexasaccharide was treated with ozone. Once we confirmed that the unsaturated uronate residue was successfully cleaved to form a heparosan pentasaccharide, we performed ozonolysis on enoxaparin, logiparin, and microbial heparosan.
2. Results and discussion
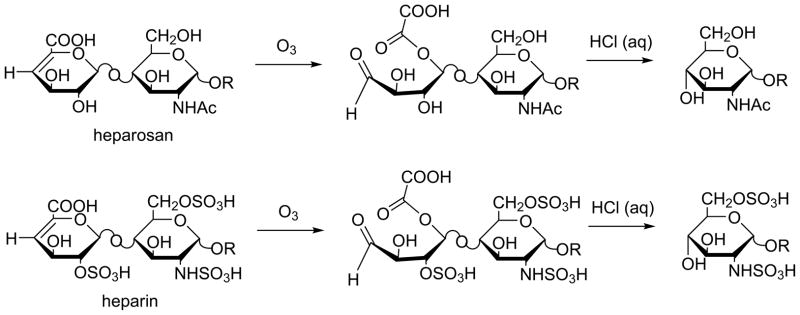
The proposed mechanism of ozonolysis of heparosan and heparin is shown in Scheme 1. Ozone cleaves the carbon–carbon double bond of the unsaturated uronate residue present at the nonreducing end. The glycosidic bond is cleaved upon acidic work-up, releasing the polysaccharide as an alcohol.
Scheme 1.
Removal of the unsaturated uronic acid residue of heparin and heparosan by ozonolysis. In heparosan R = [→4)-β-D-GlcA(1→4)- α-D-GlcNAc(1→]n4)- β-D-GlcA(1→4)- α, β-D-GlcNAc. In heparin R = → [→4)- α-L-IdoA ± 2S(or β-D-GlcA)(1 →4)- α-D-GlcNS±6Sand/or±3S(or GlcAc±6S)(1 → ]n 4)- α-L-IdoA±2S(or β-D-GlcA)(1→4)-α/β-D-GlcNS±6Sand/or±3S(or GlcAc±6S).
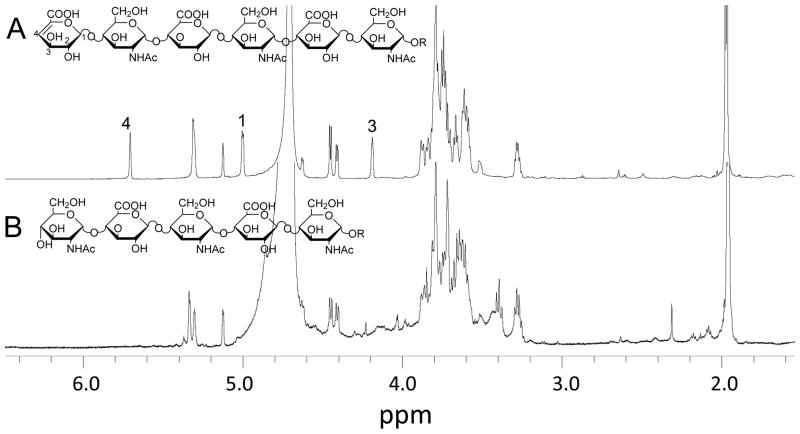
A heparosan-derived hexasaccharide was used as a model compound to carry out ozonolysis. Ozone was bubbled through an aqueous solution of the hexasaccharide for 5 min and worked up with acid. The resulting product was analyzed by 1D 1H NMR spectroscopy. Fig. 1A shows the NMR spectrum of the original hexasaccharide containing the unsaturated uronic acid residue at the nonreducing end. The numbers correspond to the position of the protons of the uronate moiety. Fig. 1B shows the NMR spectrum of the pentasaccharide product obtained after ozonolysis. The signals that were indicated in Fig. 1A are not observed in the product, suggesting that the uronate moiety was successfully removed by ozonolysis. The structure of the heparosan pentasaccharide was further confirmed by low resolution ESI-MS, which showed [M+H]+ as m/z 980.32 (m/z calcd. 980.32).
Figure 1.
1H NMR spectra (600 MHz) of heparosan-derived oligosaccharides. A. Spectrum of heparosan hexasaccharide prepared by controlled heparin lyase III-catalyzed depolymerization of heparosan. B. Spectrum of heparosan pentasaccharide prepared by ozonolysis of heparosan hexasaccharide. Peaks labeled 1, 3 and 4 in A correspond to signals assigned to protons attached to carbons 1, 3 and 4 of the nonreducing terminal ΔUA residue.
Ozone was then bubbled through an aqueous solution of K5 heparosan polysaccharide for 5 min and worked up with acid. The resulting product was analyzed by 1D 1H NMR spectroscopy. Fig. 2A shows the NMR spectrum of the original K5 heparosan containing the unsaturated uronic acid residue at the nonreducing end. The proton signal at ~5.8 ppm is indicative of the presence of an unsaturated uronic acid residue, corresponding to the C4 proton. Fig. 2B shows the NMR spectrum of the product obtained after ozonolysis. The characteristic signal of the double bond at ~5.8 ppm is no longer observed after ozone treatment, which suggests that the uronate moiety was successfully removed from K5 heparosan polysaccharide.
Figure 2.
1H NMR spectra (600 MHz) of heparosan polysaccharides. A. Spectrum of pure K5 heparosan polysaccharide. B. Spectrum of pure K5 heparosan polysaccharide following ozonolysis. Insert shows a peak at 5.785 ppm present in spectrum A but absent after ozonolysis in spectrum B assigned to the proton at C4 in the ΔUA residue at the nonreducing terminals of the chain.
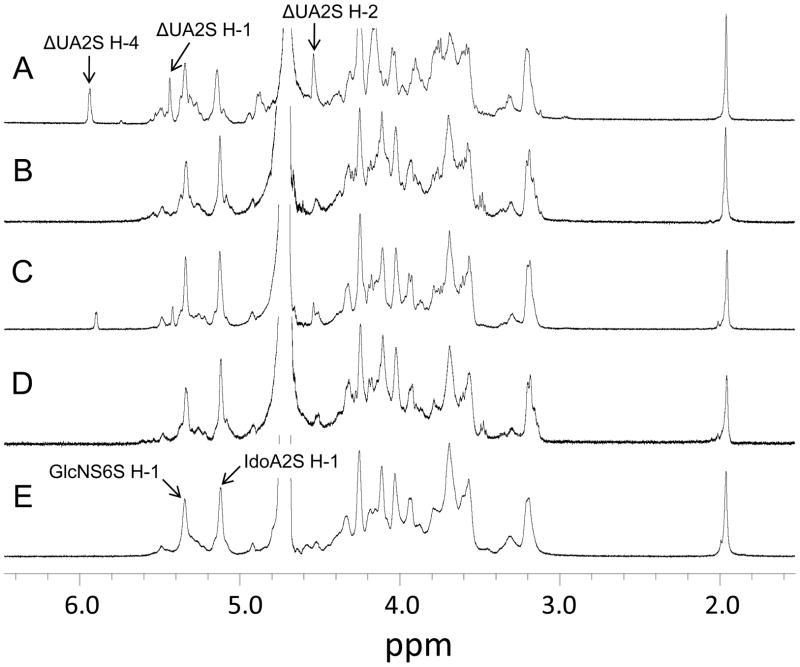
Ozone was bubbled through an aqueous solution of enoxaparin and logiparin for 5 min and worked up with acid. The resulting product was analyzed by 1D 1H NMR spectroscopy. Fig. 3A shows the NMR spectrum of the original enoxaparin containing the unsaturated uronic acid residue at the nonreducing end. The proton signals of H-1, H-2, and H-4 are indicated. Fig. 3B shows the NMR spectrum of the product obtained after ozonolysis. The characteristic signals are no longer observed after ozone treatment, which suggests that the uronate moiety was successfully removed from enoxaparin. Fig. 3C shows the NMR spectrum of the original logiparin containing the unsaturated uronic acid residue at the nonreducing end, which is confirmed by the three characteristic signals that were also seen in Fig. 3A. In Fig. 3D, these three peaks are not observed, which suggests that the uronate moiety was successfully removed from logiparin. In addition, the NMR spectra of ozonolyzed enoxaparin and logiparin are almost identical to that of sodium heparin (Celsus). The signals indicating the presence of GlcNS6S and IdoA2S, which are part of the pentasaccharide pattern required for heparin’s anti-Xa activity, are observed in each product. These data demonstrate that ozonolysis is an important tool for removing the unsaturated uronic acid residue from the nonreducing terminus of LMWHs without modification of the core structure.
Figure 3.
1H NMR spectra (600 MHz) of heparin and low-molecular-weight heparins and ozonolyzed low-molecular-weight heparins. A. Spectrum of enoxaparin; B. Spectrum of enoxaparin after ozonolysis; C. Spectrum of logiparin; D. Spectrum of logiparin after ozonolysis; E. Spectrum of heparin. Peaks indicated in spectrum A are associated with the ΔUA2S residue also found in spectrum C. Peaks labeled in E correspond to the anomeric protons of the major repeating units in heparin and are observed in all spectra.
The anticoagulation activity of enoxaparin and logiparin treated with or without ozone were examined (Table 1). The anti-factor Xa activity of ozonolyzed logiparin was comparable to that of untreated logiparin. In the case of enoxaparin, the product from ozonolysis showed higher anti-factor Xa activity than the untreated enoxaparin. These data suggest that there was no loss of sulfate groups and that the anticoagulant activity is retained after ozone treatment.
Table 1.
| Sample | Anti-factor Xa amidolytic activity (U/mg)a |
|---|---|
| Enoxaparin | 171± 3 |
| Ozonolyzed enoxaparin | 206 ± 4 |
| Logiparin | 114 ± 3 |
| Ozonolyzed logiparin | 111 ± 5 |
Std. dev. based on n = 3
3. Experimental
3.1 Chemicals
All chemicals were obtained from Sigma–Aldrich Chemical Co. (St. Louis, MO) except where otherwise stated. Oxygen was obtained from Airgas. Enoxaparin and logiparin were purchased from Sanofi Aventis (Paris, France) and Pfizer (New York, NY), respectively. Sodium heparin used for standard preparation was obtained from Celsus Laboratories (Cincinnati, OH).
3.2 Bacterial strains and culture conditions
The E. coli K5 from American Type Culture Collection (ATCC #23506) was grown in a 7 L fermentor. The fermentation consists of a batch growth stage and a fed batch growth stage. The composition of the medium for the batch growth in the fermentation was: 20 g/L glucose, 10 or 300 mg/L thiamine, 13.5 g KH2PO4; 4.0 g (NH4)2HPO4, 1.4 g MgSO4·7H2O, 1.7 g citric acid, and 10.0 mL trace metal solution. Trace metal solution consisted of (per L of 5 M HCl) 10.0 g FeSO4·7H2O, 2.0 g CaCl2, 2.2 g ZnSO4·7H2O, 0.5 g MnSO4·4H2O, 1.0 g CuSO4·5H2O, 0.1 g (NH4)6Mo7O24·4H2O, and 0.02 g Na2B4O7·10H2O. The feeding solution used in the fed batch stage consisted of (per L): 250–1000 g glucose, 20 g MgSO4·7H2O and 0.15 or 0.25 g thiamine. The pH was kept at pH ~7.0 throughout the fermentation.
The batch growth stage began with the inoculation of seed culture (300 mL of 5.6 g/L DCW) obtained from a shake flask in late exponential growth. The temperature was maintained at ~ 37 °C, and the pH was maintained at pH ~7 (by adding 29% ammonia solution). Air was sparged into the fermentor to supply oxygen, and the stirrer speed was set to 520 rpm.
The second stage of the fermentation began after glucose in the batch growth medium had been depleted and the dissolved oxygen showed a sharp increase. The feeding solution was then fed exponentially as described before. Fermentation supernatant was harvested by centrifugation (12,000g for 30 min) after no further increase in cell density was observed at 32 h.
3.3 Preparation of extracellular polysaccharide of E. coli K5
Fermentation supernatant (100 mL) was diluted two-fold using buffer A (50mM NaCl and 20 mM NaAcO, pH 4) and the pH was readjusted to 4. This diluted fermentation broth was then purified using DEAE-Sepharose fast-flow resin packed weak anion-exchange column. Heparosan (20 mg) was added to each 1 mL of DEAE resin (GE Healthcare Bio-Sciences Corp., NJ), which was equilibrated at pH 4 using 3 column volumes of buffer A. Diluted fermentation broth (200 mL containing 1 g of heparosan) was then loaded onto a 150-mL column under gravity flow conditions. The bound heparosan was eluted using 2 column volumes of buffer B (1 M NaCl and 20 mM NaAcO, pH 4). Absolute Ethanol (Fisher Scientific, PA)was added to the eluted sample in a 4:1 ratio by volume followed by incubation at 4 °C for 24 h in an explosion proof refrigerator. Heparosan was recovered in a pellet form using a Sorvall Evolution RC superspeed centrifuge at 2400g for 1 h. The recovered pellet was resolubilized using DI water and dialyzed against DI water using 3500 MWCO Spectra/por® Dialysis membranes (Spectrum Laboratories, Inc.) for 3 days. The retentate was concentrated using Buchi rotavapor R-200 and then lyophilized.
3.4 Generation of unsaturated uronic acid residues in heparosan
Heparosan hexasaccharide was prepared by a partial digestion of heparosan polysaccharide with heparin lyase III. Heparin lyase III (0.3 mU/mL) was added to a 1 mg/mL solution of heparosan, and digestion was allowed to proceed for 70 min at 35 °C and 150 rpm, or until UV absorbance at 232 nm indicated 50% digestion. Boiling for 20 min inactivated the enzyme. The sample was then centrifuged at 5,000g for 15 min. to remove any precipitate. Heparosan hexasaccharide was obtained by separation using a Bio-Gel P-10 (Bio-Rad, Hercules, CA, USA) column using aq 0.2 M NaCl as eluent. Fractions were detected by UV absorbance at 232 nm followed by desalting on a Bio-Gel P-2 (Bio-Rad, Hercules, CA, USA) column. The structure was confirmed by 1D 1H NMR (600 MHz) and low-resolution ESIMS.
3.5 Ozonolysis of heparosan, enoxaparin and logiparin
Samples were prepared for ozonolysis in water at 0.2 mg/mL, 1 mg/mL in the case of heparosan. Ozone, generated from a Welsbach model T-816 (El Sobrante, CA) apparatus set at 0.4 L/min (O2 at 21 °C) airflow and 70 V, was bubbled through the solution for up to 5 min. The reaction was worked up by adjusting the sample to pH 3 with aq 1 M HCl and heating for 30 min at 37 °C. The sample was adjusted to pH 7 with aq 10% NaOH. The sample was desalted by 3000 MWCO spin column (Millipore) and lyophilized.
3.6 NMR analysis
Ozonolyzed products were analyzed by 1D 1H NMR spectra. All NMR experiments were performed at 298 K on Bruker Avance II 600 MHz spectrometer with Topspin 2.0 software. Samples (0.5 mg to 1.0 mg) were each dissolved in 0.4 mL D2O (99.96%, Sigma–Aldrich Chemical Co.) and lyophilized three times to remove the exchangeable protons. The samples were redissolved in 0.4 mL D2O and transferred to NMR microtubes (OD 5 mm, Norrell). Experiments were performed with 32 scans and an acquisition time of 2.6 s.
3.7 Anticoagulation activity of enoxaparin and logiparin
Anti-factor Xa activity was measured using Test Team® Heparin S kit (Sekisui Medical, Tokyo, Japan). Reaction mixture 1 (0.2 mL), which contained 50 mM Tris HCl (pH 8.4), 20 μL of human plasma, 20 mU of ATIII and 50 ng of enoxaparin, ozonolyzed enoxaparin, logiparin, or ozonolyzed logiparin were incubated at 37 °C for 2 min. After incubation, reaction mixture 2 (0.3 mL), which contained 0.71 nkat of factor Xa and 150 μg of S-2222, was added and incubated for 30 s. The reaction was stopped with 300 μL of 8.33 M acetic acid and the absorbance was measured at 405 nm.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gervin AS. Surg Gynecol Obstet. 1975;140:789–796. [PubMed] [Google Scholar]
- 2.Freedman MD. J Clin Pharmacol. 1992;32:584–596. doi: 10.1002/j.1552-4604.1992.tb05765.x. [DOI] [PubMed] [Google Scholar]
- 3.Linhardt RJ. J Med Chem. 2003;46:2551–2554. doi: 10.1021/jm030176m. [DOI] [PubMed] [Google Scholar]
- 4.Green D, Hirsh J, Heit J, Prins M, Davidson B, Lensing AW. Pharmacol Rev. 1994;46:89–109. [PubMed] [Google Scholar]
- 5.Breddin HK, Fareed J, Bender N. Haemostasis. 1988;18:1–2. doi: 10.1159/000215865. [DOI] [PubMed] [Google Scholar]
- 6.Linhardt RJ, Gunay NJ. Semin Thromb Hemost. 1999;25:5–16. [PubMed] [Google Scholar]
- 7.Shivley JE, Conrad HE. Biochemistry. 1976;15:3932–3942. doi: 10.1021/bi00663a005. [DOI] [PubMed] [Google Scholar]
- 8.Fussi F. 4, 281, 108. U S Patent. 1981 July 28;
- 9.Mardiguian J. 4, 440, 926. US Patent. 1984 April 3;
- 10.Linhardt RJ, Grant A, Cooney CL, Langer R. J Biol Chem. 1982;257:7310–7313. [PubMed] [Google Scholar]
- 11.Linhardt RJ, Loganathan D, Al-Hakim A, Wang HM, Walenga JM, Hoppensteadt D, Fareed J. J Med Chem. 1990;33:1639–1645. doi: 10.1021/jm00168a017. [DOI] [PubMed] [Google Scholar]
- 12.Vann WF, Schmidt MA, Jann B, Jann K. Eur J Biochem. 1981;116:359–364. doi: 10.1111/j.1432-1033.1981.tb05343.x. [DOI] [PubMed] [Google Scholar]
- 13.Esko JD, Selleck SB. Annu Rev Biochem. 2002;71:435–471. doi: 10.1146/annurev.biochem.71.110601.135458. [DOI] [PubMed] [Google Scholar]
- 14.Hanfling P, Shashkov AS, Jann B, Jann K. J Bacteriol. 1996;178:4747–4750. doi: 10.1128/jb.178.15.4747-4750.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu H, Zhang Z, Linhardt RJ. Nat Prod Rep. 2009;26:313–321. doi: 10.1039/b819896a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linhardt RJ, Dordick JS, DeAngelis PL, Liu J. Semin Thromb Hemost. 2007;33:453–465. doi: 10.1055/s-2007-982076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Z, McCallum SA, Xie J, Nieto L, Corzana F, Jiménez–Barbero J, Chen M, Liu J, Linhardt RJ. J Am Chem Soc. 2008;130:12998–13007. doi: 10.1021/ja8026345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ludwigs U, Elgavish A, Esko JD, Meezan E, Rodén L. Biochem J. 1987;245:795–804. doi: 10.1042/bj2450795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Ornum SG, Champeau RM, Pariza R. Chem Rev. 2006;106:2990–3001. doi: 10.1021/cr040682z. [DOI] [PubMed] [Google Scholar]
- 20.Linker A, Meyer K, Hoffman P. J Biol Chem. 1955;219:13–25. [PubMed] [Google Scholar]
- 21.Wang FL, Lee SY. Biotechnol Bioeng. 1998;58:325–328. [PubMed] [Google Scholar]
- 22.Wang Z, Ly M, Zhang F, Zhong W, Suen A, Dordick JS, Linhardt RJ. Biotechnol Bioeng. 2010;107:968–977. doi: 10.1002/bit.22898. [DOI] [PMC free article] [PubMed] [Google Scholar]