Abstract
Gallstones are common and largely asymptomatic, but can result in significant morbidity in a small proportion of patients. Choledochal-enteric fistulation is one such complication with an associated mortality of 15–18%. The authors present a case of an 88-year-old man admitted to the general medical ward with an acute upper gastrointestinal bleed. Oesophagogastroduodenoscopy found a large gallstone impacted in the pylorus and CT scan revealed a choledochal-duodenal fistula. At laparotomy it was found that a 6.2 cm gallstone had fistulated into D1 and the pylorus and impacted there, causing outflow obstruction – Bouveret’s syndrome. A subtotal cholecystectomy was performed and the stone was removed by a separate gastrostomy. A radiological follow through study on day 14 showed contrast passing freely through the duodenum with no leak and the patient went on to make a slow, but uneventful recovery.
Background
Gallstones are common and largely asymptomatic, but can result in significant morbidity in a small proportion of patients. Choledochal-enteric fistulation is one such complication with an associated mortality of 15–18%.1 A large stone may fistulate into the colon or the duodenum in up to 3% of patients with chronic cholecystitis.2 A choledochal-duodenal fistula may result in a mechanical small bowel obstruction, the misnamed gallstone ileus. The most common site of obstruction is the narrow terminal ileum (50–75%) followed by the proxminal ileum and jejunum (20–40%). However, gallstones may impact and obstruct the duodenum itself producing gastric outflow obstruction (10%).3 This has been eponymously named Bouveret’s syndrome after the French internist who first described it in 1896.4 The following case describes a patient with Bourveret’s syndrome presenting unusually as an upper gastrointestinal bleed.
Case presentation
An 88-year-old man with a background of asymptomatic gallstones presented acutely with a 2 day history of gradually increasing centralised epigastric pain and a 1 day history of coffee ground vomit to the on call medical team in a district general hospital. He had no risk factors for gastric ulceration; he had no previous history of Helicobacter pylori infection, he was taking no medications which induce ulcers (for example no non-steroidal anti-inflammatory drugs, salicylates, steroids, anti-platelet agents and anticoagulants) and he was a non-smoker and rarely drank alcohol. His medical history included hypertension and previous transient ischaemic attacks, with no residual deficit but otherwise he was generally fit and well, independent requiring no additional help at home.
On admission, he looked unwell and was in obvious pain. He was tachycardic, but other observations remained stable. Clinical examination revealed only epigastric tenderness but no peritonitic features. Initial blood tests reveal haemoglobin 11.5 g/dl, haematocrit 0.349L/l, raised white cell count 22.4 x109/l, neutrophils 20.16 x109/l and C-reactive protein of 74 mg/l. Electrolytes showed normal sodium and potassium (140 mmol/l and 4.9 mmol/l respectively) but a raised urea of 15.4 mmol/l. Erect chest radiograph in the accident and emergency department revealed no free air under the diaphragm. Fluid resuscitation was administered and an urgent oesophagogastroduodenoscopy (OGD) arranged (Rockall score of three, with two being for age over 80).
Investigations
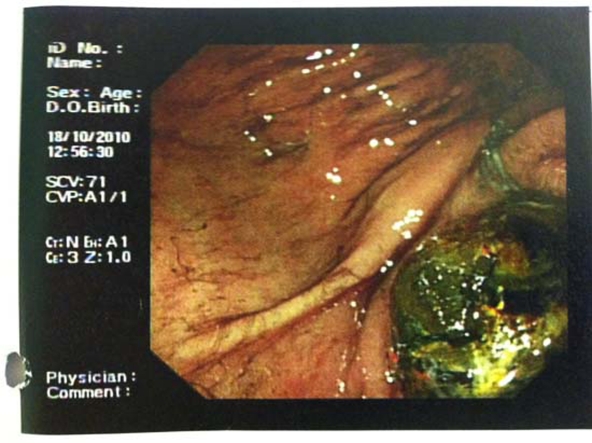
OGD found ‘coffee ground’ blood in the stomach but no ulceration. There was, however, a large mass occluding the pylorus which was initially thought to be a food bolus or clot. However, the obstructing lesion was so hard that the biopsy forceps would not bite into it, and just slipped off (figure 1). A very large gallstone was suspected and an urgent CT scan was ordered. This confirmed chronic cholecystitis with a choledochal-duodenal fistula involving D1 and the pylorus with a large, impacted gallstone causing the obstruction – Bouveret’s syndrome.
Figure 1.
Endoscopic view of the stone at OGD.
Differential diagnosis
Differential diagnosis at the time of presentation included gastric or duodenal ulceration or possibly a gastric carcinoma.
Treatment
After further resuscitation, laparotomy was undertaken which found a gallbladder empyema with a large fistula into D1 and the pylorus and a 6.2 cm by 3.7 cm gallstone causing outlet obstruction. A subtotal cholecystectomy was performed, the fistula was oversewn with no duodenal resection. The stone was removed by a separate gastrostomy (figures 2 and 3). A naso-jejunal tube was sited for postoperative feeding.
Figure 2.
At laparotomy; stone within the stomach, just prior to gastrostomy to remove stone.
Figure 3.
Large gallstone 6.2 cm by 3.7 cm retrieved from stomach at operation.
His postoperative recovery was slow but steady and without significant complication. A radiological follow through study on day 14 showed contrast passing freely through the duodenum with no leak. There was a mild narrowing at D1/D2 which was presumably due to inflammatory change.
Outcome and follow-up
He went on to make a full recovery and was discharged home. The histological analysis of the gallbladder revealed features of acute-on-chronic inflammation extending through the entire wall with reactive epithelial changes and abscess formation. Interestingly, there was widespread high grade dysplasia and a small focus of invasive adenocarcinoma extending into the lamina propria but not involving the muscle layer (pT1a). The fistula tract was not involved with the tumour, and therefore clear margins were achieved. There was no evidence of local or distant spread.
Discussion
Upper gastrointestinal bleeding is a very unusual presentation of gallstone disease. In this case it developed before any florid symptoms of gastric outlet obstruction could manifest themselves. Gallstone ileus is uncommon but usually presents as a distal small bowel obstruction.1 5 6 Gastric outlet obstruction due to impaction in the duodenum is rare with most cases being described in D1/D2. This case is even more unusual as the fistula involved the pylorus as well as D1.
Learning points.
-
▶
Upper gastrointestinal bleeding is a common presentation, but as this case illustrates, there are many causes. Urgent OGD will yield the most diagnostic information and in some cases may offer treatment options.
-
▶
Gallstones are common and mostly cause minimal symptoms. Occasionally they can cause significant pathology.
-
▶
Bouveret’s syndrome is a gastric outlet obstruction secondary to a gallstone impacted in the distal duodenum or at the pylorus.
-
▶
Early surgical intervention is indicated for gastric or intestinal obstruction due to a foreign body such as a gallstone.
-
▶
Cholecystectomy was undertaken in this case due to the concomitant empyema and high nature of the obstruction, however this is not usually indicated. In the more common pattern of distal small bowel obstruction, the gallbladder is best left undisturbed as the biliary dissection and fistula management may be very difficult due to the chronic cholecystitis resulting in significant morbidity.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg 1994;60:441–6 [PubMed] [Google Scholar]
- 2.Roslyn JJ, Thompson JE, Jr, Darvin H, et al. Risk factors for gallbladder perforation. Am J Gastroenterol 1987;82:636–40 [PubMed] [Google Scholar]
- 3.Clavien PA, Richon J, Burgan S, et al. Gallstone ileus. Br J Surg 1990;77:737–42 [DOI] [PubMed] [Google Scholar]
- 4.Bouveret L. Stenose de pyloroadherent a la vesicule calceuse. Rev Med 1896;16:1–16 [Google Scholar]
- 5.Rodríquez Hermosa JI, Codina Cazador A, Gironès Vilà J, et al. [Gallstone ileus: results of analysis of a series of 40 patients]. Gastroenterol Hepatol 2001;24:489–94 [PubMed] [Google Scholar]
- 6.Lowe AS, Stephenson S, Kay CL, et al. Duodenal obstruction by gallstones (Bouveret’s syndrome): a review of the literature. Endoscopy 2005;37:82–7 [DOI] [PubMed] [Google Scholar]