Abstract
INTRODUCTION
Breast cancer patients who have had prior axillary lymph node clearance (ALNC) can present with ipsi lateral hand conditions that could easily be treated with surgical intervention. These patients are often advised to avoid interventional procedures due to risks of complications such as lymphoedema, infection and cellulitis.
SUBJECTS AND METHODS
Between April and June 2009, we conducted an online survey of hand surgeons, breast surgeons and breast-care nurses to obtain their views on hand surgery after ipsilateral axillary lymph node clearance.
RESULTS
The majority of hand surgeons (58%) felt there was no contra-indication to surgery in a breast cancer patient with prior ipsilateral ALNC compared to just 30% of breast surgeons and 10% of breast-care nurses. The majority of breast surgeons and breast-care nurses (70% and 89%, respectively) felt that hand surgery was a relative contra-indication compared to just 41% of hand surgeons. Postoperative lymphoedema was the commonest cited reason for avoiding surgery. The majority of hand surgeons (79%) and nearly two-thirds of breast surgeons (57%) would use a tourniquet during surgery if it was normal practice.
CONCLUSIONS
A review of the published literature does not support the notion that these patients experience increased complications; therefore, we recommend the advice given to breast cancer patients regarding ipsilateral surgery be re-evaluated.
Keywords: Axillary lymph node dissection, Breast cancer, Elective hand surgery
Carpal tunnel syndrome, Dupuytren's contracture, trigger digit and basal thumb osteoarthritis are common hand conditions. A proportion of patients with symptomatic hand conditions will present to the hand surgeon having had prior breast cancer surgery with axillary lymph node clearance (ALNC). When offered surgical treatment for symptomatic hand conditions, these patients are often reluctant to proceed based on prior advice given to them. Lymphoedema is a recognised complication in patients who undergo breast cancer surgery with ALNC. The condition is difficult to treat and, therefore, the best treatment is prevention. Consequently, patients are often advised to avoid interventional procedures on the ipsilateral upper extremity such as venepuncture, intravenous catheterisation and tourniquet use for blood pressure measurement.1–7 However there is little in the literature to justify the view that these particular patients are at greater risk of developing such complications after hand surgery.
The aim of this study was to ascertain the current opinions of hand surgeons, breast surgeons and breast-care nurses on whether hand surgery should be undertaken in this particular group of patients. Furthermore, we wished to determine if a difference of opinion existed between these healthcare professionals.
Subjects and Methods
We conducted an online survey using a web-based survey tool (SurveyMonkey) comprising of three questions. Question 1 asked whether previous axillary lymph node clearance was felt to be an absolute, relative or no contra-indication to ipsilateral hand surgery in a symptomatic patient. Question 2 asked for the main reasons for avoiding surgery in these patients – postoperative lymphoedema, cellulitis or infection. Question 3 asked whether a tourniquet should be used if it was considered standard practice for a hand procedure.
An email containing a link to the online survey was distributed to consultant hand surgeons, consultant breast surgeons and breast-care nurses through their respective associations – British Society for Surgery of the Hand (BSSH), British Association of Surgical Oncologists (BASO) and Specialist Breast Care Nurses at the Royal College of Nursing (RCN).
The survey was conducted from 15 April 2009 until 1 June 2009 and was then closed to further submissions. All respondents had to complete the survey fully before submission was accepted. Statistical analysis was performed using the chi-squared test.
Results
A total of 339 responses were received during the survey period – 101 hand surgeons, 136 breast surgeons and 102 breast-care nurses.
The majority of hand surgeons (58%) felt prior ALNC was not a contra-indication to surgery compared to 30% of breast surgeons and 10% of breast care nurses (Fig. 1). This difference in opinion between hand surgeons and breast surgeons and also breast surgeons and breast-care nurses was statistically significant (P ≤ 0.001). The majority of breast surgeons and breast-care nurses (70% and 89%, respectively) felt prior ALNC was a relative contra-indication to hand surgery compared to only 41% of hand surgeons (P ≤ 0.005). Only two respondents (one hand surgeon and one breast-care nurse) felt that hand surgery was an absolute contra-indication after ALNC (Fig. 1).
Figure 1.
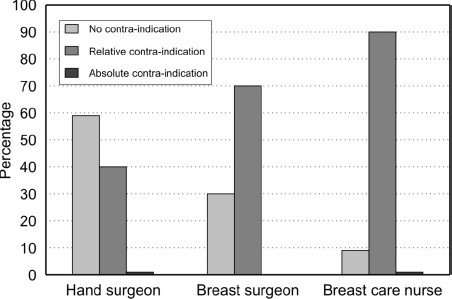
Opinion of hand surgeons, breast surgeons and breast-care nurses on hand surgery after axillary lymph node clearance.
The most commonly cited reason by hand surgeons, breast surgeons and breast-care nurses for avoiding surgery was the increased risk of postoperative lymphoedema (Fig. 2). Compared to hand surgeons, more breast surgeons and breast-care nurses felt risks of cellulitis and postoperative infection were reasons for avoiding surgery (Fig. 2).
Figure 2.
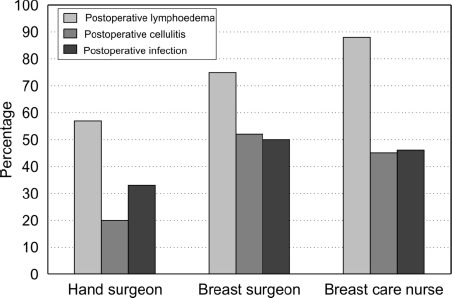
Cited reasons for avoiding surgery in patients with ipsilateral axillary lymph node clearance.
The majority of hand surgeons (79%) and nearly two-thirds of breast surgeons (57%) would use a tourniquet if this was considered standard practice, whilst the majority of breast-care nurses (68%) advised against the use of a tourniquet (Fig. 3).
Figure 3.
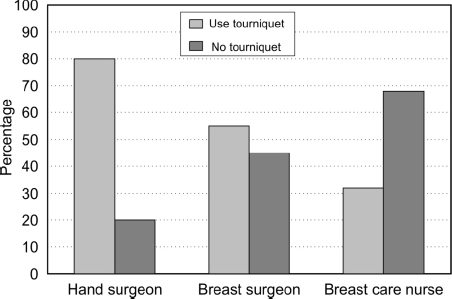
Opinion on tourniquet use on patients with ipsilateral axillary lymph node clearance.
Discussion
Symptomatic hand conditions can occur in patients who have had prior breast cancer surgery. There is evidence to suggest the risk of developing certain hand conditions such as carpal tunnel syndrome and trigger digit may actually be higher in patients after breast cancer surgery.1,3,7 In one study of 143 breast cancer patients, 10% developed carpal tunnel syndrome post breast surgery.3 Larson et al.8 reported that 28% of patients who had undergone breast surgery with ALNC developed carpal tunnel syndrome in their ipsilateral hand post surgery. The surgical management of these patients is considered problematic. The reasons for this are predominantly 2-fold. First, patients are often reluctant to undergo surgery because of prior advice given to them about interventional procedures on the ipsilateral arm. Second, from a surgical perspective, it is felt that surgery could lead to development of lymphoedema (or worsen pre-existing lymphoedema) and that patients are at greater risk of complications such as postoperative infection or wound-healing problems.1,3–7 This view is reflected to some degree in the results of our own survey (Fig. 2). The use of a tourniquet is believed to increase the risk of developing lymphoedema; therefore, precautions such as limiting tourniquet time or not using a tourniquet at all have been suggested.6 However, there is little in the published literature to support these concerns; indeed, the evidence suggests complications following ipsilateral elective hand surgery are no greater in patients with previous breast cancer surgery and ALNC than in those without.4–6,9
Dawson et al.4 reported on 15 patients who underwent carpal tunnel decompression after breast surgery and ipsilateral ALNC. Seven patients had pre-existing lymphoedema.4 All underwent surgery with a tourniquet and only one had pre-operative antibiotics. None of the 15 patients developed or displayed worsening of lymphoedema even at 16-month postoperative follow-up and there were no postoperative infections. Although a small study, Dawson et al.4 concluded that patients with prior ipsilateral axillary dissection could safely undergo elective upper limb surgery. Hershko and Stahl5 reported on 25 women (4 with pre-existing lymphoedema) who underwent surgery for various hand conditions including carpal tunnel syndrome, having had prior breast surgery with ALNC. All bar one underwent surgery with a tourniquet and none had pre-operative antibiotics. No new lymphoedema manifested at a minimum of 1 year follow-up and there were no reported postoperative infections. Of the four patients with pre-existing lymphoedema, two had temporary worsening of swelling which resolved within 3 months. They concluded there was no justification for prophylactic antibiotics or the routine use of general anaesthesia in these patients but suggested limiting tourniquet time to less than 1 h would be beneficial. Assmuss and Straub9 reported similar results in their study of 52 breast cancer patients undergoing carpal tunnel release, all performed with a tourniquet. Of the 49 patients with no preexisting lymphoedema, only four developed some postoperative swelling which resolved spontaneously by 3 months. In the three patients with pre-existing lymphoedema, two were unaffected by surgery and one had temporary worsening of symptoms. The published literature on hand surgery in these particular patients is sparse with only a handful of small studies and case reports.4,5,7,9 The reported results of hand surgery in these patients do not support the commonly perceived view that surgery carries a greater risk of developing lymphoedema or postoperative infection, particularly in those patients with no pre-exiting lymphoedema. In those with pre-existing lymphoedema, there may be a risk of worsening lymphoedema when a tourniquet is used but this is possibly a temporary phenomenon.
We have identified a clear difference of opinion exists between hand surgeons and breast surgeons in the UK regarding hand surgery after ALNC in the breast cancer patient. Nearly two-thirds of hand surgeons felt there was no contra-indication to surgery, whilst the majority of breast surgeons and breast-care nurses felt prior ALNC was a relative or absolute contra-indication to surgery. In addition, the majority of hand surgeons would still use a tourniquet if it were considered standard practice. The results of our survey are comparable to a similar study conducted amongst hand surgeons in the US.6 A survey of members of the American Society for Surgery of the Hand found 98% of hand surgeons would operate on a patient with prior ipsilateral ALNC and/or irradiation and that 94% would use a tourniquet if there was no pre-existing lymphoedema. In the presence of pre-existing lymphoedema, 84% of hand surgeons would still operate but 74% of surgeons would not use a tourniquet in these patients.
In view of this, we would suggest prior breast surgery with ALNC should not be considered a contra-indication to ipsilateral hand surgery, especially if there is no pre-existing lymphoedema. Where there are concerns about preexisting lymphoedema, procedures such as carpal tunnel decompression could safely be preformed using local anaesthetic with adrenaline, obviating the need for a tourniquet.10,11 Furthermore, the use of adrenaline in digital blocks has been shown to have no significant effect on digital blood flow, which could also be considered for digital procedures.12
Based on data provided by the respective societies, we calculated the response rates were 43% and 22% for hand surgeons and breast surgeons, respectively. We acknowledge that this could be considered a limitation of our survey and it could, therefore, be argued the results reflect the opinions of a ‘sample’ of healthcare professionals rather than the majority. An area for further research would be to conduct a patient-centred survey to determine what proportion of patients have symptomatic hand conditions and whether they have had or would undergo surgical treatment if offered. This would be with a view to identifying if advice given to patients regarding interventional procedures influences their decisions on surgery.
The evidence from the published literature suggests hand surgery can safely be performed on these patients even with a tourniquet with no increased risk of complications. Furthermore, the majority of hand surgeons both in the UK and US would offer surgery. Despite this, there is a clear difference of opinion in the UK between hand surgeons and breast surgeons and breast-care nurses. The advice given to patients by breast surgeons and nurses immediately following breast cancer surgery will notably affect patients' attitude regarding future ipsilateral interventional procedures. This advice will influence a patient's decision to seek, or agree to, treatment for a symptomatic hand condition. Based on the published evidence, advising patients to avoid surgery because of increased risk of complications may not be justified. We would recommend the advice given to breast cancer patients be re-evaluated in the hope that symptomatic patients feel comfortable seeking surgical treatment for common conditions that can significantly impact on quality of life and activities of daily living.
References
- 1.Ganel A, Engel J, Sela M, Brooks M. Nerve entrapments associated with post-mastectomy lymphedema. Cancer. 1979;44:2254–9. doi: 10.1002/1097-0142(197912)44:6<2254::aid-cncr2820440638>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 2.Breast Cancer Care UK. Reducing the risk of lymphoedema. How can I reduce my risk of developing lymphoedema. 2006:2. [Booklet] [Google Scholar]
- 3.Bozentka DJ, Beredjiklian PK, Chan PSH, Schmidt S, Buzby GP, Bora F. Hand related disorders following axillary dissection for breast cancer. Uni Pennsylvania Orthop J. 2001;14:35–7. [Google Scholar]
- 4.Dawson WJ, Elenz DR, Winchester DP, Feldman JL. Elective hand surgery in the breast cancer patient with prior ipsilateral axillary dissection. Ann Surg Oncol. 1995;2:132–7. doi: 10.1007/BF02303628. [DOI] [PubMed] [Google Scholar]
- 5.Hershko DD, Stahl S. Safety of elective hand surgery following axillary lymph node dissection for breast cancer. Breast J. 2007;13:287–90. doi: 10.1111/j.1524-4741.2007.00423.x. [DOI] [PubMed] [Google Scholar]
- 6.Gharbaoui IS, Netscher DT, Thornby J, Kessler F. Safety of upper extremity surgery after treatment for ipsilateral breast cancer: Results of an American Society For Surgery of the Hand membership survey and literature review. J Am Soc Surg Hand. 2005;5:232–8. [Google Scholar]
- 7.Donachy JE, Christian EL. Physical therapy intervention following surgical treatment of carpal tunnel syndrome in an individual with a history of postmastectomy lymphedema. Phys Ther. 2002;82:1009–16. [PubMed] [Google Scholar]
- 8.Larson D, Weinstein M, Goldberg I, Silver B, Recht A, Cady B, et al. Edema of the arm as a function of the extent of axillary surgery in patients with stage I–II carcinoma of the breast treated with primary radiotherapy. Int J Radiat Oncol Biol Phys. 1986;12:1575–82. doi: 10.1016/0360-3016(86)90280-4. [DOI] [PubMed] [Google Scholar]
- 9.Assmuss H, Staub F. Postmastectomy lymphoedema and carpal tunnel syndrome. Surgical advice and considerations for patients. Handchir Mikrochir Plast Chir. 2004;36:237–40. doi: 10.1055/s-2004-821060. [DOI] [PubMed] [Google Scholar]
- 10.Tzarnas CD. Carpal tunnel release without a tourniquet. J Hand Surg Am. 1993;18:1041–3. doi: 10.1016/0363-5023(93)90400-W. [DOI] [PubMed] [Google Scholar]
- 11.Braithwaite BD, Robinson GJ, Burge PD. Haemostasis during carpal tunnel release under local anaesthesia: a controlled comparison of a tourniquet and adrenaline infiltration. J Hand Surg Br. 1993;18:184–6. doi: 10.1016/0266-7681(93)90103-m. [DOI] [PubMed] [Google Scholar]
- 12.Sonmez A, Yaman M, Ersoy B, Numanodluj A. Digital blocks with and without adrenala randomised-controlled study of capillary blood parameters. Hand Surg Eur. 2008;33:515–8. doi: 10.1177/1753193408090143. [DOI] [PubMed] [Google Scholar]


