Abstract
INTRODUCTION
A major factor affecting patients’ length of hospitalisation following head and neck surgery remains the use of surgical drains. The optimal time to remove these drains has not been well defined. A routine practice is to measure the drainage every 24 h and remove the drain when daily drainage falls below 25 ml. This study aims to determine whether drainage measurement at shorter intervals decreases the time to drain removal and hence the length of in-patient stays.
PATIENTS AND METHODS
A 6-month prospective observational study was performed. The inclusion criteria were patients who
underwent head and neck surgery without neck dissection and had a closed suction drain inserted. Drainage rates were measured at 8-hourly intervals. Drains were removed when drainage-rate was ≤ 1 ml/h over an 8-h period.
RESULTS
A total of 43 patients were evaluated. The highest drainage rate occurred in the first 8 postoperative hours and decreased significantly in the subsequent hours. The median drainage rates at 8, 16, 24, 32 and 40 postoperative hours were 3.375, 1, 0, 0 and 0 ml/h, respectively. Applying our new removal criteria of ≤ 1 ml/h drainage rate, the drains were removed in 22 (51%) patients at the 16th postoperative hour; 37 (86%) were removed by 24 h after operation. In comparison, only nine (20.9%) patients could potentially be discharged the day after surgery if previous criteria of ≤ 25 ml/24-h were used to decide on drain removal.
CONCLUSIONS
Our 8-hourly drainage-rate monitoring has facilitated safe earlier discharge of an additional 28 (65%) patients on the day after surgery. This has led to improvement in patient care, better optimisation of hospital resources and resulted in positive economic implications to the department.
Keywords: Drainage, Postoperative care, Head and neck neoplasm, Patient discharge
Head and neck operations are associated with clinically significant postoperative morbidities such as haematoma, seroma, wound infection and skin flap complications.1,2 Surgeons often use closed drainage systems to reduce these complications. However, the use of drains is not without consequences – they require a high level of maintenance, cause discomfort, and serve as potential route for infection when drainage is prolonged. Therefore, early removal of drains or even eliminating the use of drains could reduce the period of a patient's hospitalisation and expedite recovery.3,4
Drain insertion is not a standard practice in all head and neck operations. Its use depends on individual cases as well as surgeons' experience and preference. However, in a patient with a neck drain in place, there are many associated nursing and care issues to be considered. Traditionally, the decision for drain removal is based on the total amount of drainage measured the morning after surgery. The drains are removed when the volume is ≤ 25 ml over a 24-h period (∼1 ml/h).5,6 In our experience, this measurement reflects drainage rates inaccurately. Factors such as the time of completion of surgery and expected accumulation of fluid in the dissected tissue spaces in the immediate postoperative period are not taken into consideration. The drains were usually left in situ for a further 24 h until their volumes were re-measured; thus, patients' period of hospitalisation tends to be prolonged further than necessary.
Anecdotally, most of drainage occurs in the early postoperative hours and decreases dramatically after this period. This study aimed to determine whether measurement at shorter intervals is a better basis for decisions on drain removal. We designed a prospective study measuring 8-hourly drainage rate in order to establish the optimum time for drain removal.
Patients and Methods
In the 6-month study period from December 2008 to June 2009, all patients who underwent head and neck surgery and had closed suction drains inserted were analysed. Those with neck dissections were excluded from the study to reduce confounding variables. The start of ‘postoperative hours’ is defined as the time when the patients return to ward from theatre. In all cases, the drain reservoirs were emptied and their volumes measured at 8-hourly intervals after the operation. Drains were removed once the drainage-rate was ≤ 1 ml/h over an 8-h period. Subsequent to drain removal, all patients were observed for any complications for a minimum of 2 h before discharge.
Results
We evaluated 43 patients. The operations performed consisted of 13 hemithyroidectomies, three total thyroidec-tomies, two total parotidectomies, nine superficial parotidectomies, nine excisions of neck mass and seven excisions of submandibular gland. The mean age of patients was 51 years (range, 24–83 years). The male to female ratio of the patients was 1.4:1 (Table 1).
Table 1.
Patient demographics
| Characteristic | n | % |
|---|---|---|
| No. of patients | 43 | |
| Male | 23 | 53 |
| Female | 20 | 47 |
| Mean age in years (range) | 51 (24–83) | |
| Types of surgery | ||
| Hemithyroidectomy | 13 | 30 |
| Total thyroidectomy | 3 | 7 |
| Total parotidectomy | 2 | 5 |
| Superficial parotidectomy | 9 | 21 |
| Excision neck mass | 9 | 21 |
| Excision submandibular gland | 7 | 16 |
The median of total amount of drainage the morning after surgery was 35 ml (range, 10–55 ml). The highest rate of drainage occurs in the first 8 postoperative hours (median, 3.3 ml/h) and the rates decreased significantly on subsequent 16, 24, 32 and 40 postoperative hours to median values of 1, 0, 0 and 0 ml/h respectively (Fig. 1).
Figure 1.
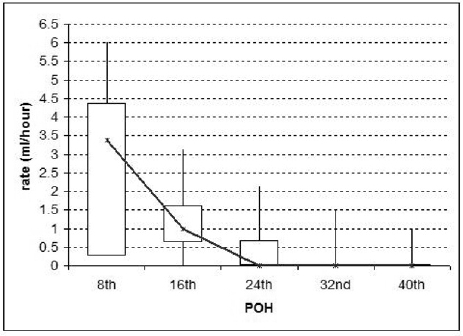
Rate of drainage as a function of postoperative hours.
By applying the new criteria for drain removal of ≤ 1 ml/h, drains were removed from 22 (51%) patients by the 16th postoperative hour and from 37 (86%) patients by the 24th postoperative hour. All patients had their drains removed by 40 h after operation. None of the patients discharged with the new criteria were re-admitted with complications (Table 2). One patient could have had the drain removed after the first 8th postoperative hour observation. However, as it was an unsocial and inconvenient time for the patient (in the middle of the night), the drain was removed at the 16th postoperative hour.
Table 2.
Rate of drainage and number of patients discharged according to postoperative hours
| Postoperative hour | |||||
|---|---|---|---|---|---|
| 8th | 16th | 24th | 32nd | 40th | |
| Patients (n) | 43 | 43 | 21 | 6 | 1 |
| Median drain-rate (ml) | 3.30 | 1.10 | 0.53 | 0.14 | 0.06 |
| 25–75 Quartiles | 0.25–4.375 | 0.625–1.625 | 0–0.687 | 0–0 | 0–0 |
| Range | 0.6–6 | 0–3.1 | 0–2.1 | 0–1.5 | 0–1 |
| Patients discharged with new criterion (≤ 1 ml/h) | 0 | 22 | 15 | 5 | 1 |
| Potential patients discharged with old criterion (≤ 25 ml/24-h) | 0 | 0 | 9 | 0 | 0 |
We found no significant difference in drainage rate between different types of operations (Table 3). Only three patients were on aspirin, which was withheld 5 days prior to surgery and resumed on discharge. Given this small number, the relationship between aspirin use and postoperative drainage could not be determined.
Table 3.
Median rate of drainage for different head and neck operations
| Postoperative hour | |||||
|---|---|---|---|---|---|
| 8th | 16th | 24th | 32nd | 40th | |
| Hemithyroidectomies (n = 16) | 2.750 | 0.625 | 0 | 0 | 0 |
| Total thyroidectomies (n = 3) | 5.000 | 1.000 | 0 | 0 | 0 |
| Superficial parotidectomies (n = 9) | 4.000 | 1.000 | 0.625 | 0 | 0 |
| Total parotidectomy (n = 2) | 4.875 | 1.000 | 0.312 | 0 | 0 |
| Excision of submandibular glands (n = 7) | 3.375 | 0.937 | 0 | 0 | 0 |
| Excisions of miscellaneous neck masses (n = 9) | 3.125 | 0.625 | 0 | 0 | 0 |
Discussion
The usual postoperative course in patients who had head and neck operations without neck dissection is uncomplicated and the duration of their in-patient stay is often dictated by the time the suction drains remain in place. Drains are often kept in situ until the daily drainage falls below 25 ml. Studies have shown that the average duration of drainage in uncomplicated head and neck operations is between 2–4 days.7–10 The presence of drains may in fact encourage further drainage by stimulating tissue reactions or by creating a suction effect.
It is always thought that the postoperative drainage after total thyroidectomy11 and parotidectomy12 would be higher and longer due to the presence of larger dead spaces. Therefore, it is interesting to note that our study shows the drainage rates of total thyroidectomy and parotidectomy to be higher than other types of operation in the first 8 postoperative hours, but no prolonged drainage or significant difference from other types of operations in the subsequent postoperative hours were observed. However, due to the small number of thyroidectomy and parotidectomy cases in this study, a definitive conclusion could not be drawn.
Although usage of drains may be considered standard postoperative care, little has been written in regards to the amount or duration of drainage. There are also considerable variations in practice with regards to drain monitoring and timing of removal. The usual practice in many departments is to measure the drain output the morning after surgery, usually at 8 a.m. the next day regardless of the time of completion of operation (which is some fraction of 24 h). Our study shows that, on average, the total volume of neck drainage in the morning after surgery is more than 25 ml in 79% of patients (median volume, 35 ml). Therefore, the drains would have to remain in situ for a further 24 h, thus delaying patients' discharge.
Williams et al.13 found that the amount of drainage that is collected in the drain reservoir is maximal in the first 24 h after insertion. Our study of 43 cases showed that the highest rate of drainage occurs in the first 8 h after operation and starts to decline significantly after this period. Therefore, it is more appropriate to measure drainage rate at shorter intervals of every 8 h to determine the optimum time for drain removal. We thus established a new drainage-rate criterion of ≤ 1 ml/h over 8-hourly intervals to decide on drain removal, based on the previously used criterion of 25 ml/24 h (i.e. ∼1 ml/h).
Using the new criterion above, we found that the majority of our patients (86%) had their drains removed and were discharged home by 24 h post-operation, with half discharged much earlier (51 % at the 16th postoperative hour). In contrast, only nine of the 43 patients (20.5%) could have been discharged on the first postoperative day if we had used the previous measurement criterion. None of the patients discharged with the new criterion developed any complications.
Conclusions
This study has demonstrated that the previous criterion for drain removal was not flexible enough to reflect the evolution of drainage rate in the subsequent postoperative hours.
Applying the new criterion of 8-hourly drainage rate monitoring has facilitated earlier and safe discharge in an additional 28 (65.1%) patients on the day after surgery.
Consequently, our department has continued to adopt the practice of 8-hourly measurement of drainage rates. We are also planning to introduce a protocol-based policy of nurse-led drain removal, which would enable the nursing staff to remove drains when the drainage rate is ≤ 1 ml/h and initiate discharge planning. These new practice and policy changes will lead to higher efficiency gained from better bed turnover and staff utilisation, improvement in morale through staff empowerment, and cost savings.
References
- 1.Byers RM, Ballantyne AJ, Goepfert H, Guillamondegui OM, Larson DL, Medina J. Clinical effects of closed suction drainage on wound healing in patients with head and neck cancer. Arch Otolaryngol. 1982;108:723–6. doi: 10.1001/archotol.1982.00790590045013. [DOI] [PubMed] [Google Scholar]
- 2.Wihlborg O, Bergljung L, Martensson H. To drain or not to drain in thyroid surgery. A controlled clinical study. Arch Surg. 1988;123:40–1. doi: 10.1001/archsurg.1988.01400250042007. [DOI] [PubMed] [Google Scholar]
- 3.Samraj K, Gurusamy KS. Wound drains following thyroid surgery. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD006099.pub2. Issue 4. CD006099. DOI: 10.1002/14651858.CD006099.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moffle PJ, Urquhart AC. Superficial parotidectomy and postoperative drainage. Clin Med Res. 2008;6:68–71. doi: 10.3121/cmr.2008.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoo J, Roth K, Hughes B, Fung K, Franklin J, et al. Evaluation of post-operative drainage with application of platelet-rich and platelet-poor plasma following hemithyroidectomy: a randomized controlled trial. Head Neck. 2008;30:1552–8. doi: 10.1002/hed.20900. [DOI] [PubMed] [Google Scholar]
- 6.Durai R, Mownah A, Ng PC. Use of drains in surgery: a review. J Perioper Pract. 2009;19:180–6. doi: 10.1177/175045890901900603. [DOI] [PubMed] [Google Scholar]
- 7.Willy C, Sterk J, Gengross H, Schmidt R. Drainage in soft tissue surgery. What is ‘evidence based’? Chirurg. 2003;74:108–14. doi: 10.1007/s00104-002-0581-7. [DOI] [PubMed] [Google Scholar]
- 8.Tabaqchali MA, Hanson JM, Proud G. Drains for thyroidectomy/ parathyroidectomy: fact or fiction? Ann R Coll Surg Engl. 1999;81:302–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Shaha AR, Jaffe BM. Selective use of drains in thyroid surgery. J Surg Oncol. 1993;52:241–3. doi: 10.1002/jso.2930520409. [DOI] [PubMed] [Google Scholar]
- 10.Conger BT, Gourin CG. Free abdominal fat transfer for reconstruction of the total parotidectomy defect. Laryngoscope. 2008;118:1186–90. doi: 10.1097/MLG.0b013e31816dd2e9. [DOI] [PubMed] [Google Scholar]
- 11.Lee SW, Choi EC, Lee YM, Lee JY, Kim SC, Koh YW. Is lack of placement of drains after thyroidectomy with central neck dissection safe? A prospective, randomized study. Laryngoscope. 2006;116:1632–5. doi: 10.1097/01.mlg.0000231314.86486.be. [DOI] [PubMed] [Google Scholar]
- 12.Sinha UK, Ng M. Surgery of the salivary glands. Otolaryngol Clin North Am. 1999;32:887–906. doi: 10.1016/s0030-6665(05)70180-8. [DOI] [PubMed] [Google Scholar]
- 13.Williams J, Toews D, Prince M. Survey of the use of suction drains in head and neck surgery and analysis of their biomechanical properties. J Otolaryngol. 2003;32:16–22. doi: 10.2310/7070.2003.35365. [DOI] [PubMed] [Google Scholar]


