Abstract
INTRODUCTION
Osteoarthritis of the trapeziometacarpal joint (TMJ) is a common condition causing significant disability. Conservative treatments include intra-articular steroid injections.
PATIENTS AND METHODS
This clinical, observational study prospectively reviewed the longevity of benefit of steroid injections into the TMJ. Eighty-three patients were recruited with a median age of 62 years and injected with steroid and local anaesthetic under radioscopic guidance. They were followed up until the analgesic effects ceased with a questionnaire including visual analogue scores.
RESULTS
Two-thirds of patients were improved at 2 months, with nearly half having a 3-month improvement. One in six patients had a 6-month benefit, with some patients still improved 2 years after injection. Previously injected patients had a reduced duration of benefit compared to their previous injection. Severity of osteoarthritis did not affect the injection efficacy.
CONCLUSIONS
Based on this study, we recommend steroid injections in all degrees of TMJ osteoarthritis.
Keywords: Osteoarthritis, Thumb, Carpometacarpal joints, Steroids, Intra-articular injections
Osteoarthritis of the trapeziometacarpal joint (TMJ) is a common condition causing significant disability. A range of non-operative and operative management options can be used for its treatment.1,2 One of the most common conservative treatments is a steroid injection into the joint, a technique employed for at least 40 years.3
The aim of intra-articular steroid injection is to ease pain by reducing inflammation. It is a commonly used treatment, even though its effectiveness is not well audited. The currently available literature has significant limitations, most notably having small numbers of patients.1,4-10 Steroid injection will only work if it is administered into the joint. Most previous publications do not specify or did not use the increased accuracy that fluoroscopic control allows. Failure to use fluoroscopic guidance may lead to a 42% risk of extra-articular injection.11
If local anaesthetic is used in addition to steroid, the site of pain can be accurately localised. This is helpful in patients with pantrapezial osteoarthritis or with other pathology in that area of the hand.
The injections can be painful and the amount and duration of pain relief is unpredictable.4-10 There is some evidence that patients with minimal arthritic changes on plain radiographs benefit more and for a longer duration compared to those with more severe arthritic changes.5,8 Potential complications include local depigmentation, fat atrophy or, very rarely, infection of the joint.
This clinical, observational study prospectively reviews the longevity of the benefit of steroid injections into the TMJ. All injections were given under fluoroscopic control to ensure accurate placement of the steroid. The clinical improvement was compared with the degree of radiological osteoarthritis.12 The aim of this study was to provide information that allows clinicians to predict potential improvement in specific subgroups of patients, hence avoiding unnecessary injections and providing a more cost-effective service.
Patients and Methods
All patients with TMJ osteoarthritis who were given an intra-articular injection of steroid (40 mg Triamcinolone) and local anaesthetic (either 1% Lidocaine or 0.5% Bupivicaine) in our out-patient clinic were considered for inclusion in the audit. The clinical decision to offer a patient an injection was completely independent of this audit. The correct placement of all steroid injections was confirmed with an image intensifier in clinic or the day-surgery ward (Fig. 1).
Figure 1.

X-ray image of needle within TMJ.
The primary outcome measure was a subjective perceived pain-relieving effect of the steroid. The secondary outcome measure was improvement measured with the ‘objective’, semi-quantitative visual analogue score (VAS). A 100-mm horizontal line allowed patients to rate their pain from ‘no pain’ (0) to ‘worst pain imaginable’ (100).
The patients were given an information sheet explaining the audit. An initial questionnaire with VAS scores before and during injection was completed. Patients were asked verbally and in writing to note how effective the injection was and how long it lasted. This was recorded by the patient on an assessment sheet they took home to record pain at 1 h and 1 week after injection. The patients were then sent an assessment sheet in the post at monthly intervals for completion and return. This ceased when the patient reported the effects of the steroid to have worn off, or the patient failed to return two consecutive monthly questionnaires (Fig. 2).
Figure 2.
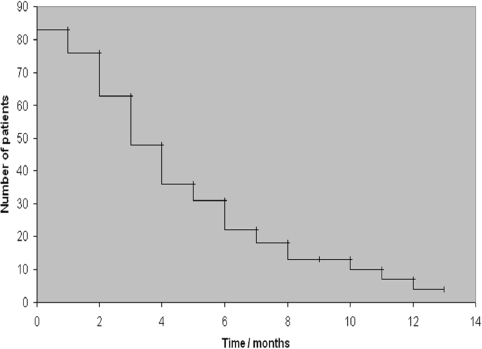
Kaplan–Meier plot of patient follow-up and end-point of the study.
The end-point for this audit was based on patient responses; i.e. when the injection had worn off and, therefore, when the pain in the base of the thumb had returned to its pre-injection level.
Patients had an up-to-date X-ray (anteroposterior and lateral) of the thumb in the two months prior to the management decision. Initial patient X-rays were reviewed. The degree of trapeziometacarpal osteo arthritis was classified prior to data analysis by the first author into one of four groups for each patient according to the Eaton classification.12 The average effect and duration of the steroid injection was calculated for each of the four grades of osteoarthritis (Table 1).
Table 1.
Perceived effectiveness versus Eaton et al.12 osteoarthritis grade
| Eaton grade | Description | Median perceived effectiveness (months) |
|---|---|---|
| 1 | Articular contours normal, joint space may be widened due to ligamentous laxity | 2 (n = 15) |
| 2 | Slight narrowing of TMJ, minimal sclerosis, osteophytes < 2 mm | 2.75 (n = 20) |
| 3 | TMJ narrowed, sclerosis, osteophytes > 2 mm | 2.25 (n = 14) |
| 4 | TMJ narrowed and sclerotic, scaphotrapezial joint also narrowed and sclerotic | 5.75 (n = 6) |
Eighty-three patients were recruited over a 3-year period between 1 October 2006 and 1 September 2009. Sixty were female. The left side was affected in 42 patients. The median age was 62 years (range, 41-93 years). The patients reported that the pain had been present for a median duration of 18 months (range, 2 months to 19 years).
Fifty-three patients had had no previous steroid injection into the joint; the other 25 had received one or more radio-logically guided injection before.
Twelve patients were lost to follow-up, all after completing VAS questionnaires up to 1 week. The other patients were all followed-up until they reported the pain had returned to pre-injection levels, i.e. the end-point for this study (Fig. 2).
Results
Subjective
Seventeen of the 83 patients did not report the duration of perceived effectiveness of the injection. Ten of the remaining 66 patients were still obtaining pain relief at 6 months. Thirty (about half) reported a benefit for three or more months. Forty-two patients (about two-thirds) reported a benefit for two or more months. Two patients reported no effect at all and two reported a duration of effect of 2 years. The median result for all patients was an effective duration of 2.5 months after injection (range, 0-24 months).
Objective
The median VAS immediately prior to the injection was 68 (range, 11-97). During the procedure the reported median VAS was also 68 (range, 1-100; Fig. 3).
Figure 3.
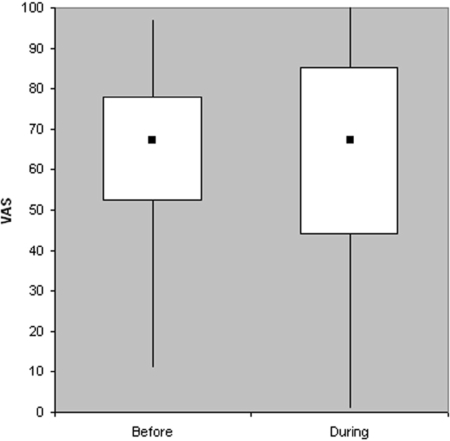
Pain before and during injection, demonstrating VAS range, interquartile range and median.
The median VAS dropped to 25 (77/83 patients) one week after injection and down to 16 (57/83 patients) one month after injection.
Effectiveness was not affected by Eaton grade from 1 to 5 (Table 1). It appeared more effective in Eaton grade 4 although this was a very small sample of patients.
We are aware of no complications except pain during injection (Fig. 3).
Previous injection
Twenty-seven patients reported that they had had at least one previous TMJ injection. Their previous median duration of efficacy was 3 months (range, 0-14 months). This now dropped to 2.25 months (range, 0-11 months). This is to be compared with those patients who had not had a previous injection, which had a median response of 2.5 months (range, 0-24 months).
Summary of findings
One in six patients (10/66) reported beneficial pain-relieving effects of the steroid injection still at 6 months. Furthermore, nearly half the patients had pain relief for more than 3 months. Two-thirds of patients reported a benefit of 2 months. The median response was 2.5 months (range, 0-2 years; Fig. 2). This gives clinicians useful figures to discuss with patients when planning their treatment.
Discussion
There is minimal evidence in the literature to support the efficacy of steroid injections in the TMJ. We present a larger number of patients compared to the other studies which varied from 20 to 41 (Table 2).4-10 Results from these studies are mixed. There has been a varied response, from no benefit over placebo in moderate to severe osteoarthritis,9 to reported useful benefit with steroid injection and splinting, particularly in early osteoarthritis.5,8 Other studies have reported both short6,7,10 and long-term4 effectiveness of steroid injection to the TMJ. Two of these studies include power calculations although only one was able to recruit sufficient numbers to satisfy the calculation (Table 2).6
Table 2.
Comparison of literature results with this study
| Reference THIS STUDY |
| Size 83 |
| Mean age (range) 62 (41–93) |
| M:F 60:23 |
| Adequate power calculation No |
| Radiologically guided Yes |
| Outcome measures Patient perceived effectiveness, VAS |
| Results Effective for half at 3 months (range, 0–2 years), Eaton grade did not affect response |
| Conclusion Safe, can be beneficial in all grades of osteoarthritis |
| Reference Bahadir et al. (2009)4 |
| Size 20 |
| Mean age (range) 62.9 (52–84) |
| M:F 0:20 |
| Adequate power calculation No |
| Radiologically guided No |
| Outcome measures VAS, pinch+grip strength, hand function |
| Results VAS decrease to 12 months, grip improved to 3 months, no change in pinch, function improved to 6 months |
| Conclusion Significant benefit to at least 6 months |
| Reference Day et al. (2004)5 |
| Size 30 |
| Mean age (range) 61 (41–80) |
| M:F 3:27 |
| Adequate power calculation No |
| Radiologically guided No |
| Outcome measures VAS, DASH, pinch+grip strength |
| Results 17/30 had no improvement, 12/30 had sustained improvement to 18 months |
| Conclusion Sustained pain relief in Eaton grade 1, may help grades 2 and 3, but unlikely for grade 4 |
| Reference Heyworth et al. (2008)6 |
| Size 22 |
| Mean age (range) 63 (48–85) |
| M:F 2:20 |
| Adequate power calculation Yes |
| Radiologically guided No |
| Outcome measures VAS, DASH, ROM, pinch+grip strength |
| Results VAS decrease only at 4 weeks, lower DASH to 26 weeks, ROM no change, slight pinch decrease and grip increase |
| Conclusion Small, short-term improvement |
| Reference Joshi (2005)7 |
| Size 25 |
| Mean age (range) Unknown |
| M:F 3:22 |
| Adequate power calculation No |
| Radiologically guided No |
| Outcome measures VAS, Health Assessment Questionnaire |
| Results VAS decreased at 1 month but not beyond |
| Conclusion Limited though well tolerated and safe, effective in short term |
| Reference Khan et al. (2009)8 |
| Size 40 |
| Mean age (range) 65.1 (53–81) |
| M:F 11:29 |
| Adequate power calculation No |
| Radiologically guided No |
| Outcome measures VAS, DASH, subjective reporting |
| Results VAS, DASH and subjective all improved shortterm. Sustained benefit up to 6 months only in early osteoarthritis |
| Conclusion Beneficial 4–6 months in early osteoarthritis, only 4 weeks if advanced |
| Reference Meenagh et al. (2004)9 |
| Size 20 |
| Mean age (range) 60.6 (41–71) |
| M:F 1:19 |
| Adequate power calculation No |
| Radiologically guided Yes |
| Outcome measures VAS, tenderness, stiffness, global assessment |
| Results No change in VAS, stiffness or tenderness. Global assessment improved to 12 weeks but not 24 weeks |
| Conclusion Steroid has no benefit over placebo in moderate to severe osteoarthritis |
| Reference Maarse et al. (2009)10 |
| Size 41 |
| Mean age (range) 60 (39–83) |
| M:F 10:31 |
| Adequate power calculation No |
| Radiologically guided Yes |
| Outcome measures VAS, hand function |
| Results Short-term benefit in three-quarters, longer-term benefit in one-quarter |
| Conclusion Short-term pain relief, not effective long-term |
Inappropriate needle positioning has been found in almost half (42%) of patients before fluoroscopy was then used to check where the injection was aimed.11 Only two previous studies describe the injections to be carried out under radiological guidance.9,10 Consequently, the various outcomes in other previous studies4∧ may be contributed to inappropriate deposition of steroids outside the affected joints. We, therefore, advocate the use of radiological guidance to confirm correct steroid placement into the TMJ. Furthermore, we consider the results of this study to identify more accurately the clinical effect of steroid injection into the TMJ. The overall outcome is, therefore, more likely to be reflected by our study, which showed that nearly half the patients benefited more than 3 months.
We did not find any difference between response to steroid injections and the severity of TMJ osteoarthritis as graded by Eaton et al.12 This is surprising, as we hypothesised, similar to previous studies, that those patients with less advanced osteoarthritis (i.e. grades 1 or 2) would respond better to steroid injection.5,8 It seems that the use of steroids may not have reduced the inflammation and/or synovitis, as we assumed; rather it seems that the response was unpredictable.
Visual analogue scale (VAS) is a semi-quantitative subjective outcome measurement. The reported effectiveness did not always correlate with VAS, which makes it hard to interpret the patients' assessments and our findings fully. In fact, several patients reported that the injection was still effective even though VAS had returned to initial levels. Others reported that the injection had ceased working even though their VAS was considerably lower than the initial score. The VAS provides a snapshot of pain at one particular time-point. The patient's perception of whether the steroid is still working is more reliable since it will guide future intervention.
Many patients found the steroid injection quite painful with some patients scoring it as a VAS of 100 (Fig. 3). We, therefore, propose the use of local anaesthetic as a local block at the injection site to reduce discomfort prior to the intra-articular injection. This is particularly important for less experienced doctors.
One of the weaknesses with this study was that patients were only followed up until they reported that their pain had returned to pre-injection levels or failed to return questionnaires. Seven patients were lost to follow-up beyond the 1-month questionnaire. However, patients who did not respond may have had a satisfactory outcome, since they did not contact the hospital for further intervention. Interventions such as analgesia, splint usage and patient life-style changes were not controlled for, and may have influenced outcomes.
The Eaton grading system is a well-known, but coarse, instrument for recording the degree of trapeziometacarpal osteoarthritis. It is well known that ordinal scales (i.e. 4-point classification) for a continuous variable (i.e. degree of osteoarthritis) are very prone to inter- and intra-observer error. Only one observer scored the X-rays in our study.
Conclusions
This study demonstrates that there are potentially significant benefits to be gained from steroid injections into the TMJ. One-sixth of patients had pain relief still at 6 months, with some patients still being improved 2 years after injection. We believe that the outcome will improve by using flu-oroscopically assisted injections (Fig. 1) and by adding local anaesthetic (Fig. 3). Previously injected patients must expect a reduced duration of benefit compared to their previous injection. Most importantly, steroid injections remain a low-risk procedure and are helpful before considering more invasive treatments. Based on this study, we recommend steroid injections in all degrees of TMJ osteoarthritis.
References
- 1.Yao J, Park MJ. Early treatment of degenerative arthritis of the thumb carpometacarpal joint. Hand Clin. 2008;24:251–61. doi: 10.1016/j.hcl.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Wajon A, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2009;(4):CD004631. doi: 10.1002/14651858.CD004631.pub3. [DOI] [PubMed] [Google Scholar]
- 3.Mayer JH. Carpometacarpal osteoarthritis of the thumb. Lancet. 1970;2:270. doi: 10.1016/s0140-6736(70)92628-0. [DOI] [PubMed] [Google Scholar]
- 4.Bahadir C, Onal B, Dayan VY, Gürer N. Comparison of therapeutic effects of sodium hyaluronate and corticosteroid injections on trapeziometacarpal joint osteoarthritis. Clin Rheumatol. 2009;28:529–33. doi: 10.1007/s10067-008-1079-6. [DOI] [PubMed] [Google Scholar]
- 5.Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI. Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. J Hand Surg Am. 2004;29:247–51. doi: 10.1016/j.jhsa.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Heyworth BE, Lee JH, Kim PD, Lipton CB, Strauch RJ, Rosenwasser MP. Hylan versus corticosteroid versus placebo for treatment of basal joint arthritis: a prospective, randomized, double-blinded clinical trial. J Hand Surg Am. 2008;33:40–8. doi: 10.1016/j.jhsa.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Joshi R. Intraarticular corticosteroid injection for first carpometacarpal osteoarthritis. J Rheumatol. 2005;32:1305–6. [PubMed] [Google Scholar]
- 8.Khan M, Waseem M, Raza A, Derham D. Quantitative assessment of improvement with single corticosteroid injection in thumb CMC joint osteoarthritis? Open Orthop J. 2009;19:48–51. doi: 10.2174/1874325000903010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meenagh GK, Patton J, Kynes C, Wright GD. A randomised controlled trial of intra articular corticosteroid injection of the carpometacarpal joint of the thumb in osteoarthritis. Ann Rheum Dis. 2004;63:1260–3. doi: 10.1136/ard.2003.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maarse W, Watts AC, Bain GI. Medium-term outcome following intra-articular corticosteroid injection in first CMC joint arthritis using fluoroscopy. Hand Surg. 2009;14:99–104. doi: 10.1142/S0218810409004311. [DOI] [PubMed] [Google Scholar]
- 11.Helm AT, Higgins G, Rajkumar P, Redfern DR. Accuracy of intra-articular injections for osteoarthritis of the trapeziometacarpal joint. Int J Clin Pract. 2003;57:265–6. [PubMed] [Google Scholar]
- 12.Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9:692–9. doi: 10.1016/s0363-5023(84)80015-5. [DOI] [PubMed] [Google Scholar]


