Abstract
INTRODUCTION
The treatment of soft-tissue injuries associated with tibial diaphyseal fractures presents a clinical challenge that is best managed by a combined plastic and orthopaedic surgery approach. The current study was undertaken to assess early treatment outcomes and burden of service provision across five regional plastic surgery units in the South-West of England.
SUBJECTS AND METHODS
We conducted a prospective 6-month audit of open tibial diaphyseal fracture management in five plastic surgery units (Bristol, Exeter, Plymouth, Salisbury, Swansea) with a collective catchment of 9.2 million people. Detailed data were collected on patient demographics, injury pattern, surgical management and outcome followed to discharge.
RESULTS
The study group consisted of 55 patients (40 male, 15 female). Twenty-two patients presented directly to the emergency department at the specialist hospital (primary group), 33 patients were initially managed at a local hospital (tertiary group). The mean time from injury to soft tissue cover was significantly less (P < 0.001) in the primary group (3.6 ± 0.8 days) than the tertiary group (10.8 ± 2.2 days), principally due to a delay in referral in the latter group (5.4 ±1.7 days). Cover was achieved with 39 flaps (19 free, 20 local), eight split skin grafts. Nine wounds closed directly or by secondary intention. There were 11 early complications (20%) including one flap failure and four infections. The overall mean length of stay was 17.5 ± 2.8 days.
CONCLUSIONS
Multidisciplinary management of severe open tibial diaphyseal may not be feasible at presentation of injury depending on local hospital specialist services available. Our results highlight the need for robust assessment, triage and senior orthopaedic review in the early post-injury phase. However, broader improvements in the management of lower limb trauma will additionally require further development of combined specialist trauma centres.
Keywords: Open fracture, Soft tissue, Reconstruction, Tibia
Open tibial fractures constitute high-energy injuries associated with significant morbidity, prolonged rehabilitation and variable functional outcome. The established surgical principles include immediate debridement, skeletal stabilisation and early soft tissue cover.1 The joint British Orthopaedic Association and British Association of Plastic Reconstructive and Aesthetic Surgeons (BOA/BAPRAS) standards of care emphasises the need for cross-disciplinary collaboration between plastic and orthopaedic surgeons in complex lower limb trauma.2 Only a minority of acute hospitals provide a plastic surgery service and the initial debridement and fracture fixation are frequently performed in peripheral hospitals before transfer to a hospital with a plastic surgery unit.
The South-West of England is a large region served by five plastic surgery units with a collective catchment of 9.2 million people (16% UK population, UK Census 2001). The units are dispersed across a wide geographical area; therefore, lower limb trauma patients are often initially managed at hospitals without on-site access to a plastic surgery opinion. The aim of our study was to provide a snapshot of early treatment outcomes and burden of lower limb trauma service provision across the South-West.
Subjects and Methods
We conducted a prospective audit of the management of open tibial diaphyseal fractures across five regional plastic surgery units in the South-West of England. The five centres included Bristol (Frenchay Hospital, a specialist trauma centre), Exeter (Royal Devon and Exeter Hospital), Plymouth (Derriford Hospital), Salisbury (Salisbury District Hospital) and Swansea (Morriston Hospital, a specialist trauma centre). Consecutive patients presenting with open tibial diaphyseal wounds to the five plastic surgery units between 1 May and 31 October 2008 were included in the study. Patients admitted during this period but not discharged by 31 October were excluded. In addition, patients presenting with open tibial intra-articular fractures (e.g. plateau, pilon or malleolar) were excluded. Data were entered prospectively using an agreed proforma.
Patient demographics, referral source, characteristics of the injury, fracture pattern and extent of soft tissue according to the Gustilo and Anderson grading system were recorded.3 Details of each procedure were noted including grade of surgeon, fracture fixation system and soft tissue cover. Outcome was assessed by length of time to achieve definitive soft tissue cover, length of in-hospital stay and early postoperative complications.
Statistical analysis was performed using a statistical software package (SPSS, Chicago, IL, USA). An unpaired t-test was employed to compare results between two groups. Probabilities with P < 0.05 were considered statistically significant. The data are described in terms of mean ± SEM.
Results
Over the 6-month study, 55 patients with open tibial shaft fractures presented to the five plastic surgery units in the South-West. The study group consisted of 40 male and 15 female patients with a mean age of 37 years (range, 7-95 years). Patient demographics, fracture characteristics and source of referral are listed in Table 1. Twenty-six (47%) of the patients were involved in road traffic accidents, of whom 17 (31%) were motorcyclists.
Table 1.
Patient demographic details and injury patterns
| Patients | 55 (40 male, 15 female) | ||
| Age | 37 years (range, 7–95 years) | ||
| Mechanism | |||
| Road traffic accident | 27 | ||
| Motorcyclist | 18 | ||
| Pedestrian | 7 | ||
| 4-Wheeled vehicle | 2 | ||
| Fall | 18 | ||
| Bicyclist | 3 | ||
| Other | 7 | ||
| Fracture fixation | |||
| Intramedullary nail | 27 | ||
| External fixator | 23 | ||
| Plate | 4 | ||
| External splint | 1 |
In 22 cases (40%), the patient presented directly to the emergency department at the specialist hospital (primary group), whereas, in 33 cases (60%), the patient was initially managed at a local hospital without a plastic surgery unit (tertiary group). Of patients in the tertiary group, the mean time to referral to a plastic surgery unit was 5.4 ± 1.7 days (range, 0-41 days) and the mean time to admission from injury was 6.4 ± 2.0 days (range, 0-45 days). Fourteen of 33 patients (42%) were referred at the time of the first operation. Reasons for delay in referral included incorrect assessment of grade of soft tissue injury (5/33; 15%) and initial treatment abroad (3/33; 9%). In addition, four patients suffered multiple injuries, which may have taken priority over their injured limb. Amongst patients presenting directly to hospitals with a plastic surgery unit, the mean delay in involving the plastic surgery team was 0.7 ± 0.3 days (range, 0-5 days).
The extent of soft tissue injury and reconstruction performed are listed in Table 2. Most patients suffered fractures associated with significant soft tissue injury (49 cases of Grade IIIa, b or c), whereas, there were few Grade I (3) or Grade II (3) open fractures. In 15 cases, split thickness skin grafting or direct closure of the wound was feasible. In total, 39 flaps were performed to achieve soft tissue cover, of which 20 were local muscle or fasciocutaneous flaps and 19 were free flaps. In keeping with the complexity of the cases, it was found that there was a high frequency of senior surgical input. A consultant plastic surgeon was present in 36 cases (65%) at the first operation performed by the admitting plastic surgery team and involved in the majority of flaps (37 of 39 flaps, 95%).
Table 2.
Fracture grade and selection of soft tissue cover
| Soft tissue reconstruction | Gustilo and Anderson grade | ||||||
|---|---|---|---|---|---|---|---|
| I | II | IIIa | IIIb | IIIc | Total | ||
| Free flaps | Muscle | 0 | 0 | 0 | 9 | 1 | 10 |
| Fasciocutaneous | 0 | 0 | 0 | 9 | 0 | 9 | |
| Local flaps | Muscle | 0 | 0 | 6 | 8 | 0 | 14 |
| Fasciocutaneous | 0 | 0 | 1 | 4 | 0 | 5 | |
| Split skin graft | 0 | 2 | 2 | 4 | 0 | 8 | |
| Direct closure or secondary intention | 3 | 1 | 5 | 0 | 0 | 9 | |
| Total | 3 | 3 | 14 | 34 | 1 | 55 | |
The mean time from injury to soft tissue cover in all patients was 7.9 ± 1.4 days (range, 0-49 days). However, in the primary group, the mean time to definitive soft tissue reconstruction (3.6 ± 0.8 days; range 0-15 days) was significantly less (P < 0.001) than patients initially managed at local hospitals (mean 10.8 ± 2.2 days; range, 2-49 days). In terms of operative burden, patients underwent a mean of 2.9 ± 0.3 procedures (range, 0-10) before discharge with no significant difference between the primary (2.5 ± 0.2 operations) and tertiary groups (3.1 ± 0.4 operations) as summarised in Figure 1.
Figure 1.
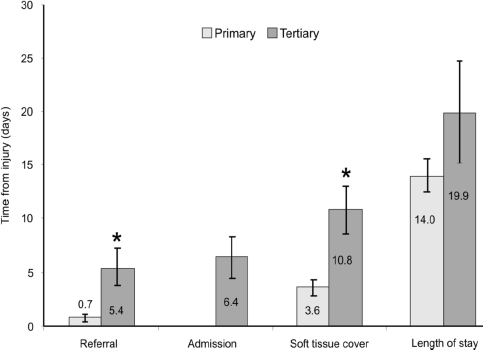
Time taken for admission, referral, soft tissue cover and discharge in patients presenting to specialist centres (primary group) and local hospitals (tertiary group). *Indicates a significant difference between primary and tertiary groups (P < 0.05).
Figure 2.
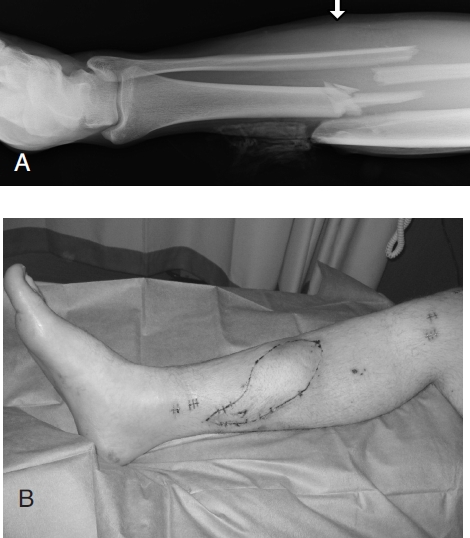
(A) Radiograph demonstrating a mid-shaft tibial fracture in a pedestrian involved in a road traffic accident. (B) The fracture was fixated with an intramedullary nail and the soft tissue defect (Grade IIIb) was reconstructed with a free anterolateral thigh flap.
One patient was deemed to have an unsalvageable limb at presentation due to the severity of the injury and underwent a primary below knee amputation. In the other 54 of 55 patients (98%), the injured lower limb was salvaged. Four of 19 free flaps required re-exploration, of which three were salvaged (one failure, 5.3%). There were two cases of partial flap failure (1 local fasciocutaneous, 1 free serratus anterior muscle flap). Superficial wound infections complicated three reconstructions and there was one metalwork infection, which resulted in removal of an intramedullary nail. All four cases of infection occurred in patients managed initially in local hospitals. There was one mortality. The overall mean length of stay was 17.5 ± 2.8 days (range, 3-150 days) with patients in the tertiary group tending to experience longer stays (19 ± 4.7 days) than patients in the primary group (13.9 ± 1.5 days), although the difference did not achieve statistical significance.
Discussion
The management of open tibial fractures presents a challenge due to the propensity for fracture non-union, difficulty in achieving robust soft tissue cover and morbidity from concomitant injuries. This study provided an insight into early treatment outcomes and burden of service provision across five plastic surgery units in the South-West of England, which collectively serve a large population catchment. The BOA/BAPRAS standards of care provide a benchmark for delivery of care, although the specific remit of the study was not to evaluate compliance with the guidelines, which has been examined in other regions.4,5
Most patients enlisted in the study were involved in high-energy trauma suffering comminuted fractures with severe soft tissue disruption. This finding implies that orthopaedic surgeons manage the majority of minor soft tissue injuries without collaboration. The number of patients was relatively low for the study population due to the exclusion of patients with non-diaphyseal tibial fractures, although it is acknowledged this group requires a similar management approach.6
One of the key findings of the study was a significant delay in admission to a plastic surgery centre for patients presenting to local hospitals (6.4 days). A closer examination of the data revealed that the delay was in initiating a plastic surgery referral (5.4 days) and not bed availability. The majority of patients were not referred by the time of the first surgical procedure. In some cases, underestimation of the extent of soft tissue injury by the admitting team prevented timely referral. The knock-on effect was delayed soft tissue cover.
The timing of soft tissue cover in lower limb trauma is a critical determinant of outcome.7 Evidence suggests that early cover reduces the risk of osteomyelitis and fracture non-union.8,9 In addition, there is a strong suspicion that early reconstruction improves flap survival although the evidence is less compelling.10,11 Certainly, microsurgery becomes more challenging with a delay due to an increased pro-thrombotic environment, tissue oedema and the vessels become increasingly friable. The current standards of care recommend that free flap reconstruction should be performed on a scheduled trauma list to allow appropriate planning, patient preparation and senior surgical and anaesthetic input.2 In practical terms, the 5-day rule has been loosened to a 7-day window for definitive soft tissue reconstruction.
Our results demonstrated a 3-fold difference in time taken to achieve soft tissue cover between patients in the primary and tertiary groups. Specifically, patients presenting to local hospitals endured a mean delay of greater than 10 days before fracture wounds were definitively covered. It was notable that all four cases of wound infection and the one flap failure occurred in this group. However, no firm conclusions can be drawn between timing and definitive outcome as the follow-up period did not enable an assessment of fracture union or function.
Conclusions
A critical finding of our study is that only patients presenting to a hospital with a combined orthopaedic and plastic surgery service are likely to receive definitive treatment of their injury within the established parameters of good practice. Cross-disciplinary management of severe lower limb trauma is a logistical challenge as most hospitals do not have a plastic surgery unit and even fewer provide an actual dedicated orthoplastic trauma service. The need for robust assessment, triage and senior orthopaedic review in the early post-injury phase is, therefore, essential. Ultimately, improvement in the management of lower limb trauma in the UK is contingent on surgeons from both disciplines demonstrating an interest in the specialty to facilitate further development of combined trauma centres.
References
- 1.BOA/BAPRAS. A report by the British Orthopaedic Association/British Association of Plastic Surgeons Working Party on the management of open tibial fractures. Br J Plast Surg. 1997;50:570–83. doi: 10.1016/s0007-1226(97)90501-4. [DOI] [PubMed] [Google Scholar]
- 2.Nanchahal J, Nayagam D, Khan U, Barrett S, Sanderson F, Pallister I. Standards for the management of open fractures of the lower limb. London: RSM Press; 2009. [Google Scholar]
- 3.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 4.Allison K, Wong M, Bolland B, Peart F, Porter K. The management of compound leg injuries in the West Midlands (UK): are we meeting current guidelines? Br J Plast Surg. 2005;58:640–5. doi: 10.1016/j.bjps.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Clough TM, Bale RS. Audit of open tibial diaphyseal fracture management at a district accident centre. Ann R Coll Surg Engl. 2000;82:436–40. [PMC free article] [PubMed] [Google Scholar]
- 6.Khan U, Smitham P, Pearse M, Nanchahal J. Management of severe open ankle injuries. Plast Reconstr Surg. 2007;119:578–89. doi: 10.1097/01.prs.0000246506.58128.ec. [DOI] [PubMed] [Google Scholar]
- 7.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78:285–92. doi: 10.1097/00006534-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Fischer MD, Gustilo RB, Varecka TF. The timing of flap coverage, bone-grafting, and intramedullary nailing in patients who have a fracture of the tibial shaft with extensive soft-tissue injury. J Bone Joint Surg Am. 1991;73:1316–22. [PubMed] [Google Scholar]
- 9.Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82:959–66. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 10.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg Br. 2006;88:351–7. doi: 10.1302/0301-620X.88B3.17120. [DOI] [PubMed] [Google Scholar]
- 11.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) Study Group. J Bone Joint Surg Am. 2000;82:1681–91. [PubMed] [Google Scholar]


