Abstract
INTRODUCTION
The aim of this pilot study was to assess the effect of pre-operative inspiratory muscle training (IMT) on respiratory variables in patients undergoing major abdominal surgery.
PATIENTS AND METHODS
Respiratory muscle strength (maximum inspiratory [MIP] and expiratory [MEP] mouth pressure) and pulmonary functions were measured at least 2 weeks before surgery in 80 patients awaiting major abdominal surgery. Patients were then allocated randomly to one of four groups (Group A, control; Group B, deep breathing exercises; Group C, incentive spirometry; Group D, specific IMT). Patients in groups B, C and D were asked to train twice daily, each session lasting 15 min, for at least 2 weeks up to the day before surgery. Outcome measurements were made immediately pre-operatively and postop-eratively.
RESULTS
In groups A, B and C, MIP did not increase from baseline to pre-operative assessments. In group D, MIP increased from 51.5 cmH2O (median) pre-training to 68.5 cmH2O (median) post-training pre-operatively (P < 0.01). Postoperatively, groups A, B and C showed a fall in MIP from baseline (P < 0.01, P < 0.01) and P = 0.06, respectively). No such significant reduction in postoperative MIP was seen in group D (P = 0.36).
CONCLUSIONS
Pre-operative specific IMT improves MIP pre-operatively and preserves it postoperatively. Further studies are required to establish if this is associated with reduced pulmonary complications.
Keywords: Powerbreathe®, Incentive spirometry, Deep breathing exercises, Inspiratory muscle training, Pulmonary function tests
Patients undergoing major surgery suffer postoperative respiratory complications with significant postoperative morbidity and mortality.1,2 Complications include atelectasis, pneumonia and adult respiratory distress syndrome. Nearly one-quarter of deaths occurring within 6 days of surgery are related to postoperative pulmonary complications.3 Thoracotomy and coronary artery bypass grafting carry with them a particularly high risk of pulmonary complications.4,5 The incidence of postoperative pulmonary complications after abdominal surgery is reported to be 6-76%,6–9, 16 with the incidence following upper abdominal operations as high as 60-75%.2,6 A leading cause of postoperative pulmonary complications is inadequate inspiratory effort leading to inadequate expectoration of sputum. Furthermore, a high respiratory demand leads to inspiratory muscle fatigue and exacerbates collapse of alveoli. Mean length of stay in the hospital has been shown to be 6 times more in patients who develop postoperative pulmonary complications following elective non-thoracic surgery.10
Inspiratory muscle training (IMT) improves performance in athletes11,12 as well as exercise tolerance and quality of life in patients with chronic obstructive pulmonary disease13,14 and other conditions affecting the respiratory system such as cystic fibrosis, Parkinson's disease and myas-thenia gravis.15–17 Pre-operative IMT may prevent postoperative pulmonary complications by increasing inspiratory muscle strength as assessed by inspiratory pressures in patients undergoing CABG4 and thoracic surgery.5 Although there may be some benefit of pre-operative incentive spirometry, deep breathing exercises and chest physiotherapy in reducing postoperative pulmonary complications following major abdominal surgery,18–20 systematic analysis does not support the use of incentive spirometry for decreasing the incidence of postoperative pulmonary complications following cardiac or upper abdominal surgery.21 However, there is virtually no research of specific IMT in preventing postoperative pulmonary complications in patients undergoing major elective general surgical operations where fewer respiratory complications could make a substantial difference to morbidity, mortality, length of stay and cost of care.
Powerbreathe® (HaB Ltd, UK) is a hand-held specific inspiratory muscle trainer available on NHS prescription that improves maximal static inspiratory mouth pressure22 in healthy humans and patients with lung disease.13 It is simple to use and rapid to learn. It has not been used previously to train surgical patients. Incentive spirometry (Henley's Medical Ltd, UK) is also simple and quick to learn. Both devices are self-administered and cheaper than physiotherapy. Our hypothesis is that pre-operative IMT is more effective than incentive spirometry or deep breathing exercises (DBE) in preserving inspiratory muscle function postoperatively.
Patients and Methods
Setting and patients
Patients undergoing major abdominal surgery were assessed and trained by the researcher. Ethics committee approval was granted by the Southmead Research Ethics Committee, Bristol with reference number 06/Q2002/88. The study adhered to the Declaration of Helsinki.
Patients were included if they were: (i) over 18 years of age; and (ii) undergoing major abdominal general surgery (defined as deliberate breach of peritoneum), or major uro-logical surgery, with ASA (American Society of Anesthesiologists) grades I-IV requiring any length of hospital stay. Patients were excluded if they were ASA grade V, had suspected or established respiratory infection, were likely to undergo surgery to be performed within 2 weeks of initial assessment, had previous spontaneous pneumotho-rax, or were unable to give informed consent.
Randomisation
Patients were allocated to four groups by computer-generated, random numbers placed in sequentially numbered sealed envelopes: Group A, control (no training); Group B, deep breathing exercise; Group C, incentive spirometry; and group D, specific inspiratory muscle training using Powerbreathe®. Group allocation was non-blinded and done after baseline assessment.
Assessments and intervention
ASSESSMENT 1 - BASELINE
Baseline assessment included: (i) type of surgical procedure and past medical history; (ii) pulmonary function including vital capacity (VC), forced vital capacity (FVC), and forced expiratory volume in 1 s (FEV1); and (iii) maximum inspiratory mouth pressure (MIP: pressure generated in the mouth on maximum inspiration against an occluded airway after exhaling completely to residual volume) and maximum expiratory mouth pressure (MEP: pressure generated in the mouth on maximum expiration against an occluded airway after inhaling completely to total lung capacity). A minimum of three technically correct measurements of each was made and the highest value recorded.
INTERVENTION
Patients were expected to train twice daily for 2 weeks minimum,4 since most were to undergo surgery within 2-3 weeks after decision to operate. Patients were instructed in technique by the researcher and were asked to train twice daily each session lasting 15 min up to the day before surgery at home. They undertook self-assessment of training completed and ease of training method (1-5, 1 being very easy and 5 being very difficult).
Patients in group B were taught deep breathing exercises. Patients in group C used Spiroball®, an incentive spirometry device. The training load was set depending on age and gender. Patients in group D trained using Powerbreathe®. The initial device resistance loading was set to 20-30% of baseline MIP and according to ease of use in the first session. The load varied from 1 to 9 and was increased incrementally by half a level daily for the first week. For the remaining duration, patients trained at a level achieved at the end of the first week.
ASSESSMENT 2 - IMMEDIATE PRE-OPERATIVE
This was performed within 48 h before surgery and included the aforementioned respiratory variables.
ASSESSMENT 3 - FINAL POSTOPERATIVE
Usually performed between 1-7 days postoperatively depending on the patient's physical ability, pain score and the discharge date, the respiratory variables were re-measured.
Outcome measures
Primary end-points were absolute and relative change in all respiratory variables following training before surgery and after surgery. Secondary outcome measures included length of stay of patients, time in HDU/ITU postoperatively, time on a ventilator, respiratory rates and oxygen saturations from charts at a fixed time postoperatively off oxygen, proven respiratory infection (positive sputum culture) and other pulmonary complications.
Statistical analysis
This was performed using Statistics Package for Social Sciences (SPSS) with guidance from a statistician. Pre-training and post-training and after surgery differences in VC, FCV, FEV1, MIP and MEP were analysed for significance. Wilcoxon signed rank test (non-parametric method) was used for analysis of the differences and a P-value < 0.05 was taken as significant. Since this was a pilot study, formal calculation of sample size was not necessary.
Results
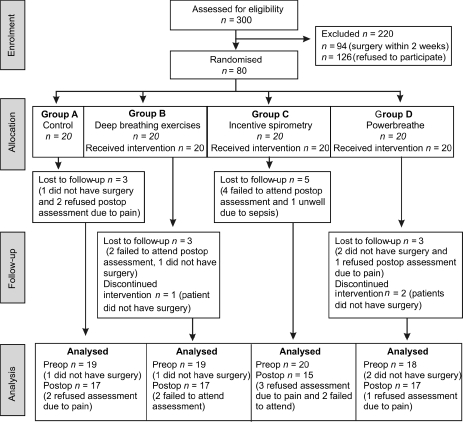
A total of 300 eligible patients were invited to participate, and 80 patients consented (Fig. 1). Their demographics and clinical characteristics are shown in Supplementary Material Table 1 (online). Four patients due to have laparoscopic surgery did not and, therefore, were not assessed further. Thirty-two patients recruited underwent colorectal operations, 22 upper gastrointestinal, 11 vascular, 10 general surgical operations and one underwent urological surgery. Patients in group A did not train. Patients in group B trained for 14 days (median; range, 6-35 days) with grade 3 difficulty (median; range, 1–4). Those in group C trained for 14 days (median; range, 10–50 days) with grade 2 difficulty (median; range, 1–5) and those in group D trained for 14 days (median; range, 8–28 days) with grade 3 difficulty (median; range, 1–4). Nineteen patients in groups A and B, 20 in group C and 18 in group D had pre-operative measurements of all respiratory variables. Postoperative measurements of all respiratory variables were performed in 17 patients in group A (median, 7 days; range, 1–27 days), B (median, 2 days; range, 1–33) and D (median, 6 days; range, 1–22 days) and 15 patients in group C (median, 6 days; range, 1–24 days). Fourteen patients did not have postoperative measurements; six patients due to pain, four patients failed to attend follow-up appointment and four patients did not have surgery.
Figure 1.
Consort flow diagram.
Inspiratory muscle strength
In group D, MIP increased from 51.5 cmH2O before training to 68.5 cmH2O (median) after training pre-operatively (P < 0.01). No such changes were seen pre-operatively in the other groups. Postoperatively, groups A, B, and C showed a fall in MIP and only in group D did the MIP remain more than pre-training level (Table 2A).
Table 2A.
Maximum inspiratory pressure of all the groups
| Baseline MIP (median) cmH2O (range) | Pre-operative MIP (median) cmH2O (range) | aP-value | Postoperative MIP (median) cmH2O (range) | b,cP-value | |
|---|---|---|---|---|---|
| Group A | 55 (30–93) | 48 (21–94) | 0.25 | 42 (25–97) | < 0.01 |
| Group B | 55 (10–120) | 48 (9–118) | 0.04 | 43 (6–79) | < 0.01 |
| Group C | 50.5 (14–94) | 44 (15–88) | 0.19 | 35 (14–84) | 0.06 |
| Group D | 51.5 (33–97) | 68.5 (44–121) | <0.01 | 61 (28–106) | 0.36 |
| dP-value | < 0.01 | 0.01 |
Comparing baseline with pre-operative.
Comparing baseline with postoperative.
Wilcoxon signed rank test.
Kruskal–Wallis test.
Expiratory muscle strength
MEP showed little or no change between pre-training and pre-operatively, and reduced postoperatively in all four groups (Supplementary Material Table 2B online).
Vital capacity and forced vital capacity
VC showed little change between baseline and pre-operative measurements in all four groups. It reduced in all four groups postoperatively but only in group D was this reduction not statistically significant (Table 3A). Postoperatively, FVC reduced significantly in all groups (Supplementary Material Table 3B online).
Table 3A.
Vital capacity of all the groups
| Baseline VC (median) litres (range) | Pre-operative VC (median) litres (range) | a,cP-value | Postoperative VC (median) litres (range) | b,cP-value | |
|---|---|---|---|---|---|
| Group A | 3.74 (1.93–5.28) | 3.84 (2.16–5.03) | 0.20 | 3.24 (1.33–4.55) | < 0.01 |
| Group B | 3.29 (2.10–5.86) | 3.14 (2.10–5.60) | 0.97 | 2.72 (1.69–5.79) | < 0.01 |
| Group C | 3.14 (1.73–5.81) | 3.16 (1.92–5.62) | 0.44 | 2.33 (1.49–4.31) | < 0.01 |
| Group D | 3.28 (2.08–4.60) | 3.13 (2.18–5.20) | 0.16 | 3.08 (1.78–4.70) | 0.11 |
| dP-value | 0.65 | 0.34 |
Comparing baseline with pre-operative.
Comparing baseline with postoperative
Wilcoxon signed rank test
Kruskal–Wallis test.
Forced expiratory volume in 1 second
FEV1 showed little change pre-operatively, and reduced significantly postoperatively compared to baseline levels (Supplementary Material Table 3C online).
Secondary outcome measures
No patients in groups C and D had respiratory complications following surgery. Two patients in group A and one in group B had chest infections requiring antibiotic treatment (Supplementary Material Table 4 online).
Discussion
This study demonstrates that inspiratory muscle training for 2 weeks before surgery using a prescribable inspiratory muscle trainer (Powerbreathe®) resulted in a significant increase in inspiratory muscle strength before major abdominal surgery that continued to be significantly better than other groups postoperatively. Patients in all the other groups showed significant impairment in respiratory muscle strength as well as lung function postoperatively, but vital capacity appeared better preserved in the IMT group. These results accord with other randomised studies of IMT in patients undergoing cardiac and thoracic surgeries.4,5 Moreover, these findings are consistent with studies of IMT performed on athletes11,12,23 and patients with COPD13,14,24,25 that showed improvement in inspiratory muscle strength, exercise tolerance and quality of life after training.
The study also included two other common, inexpensive techniques - incentive spirometry and deep breathing exercises. Although these techniques are used on postoperative patients to improve their breathing function, these training methods failed to confer any benefits on lung function and the inspiratory muscle strength pre- and postoperatively.
There is a high incidence of postoperative pulmonary complications in patients undergoing major abdominal surgery. 2,6,7,9,16 This is thought to be due to inspiratory muscle fatigue leading to collapse of alveoli. Although this study does not accurately reflect the true incidence of postoperative pulmonary complications, one might speculate that improvement in inspiratory muscle strength following training is likely to prevent inspiratory muscle fatigue and, in turn, lead to reduced postoperative pulmonary complications and hospital stay. Interestingly, studies on healthy young athletes indicate that exercise-induced inspiratory muscle fatigue is attenuated substantially after IMT.11,12
Remarkably, pulmonary function including VC, FVC and FEV1 remained almost unchanged at the end of the training period pre-operatively in all the groups (IMT). After surgery, there was a significant reduction in almost all lung function variables in groups A-C, but VC in patients of group D was maintained at near baseline levels. This indicates that a patient's ability to overcome the elastic load to inhalation was improved following IMT. Since other variables are indices of airway function, we would not predict these to change in patients without lung disease. Maintenance of vital capacity may improve cough function, and lessen the risk of postoperative pulmonary complications.26
The inclusion and exclusion criteria were deliberately very open so that the results could be generalised to wider age groups undergoing abdominal surgery rather than to a few young patients with better compliance. This study fulfilled the aim of testing the feasibility of pre-operative training in major abdominal surgical patients. Almost all patients were able to train for at least 2 weeks before surgery and very few found the training difficult to perform. However, some patients may be fitter and at lower risk than others, which may have had an impact on results. There may be a case for selecting only high-risk patients for pre-operative IMT based on their pulmonary risk score.27
The strict exclusion criteria meant that patients unlikely to wait for 2 weeks to undergo surgery were excluded. Consequently, a large number of patients awaiting intra-abdominal cancer surgery were not included in the study and may, in future, miss out on an opportunity to improve breathing before surgery. It may be necessary to keep the training period more flexible to suit needs of such challenging groups of patients who deserve to have urgent surgery. Arguably, perhaps for patients at high risk of postoperative pulmonary complications, it may become important to defer surgery to allow for a short period of IMT.
Whilst the results are interesting, this pilot study was not designed to provide clear evidence of benefits of IMT in reducing incidence of postoperative pulmonary complications and hospital stay. Nonetheless, it is clear that IMT improves and preserves inspiratory muscle strength and vital capacity pre- and postoperatively. It remains to be seen whether these improvements translate into a reduced incidence of postoperative pulmonary complications and hospital stay. However, these data provide justification for a larger randomised controlled trial to answer this question.
Acknowledgments
Gloucestershire Hospitals NHS Foundation Trust funded this study. The authors would like to thank Mr A Goodman, Mr J Wheeler, Mr N Borley (consultant colorectal surgeons), Mr J Bristol, Mr C Chan (consultant breast and general surgeons), Mr H Gilbert, Mr R Kinder (consultant urologists), Mr M Aljarabah (clinical research fellow) and Dr H Nabti (specialist trainee) for their contribution and support. The authors would also like to thank Chris Foy for statistical advice and Alex Townsend, Linda Henderson, Helen Sandercock and Sophia Mulcahy for secretarial support.
Conflict of interest
Professor Alison McConnell has a beneficial interest in the Powerbreathe - inspiratory muscle trainer in the form of a royalty share on licence income to the University of Birmingham, UK. She also acts as a consultant to HaB Ltd.
References
- 1.Teba L, Omert LA. Postoperative respiratory insufficiency. Am Fam Phys. 1995;51:1473–80. [PubMed] [Google Scholar]
- 2.Roukema JA, Carol EJ, Prins JG. The prevention of pulmonary complications after upper abdominal surgery in patients with noncompromised pulmonary status. Arch Surg. 1988;123:30–4. doi: 10.1001/archsurg.1988.01400250032004. [DOI] [PubMed] [Google Scholar]
- 3.Brooks-Brunn JA. Postoperative atelectasis and pneumonia. Heart Lung. 1995;24:94–115. [PubMed] [Google Scholar]
- 4.Weiner P, Zeidan F, Zamir D, Pelled B, Waizman J, et al. Prophylactic inspiratory muscle training in patients undergoing coronary artery bypass graft. World J Surg. 1998;22:427–31. doi: 10.1007/s002689900410. [DOI] [PubMed] [Google Scholar]
- 5.Nomori H, Kobayashi R, Fuyuno G, Morinaga S, Yashima H. Preoperative respiratory muscle training. Assessment in thoracic surgery patients with special reference to postoperative pulmonary complications. Chest. 1994;105:1782–8. doi: 10.1378/chest.105.6.1782. [DOI] [PubMed] [Google Scholar]
- 6.Hallbook T, Linblad B, Lindroth B, Wolff T. Prophylaxis against pulmonary complications in patients undergoing gall bladder surgery. Ann Chir Gynaecol. 1984;73:55–8. [PubMed] [Google Scholar]
- 7.Dripps RD, Deming M. Postoperative atelectasis and pneumonia. Ann Surg. 1946;124:94–110. [PubMed] [Google Scholar]
- 8.Thoren L. Postoperative pulmonary complications. Acta Chir Scand. 1954;107:193–205. [PubMed] [Google Scholar]
- 9.Latimer RG, Dickman M, Day WC, Gunn ML, Schmidt CD. Ventilatory patterns and pulmonary complications after upper abdominal surgery determined by pre operative and postoperative computerised spirometry and blood gas analysis. Am J Surg. 1971;122:622–32. doi: 10.1016/0002-9610(71)90290-x. [DOI] [PubMed] [Google Scholar]
- 10.McAlister FA, Bertsch K, Man J, Beadley J, Jacka M. Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med. 2005;171:514–7. doi: 10.1164/rccm.200408-1069OC. [DOI] [PubMed] [Google Scholar]
- 11.Romer LM, McConnell AK, Jones DA. Inspiratory muscle fatigue in trained cyclists: effects of inspiratory muscle training. Med Sci Sports Exer. 2002;34:785–92. doi: 10.1097/00005768-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Volianitis S, MacConnell AK, Koutedakis Y, MacNaughton L, Backx K, Jones DA. Inspiratory muscle training improves rowing performance. Med Sci Sports Exerc. 2001;33:803–9. doi: 10.1097/00005768-200105000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Beckerman M, Magadle R, Weiner M, Weiner P. The effects of 1 year of specific inspiratory muscle training in patients with COPD. Chest. 2005;128:3177–82. doi: 10.1378/chest.128.5.3177. [DOI] [PubMed] [Google Scholar]
- 14.Weiner P, Weiner M. Inspiratory muscle training may increase peak inspiratory flow in chronic obstructive pulmonary disease. Respiration. 2006;73:151–6. doi: 10.1159/000088095. [DOI] [PubMed] [Google Scholar]
- 15.Enright S, Chatham K, Ionescu AA, Unnithan VB, Shale DJ. Inspiratory muscle training improves lung function and exercise capacity in adults with cystic fibrosis. Chest. 2004;126:405–11. doi: 10.1378/chest.126.2.405. [DOI] [PubMed] [Google Scholar]
- 16.Inzelberg R, Peleg N, Nisipeaanu P, Magadle R, Carasso RL, Weiner P. Inspiratory muscle training and the perception of dyspnoea in Parkinson's disease. Can J Neurol Sci. 2005;32:213–7. doi: 10.1017/s0317167100003991. [DOI] [PubMed] [Google Scholar]
- 17.Weiner P, Gross D, Meiner Z, Ganem R, Weiner M, et al. Respiratory muscle training in patients with moderate to severe myasthenia gravis. Can J Neurol Sci. 1998;25:236–41. doi: 10.1017/s0317167100034077. [DOI] [PubMed] [Google Scholar]
- 18.Fagevik Olsen M, Hahn I, Nordgren S, Lonroth H, Lundholm K. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg. 1997;84:1535–8. doi: 10.1111/j.1365-2168.1997.02828.x. [DOI] [PubMed] [Google Scholar]
- 19.Celli BR, Rodriguez KS, Snider GL. A controlled trial of intermittent positive pressure breathing, incentive spirometry, and deep breathing exercises in preventing pulmonary complications after abdominal surgery. Am Rev Respir Dis. 1984;130:12–5. doi: 10.1164/arrd.1984.130.1.12. [DOI] [PubMed] [Google Scholar]
- 20.Thomas JA, McIntosh JM. Are incentive spirometry, intermittent positive pressure breathing, and deep breathing exercises effective in the prevention of post operative pulmonary complications after upper abdominal surgery? A systematic overview and meta-analysis. Phys Ther. 1994;74:3–10. doi: 10.1093/ptj/74.1.3. discussion 10-6. [DOI] [PubMed] [Google Scholar]
- 21.Overend TJ, Anderson CM, Lucy SD, Bhatia C, Jonsson BI, Timmermans C. The effect of incentive spirometry on postoperative pulmonary complications: a systematic review. Chest. 2001;120:971–8. doi: 10.1378/chest.120.3.971. [DOI] [PubMed] [Google Scholar]
- 22.Hart N, Sylvester K, Ward S, Cramer D, Moxham J, Polkey MI. Evaluation of an inspiratory muscle trainer in healthy humans. Respir Med. 2001;95:526–31. doi: 10.1053/rmed.2001.1069. [DOI] [PubMed] [Google Scholar]
- 23.Griffiths LA, McConnell AK. The influence of inspiratory and expiratory muscle training upon rowing performance. Eur J Appl Physiol. 2007;99:457–66. doi: 10.1007/s00421-006-0367-6. [DOI] [PubMed] [Google Scholar]
- 24.McConnell AK. The role of inspiratory muscle function and training in the genesis of dyspnoea in asthma and COPD. Prim Care Respir J. 2005;14:186–94. doi: 10.1016/j.pcrj.2005.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lima EV, Lima WL, Nobre A, dos Santos AM, Brito LM, Costa Mdo R. Inspiratory muscle training and respiratory exercises in children with asthma. J Bras Pneumol. 2008;34:552–8. doi: 10.1590/s1806-37132008000800003. [DOI] [PubMed] [Google Scholar]
- 26.Kang SW, Shin JC, Park CI, Moon JH, Rha DW, Cho DH. Relationship between inspiratory muscle strength and cough capacity in cervical spinal cord injured patients. Spinal Cord. 2006;44:242–8. doi: 10.1038/sj.sc.3101835. [DOI] [PubMed] [Google Scholar]
- 27.Hulzebos EH, Helders PJ, Favie NJ, De bie RA, Brutel de la Riviere A, Van Meeteren NL. Preoperative intensive inspiratory muscle training to prevent post operative pulmonary complications in high-risk patients undergoing CABG surgery - A randomized clinical trial. JAMA. 2006;296:1851–7. doi: 10.1001/jama.296.15.1851. [DOI] [PubMed] [Google Scholar]