Abstract
Parry–Romberg syndrome (PRS) or progressive hemi facial atrophy syndrome is a rare condition of unknown aetiology that is characterised by progressive unilateral facial and cranial atrophic changes of skin, subcutaneous tissues and bone. The authors describe a 37-year-old female with a history of PRS, who presented with a subarachnoid haemorrhage secondary to rupture of a 9 mm fusiform aneurysm of the posterior cerebral artery. There was an associated external carotid arterio-venous fistula noted with this aneurysm. The aneurysm was treated by endovascular route and was successfully coiled. Follow-up angiogram revealed spontaneous resolution of the fistula with good occlusion of the aneurysm. The aetio-pathogenesis of this rare occurrence, literature review and its management is discussed.
Background
Parry–Rhomberg syndrome (PRS) is a rare condition and associated intracranial vascular abnormality is a rare occurrence. In our case, we describe the first case of posterior communicating artery aneurysm causing subarachnoid haemorrhage. This was incidentally associated with a external carotid arterio-venous (AV) fistula. The aneurysm was successfully managed by coiling and subsequently the AV fistula regressed spontaneously. We have written this case up due to the rarity and we also describe the aetio-pathogenesis of this condition with review of literature
Case presentation
A 37-year-old lady with a background of PRS, presented with a history of sudden onset severe occipital headache associated with a right hemiparesis. Her Glascow coma scale at admission was 13/15 and had a right-sided hemianopia. A non-contrast CT showed a diffuse subarachnoid haemorrhage with intraventricular extension (figure 1). Cerebral angiogram demonstrated a left P2/P3 posterior cerebral artery (PCA) aneurysm (figure 2) associated with a left external carotid artery AV fistula (figure 3). Significant dysplastic collaterals supplying the left anterior cerebral artery territory were seen arising from the right internal carotid artery (ICA). In addition collateralisation was seen from the left external artery through the middle meningeal supplying the left parietal cortex. These findings were noted in the previous angiogram performed 3 years prior to this presentation.
Figure 1.
CT non-contrast brain demonstrating subarachnoid haemorrhage.
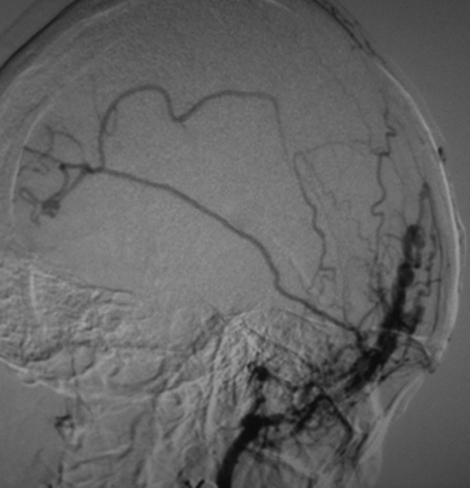
Figure 2.
Cerebral angiogram demonstrating 9 mm P2/P3 PCA aneurysm.
Figure 3.
Angiogram demonstrating the dural AV fistula.
She presented 3 years ago, when she was 32 weeks pregnant, with left-sided facial swelling associated with a throbbing sensation, left ear pulsatile tinnitus, jaw pain and left facial erythema. These symptoms gradually improved over the subsequent week. An MRI brain at that stage showed a PCA aneurysm and left hypoplastic ICA. Subsequent six-vessel angiogram confirmed an 8 mm fusiform aneurismal dilatation of the left P2/P3 segment of the posterior communicating artery. She was treated conservatively owing to her clinical improvement. In her current presentation, the PCA aneurysm was noted to be 9 mm in size.
Differential diagnosis
-
▶
AV malformation
-
▶
Aneurysmal subarachnoid haemorrhage.
Treatment
After discussing the treatment options, she was considered for endovascular management. Wada test was performed, which resulted in slight facial weakness and mild dysphasia, prior to the embolisation. She made an uncomplicated postoperative recovery and the aneurysm was completely occluded (figure 4). CT brain post coiling revealed a small left PCA infarction with no neurological sequelae. Interestingly, subsequent angiogram at 15 months post coiling showed resolution of the left external carotid AV fistula.
Figure 4.
Post coiling angiogram with complete occlusion of the aneurysm.
Outcome and follow-up
She remains clinically well with a mild improvement in her right homonymous hemianopia.
Discussion
PRS is a rare condition of unknown aetiology comprising of progressive atrophy of skin, subcutaneous tissue, fat and muscles of one side of the face. This is also known as progressive hemi facial atrophy. The onset is usually during the first or second decade progressing over a period of 2 to 10 years and then spontaneously remitting leaving the patient with considerable disfigurement. In individuals with this disorder, initial changes usually involve the tissues above maxilla or nasolabial fold and progress to involve the angle of mouth, eye, brow, ear and/or neck (figure 5).1 Overlying skin may become either hyper or hypopigmented. Neurological sequelae include epilepsy, migraine and facial pain and brain lesions on CT and MRI such as ipsilateral cerebral atrophy or calcifications.1 Intracranial vascular malformations including intracranial aneurysm have been rarely described in PRS.2–7 Table 1 summarises the available relevant literature on PRS and intracranial aneurysms.
Figure 5.
Facial appearance of Parry–Rhomberg syndrome (eyes morphed).
Table 1.
Summary of publications on intracranial aneurysms in PRS
| Year | Author | Age | Location | Type | Management |
|---|---|---|---|---|---|
| 1996 | Schievink et al5 | 5 | Ipsilateral ICA | Giant fusiform | Carotid artery ligation and bypass |
| 12 | Contralateral ICA | Giant fusiform | Carotid artery ligation and bypass endovascular | ||
| 21 | PCA | Saccular | Endovascular | ||
| Distal PCA | Fusiform | ||||
| 2002 | Pichiecchio et al7 | 32 | Ipsilateral MCA | Saccular | Conservative |
| 2006 | Aoki et al4 | 56 | Ipsilateral ICA | Giant Fusiform | Conservative |
| 2009 | Bosman et al2 | 10 | Ipsilateral ICA | Giant Fusiform | Ligation with high flow bypass |
| 2011 | Current case | 35 | Ipsilateral PCA | Fusiform | Endovascular embolism |
ICA, internal carotid artery; MCA, middle cerebral artery; PCA, posterior cerebral artery.
Aetio-pathogenesis
Two current hypotheses on the aetiology of PRS present in the literature provide explanations as the origin of intracranial aneurysm in the disease. First it has been postulated that a failure of neural crest migration may explain some of the features of Perry-Romberg including vascular abnormalities and aneurysm formation.5 7 8 There are a number of features of vascular malformations that seem to support this hypothesis in the literature. First, most of the lesions are ipsilateral to the facial atrophy with a recent study on intracranial vascular malformations in PRS describing eight cases of intracranial vascular malformation including their own all reporting this feature.2 Second, our own and two previous studies have described hypoplasia of the ICA in PRS.8 9 Congenital hypoplastic ICA is rare, and has been noted to be consistent with a failure of embryological development of the ICA, which forms by fusion of a succession of embryological arterial segments that lead from the carotid bifurcation in the neck to the Circle of Willis.10 Finally, there are common progenitors in the neural crest during development that derive the tunica media of cervicocephalic arteries and mesenchymal structures of the head and neck, such as the facial dermis, subcutaneous tissues, muscle and skeleton–all structures effected by Perry-Romberg syndrome.11 How these factors could result in aneurysm formation remains unexplained, however it seems plausible that the coexistence of aneurysm with other lesions of known developmental origin makes a strong case for a developmental abnormality in Parry-Romberg.
A second hypothesis for the aetiology of PRS postulates that it is caused by a localised vasculitis and it has been postulated that Parry–Romberg is a variant of linear scleroderma.12 This is supported by histological examinations of facial specimens from patients with PRS that noted a proliferative interstitial neurovasculitis.13 In addition, there appears to be a propensity for giant ICA aneurysm, and fusiform aneurysms in case reports published in the literature (table 1).
These aneurysms are thought to arise from dissection of the arterial wall, and have been associated with both arterial wall inflammation (atherosclerosis) and connective tissue diseases such as Marfan’s and Osteogenesis Imperfecta, which result in underlying arterial wall weakness.14 Still, most cases of fusiform intracranial aneurysm are of unknown origin likely resulting from an unidentified vascular pathology.15 If an underlying inflammatory vasculitis was present this may explain the development of fusiform aneurysm, however, it would not account for the focal nature of the disease.
Learning points.
-
▶
Subarachnoid haemorrhage caused by intracranial aneurysm rupture in Perry-Romberg syndrome is rare.
-
▶
Fusiform aneurysms in this clinical setting may pose a management challenge and the possibility of aneurysmal subarachnoid haemorrhage should be anticipated in this group of patients when intracranial aneurysms are detected.
-
▶
The cerebral aneurysm may be accompanied by other vascular malformation like AV fistula and these may not need treatment as demonstrated in our case.
-
▶
Endovascular treatment appears to be a safe option in the management of subarachnoid haemorrhage.
-
▶
Radiological follow-up by magnetic resonance angiography or cerebral angiogram may prove beneficial.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Stone J. Parry-Romberg syndrome. Practical Neurology 2006;6:185–8 [Google Scholar]
- 2.Bosman T, Van Bei Jnum J, Van Walderveen MA, et al. Giant intracranial aneurysm in a ten-year-old boy with parry romberg syndrome. A case report and literature review. Interv Neuroradiol 2009;15:165–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirata K, Katayama S, Yamano K, et al. Arteriovenous malformation with crossed total hemiatrophy: a case report. J Neurol 1988;235:165–7 [DOI] [PubMed] [Google Scholar]
- 4.Aoki T, Tashiro Y, Fujita K, et al. Parry-Romberg syndrome with a giant internal carotid artery aneurysm. Surg Neurol 2006;65:170–3 [DOI] [PubMed] [Google Scholar]
- 5.Schievink WI, Mellinger JF, Atkinson JL. Progressive intracranial aneurysmal disease in a child with progressive hemifacial atrophy (Parry-Romberg disease): case report. Neurosurgery 1996;38:1237–41 [DOI] [PubMed] [Google Scholar]
- 6.Miediak Al, Stefanyszyn M, Flanagan J, et al. Parry-Romberg syndrome associated with intracranial vascular malformations. Arch Ophthalmol 1998;116:1235–7 [DOI] [PubMed] [Google Scholar]
- 7.Pichiecchio A, Uggetti C, Grazia Egitto M, et al. Parry-Romberg syndrome with migraine and intracranial aneurysm. Neurology 2002;59:606–8; discussion 481. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi UA, Wani NA, Altaf U. Parry-Romberg syndrome associated with unusual intracranial vascular malformations and Phthisis bulbi. J Neurol Sci 2010;291:107–9 [DOI] [PubMed] [Google Scholar]
- 9.Miedziak AI, Stefanyszyn M, Flanagan J, et al. Parry-Romberg syndrome associated with intracranial vascular malformations. Arch Ophthalmol 1998;116:1235–7 [DOI] [PubMed] [Google Scholar]
- 10.Lasjaunias P, Santoyo-Vazquez A. Segmental agenesis of the internal carotid artery: angiographic aspects with embryological discussion. Anat Clin 1984;6:133–41 [DOI] [PubMed] [Google Scholar]
- 11.Noden DM. The role of the neural crest in patterning of avian cranial skeletal, connective, and muscle tissues. Dev Biol 1983;96:144–65 [DOI] [PubMed] [Google Scholar]
- 12.Lehman TJ. The Parry Romberg syndrome of progressive facial hemiatrophy and linear scleroderma en coup de sabre. Mistaken diagnosis or overlapping conditions? J Rheumatol 1992;19:844–5 [PubMed] [Google Scholar]
- 13.Pensler JM, Murphy GF, Mulliken JB. Clinical and ultrastructural studies of Romberg’s hemifacial atrophy. Plast Reconstr Surg 1990;85:669–74; discussion 675–6 [PubMed] [Google Scholar]
- 14.Park SH, Yim MB, Lee CY, et al. Intracranial fusiform aneurysms: it’s pathogenesis, clinical characteristics and managements. J Korean Neurosurg Soc 2008;44:116–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drake CG, Peerless SJ. Giant fusiform intracranial aneurysms: review of 120 patients treated surgically from 1965 to 1992. J Neurosurg 1997;87:141–62 [DOI] [PubMed] [Google Scholar]