Abstract
An adolescent boy underwent laparoscopic evaluation with persisting fever associated with colicky abdominal pain of about 3 weeks duration after a CT study of his abdomen revealed mesenteric adenopathy. Histopathological evaluation of the excised mesenteric nodes showed features of histiocytic necrotising lymphadenopathy suggestive of Kikuchi-Fujimoto lymphadenopathy which was confirmed on immunehistochemistry staining. Kikuchi-Fujimoto’s disease involving the mesenteric nodes is extremely unusual and can be confounding with a mistaken diagnosis of and prolonged treatment for tuberculosis. The authors present a case of Kikuchi-Fujimoto’s disease involving the mesenteric lymph nodes and discuss the various aspects of diagnosis and management of the case along with a review of published literature.
Background
Necrotising lymphadenitis with predominant histiocytic infiltration was described independently by Kikuchi and Fujimoto in 1972 as a benign self-limiting illness characterised by regional lymphadenopathy, low-grade fever and night sweats often involving the cervical lymph nodes in young people with less frequent involvement of lymph nodes elsewhere.1–4 Involvement of intraabdominal lymph nodes by Kikuchi-Fujimoto’s disease (KFD) is extremely uncommon with only 17 cases thus far having been reported in the world literature.4–12 The diagnosis of intraabdominal KFD can be perplexing and is made on histological examination of the resected nodes with additional confirmation by immunestaining techniques.
Case presentation
A young teenage boy was admitted with persisting complaints of unremitting fever since 2 weeks associated with colicky abdominal pain, leg cramps, painful swallowing and a reduced appetite that was worse over the 2 days prior to admission. He stated that the fever at times peaked to nearly 104 degree F with early morning increases; the fever was accompanied with chills and rigors. He denied any cough, running nose, headache, dysuria, loss of weight, vomiting, loose stools or constipation. He stated that the colicky abdominal pain was mainly located in the central and right lower abdomen and was worse soon after ingesting food. He denied any such symptoms previously and stated that he had no known allergies.
Clinical examination revealed a moderately built and nourished young adolescent, febrile, looking ill and with no anaemia, cyanosis, peripheral lymphadenopathy (cervical, axillary or inguinal) or obvious icterus. Systemic examination was unremarkable except for mild deep seated tenderness in the right lower abdomen and paraumbilical regions.
Investigations
Laboratory investigations revealed a total white cell count of 10200 cells/cu mm with a polymporphonuclear cell percentage of 68, a platelet count of 4.5 lakhs/cumm, a raised erythrocyte sedimentation rate of 95 mms/1st h. Urinalysis revealed no evidence of infection; serology showed a negative Widal test, a negative antibody test for dengue and leptospiral infections and negative antibody test for malaria. A dermal tuberculin test was negative; antinuclear antibody was not detected. Renal parameters were normal as was his liver function tests; amylase and lipase levels were normal. Serum IgG, IgA levels of antibody titres for mycobacterium tuberculosis were within reference ranges. A chest radiograph was normal; an ultrasound examination and CT of the abdomen revealed mild hepato-splenomegaly, multiple enlarged nodes in the mesentery and small bowel wall thickening with no ascites. The few mediastinal sections taken during the CT of the abdomen revealed no mediastinal adenopathy. A colonoscopy revealed mild inflammation of the distal ileum from which biopsies were taken to rule out yersinia infection.
Analysis of the fluid aspirated during laparoscopy showed a total count of 300 cells/cumm, predominantly lymphocytes, a few red blood cells, sugar of 60 mg/dl, protein of 5 gm/dl and a chloride level of 72 mq/l. Stains for acid fast bacilli were negative and the culture yielded no growth.
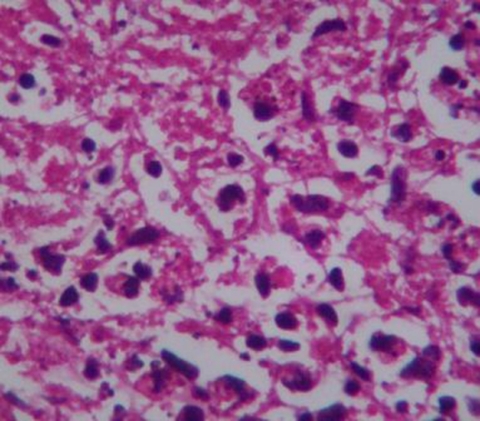
Histology of the resected nodes showed loss of architecture, eosinophilic necrosis, karyorrhectic and karyolytic debris, collection of transformed lymphocytes, histiocytes and plasmacytoid monocytes (figure 1). Neutrophils, giant cells, epithelioid cells were not seen and no granulomas were identified. The appendix showed minimal inflammatory changes while the liver tissue showed normal parenchyma. Immunestaining of the paraffin blocks of the resected nodes showed strong positivity of CD 68 and CD 3 indicating numerous histiocytes and predominance of T-lymphoid cells. A negative CD 15 reflected neutrophil paucity and a weakly positive CD 20 indicated few B lymphoid cells. The ileal biopsy showed mild congestion of vessels with sparse inflammatory cells and the serological tests for yersinia antibody were negative. A final diagnosis was clearly in favour of KFD rather than a lymphoma.
Figure 1.
Lymphnode section showing eosinophilic necrosis, absence of neutrophils and presence of histiocytes and lymphoid cells. H&E ×200.
Treatment
Since the clinical examination was unremarkable except for mild tenderness in the right lower abdomen and the CT scan showed a conglomerated group of lymph nodes in the mesentery of the small bowel, the patient was subjected to a laparoscopic evaluation. Laparoscopy revealed a small amount of yellowish free fluid in the pelvis; peritoneal congestion and inflammatory changes were evident in the pelvis, right paracolic gutter and root of the mesentery of the small bowel (figure 2). A paracecal, congested appendix with its mid third distended was noted. Enlarged, inflamed and matted mesenteric nodes were noted in a thickened ileocolic mesentery. The liver and spleen were mildly enlarged and the rest of the intestines appeared normal. Appendectomy, lymph node resection and a wedge biopsy of the liver were carried out.
Figure 2.
Note the congested mesentery with the enlarged lymphnode underneath.
Outcome and follow-up
The patient’s postoperative recovery was remarkable for a few episodes of semiformed motions, continuing abdominal pain and fever; he also had a stitch abscess of one of the trocar sites that grew Escherichia coli that responded to clarithromycin. Based on the final diagnosis of KFD, he was administered low dose steroid therapy. With this his fever settled and he had no further episodes of pain, fever or loose stools. At 1 year follow-up to date, he has had no further episodes of pain or fever and his check abdominal ultrasound examination has showed no significant residual lymphadenopathy.
Discussion
Even though KFD has a worldwide distribution, the Asiatic population has a predominant involvement especially the younger female population with implication of bacterial, viral and autoimmune causative factors. No single aetiological factor has been identified with certainty although an association between KFD and Epstein-Barr virus, herpes viruses 6 and 82 has been suggested; others have questioned the inclusion of infection with Toxoplasma gondi and herpes virus. A viral aetiology is considered eminently possible in view of the vague clinical manifestations, the lack of response to antibiotic therapy and certain histopathologic features; however, the lack of identification of viral particles on ultrastructural study has questioned this hypothesis. The negative serological tests for rheumatoid factor, antinuclear antibody and other immune diseases have led to the suggestion that KFD could be a hyper immune reaction to several organisms.
The commonest presentation is an acute or subacute febrile illness associated often with cervical lymphadenopathy, occasionally generalised lymphadenopathy and very rarely involving the mediastinal or retroperitoneal nodes.2 9 The illness evolves over 2–3 weeks with most patients having tender lymphadenopathy, generally unilateral and involving the posterior cervical triangle; most lymph nodes range between 0.5 to 4 cm.2 The fever is generally low grade; other less frequent symptoms include weight loss, nausea, vomiting, sore throat and night sweats.2 Systemic symptoms are more often seen when there is extranodal involvement. Involvement of the lymph nodes of the mesentery has thus far been reported in 17 cases4–12 with most patients presenting as acute abdomen and commonly mimicking acute appendicitis.
The diagnosis of KFD is based on histopathological examination of the excised lymph nodes since there are no characteristic ultrasonographic or radiological appearances.2 CT or MRI techniques show appearances that mimic lymphoma apart from other various necrotic nodal diseases such as tuberculosis and metastasis.2 The only significant finding in a small group of patients through these radiological investigations was the presence of many groups of clustered lymph nodes. Fine needle aspiration cytology is limited to only those in whom a sure diagnosis of KFD is made on aspirate studies.2 It is highly likely that KFD is an underdiagnosed disease given the fact that it is a self-limiting disease with sometimes minimal clinical manifestations and especially where no lymph nodal biopsy is routinely carried out.
In as far as the involvement of mesenteric or intraabdominal lymph nodes goes, the diagnosis is confounding and must be ascertained on lymph nodal biopsy based on a high clinical suspicion. Differential diagnoses should include abdominal tuberculosis, non-Hodgkin’s lymphoma, systemic lupus erythematosus, infections with T gondii or Yersinia enterocolitica.
The histopathological classification into three evolving stages by Kuo described proliferative, necrotising and xanthomatous types based on cell pattern and histological findings of necrosis.3 Kuo pointed out that the three histologic types actually might represent a spectrum of the different stages of the disease with an initial proliferative phase that progresses to necrotising and finally resolves into an xanthomatous phase. The common necrotising type with coagulative necrosis, nuclear debris, histiocytes and absence of neutrophils needs to be differentiated from tuberculosis, systemic lupus erythematosus, cat scratch disease and Yersinia pseudotuberculosis infection. The proliferative type is characterised by presence of nodular aggregates of pale cells (usually histiocytes and plasmacytoid monocytes) with scattered nuclear debris and absence of necrosis. This type needs differentiation from lymphoma. The least common type is the xanthomatous type which shows foamy xanthomatous histiocytes without necrosis. Since multiple diagnoses need to be considered, it is appropriate that immunehistochemistry is performed on all resected nodes before a conclusive diagnosis of KFD is made.
In the present case, the immunehistochemistry helped confirm the diagnosis permitting steroid therapy. The histological features and immunestaining study confirmed a necrotising type of KFD and ruled out a lymphoma. He was maintained on low dose prednisolone therapy for about 3 weeks following which his fever and other symptoms completely resolved; a check ultrasound study of the abdomen showed no residual adenopathy in his follow-up review.
KFD is a self-limiting disease that needs a careful and systematic approach for a diagnosis; once the diagnosis is made and confirmed by immunehistochemistry techniques, symptomatic treatment alone would suffice in most cases with a few needing low dose steroid therapy.2
Learning points.
-
▶
KFD should be considered in the differential diagnosis of fever of unknown origin especially in those with mesenteric adenopathy.
-
▶
Ileocolic mesenteric lymph node enlargement with KFD is rare and can be a diagnostic challenge.
-
▶
A high degree of clinical suspicion is essential for proper management.
-
▶
The differential diagnoses to be considered include lymphoma, tuberculosis, systemic lupus erythematosus and infections with Y enterocolitica or T gondii.
-
▶
The diagnosis of KFD is made on histological examination of resected lymph nodes; additional immune staining studies are mandatory to rule out other causes and diseases.
-
▶
Being a self-limiting disease, only supportive therapy is needed with low dosage steroid therapy in those cases where the fever persists.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Dorfman RF. Histiocytic necrotizing lymphadenitis of Kikuchi and Fujimoto. Arch Pathol Lab Med 1987;111:1026–9 [PubMed] [Google Scholar]
- 2.Bosch X, Guilabert A, Miquel R, et al. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol 2004;122:141–52 [DOI] [PubMed] [Google Scholar]
- 3.Kuo TT. Kikuchi’s disease (histiocytic necrotizing lymphadenitis). A clinicopathologic study of 79 cases with an analysis of histologic subtypes, immunohistology, and DNA ploidy. Am J Surg Pathol 1995;19:798–809 [DOI] [PubMed] [Google Scholar]
- 4.Min KW, Jang KS, Jang HS, et al. Kikuchi’s disease of the mesenteric lymph nodes presenting as acute appendicitis. The Korean J of Pathology 2007;41:44–6 [Google Scholar]
- 5.McLoughlin J, Creagh T, Taylor A, et al. Kikuchi’s disease simulating acute appendicitis. Br J Surg 1988;75:1206. [DOI] [PubMed] [Google Scholar]
- 6.Tsang WY, Chan JK, Ng CS. Kikuchi’s lymphadenitis. A morphologic analysis of 75 cases with special reference to unusual features. Am J Surg Pathol 1994;18:219–31 [PubMed] [Google Scholar]
- 7.Teranishi H, Kawasaki K, Sasaki A, et al. Localized intraabdominal Kikuchi-Fujimoto’s disease: a case report and review of literature. Kawasaki Med J 2008;34:285–9 [Google Scholar]
- 8.Poulose V, Chiam P, Poh WT. Kikuchi’s disease: a Singapore case series. Singapore Med J 2005;46:229–32 [PubMed] [Google Scholar]
- 9.Turner RR, Martin J, Dorfman RF. Necrotizing lymphadenitis. A study of 30 cases. Am J Surg Pathol 1983;7:115–23 [PubMed] [Google Scholar]
- 10.Tsujino I, Oguma Y, Yamaguchi J. [Involvement of the intraabdominal lymph nodes in a case of subacute necrotizing lymphadenitis]. Rinsho Ketsueki 1993;34:937–41 [PubMed] [Google Scholar]
- 11.Han H, Kim G, Cho YS, et al. Intraabdominal Kikuchi’s disease mimicking malignant lymphoma on FDG PET-CT. Nucl Med Mol Imaging 2009;43:363–5 [Google Scholar]
- 12.Fernandez SH. Kikuchi’s lymphadenitis (necrotizing lymphadenitis) and systemic lupus erythematosus: a case report. Malays J Pathol 2000;22:25–9 [PubMed] [Google Scholar]