Abstract
African Americans are overrepresented on the organ transplant waiting list because they are disproportionately impacted by certain health conditions that potentially warrant a life-saving transplant. While the African American need for transplantation is considerably high, organ and tissue donation rates are comparatively low, resulting in African Americans spending more than twice the amount of time on the national transplant waiting list as compared to people of other racial/ethnic backgrounds. There are a multitude of factors that contribute to the reluctance expressed by African Americans with respect to organ donation. This study proposes the use of an adaptation of the Organ Donation Model to explore the ways in which knowledge, trust in the donation/allocation process, and religious beliefs impact African American donation decision making. Bivariate and path analyses demonstrated that alignment with religious beliefs was the greatest driving factor with respect to attitudes towards donation; attitudes were significantly associated with donation intentions; and knowledge is directly associated with intentions to serve as a potential deceased organ donor. The significance of these variables speaks to the importance of their inclusion in a model that focuses on the African American population and offers new direction for more effective donation education efforts.
Keywords: organ donation, African American, theory of reasoned action, religion, trust
African Americans represent just 13% of the general population (U.S. Census, 2010) but, represent more than ⅓ of those with end-stage renal disease (ESRD, USRDS, 2009). While transplantation is the preferred treatment modality for ESRD, because of the ongoing shortage of donors, less than 20% of persons on the national transplant waiting list actually receive a transplant and many thousands die waiting (OPTN, 2010b). This gap between the need and the number of available organs is steadily widening. As of June 2011, there were more than 110,000 persons on the waiting list, with approximately 78% of patients specifically awaiting a kidney transplant (OPTN, 2010a). African Americans, in particular, have a disproportionately higher need than other ethnic/racial groups, due to predisposing health conditions such as diabetes and hypertension, which are important contributors to renal failure (Siminoff, Burant, & Ibrahim, 2006). They are over-represented on the transplant waiting list, yet under-represented amongst transplant recipients. This disparity is exacerbated by the relatively low organ and tissue donation rates among African Americans, who donate at rates equal to their representation in the population—not rates equal to their representation on the national waiting list (OPTN, 2010c).
African Americans are also overrepresented on the transplant waiting list, due in part, to the lack of histo-compatible donors. While cross-race transplantation is the norm, transplantation is often most successful when donated organs are matched to others who are genetically similar. The kidney matching process is heavily dependent on the similarity of the protein complex HLA (human lymphocyte antigens), and persons of the same racial/ethnic group tend to be a better match for HLA within their own ethnicity than persons of other races (DHHS, 2008). Taken together, all these factors contribute to African Americans spending up to twice the amount of time on the transplant waiting list compared to other racial/ethnic groups (Danovitch et al., 2005; Louis, Sankar, & Ubel, 1997; Randhawa, 2004; Rozon-Solomon & Burrows, 1999; Sander & Miller, 2005; Young & Gaston, 2002).
An abundance of research has sought to gain an understanding of the lower donation rates among African Americans relative to those of other racial and ethnic backgrounds (Boulware, Ratner, Cooper et al., 2002; Boulware, Ratner, Sosa et al., 2002; Callender, 1987; Callender, Burston, Yeager, & Miles, 1997; Callender, Miles, & Hall, 2002; Callender, Miles, Hall, & Gordon, 2002; Callender & Washington, 1997; Durand, Decker, & Bruder, 2002). Research suggests five key factors that greatly contribute to this reluctance to donate among African Americans: lack of knowledge, religious beliefs, fear of premature death, distrust of the healthcare system, and racism (Callender, 1987; Callender, Hall, & Branch, 2001; Callender, Miles, & Hall, 2002; Gamble, 1997). African Americans may also be hesitant to discuss the topic of donation (Morgan, 2004; Morgan & Miller, 2001, 2002; Morgan, Miller, & Arasaratnam, 2003) and express their intentions via formal means of communication (i.e., documenting it on their driver’s license, a donor card, or on a donor registry; Wagstaff, Korda, & McCleary, 2008). All of these barriers are critical limiting factors to donation and have been the focal point of educational efforts to increase African Americans’ deceased and living donation intentions and behavior (Arriola, Robinson, Thompson, & Perryman, 2010; Boulware, Ratner, Cooper et al., 2002; Boulware, Ratner, Sosa et al., 2002; Durand et al., 2002; Gallagher, 1997; Siminoff & Arnold, 1999).
Despite all of the work in this area, there has been little effort to systematically explore the relative contributions of each of these factors towards shaping African Americans’ donation intentions. Explanatory models that explore the interrelationships among donation-related knowledge, attitudes, and beliefs and the causal pathways linking them to donation intentions and, ultimately, the communication of these intentions, are scarce. One notable exception is the Organ Donation Model (ODM) proposed by Morgan and Miller (2001). Drawing from the work of Radecki and Jaccard (1997; 1999) and the Theory of Reasoned Action, the ODM asserts that the most important determinant of donation behavior is an individual’s behavioral intention and willingness to become a donor, assuming that individuals critically evaluate the positives and negatives of the behavior before deciding to act. According to Morgan and Miller (2001), the most influential components of this intention are an individual’s attitudes toward donation, knowledge about donation, and perception of positive social norms regarding organ donation (Morgan, 2004, 2006; Morgan & Miller, 2001, 2002; Morgan et al., 2003). There is some empirical support for this theory among both white (Morgan & Miller, 2001, 2002; Morgan et al., 2003) and African American (Morgan, 2004, 2006) participants. However, the ODM fails to address two key factors that appear to be strongly related to African Americans’ donation intentions based on the available empirical evidence: the importance of (1) trust in the organ allocation system and the health care system more generally; and (2) religious beliefs relevant to donation.
Distrust of the medical community has been cited as one of the most influential barriers to donation among African Americans (Arriola, Perryman, & Doldren, 2005; Callender et al., 2001; Durand et al., 2002; Minniefield, Yang, & Muti, 2001; Morgan et al., 2003; Terrell, Moseley, Terrell, & Nickerson, 2004). African Americans’ knowledge of historical discrimination and institutional racism not only undermines participation in research studies, but also diminishes overall trust in health systems and clinicians as well (Boulware, Cooper, Ratner, LaVeist, & Powe, 2003; Gamble, 1997; Washington, 2006). African Americans tend to have concerns about the fairness of the organ allocation system (Schutte & Kappel, 1997), whether they will receive the same quality of care as whites (Watkins, Terrell, Miller, & Terrell, 1989), and whether consenting to donation might hasten death (Kurz, Scharff, Terry, Alexander, & Waterman, 2007). Thus, any theoretical model that attempts to explain African Americans’ donation intentions must pay some attention to distrust of the medical community, and organ allocation more specifically.
Because religion maintains a prominent role in African American culture, it can also be quite influential in shaping African Americans’ donation decision making (Arriola, Perryman, Doldren, Warren, & Robinson, 2007). Previous research has found religious beliefs to function as a barrier to donation among minorities (Arriola et al., 2007; Bhengu & Uys, 2004; Darr & Randhawa, 1999; Lam & McCullough, 2000)—namely due to concerns about mutilation of the body or the belief that the body must be whole in order to enter Heaven. Even though almost all major religions have supportive policy statements about donation (Gallagher, 1998; LifeGift, 2002), parishioners’ beliefs have not always aligned with this stance. Research has found that willingness to become a deceased donor is inversely associated with one’s perceived importance of spirituality and religion (Boulware, Ratner, Sosa et al., 2002; Modlin, Bairagi, Chidmeme-Mundowafa, Yoo, & Saffore, 2009; Rumsey, Hurford, & Cole, 2003) . Findings linking religious beliefs to donation intentions are robust and support the need to include them in any explanatory models identifying the barriers and facilitators of deceased donation intentions among African Americans.
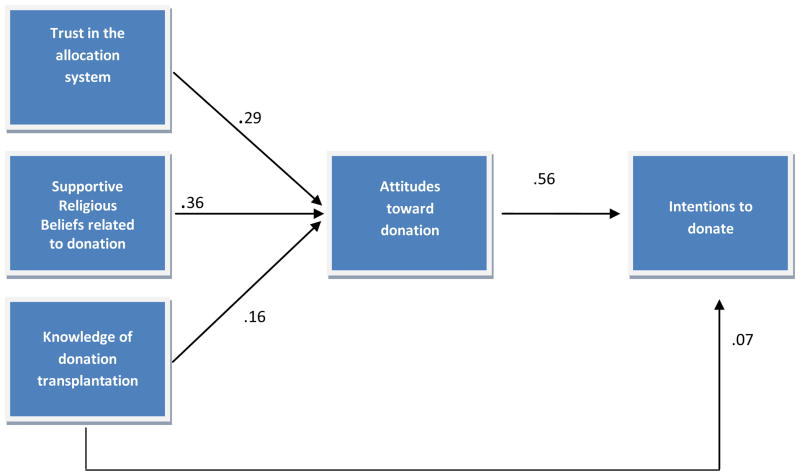
The purpose of this study is to test an adaptation of the ODM that increases its cultural relevance to African Americans by incorporating a stronger emphasis on trust in the organ allocation system and religious beliefs relevant to donation. Specifically, the modified model replaces “Altruism” in the ODM with “Trust in the Organ Allocation system” and “Religious beliefs related to donation” (see Figure 1). The modified ODM hypothesizes a direct pathway between knowledge of organ and tissue donation/transplantation and deceased donation intentions and an indirect pathway from trust in the organ allocation process, knowledge of donation/transplantation, and religious beliefs, to deceased donation intentions via attitudes towards donation and transplantation.
Figure 1.
Modified Organ Donation Model (Standardized Regression Coefficients)
Note. Analyses control for the Community Health Advocate variable.
This study makes novel contributions to the overall body of literature examining factors that impact donation-related intentions among African Americans. There has been little theory development and testing to explain donation intentions among African Americans. Existing research in this area has been largely atheoretical. Those studies that do develop theory have tended to use small subsamples of African Americans and sought to compare them to whites (Morgan & Miller, 2001 but see Morgan & Miller , 2004 as an exception) or developed theoretical models with broad application to several different racial/ethnic groups, thereby missing the nuances of each group (Radecki & Jaccard, 1997). This study is among the first to advance a theoretical model that emphasizes values and cultural beliefs with greatest salience to African Americans, for whom barriers to donation are well-documented. Such work is necessary for the development of culturally-sensitive interventions that shape African Americans’ deceased donation intentions.
This study is guided by the following research hypotheses (see Figure 1):
Trust in the organ allocation system, greater donation-related knowledge, and supportive religious beliefs related to donation would be associated with positive attitudes towards donation.
Positive attitudes towards donation would be associated with greater intentions to serve as a potential deceased organ donor.
Greater donation-related knowledge would be directly associated with greater intentions to serve as a potential deceased organ donor.
Methods
The present study is part of a larger study testing the effectiveness of a culturally-sensitive organ and tissue donation intervention for African American adults. The parent study uses a randomized, pre-post design with a control group; data from the current study were collected during the baseline assessment (which occurred March to December 2009).
Design
Using a cross-sectional research design, the current study combined pre-intervention data from both intervention and control groups. Community Health Advocates (CHAs) facilitated participant recruitment (Eng & Parker, 2002). CHAs were selected based on their demographic similarity to our target population, as well as their ability to bring together a diverse group of people. In order to recruit such individuals, fliers that detailed the opportunity to educate African Americans about the importance of organ donation were distributed to community-based organizations, local church affiliated groups, hospitals, transplant centers, and surrounding dialysis clinics. A total of 19 persons elected to become CHAs and underwent the necessary training.
Data Collection
To ensure diversity in participant recruitment, CHAs were representative of a variety of socioeconomic backgrounds, professions, and affiliations. They were each tasked with individually recruiting a total of 32 participants from members of their social networks (church, professional or community affiliations, family, friends, associates, etc.). They were provided with the necessary recruitment materials including talking points, personalized participant recruitment fliers, and tailored form letters that informed interested persons about the study. Participants were recruited with the understanding that they were participating in a two-hour, group, health-related discussion and would be compensated $15 in appreciation for their time.
Participants were considered eligible if they self-identified as black or African American (for the purpose of this study, the term “black” includes people of African descent regardless of cultural identification) and were 18 years of age or older. Project staff distributed consent forms and questionnaires. Prospective participants read and signed the consent form and completed the baseline questionnaire independently. This study was conducted with approval of the Emory University Institutional Review Board.
Measures
Participants completed a survey that included measures of knowledge of the donation and transplantation system; attitudes and beliefs regarding donation and transplantation; trust in the healthcare system; religiosity and spirituality; donation intentions; and demographic characteristics. In order to allow for testing of the ODM amongst these items, the following scales were created:
Trust in the allocation system was measured using a 6-item scale. This scale examines participants’ attitudes regarding the existence of discrimination and racism within the allocation system and was adapted from the works of Sander et al. (2005), Rumsey et al. (2003) and McNamara et al. (1999; see Appendix). Participants were asked to indicate their agreement with the statements using a 5-point scale from 1 (strongly disagree) to 5 (strongly agree), such that higher scores indicate greater trust in the organ allocation system. Scores ranged from 9 to 30 (M=20.6, SD=3.7), and α=.66.
Knowledge of the donation and/or transplantation system was assessed with 14 true/false items adapted from the works of Sander and Miller (2005) and Weaver, Spigner, Pineda, Rabun, and Allen (2000). The scale captured different dimensions of knowledge, including: general donation-related statistics, African American donation-related statistics, knowledge of the donation process, knowledge of what signing a donor card means, and knowledge of how medical suitability for donation is determined (see Appendix). We calculated a knowledge score for each participant by counting the number of items for which the participant indicated the correct answer out of 14. Scores ranged from 0 to 14 (M=8.8, SD=2.2).
Religious beliefs related to donation were measured by a single item, “I have been taught that organ donation is against my religion”. Response options for this item ranged from 1 (strongly disagree) to 5 (strongly agree; M=4.3, SD 0.95); thereby, high scores would indicate less support for donation. However, to facilitate ease of interpretation, we reverse scored this negatively worded item such that in all analyses higher scores indicate supportive beliefs related to donation. In other words, for the purposes of analyses, higher scores indicate support for the belief that organ donation is aligned with one’s religion. This variable was highly skewed such that, after recoding, 53% of the participants “strongly agreed” with this item. Thus, we created a dichotomous variable based on whether participants held supportive beliefs related to donation (N=309) or otherwise (N=259). This categorical variable was used in bivariate and multivariate analyses.
We created a 6-item scale that captured attitudes and beliefs about donation and transplantation. This scale included items that measured support for and concerns about donation (DeJong et al., 1998; Sander & Miller, 2005). Response options for these items ranged from 1 (strongly disagree) to 5 (strongly agree), such that higher scores indicate more positive attitudes towards organ and tissue donation. Total scores ranged from 13 to 30 (M=24.2, SD=3.4), and α=.72.
Donation Intentions were measured using a sum of two items: (1) “I am willing to have my organs donated after my death” and (2) “I would be willing to donate an organ to a person of a different race than myself”. Response options for each of these items ranged from 1 (strongly disagree) to 5 (strongly agree). Total scores ranged from 2 to 10 (M=8.1, SD=1.8). These two items were significantly correlated with each other, r(554)=.65, p<.001. Acknowledging apprehensions with formal communication of donation expression (Siminoff et al., 2006), these measures were specifically selected to allow participants to express philosophical support of donation without being confined to a specific mode of documentation (e.g. license, donor card, donor registry).
The last section of the questionnaire included demographic items (e.g., age, gender, race/ethnicity, health insurance status, and marital status).
Data Analyses
Participant demographic characteristics (age, gender, health insurance status and marital status) were analyzed using descriptive statistics. Next, they were analyzed in relationship to each study variable in the model. Pearson correlations were used to explore the relationship between age and each of the continuous variables in the model (i.e., trust in the organ allocation system, knowledge of donation and transplantation, donation-related attitudes, and intentions to serve as a deceased donor). T-tests were used to explore mean differences in each categorical variable in the model (i.e., between men and women and between married and unmarried participants). Finally, we used chi-square to determine whether gender, health insurance status, and marital status were associated with religious beliefs that align with organ donation (yes/no).
Next, ANOVA was conducted to determine whether participants recruited by a given CHA were similar in their donation intentions as compared to participants recruited by another CHA. Using CHA as the independent variable and donation intentions as the dependent variable, ANOVA allowed us to test whether between group variability in donation intentions (across CHA) was greater than within group variability in donation intentions (within CHA). Results from this analysis were significant (p=.01), indicating a need to control for CHA. Thus we created a three category variable that differentiated participants based on the CHA they were recruited by. To create this variable, a mean donation intention score was created for each group of participants recruited by a given CHA. This created a distribution of mean scores ranging from 6.5 to 9.2 (SD=1.8). We then trichotomized this distribution of means into high, medium, and low donation intentions. Participants were grouped based on whether their CHA recruited participants of high, medium, or low donation intentions. This variable was then entered into the path analysis as a control variable.
Before conducting a path analyses, we used correlation to assess bivariate associations among all of the variables in the model. Path analysis was used to test the fit of the proposed model, using the maximum likelihood method within SPSS AMOS 17.0 (Arbuckle, 2008 see ). This statistical tool is used to test direct and indirect paths among observed variables when a single indicator variable is used for each variable (Kline, 1998). It allows researchers to test the magnitude of the hypothesized effects as well as whether the model is consistent with the observed data (Klem, 1995); it is commonly used to test models that are based on the Theory of Reasoned Action/Planned Behavior (Fishbein & Ajzen, 1975; Ajzen, 1985) as is the original Organ Donation Model (Morgan et al. 2003).
Whether the proposed model fit the data was evaluated using the χ2 test as well as additional fit indices that are less sensitive to sample size. The χ2 statistic is used to determine whether the proposed (reduced model) fits the data significantly worse than the saturated model (in which all possible pathways are hypothesized to exist). Kline (1998) recommends dividing the χ2 statistic by the degrees of freedom in studies with large samples as a way for controlling for its sensitivity to sample size; evidence of good model fit is a χ2 statistic less than 3. The additional fit indices we report are the comparative fit index (CFI; values >.05 are desirable; Bentler, 1990); the root square error of approximation (RMSEA; values between .05 and .08 are desirable; Steiger & Lind 1980), and the normed fit index (NFI; values >.80 are desirable; Byrne, 2001). An α of .05 was used to determine statistical significance.
Results
Participant Characteristics
A total of 585 participants completed the survey, the majority of whom were female (69%). Similar proportions of the sample reported that their highest level of education was high school graduate (39%) or college graduate (42%). Similar proportions of participants also reported being single/never married (37%) and married (39%). Participants tended to report working full or part time and having health insurance. Participants ranged in age from 19 to 96 years (M=46.3, SD=14.6; Table 1).
Table 1.
Participant Demographic Characteristics
| Characteristic | N (%) |
|---|---|
| Female | 405 (69.2) |
| Race/Ethnicity | |
| Black/African American | 499 (87.1) |
| Black/Caribbean | 52 (9.1) |
| Black/Hispanic | 10 (1.7) |
| Other | 12 (2.0) |
| Highest level of education completed | |
| Less than high school | 29 (5.1) |
| Completed high school or equivalent GED | 224 (39.4) |
| Completed college | 237 (41.7) |
| Professional degree | 79 (13.9) |
| Employment status | |
| Unemployed | 119 (20.9) |
| Retired | 91 (16.0) |
| Working part or full time | 360 (63.2) |
| Marital status | |
| Never married | 210 (36.9) |
| Married | 223 (39.2) |
| Divorced/separated/widowed | 136 (23.9) |
| Health insurance status | |
| Yes | 447 (78.3) |
Note. Due to missing data, sample size (n) ranges from 552–585.
The next analyses explored the demographic variables in relationship to each of the study variables. Participants who held supportive religious beliefs related to donation tended to be younger (M=44.99) than those who did not (M=47.63; t(551)=2.14, p<.05. Additionally, younger participants were more likely to express supportive donation intentions than older participants (r =−.09, p<.05). Women (M=20.92) were significantly more likely to trust the organ allocation system than men (M=19.98; t(537)=2.79, p<.01 and 2.79, p<.01 respectively). Finally, married participants had more positive attitudes towards deceased organ donation (M=24.66) than non-married participants (M=23.95; t(535)=−2.35 p<.05 and −2.34, p<.05 respectively).
Bivariate and Path Analyses
Results indicated significant positive associations for all hypothesized pathways in the model (see Table 2). The path analysis indicates that the proposed model in Figure1 is an acceptable fit of the data. Results indicate that χ2 (6)=16.25, p=.01. However, when divided by 6, the new χ2 statistic is 2.71, which is in an acceptable range (Kline, 1998). Other fit statistics also indicate good model fit: CFI=.98; NFI=.97; RMSEA=.05. The path analysis supports study hypothesis one: trust in the organ allocation system (β=.29), greater donation knowledge (β=.16), and supportive religious beliefs related to donation (β=.36) are associated with positive attitudes towards donation. In testing the study hypothesis two, positive attitudes toward donation are directly associated with greater intentions to serve as a potential deceased organ donor (β= .56). The study hypothesis three, concerning donation-related knowledge, was also supported in that greater knowledge is directly associated with greater intentions to serve as a potential deceased organ donor (β=.07).
Table 2.
Zero-Order Correlations among Continuous Variables
| Trust in the OTDT process | Knowledge of OTDT | Religious Beliefs | Donation-related attitudes | Donation Intentions | |
|---|---|---|---|---|---|
| Trust in the OTDT process | __ | ||||
| Knowledge of OTDT | −.06 | __ | |||
| Religious Beliefs | .14** | .12** | __ | ||
| Donation-related attitudes | .36** | .16** | .38** | __ | |
| Donation Intentions | .24** | .17** | .30** | .58** | __ |
Note. OTDT = Organ and tissue donation and transplantation; Due to missing data, N ranges from 515–585;
p ≤ .01;
p ≤ .001.
Discussion
This study sought to test a modified version of Morgan and Miller’s Organ Donation Model (2001) by exploring the ways in which trust in the donation/allocation process and religious beliefs impact African Americans’ donation decision making. Results support the modified ODM: Knowledge, trust in the process of organ donation and allocation, and religious beliefs are associated with attitudes, which are, in turn, associated with donation intentions. Of the three predictor variables, religious beliefs related to donation was the variable most strongly correlated variable with attitudes towards donation; this was followed by trust in the donation and allocation process (Figure 1). The significance of these variables speaks to the importance of their inclusion in a model that focuses on deceased donation among the African Americans.
Results of this study suggest that religious beliefs are central to shaping donation attitudes, intentions, and behavior. Because religion and religious institutions maintain a prominent role among African Americans, overcoming religious misconceptions, myths and spiritual concerns are integral to efforts to improve donation rates. The notion of wanting to ‘remain whole’ when transitioning to heaven and fear that donation mutilates the body and inhibits an open casket funeral are some of the religious sentiments that inhibit deceased organ and tissue donation. In other instances, regardless of what religious affiliation a person holds, when their religious perspectives on organ donation are unknown, an unsupportive stance is taken (Gallagher, 1998). Our findings underscore the importance of addressing the influence of religious beliefs and collaborating with religious entities to educate African Americans about donation. Previous research suggests that teaching religious leaders about the stance their religious organization takes and how to talk to parishioners about organ and tissue donation may be a useful point of intervention (Arriola et al., 2007). Specifically, religious leaders and clergy have the ability to positively impact their congregation through sermons, pastoral counseling, and Bible study classes. This influence, in turn, can be used to educate parishioners by clarifying misconceptions, fears of mutilation, and issues of mistrust of the medical system (Atkins, Davis, Holtzman, Durand, & Decker, 2003; Davis et al., 2005; Rumsey et al., 2003).
Distrust of the healthcare system has also been widely cited as one of the most influential barriers to deceased donation (Callender, Miles, & Hall, 2002; Callender, Miles, Hall et al., 2002; Durand et al., 2002; Minniefield et al., 2001; Morgan et al., 2003; Terrell et al., 2004). This fear of exploitation is not thought to be limited to the donation process alone, but expands to influencing how African Americans seek care, whether they participate in medical research, and even in the signing of living wills (Blanchard & Lurie, 2004; Boulware et al., 2003; Corbie-Smith, Thomas, & St. George, 2002; Gamble, 1997; McCaskill-Stevens et al., 1999; Randall, 1996; Siminoff & Arnold, 1999; Wolinsky, 1997). This study found that trust in the donation and allocation system is fundamental in shaping donation attitudes, intentions and behavior. Addressing these concerns about inequalities in the transplant system can be difficult, in part, because of the paradoxical nature of the situation: data clearly show that ethnic minorities are not transplanted at rates equal to that of whites (OPTN, 2010d), yet ethnic minorities must still be encouraged to donate in order to increase the donor pool, and ultimately improve access to organs among all patients. Educational efforts need to address these concerns about inequalities, while not discounting the legitimacy of these apprehensions, by highlighting the overrepresentation of African Americans on the waiting list as well as discussing the development of interventions to improve equal access to care in the transplantation process, and within the broader healthcare system.
Although, knowledge of donation and transplantation was significant, it had the weakest association with attitudes. It may be that more significant findings were masked by the composite nature of the scale, inclusive of different dimensions of knowledge, general statistics, the donation process, what signing a donor card means and medical suitability. Previous research indicates that the relationship between donation-related knowledge and deceased donation intentions is complex and may depend on the specific type of knowledge being measured (Arriola, Robinson, Thompson, & Perryman, 2008).
Limitations
There are several issues that may limit the interpretation and application of our findings. This study utilized a convenience sample of African American participants within the southeastern United States. To ensure a diverse participant pool, we utilized CHAs, who recruited from within their formal and informal networks. This allowed us to recruit participants from diverse backgrounds; however, we were unable to accurately describe the participants who did not enroll in the study, as we did not track the number of contacts each CHA made. Therefore selection bias may be a concern. As a result, participants may have been more homogenous with respect to their thoughts and feelings regarding organ donation than if another recruitment strategy had been utilized. By virtue of their willingness to participate, it might be that participants were generally more supportive of donation than those who did not agree to participate. However, the great variability in donation intentions suggests that this probably was not the case (i.e., the data did not indicate overwhelming support for donation). The cross-sectional ascertainment of study data from a convenience sample, as well as the overrepresentation of women among our sample of participants, may have also impacted the findings. Another limitation is that participants completed a self-administered survey and may have overestimated or underestimated responses related to knowledge, attitudes, or donation intentions, i.e. what participants said they are likely to do in this survey may differ from what they would actually do in a real life situation. Lastly, the use of a single-item to measure religious beliefs related to donation is typically a somewhat crude approach to measure this construct and limits the interpretation of this measure. Based on this item, it cannot be determined as to whether a participant held supportive beliefs about donation or rather his/her religion did not explicitly teach that organ donation was misaligned with their values.
Study Strengths and Significance
A considerable amount of research has been conducted over the past three decades to understand the motivators, attitudes, and barriers to organ donation among ethnic minorities. Specifically regarding African Americans, numerous studies have explored knowledge, beliefs, attitudes, and the cultural reasons for low donation rates, such as a lack of awareness of the need for transplantable organs, mistrust of the health care system, fear of premature death, racism, and religious misconceptions. Despite this research, a true understanding of the interrelationship between these factors and the causal pathway linking them have yet to be truly understood and incorporated in intervention development. Overall, this study makes an important contribution to the existing literature about organ donation by adapting the Organ Donation Model and specifically tailoring it to address the process of African Americans’ donation decision-making. Our research has shown that in addition to the standard variables of knowledge and attitudes, trust and religious beliefs are important components. This study offers new direction for effective education efforts targeting African Americans and their designation of consent for organ donation. The development of interventions that not only address knowledge, but most importantly, issues of trust and concerns with religious beliefs is paramount. The incorporation of these key components may be vital in changing the way that African Americans view the topic of organ donation.
Overcoming the African American disparity in organ donation is vital to increasing donation rates. With the emergence of first-person consent and the exploration of ways to combat the ever increasing waiting list, the emphasis of individual donation decision making is of great importance. First-person consent legislation is acknowledged in forty-eight of fifty states and, perhaps, impacts the largest number of people (UNOS, 2010). This legislation has important implications, specifically for African Americans who tend to be characterized by strong extended family networks. When written documentation exists, it might ameliorate the situation to remove the burden of donation decision from the family.
Acknowledgments
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (1R01DK079713-04). Also, we thank Rianot Amzat and Rhonda DeLaremore for their assistance with data collection and analysis.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (Grant 5 R01 DK79713-3).
Appendix
Trust in the Allocation System Scale
I trust that doctors and hospitals use donated organs as they are intended to be used.
I think that doctors would try just as hard to save my life whether or not I plan to be an organ donor.
People who choose to donate a family member’s organs end up paying extra medical bills.
Racial discrimination prevents minority patients from receiving the organ transplants they need.
Organs can be bought and sold on the black market in the United States.
Given equal need, a poor person has as good a chance as a rich person of getting an organ transplant.
Knowledge of Donation/Transplantation Scale
For most organs, the demand for transplants is higher than the availability.
Organ and tissue donation disfigures the body so an open casket funeral is not possible.
People on the waiting list for a transplant die every day because there are not enough organs available.
African Americans wait longer for kidney transplants than Caucasians.
Almost one-half of the persons waiting for transplants in the U.S. are from minority groups.
People can recover (get better) when they are brain dead.
A person can specify on a donor card what organs and tissues they want to donate.
Most major religions oppose organ and tissue donation.
Signing a donor card will not change the medical treatment I receive to save my life at the hospital.
Anyone can decide to be a donor regardless of their age or medical condition.
It is illegal to sell your organs in the United States.
A large percentage of people who need kidneys are African American.
What percent of the U.S. population is African American?
What percent of people waiting for a life-saving kidney in the U.S. is African American?
Attitudes and Beliefs about Donation and Transplantation Scale
Organ donation is a cause worth supporting.
I think that organ donation is a safe and effective practice.
Organ donation disfigures the body.
In general, I think that organ donation is a good thing.
I believe it is important for a person’s body to have all of its parts when buried.
Organ donation allows for something positive to come out of a person’s death.
Contributor Information
Dana H. Z. Robinson, Department of Behavioral Sciences and Health Education, Rollins School of Public Health of Emory University
Jennie P. Perryman, Policy and Outcomes Management, Emory University Transplant Center
Nancy J. Thompson, Department of Behavioral Sciences and Health Education, Rollins School of Public Health of Emory University
Sandra Amaral, Emory University School of Medicine.
Kimberly R. Jacob Arriola, Department of Behavioral Sciences and Health Education, Rollins School of Public Health of Emory University
References
- Arbuckle JL. AMOS programming reference guide. Small Waters; Chicago: 2008. [Google Scholar]
- Arriola KJ, Perryman JP, Doldren M. Moving beyond attitudinal barriers: Understanding African Americans’ support for organ and tissue donation. Journal of the National Medical Association. 2005;97:339–350. Retrieved from http://www.nmanet.org/index.php/publications_sub/jnma. [PMC free article] [PubMed] [Google Scholar]
- Arriola KJ, Perryman JP, Doldren MA, Warren CM, Robinson DHZ. Understanding the role of clergy in African American organ and tissue donation decision-making. Ethnicity and Health. 2007;12:465–482. doi: 10.1080/13557850701616896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arriola KJ, Robinson DHZ, Thompson NJ, Perryman JP. Project ACTS: An intervention to increase organ and tissue donation intentions among African Americans. Health Education and Behavior. 2010;37:264–274. doi: 10.1177/1090198109341725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arriola KJ, Robinson DHZ, Thompson NJ, Perryman JP. Understanding the relationship between knowledge and African American’s donation decision making. Patient Education and Counseling. 2008;70:242–250. doi: 10.1016/j.pec.2007.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins L, Davis K, Holtzman SM, Durand R, Decker PJ. Family discussion about organ donation among African Americans. Progress in Transplantation. 2003;13:28–32. doi: 10.1177/152692480301300106. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychlogical Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bhengu BR, Uys HH. Organ donation and transplantation within the Zulu culture. Curationis. 2004;27:24–33. doi: 10.4102/curationis.v27i3.995. [DOI] [PubMed] [Google Scholar]
- Blanchard J, Lurie N. R-E-S-P-E-C-T: Patient reports of disrespect in the health care setting and its impact on care. The Journal of Family Practice. 2004;53:721–730. Retrieved from http://www.jfponline.com/ [PubMed] [Google Scholar]
- Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Reports. 2003;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. Retrieved from http://www.publichealthreports.org/index.cfm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulware LE, Ratner LE, Cooper LA, Sosa JA, LaVeist TA, Powe NR. Understanding disparities in donor behavior: Race and gender differences in willingness to donate blood and cadaveric organs. Medical Care. 2002;40(2):85–94. doi: 10.1097/00005650-200202000-00003. [DOI] [PubMed] [Google Scholar]
- Boulware LE, Ratner LE, Sosa JA, Cooper LA, LaVeist TA, Powe NR. Determinants of willingness to donate living related and cadaveric organs: Identifying opportunities for intervention. Transplantation. 2002;73:1683–1691. doi: 10.1097/00007890-200205270-00029. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. Lawrence Erlbaum Associated, Inc; Mahwah, NJ: 2001. [Google Scholar]
- Callender CO. Organ donation in blacks: a community approach. Transplantation Proceedings. 1987;19:1551–1554. [PubMed] [Google Scholar]
- Callender CO, Burston B, Yeager C, Miles PA. A national minority transplant program for increasing donation rates. Transplantation Proceedings. 1997;29:1482–1483. doi: 10.1016/S0041-1345(96)00697-5. [DOI] [PubMed] [Google Scholar]
- Callender CO, Hall MB, Branch D. An assessment of the effectiveness of the Mottep model for increasing donation rates and preventing the need for transplantation--adult findings: program years 1998 and 1999. Seminars in Nephrology. 2001;21:419–428. doi: 10.1053/snep.2001.23778. Retrieved from http://www.seminarsinnephrology.org/ [DOI] [PubMed] [Google Scholar]
- Callender CO, Miles PV, Hall MB. National MOTTEP: Educating to prevent the need for transplantation. Ethnicity and Disease. 2002;12:34–37. Retrieved from http://www.ishib.org/ed_index.asp. [PubMed] [Google Scholar]
- Callender CO, Miles PV, Hall MB, Gordon S. Blacks and Whites and kidney transplantation: A disparity! but why and why won’t it go away? Transplantation Reviews. 2002;16:163–176. doi: 10.1053/trre.2002.127298. [DOI] [Google Scholar]
- Callender CO, Washington AW. Organ/tissue donation the problem! Education the solution: A review. Journal of the National Medical Association. 1997;89:689–693. Retrieved from http://www.nmanet.org/index.php/publications_sub/jnma. [PMC free article] [PubMed] [Google Scholar]
- Chan DCN, Wu AMS, Hung EPW. Invulnerability and the intention to drink and drive: An application of the theory of planned behavior. Accident Analysis and Prevention. 2010;42:1549–1555. doi: 10.1016/j.aap.2010.03.011. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Archives of Internal Medicine. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. Retrieved from http://archinte.ama-assn.org/ [DOI] [PubMed] [Google Scholar]
- Danovitch GM, Cohen DJ, Weir MR, Stock PG, Bennett WM, Christensen LL, Sung RS. Current status of kidney and pancreas transplantation in the United States, 1994–2003. American Journal of Transplantation. 2005;5:904–915. doi: 10.1111/j.1600-6135.2005.00835.x. [DOI] [PubMed] [Google Scholar]
- Darr AR, Randhawa G. Public opinion and perceptions of organ donation and transplantation among Asian communities: An exploratory study in Luton, UK. International Journal of Health Education. 1999;37:68–74. [Google Scholar]
- Davis K, Holtzman S, Durand R, Decker PJ, Zucha B, Atkins L. Leading the flock: Organ donation feelings, beliefs, and intentions among African American clergy and community residents. Progress in Transplantation. 2005;15:211–216. doi: 10.1177/152692480501500303. [DOI] [PubMed] [Google Scholar]
- DeJong W, Franz HG, Wolfe SM, Nathan H, Payne D, Reitsma W, Beasley C. Requesting organ donation: An interview study of donor and nondonor families. American Journal of Critical Care. 1998;7:13–23. Retrieved from http://ajcc.aacnjournals.org/ [PubMed] [Google Scholar]
- Durand R, Decker PJ, Bruder P. Organ Donation among African Americans: Opportunities for Increasing Donor Rates. Hospital Topics. 2002;80:34. doi: 10.1080/00185860209598002. [DOI] [PubMed] [Google Scholar]
- Eng E, Parker E. Natural helper models to enhance a community’s health and competence. In: DiClemente R, Crosby R, Kegler M, editors. Emerging theories in health promotion practice and research. San Francisco: Jossey-Bass; 2002. pp. 126–156. [Google Scholar]
- Gallagher CM. “Hear a just cause, O Lord, attend to my cry”: Organ donation and pastoral care. Journal of Pastoral Care. 1997;51:213–221. doi: 10.1177/002234099705100209. Retrieved from http://www.jpcp.org/ [DOI] [PubMed] [Google Scholar]
- Gallagher CM. Religious outreach for organ and tissue donation. Journal of Transplant Coordination. 1998;8:60–62. doi: 10.7182/prtr.1.8.1.e31h427t8106367g. Retrieved from http://www.medscape.com/viewpublication/130. [DOI] [PubMed] [Google Scholar]
- Gamble VN. Under the shadow of Tuskegee: African Americans and health care. American Journal of Public Health. 1997;87:1773–1778. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 7. Upper Saddle River, NJ: Prentice Hall; 2009. [Google Scholar]
- Ingram KL, Cope JG, Harju BL, Wuensch KL. Applying to graduate school: A test of the theory of planned behavior. Journal of Social Behavior and Personality. 2000;15:215–226. Retrieved from http://www.sbp-journal.com/ [Google Scholar]
- Klem L. Path analysis. In: Grimm LG, Yarnold PR, editors. Reading and understanding multivariate statistics. Washington, DC: American Psychological Association; 1995. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: The Guilford Press; 1998. [Google Scholar]
- Kurz RS, Scharff DP, Terry T, Alexander S, Waterman A. Factors influencing organ donation decisions by African Americans: A review of the literature. Medical Care Research and Review. 2007;64:475–517. doi: 10.1177/1077558707304644. [DOI] [PubMed] [Google Scholar]
- Lam WA, McCullough LB. Influence of religious and spiritual values on the willingness of Chinese-Americans to donate organs for transplantation. Clinical Transplantation. 2000;14:449–456. doi: 10.1034/j.1399-0012.2000.140502.x. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Medical Care Research and Review. 2000;57:146–161. doi: 10.1177/1077558700574007. [DOI] [PubMed] [Google Scholar]
- LifeGift. The word is a lamp unto my feet, and a light unto my path: A biblical perspective to organ and tissue donation. Houston: LifeGift Organ Donation Center; 2002. [Google Scholar]
- Louis ON, Sankar P, Ubel PA. Kidney transplant candidates’ views of the transplant allocation system. Journal of General Internal Medicine. 1997;12:478–484. doi: 10.1046/j.1525-1497.1997.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaskill-Stevens W, Pinto H, Marcus AC, Comis R, Morgan R, Plomer K, Schoentgen S. Recruiting minority cancer patients into cancer clinical trials: A pilot project involving the Eastern Cooperative Oncology Group and the National Medical Association. Journal of Clinical Oncology. 1999;17:1029–1039. doi: 10.1200/JCO.1999.17.3.1029. Retrieved on http://jco.ascopubs.org/ [DOI] [PubMed] [Google Scholar]
- McNamara P, Guadagnoli E, Evanisko MJ, Beasley C, Santiago-Delpin EA, Callendar CO, Christiansen E. Correlates of support for organ donation among three ethnic groups. Clinical Transplantation. 1999;13:45–50. doi: 10.1034/j.1399-0012.1999.t01-2-130107.x. [DOI] [PubMed] [Google Scholar]
- Minniefield WJ, Yang J, Muti P. Differences in attitudes toward organ donation among African Americans and Whites in the United States. Journal of the National Medical Association. 2001;93:372–379. Retrieved from http://www.nmanet.org/index.php/publications_sub/jnma. [PMC free article] [PubMed] [Google Scholar]
- Modlin CS, Bairagi D, Chidmeme-Mundowafa A, Yoo JW, Saffore L. Religious beliefs as a negative predictor of kidney donations in African American men. Journal of Urology. 2009;181:807. Retrieved from http://www.jurology.com/ [Google Scholar]
- Morgan SE. The power of talk: African Americans’ communication with family members about organ donation and its impact on the willingness to donate. Journal of Social and Personal Relationships. 2004;21:112–124. doi: 10.1177/0265407504039845. [DOI] [Google Scholar]
- Morgan SE. Many facets of reluctance: African Americans and the decision (not) to donate organs. Journal of the National Medical Association. 2006;98:695–703. Retrieved from http://www.nmanet.org/index.php/publications_sub/jnma. [PMC free article] [PubMed] [Google Scholar]
- Morgan SE, Miller JK. Beyond the organ donor card: The effect of knowledge, attitudes and values on willingness to communicate about organ donation to family members. Health Communication. 2001;14:121–134. doi: 10.1207/S15327027HC1401_6. [DOI] [PubMed] [Google Scholar]
- Morgan SE, Miller JK. Communicating about gifts of life: The effect of knowledge, attitudes, and altruism on behavior and behavioral intentions regarding organ donation. Journal of Applied Communication Research. 2002;30:163–178. doi: 10.1080/00909880216580. [DOI] [Google Scholar]
- Morgan SE, Miller JK, Arasaratnam LA. Similarities and differences between African Americans’ and European Americans’ attitudes, knowledge, and willingness to communicate about organ donation. Journal of Applied Social Psychology. 2003;33:693–715. doi: 10.1111/j.1559-1816.2003.tb01920.x. [DOI] [Google Scholar]
- Organ Procurement and Transplant Network (OPTN) Current US waiting list, overall by organ. U.S Department of Health and Human Services, Health Resources and Services Administration; 2010a. Retrieved July 26 2010, from http://optn.transplant.hrsa.gov/latestData/step2.asp. [Google Scholar]
- Organ Procurement and Transplant Network (OPTN). Transplants by donor type, US transplants Performed: January 1, 1988– April 30, 2010. U.S Department of Health and Human Services, Health Resources and Services Administration; 2010b. Retrieved July 26, 2010, from http://optn.transplant.hrsa.gov/latestData/rptData.asp. [Google Scholar]
- Organ Procurement and Transplant Network (OPTN). Donors recovered in the US by donor type: January 1, 1988– April 30, 2010. U.S Department of Health and Human Services, Health Resources and Services Administration; 2010c. Retrieved July 26, 2010, from http://optn.transplant.hrsa.gov/latestData/step2.asp. [Google Scholar]
- Organ Procurement and Transplant Network (OPTN) Transplants in the US by recipient ethnicity, US Transplants Performed: January 1, 1988– April 30, 2010. U.S Department of Health and Human Services, Health Resources and Services Administration; 2010d. Retrieved July 26, 2010, from http://optn.transplant.hrsa.gov/latestData/rptData.asp. [Google Scholar]
- Radecki CM, Jaccard J. Psychological aspects of organ donation: A critical review and synthesis of individual and next-of-kin donation decisions. Health Psychology. 1997;16:183–195. doi: 10.1037/0278-6133.16.2.183. [DOI] [PubMed] [Google Scholar]
- Radecki CM, Jaccard J. Signing an organ donation letter: The prediction of behavior from behavioral intentions. Journal of Applied Social Psychology. 1999;29:1833–1853. doi: 10.1111/j.1559-1816.1999.tb00154.x. [DOI] [Google Scholar]
- Randall VR. Slavery, segregation and racism: Trusting the health care system ain’t always easy! An African American perspective on bioethics. Saint Louis University Public Law Review. 1996;15:191–235. Retrieved from http://law.slu.edu/journals/LawReview/ [PubMed] [Google Scholar]
- Randhawa G. The challenge of kidney transplantation among minority ethnic groups in the UK. EDTNA/ERCA Journal. 2004;30:182–187. doi: 10.1111/j.1755-6686.2004.tb00365.x. [DOI] [PubMed] [Google Scholar]
- Rozon-Solomon M, Burrows L. ‘Tis better to receive than to give: The relative failure of the African American community to provide organs for transplantation. The Mount Sinai Journal of Medicine. 1999;66:273–276. Retrieved from http://mountsinai.site-ym.com/?page=Journal_of_Medicine. [PubMed] [Google Scholar]
- Rumsey S, Hurford DP, Cole AK. Influence of knowledge and religiousness on attitudes toward organ donation. Transplantation Proceedings. 2003;35:2845–2850. doi: 10.1016/j.transproceed.2003.10.078. [DOI] [PubMed] [Google Scholar]
- Sander S, Miller B. Public knowledge and attitudes regarding organ and tissue donation: An analysis of the northwest Ohio community. Patient Education and Counseling. 2005;58:154–163. doi: 10.1016/j.pec.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Schutte L, Kappel D. Barriers to donation in minority, low-income, and rural populations. Transplantation Proceedings. 1997;29:3746–3747. doi: 10.1016/S0041-1345(97)01096-8. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Arnold R. Increasing organ donation in the African-American community: Altruism in the face of an untrustworthy system. Annals of Internal Medicine. 1999;130:607–609. doi: 10.7326/0003-4819-130-7-199904060-00023. Retrieved from http://www.annals.org/ [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. Journal of General Internal Medicine. 2006;21(9):995–1000. doi: 10.1111/j.1525-1497.2006.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stage FK, Carter HC, Nora A. Path analysis: An introduction and analysis of a decade of research. Journal of Educational Research. 2004;98:5–12. Retrieved from http://www.tandf.co.uk/journals/journal.asp?issn=0022-0671&linktype=1. [Google Scholar]
- Steiger JH, Lind JM. Statistically based tests for the number of common factors. IA: Iowa City; 1980. [Google Scholar]
- Streiner DL. Finding our way: An introduction to path analysis. Canadian Journal of Psychiatry. 2005;50:115–122. doi: 10.1177/070674370505000207. Retrieved from http://publications.cpa-apc.org/browse/sections/0. [DOI] [PubMed] [Google Scholar]
- Terrell F, Moseley KL, Terrell AS, Nickerson KJ. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. Journal of the National Medical Association. 2004;96:53–60. Retrieved from http://www.nmanet.org/index.php/publications_sub/jnma. [PMC free article] [PubMed] [Google Scholar]
- United Network for Organ Sharing (UNOS). Donor designation (first person consent) status by state. 2010 Retrieved July 26, 2010, from http://www.unos.org/inTheNews/factsheets.asp?fs=6.
- U.S. Renal Data System (USRDS). 2009 Retrieved July 26, 2010, from www.usrds.org.
- U.S. Census Bureau. American Fact Finder. 2010 Retrieved May 18, 2010, from www.census.gov.
- Wagstaff DA, Korda H, McCleary KJ. African Americans’ organ donor intentions: Who has used which registration mode to express her or his intentions? Journal of Public Health Management and Practice. 2008;14:E7–E13. doi: 10.1097/01.PHH.0000303420.83518.65. [DOI] [PubMed] [Google Scholar]
- Washington HA. Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. New York: Doubleday Broadway Publishing Group; 2006. [Google Scholar]
- Watkins CE, Terrell F, Miller FS, Terrell SL. Cultural mistrust and its effects on expectational variables in Black client-White counselor relationships. 1989 doi: 10.1037/0022-0167.36.4.447. [DOI] [Google Scholar]
- Weaver M, Spigner C, Pineda M, Rabun KG, Allen MD. Knowledge and opinions about organ donation among urban high school students: Pilot test of a health education program. Clinical Transplantation. 2000;14:292–303. doi: 10.1034/j.1399-0012.2000.140404.x. [DOI] [PubMed] [Google Scholar]
- Wolinsky H. Steps still being taken to undo damage of “America’s Nuremberg”. Annals of Internal Medicine. 1997;127(4):143–44. Retrieved from http://www.annals.org/ [PubMed] [Google Scholar]
- Wuensch KL. Conducting a path analysis with SPSS/AMOS. 2008 Available at http://core.ecu.edu/psyc/wuenschk/StatsLessons.htm Retrieved March 14, 2011.
- Young CJ, Gaston RS. African Americans and renal transplantation: Disproportionate need, limited access, and impaired outcomes. The American Journal of the Medical Sciences. 2002;323:94–99. doi: 10.1097/00000441-200202000-00007. Retrieved from http://journals.lww.com/amjmedsci/pages/default.aspx. [DOI] [PubMed] [Google Scholar]