Abstract
Objective
To determine if less severe depression spectrum diagnoses such as dysthymia, as well as depression, are associated with risk of developing dementia and mortality in a “real world” setting.
Design
Retrospective cohort study conducted using the Department of Veterans Affairs (VA) National Patient Care Database (1997-2007).
Setting
VA medical centers in the United States.
Participants
A total of 281,540 veterans 55 years and older without dementia at study baseline (1997-2000).
Measurements
Depression status and incident dementia were ascertained from ICD-9 codes during study baseline (1997-2000) and follow-up (2001-2007), respectively. Mortality was ascertained by time of death dates in the VA Vital Status File.
Results
Ten percent of veterans had baseline diagnosis of depression and nearly 1% had dysthymia. The unadjusted incidence of dementia was 11.2% in veterans with depression, 10.2% with dysthymia and 6.4% with neither. After adjusting for demographics and comorbidities, patients diagnosed with dysthymia or depression were twice as likely to develop incident dementia compared to those with no dysthymia/depression (adjusted dysthymia hazard ratio [HR]: 1.96, 95% confidence interval [CI]: 1.71-2.25; and depression HR: 2.18, 95% CI: 2.08-2.28). Dysthymia and depression also were associated with increased risk of death (31.6% dysthymia and 32.9% depression vs 28.5% neither; adjusted dysthymia HR: 1.41, 95% CI: 1.31-1.53; and depression HR: 1.47, 95% CI: 1.43-1.51).
Conclusions
Findings suggest that older adults with dysthymia or depression need to be monitored closely for adverse outcomes. Future studies should determine whether treatment of depression spectrum disorders may reduce risk of these outcomes.
Keywords: Dysthymia, Depression, Dementia, Mortality
Introduction
Major depression is common in older adult populations1 and associated with impaired physical, mental, and social functioning.2-4 Two of the most insidious, but under recognized, associated outcomes of depression are dementia and mortality. Depressive symptoms are prevalent in dementia, and converging evidence suggests it may be a risk factor or prodrome of dementia5-11 although this remains controversial.12-15 Further, there exists conflicting evidence of depression increasing the risk of mortality in the elderly population.16-23 Interestingly, to our knowledge, no study has investigated if less severe depression spectrum diagnosis, i.e., dysthymia, increases risk of dementia and mortality.
Because both dysthymia and depression (usually considered major depression) are common and treatable disorders, thorough investigation of their association to dementia and mortality is imperative. In fact, recent studies have shown that treatment of depression leads to improved memory and cognitive performance,24,25 suggesting if a relationship is found between dysthymia and risk of dementia and death that treatment of lower threshold depression could potentially improve cognition, prevent the onset of dementia, or prolong life. The Veterans Affairs (VA) Veterans Health Administration Data provides an important resource to this study, as depression is prominent in veterans.26 And, as the largest national health care system, carefully collected data from VA medical centers on diagnoses of depression and confounding variables provides the precision and power to test intricate models (e.g., models with medical comorbidities, such as cardiovascular and psychiatric condition2,27-29). In other studies, investigation has been limited by sample size and lack of clinical diagnoses.6
The objective of our study was to determine if dysthymia and depression were associated with an increased risk of being diagnosed with dementia and risk of death among older veterans in the U.S. In addition, we considered death as a competing risk,30 given it may preclude the occurrence of dementia in an elderly population.
Methods
Data and Participants
Data for this retrospective cohort study were obtained from the Department of Veterans Affairs (VA) National Patient Care Database, which captures all inpatient and outpatient services within the VA fiscal year (October 1 through September 30). Records were extracted for veterans aged 55 years and older who had been seen at either inpatient or outpatient VA health care facilities between 1997 and 2000 (our study baseline). Two additional inclusion criteria were implemented to obtain our study cohort: 1) no diagnosis of dementia during the baseline period, fiscal years 1997 through 2000; and 2) at least one visit during the follow-up period from fiscal year 2001 (October 1, 2000) to the end of the calendar year 2007. Of the 385,047 available for study, we excluded the 49,675 (13%) who died during the baseline period and 53,832 (14%) who were not seen at a VA health care facility during the follow-up period as we did not have the ability to determine whether they developed incident dementia or if they died. Thus, our final study cohort included 281,540 veterans.
The Committee on Human Research at the University of California, San Francisco, the Committee for Research and Development at the San Francisco VA and the Human Research Protection Office of the U.S. Army Medical Research and Materiel Command approved the study.
Measures
Depression Status
Veterans with baseline depression or dysthymia were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes recorded in the VA database. Depression was determined by ICD-9-CM codes 296.2, 296.3 (major depressive disorder), and 311 (depression not otherwise specified). Dysthymia was determined by a separate diagnosis, ICD-9 code 300.4 (dysthymic disorder). VA and non-VA studies with common risk factors have used similar definitions of depression,31,32 and dysthymia.33 A three level categorical variable of dysthymia, depression, and no dysthymia/depression diagnosis was created from these ICD-9-CM codes. If a veteran had both a depression and dysthymia diagnosis during the baseline period, they were considered to have met criteria for depression.
Dementia and Mortality
Veterans with dementia were identified using ICD-9-CM codes, including diagnosis codes 290.0, 290.2, 290.3, 331.2 (senile dementia), 290.4 (vascular dementia), 294.8 (dementia not otherwise specified), 331.0 (Alzheimer's Disease), 331.1 (frontotemporal dementia), and 331.82 (Lewy body dementia). These codes were applied during the baseline period to exclude prevalent cases and during the follow-up period to identify incident cases of dementia between October 1, 2000 and December 31, 2007. Diagnosis of dementia included any one of these codes.
Date of death was determined by dates in the VA Vital Status File. The Vital Status File combines death data from the VA, the Center for Medicare and Medicaid Services, and the Social Security Administration.34
Baseline Characteristics
Demographic Variables
VA database records had available information on age and gender. We used 2000 U.S. Census Data to classify veterans as living in broad educational and income strata according to zip code tabulation areas (ZCTA).35 Education was defined as a two level variable categorized according to whether veterans were living in a ZCTA where ≤25% versus >25% of the adult population had completed a college education (bachelor's degree or higher). Income was defined as a three level variable categorized in tertiles of median ZCTA income for adults <75 or ≥75 years old.
Comorbidities
Neuropsychiatric and behavioral conditions were coded from ICD-9-CM codes including diagnoses of posttraumatic stress disorder (PTSD), bipolar disorder, anxiety, head injury, alcohol abuse, and drug abuse (including tobacco). Medical comorbidities related to cardiovascular disease (CVD) included diagnoses of hypertension, diabetes, myocardial infarct, and cerebrovascular events (i.e., stroke or transient ischemic attack).
Statistical Analyses
We conducted descriptive and bivariate analyses of the baseline data. Baseline characteristics were summarized using means and standard deviations or frequencies and proportions for veterans with dysthymia, depression, and those without depression/dysthymia. The statistical significance of differences between the three groups was tested by F tests for continuous variables and chi-square tests for categorical variables.
For longitudinal analyses, follow-up time was calculated from the date of diagnosis of dysthymia or depression (i.e., sometime during the baseline period, 1997-2000) until the date of diagnosis of dementia or mortality (post-2000). In all final analyses, the time scale was defined by age.
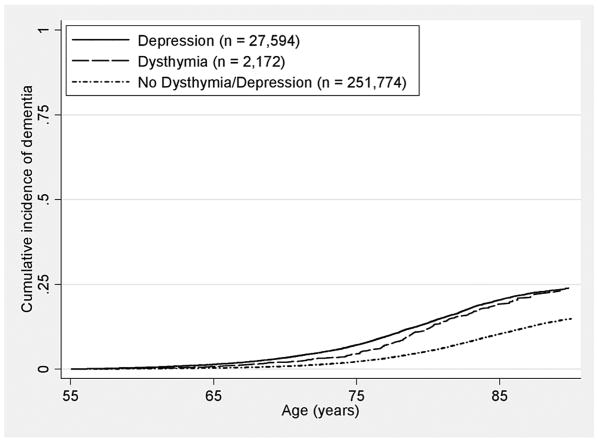
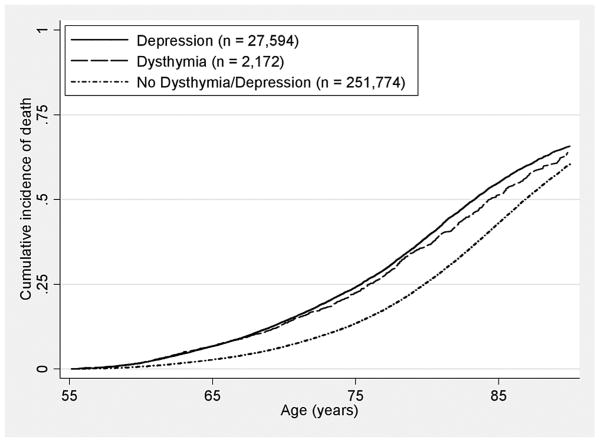
Cumulative incidence of dementia was plotted by patient age in years for each depression group. These curves show estimates of the cumulative incidence by age in the presence of death as a competing risk with complete follow up; this could be estimated by the simple proportion with a dementia diagnosis by any given age. This is in contrast to Kaplan-Meier curves, which estimate the incidence that would be observed if the competing risk could be “removed.” In addition, cumulative incidence of death was plotted by age in the presence of dementia as a competing event.
Cox proportional cause-specific hazards models were used to compare the age in years of incident dementia and death (defined by the event that occurred first) in patients with dysthymia and depression versus those without dysthymia/depression. Hazard ratios were estimated for the association between baseline depression status and risk of dementia and death in unadjusted and multivariable adjusted models. To determine whether the association was independent of demographic, medical and neuropsychiatric comorbidities, we conducted three stages of multivariable Cox regression models as follows: 1) adjusted for demographic characteristics (gender, educational and income strata) to establish a baseline model; 2) adjusted for demographic variables and medical comorbidities related to cardiovascular disease (CVD: hypertension, diabetes, myocardial infarct, and cerebrovascular disease); and 3) adjusted for demographic variables, CVD, and behavioral and neuropsychiatric conditions (alcohol abuse, drug abuse, bipolar disorder, PTSD, anxiety, and head injury).
Additional analyses were performed to examine associations of dysthymia and depression with specific dementia subtypes including Alzheimer's disease, senile dementia, vascular dementia and dementia not otherwise specified. In addition, sensitivity analyses were performed to test the integrity of findings by first applying a more conservative definition for depression status—depression and dysthymia were defined by ICD-9 clinical diagnoses codes on at least two different visits during the baseline period, excluding those with only one diagnosis (n = 11,265). In a second set of models, patients with schizophrenia or schizoaffective disorder or bipolar disorder were excluded in order to remove potential bias, because patients with more serious mental illness likely have different prognoses,36 and possibly a heightened risk of dementia and death.
Proportional hazards assumption was evaluated graphically and statistically and determined to be satisfied for all models. Statistical tests for models were two-tailed with p < 0.01 defining statistical significance. This was determined by correcting for our four primary tests [i.e., testing the association of (1) depression and (2) dysthymia to risk of developing dementia and the association of (3) depression and (4) dysthymia to risk of mortality] using the Bonferroni correction and maintaining an overall Type I error rate of 0.05. In this case, we would conduct each of the individual tests at a Type I error rate of 0.05/4 or 0.01. All analyses were performed using Stata version 10.1 (StataCorp LP, College Station, Texas) and SAS version 9.2 (SAS Institute Inc, Cary, North Carolina).
Results
At baseline, approximately 9.8% of the veterans had a current diagnosis of depression and 0.8% were diagnosed with dysthymia. The demographic, medical and neuropsychiatric characteristics of the 281,540 veterans in our cohort by depression spectrum diagnoses are presented in Table 1. The mean age was 69.7 years (SD 8.2). Four percent were female (n = 11,301). Compared to veterans with no depression spectrum diagnosis, those with dysthymia or depression were significantly younger but were more likely to have a comorbid medical diagnoses (hypertension, diabetes, myocardial infarctions, and cerebrovascular disease) or neuropsychiatric diagnoses (alcohol abuse, drug abuse, bipolar disorder, PTSD, anxiety, and head injury). In addition, they were more likely to live in zip codes with less college-educated and higher mid-income individuals, although absolute differences were quite small (Table 1). Gender was not associated with either depression or dysthymia.
Table 1. Baseline Characteristics of Veterans with Dysthymia, Depression, and No Dysthymia/Depression.
| Characteristic | No Dysthymia/Depression (n = 251,774) | Dysthymia (n = 2,172) | Depressiona (n = 27,594) | df, pb |
|---|---|---|---|---|
| Age, y, mean (SD)c | 70.0 (8.2) | 67.3 (8.4) | 67.1 (8.1) | 2, <0.001 |
| Age range, y, n (%) | 6, <0.001 | |||
| 55-64 | 73,262 (29.1) | 921 (42.4) | 12,159 (44.1) | |
| 65-74 | 103,512 (41.1) | 773 (35.6) | 10,033 (36.4) | |
| 75-84 | 69,464 (27.6) | 458 (21.1) | 5,102 (18.5) | |
| ≥85 | 5,536 (2.2) | 20 (0.9) | 300 (1.1) | |
| Male, n (%) | 241,702 (96.0) | 2,086 (96.0) | 26,451 (95.9) | 2, 0.52 |
| Education of ZCTAd, n (%) | ||||
| >25% college-educated | 74,261 (29.5) | 637 (29.3) | 7,874 (28.5) | 2, <0.001 |
| Income (median) of ZCTAd,e, n (%) | 4, <0.001 | |||
| Low tertile (<$23.8K) | 80,197 (31.9) | 671 (30.9) | 8,481 (30.7) | |
| Middle tertile | 82,233 (32.7) | 725 (33.4) | 9,216 (33.4) | |
| High tertile (>$31.5K) | 80,046 (31.8) | 678 (31.2) | 8,696 (31.5) | |
| Comorbidities, n (%) | ||||
| Hypertension | 144,027 (57.2) | 1,469 (67.6) | 19,424 (70.4) | 2, <0.001 |
| Diabetes | 58,325 (23.2) | 606 (27.9) | 8,153 (29.6) | 2, <0.001 |
| Myocardial infarct | 13,247 (5.3) | 204 (9.4) | 2,662 (9.7) | 2, <0.001 |
| Cerebrovascular disease | 22,649 (9.0) | 290 (13.4) | 4,482 (16.2) | 2, <0.001 |
| Alcohol abuse | 7,430 (3.0) | 210 (9.7) | 3,670 (13.3) | 2, <0.001 |
| Drug abuse | 26,115 (10.4) | 448 (20.6) | 7,425 (26.9) | 2, <0.001 |
| Bipolar Disorder | 1,390 (0.6) | 129 (5.9) | 2,659 (9.6) | 2, <0.001 |
| PTSD | 2,602 (1.0) | 299 (13.8) | 3,228 (11.7) | 2, <0.001 |
| Anxiety | 9,521 (3.8) | 802 (36.9) | 9,318 (33.8) | 2, <0.001 |
| Head injury | 4,069 (1.6) | 68 (3.1) | 1,187 (4.3) | 2, <0.001 |
Depression includes MDD or Depression NOS without Dysthymia.
P-value based on F test for continuous variables and χ2 test for categorical variables comparing across depression status.
Denominator df for the F-test of age (continuous) is 281,537.
Zip Code Tabulation Area from the 2000 census (3.8% of data missing).
Median income levels are age-specific (<75 years and ≥75 years calculated separately).
Risk of Dementia
Cumulative incidence rates of dementia were significantly higher for veterans with dysthymia and depression compared to those without dysthymia/depression. Veterans without either diagnosis had a 7-year incident dementia cumulative rate of 6.4%, while veterans with a diagnosis of dysthymia had a 7-year rate of 10.2% and veterans with a diagnosis of depression had a rate of 11.2% (χ2 = 942.2, df = 2, p < 0.001). Incident dementia rates were higher for patients with dysthymia and depression than those with no depression throughout the follow-up period of an average of 7.2 years (Figure 1). Dysthymic or depressed patients were over twice as likely to develop incident dementia compared to those without dysthymia/depression (unadjusted dysthymia hazard ratio [HR]: 2.35, 95% confidence interval [CI]: 2.06-2.69, Wald χ2 = 159.7, df = 1, p < 0.001; and depression HR: 2.88, 95% CI: 2.78-3.00, Wald χ2 = 2894.8, df = 1, p < 0.001).
Figure 1. Cumulative Incidence of Dementia by Age.
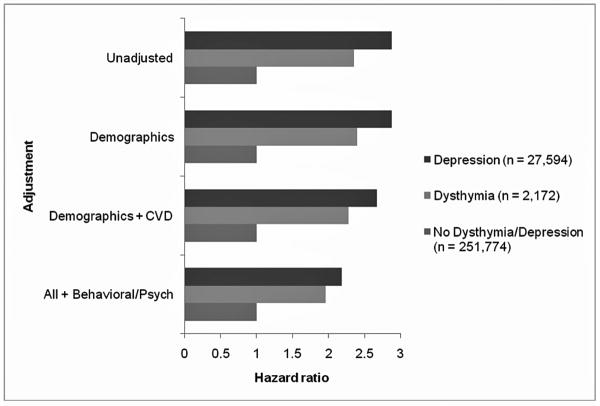
Figure 2 shows the unadjusted and adjusted cause-specific hazard ratios for dementia. These estimates were based on Cox proportional hazards models using age as the time scale. After adjusting for demographic variables of gender, education, and income, results were similar to the unadjusted hazard ratios (dysthymia HR: 2.40, 95% CI: 2.09-2.74, Wald χ2 = 160.2, df = 1, p < 0.001; and depression HR: 2.88, 95% CI: 2.76-2.99, Wald χ2 = 2740.6, df = 1, p < 0.001). The addition of medical comorbidities to this model only slightly altered hazard ratios (dysthymia HR: 2.28, 95% CI: 1.99-2.61, Wald χ2 = 142.5, df = 1, p < 0.001; and depression HR: 2.67, 95% CI: 2.57-2.79, Wald χ2 = 2330.9, df = 1, p < 0.001). Further adjustment for behavioral and neuropsychiatric diagnoses reduced the magnitude of the association somewhat; however, patients who were diagnosed with dysthymia or depression were still twice as likely to develop incident dementia (dysthymia HR: 1.96, 95% CI: 1.71-2.25, Wald χ2 = 91.6, df = 1, p < 0.001; and depression HR: 2.18, 95% CI: 2.08-2.28, Wald χ2 = 1105.9, df = 1, p < 0.001).
Figure 2.
Association between Depression Status and Risk of Dementia in Older Veterans Abbreviations: CVD = medical comorbidities related to cardiovascular disease; hazard ratio (HR) of 1 = reference group, i.e., veterans with no dysthymia/depression.
Results were similar when examined by sub-types of dementia (not shown). Alzheimer's Disease, senile dementia, vascular dementia, and dementia not otherwise specified were statistically significantly associated to dysthymia and depression after adjustment for demographics, cardiovascular conditions, and behavioral and psychiatric conditions and of similar magnitudes.
In sensitivity analyses, we first examined the effect of restricting depression and dysthymia to at least two clinical diagnoses. We found almost identical results for dysthymia and depression, where in the final fully-adjusted model patients with at least two dysthymia (n = 1,604) or two depression (n = 16,897) diagnoses remained twice as likely to develop incident dementia (dysthymia HR: 2.01, 95% CI: 1.72-2.35, Wald χ2 = 75.8, df = 1, p < 0.001; and depression HR: 2.13, 95% CI: 2.01-2.26, Wald χ2 = 656.5, df = 1, p < 0.001). In a second set of analyses, we excluded patients with schizophrenia or schizoaffective disorder (n = 5,016) or bipolar disorder (n = 3,581). We found that the magnitude and statistical significance of the HRs for dysthymia and depression remained similar to the original models.
Risk of Death
Cumulative incidence rates of death were also significantly higher for veterans with dysthymia and depression than those without dysthymia/depression. Veterans without a diagnosis had a 7-year rate of 28.5%, while those with a diagnosis of dysthymia had a rate of 31.6% and veterans with a diagnosis of depression had a rate of 32.9% (χ2 = 236.5, df = 2, p < 0.001). Mortality rates were higher for patients with dysthymia and depression throughout the follow-up period (Figure 3). The unadjusted hazard ratios for death were 1.58 (95% CI: 1.47-1.70, Wald χ2 = 141.9, df = 1, p < 0.001) for dysthymia and 1.79 (95% CI: 1.75-1.83, Wald χ2 = 2696.4, df = 1, p < 0.001) for depression versus no dysthymia/depression.
Figure 3. Cumulative Incidence of Death by Age.
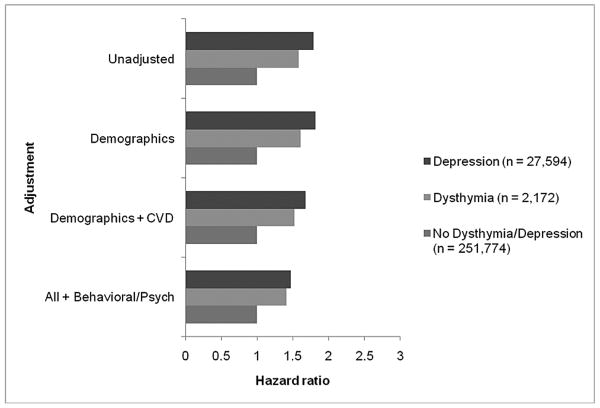
Figure 4 shows the unadjusted and adjusted cause-specific hazard ratios for death. As with dementia, results remained similar after adjusting for demographic variables (dysthymia HR: 1.61, 95% CI: 1.49-1.74, Wald χ2 = 148.3, df = 1, p < 0.001; and depression HR: 1.81, 95% CI: 1.77-1.85, Wald χ2 = 2692.5, df = 1, p < 0.001). Addition of covariates to this model, particularly behavioral and neuropsychiatric measures, accounted for some of the observed association between depression status and death. Yet, both dysthymia and depression remained independently and significantly associated with increased risk of death after adjustment for these factors (dysthymia HR: 1.41, 95% CI: 1.31-1.53, Wald χ2 = 75.8, df = 1, p < 0.001; and depression HR: 1.47, 95% CI: 1.43-1.51, Wald χ2 = 902.9, df = 1, p < 0.001).
Figure 4.
Association between Depression Status and Risk of Mortality in Older Veterans Abbreviations: CVD = medical comorbidities related to cardiovascular disease; hazard ratio (HR) of 1 = reference group, i.e., veterans with no dysthymia/depression.
When we examined the effect of restricting depression and dysthymia to at least two clinical diagnoses the results were similar. The same was true when we excluded patients with schizophrenia or schizoaffective disorder or bipolar disorder.
Conclusions
In this study of primarily male veterans, we found that both patients diagnosed with dysthymia and those diagnosed with depression had more than a two-fold increased risk of dementia diagnosis compared to those without dysthymia or depression. In addition, the risk of death was over 40% higher for those with dysthymia or depression compared to patients without either disorder. Compared to those with no dysthymia/depression diagnosis, risk of dementia and mortality associated with dysthymia or depression remained high regardless of age. Furthermore, these associations remained after adjustment for important factors, such as demographic variables and cardiovascular and psychiatric comorbidities.
Although prior research on the relationship of depression to risk of dementia and mortality has been mixed,5-23 our results provide evidence supporting longitudinal studies that have found an association between depression and risk of cognitive decline or dementia5-11 and mortality.16-21 However, unlike our study, to date few longitudinal studies have examined this relationship with adjustment for medical and neuropsychiatric disorders including cardiovascular diagnoses, or have used diagnostic measures to assess depression and dysthymia. Previous longitudinal work from our group investigating depressive symptoms in a cohort of community-dwelling older adults found that depressive symptoms at baseline were associated with an increased risk of mild cognitive impairment at follow up, even after adjustment for vascular disease.7 Additionally, a recent longitudinal study found a strong relationship between subsyndromal depressive symptoms and incident cognitive impairment over 9 years in women aged 70 years and older,11 adjusting for cardiovascular disorders. Our present findings suggest similar results to these studies, but instead of depressive symptoms we found that a clinical diagnosis of dysthymia and depression increased risk of dementia.
As important, our results on dysthymia support the hypothesis that diagnosis of major depression does not capture the full range of depressive phenomena that has clinical relevance in late life.37 Thus, our findings provide evidence that the larger spectrum of depression is associated with increased risk of dementia and death. It is possible that depression or subthreshold depression is a prodrome for dementia,38 or is associated with an intermediary process that then leads to cognitive deficit (e.g., subthreshold vascular disease, which leads to neurodegenerative cerebral lesions,28,39 or high levels of cortisol may be associated with depression and may also lead to neuronal death and cognitive decline).9 Thus, depression may be part of the same disease process that produces dementia, or a separate process that is directly associated with an increased risk for cognitive decline. The relationship of depression to risk of death may be explained by motivational depletion (i.e., individuals who “give up” are likely to disengage from preventive and potentially restorative health behaviors).19 On the other hand, studies examining biological pathways between depression and mortality have suggested potential mediating effects of vascular disease and vascular indicators of disease.40
Our study has several important strengths, including the application of a longitudinal study design in a large, national sample of patients aged 55 years and older. The VA National Patient Care Database provided detailed records of medical and psychiatric disorders, an advantage over self-report data that is subject to recall bias. In particular, the data allowed for documentation of dementia diagnosis up to 7 years of care. We also carefully adjusted for possible confounding from cardiovascular and neuropsychiatric comorbidities and accounted for the competing and independent risk of death. Of note, the maintenance of the magnitude of association and statistical significance upon addition of other psychiatric and behavioral disorders to the models may be explained in part by an acceptable amount of collinearity (r < 0.25) between depression and these disorders (e.g., alcohol abuse and PTSD); therefore, explaining a similar amount of variability in risk of dementia. In addition, most other studies have not assessed competing risks, which have been found to be important to consider explicitly in elderly populations.30 Finally, this study is the first, to our knowledge, that has reported that dysthymia may increase risk of developing dementia and mortality.
An additional strength is that our study adds to the literature by using “real world” clinical diagnoses assessed in a “real world” health care system. The majority of prior epidemiological research examined depression and dementia assessed by diagnostic algorithms based on symptom scales (e.g., for depression using CES-D, GDS, and for dementia using MMSE, 3MS).7,10-14 Our study used ICD-9 codes available through the VHA claims data determined mostly by primary care clinicians. Additionally, our results convey the seriousness of a dysthymia diagnosis to nonmental health clinicians. Of note, clinician ICD-9 codes also have their disadvantages, because they are an insensitive assessment of symptoms compared with structured research diagnostic interviews. Still, ICD-9 codes are standard measures that are more than a physiologic endpoint, i.e., the diagnosis of dementia is a profoundly important event for patients, families, and health systems.
Other limitations of our study are also important to mention. Our study population included mainly male veterans followed by the VA system. Thus, we need to determine if our findings generalize to female veterans, veterans not cared for at VA medical centers and non-veterans. In addition, the validity of diagnoses could not be confirmed. Further, we did not have medication data available to assess antidepressant use. Some studies have shown that treatment of depression in elderly patients (i.e., pharmacological, behavioral, or other modalities) improves cognition.24,25 However, whether treatment of dysthymia can delay or prevent cognitive decline remains to be studied.
The findings of this study emphasize the importance of closely monitoring all levels of depression for development of dementia and risk of death. Further study of potential mechanisms linking dysthymia and depression to adverse outcomes including dementia and mortality is required in order to target intervention, prevention, and health care needs. Given the rapid aging of the U.S. population, it is imperative that the diagnosis and successful treatment of depression, as well as dysthymia, is achieved in order to improve the health and outcomes of elders with depression spectrum disorders.
Acknowledgments
Study funding: This work was supported by the Department of Defense (W81XWH-05-2-0094 [KY]) and the National Institute of Mental Health (K01 MH079093 [ALB]). Dr. Yaffe and Dr. Covinsky are supported in part by K24 Midcareer Investigator Awards from the National Institute on Aging (AG031155 [KY] and AG029812 [KEC]). Dr. Barnes was supported in part by NARSAD.
Disclaimer: We acknowledge that the original collector of the data, sponsoring organizations, agencies, or the U.S. government bear no responsibility for use of the data or for interpretations or inferences based upon such uses. The views and opinions expressed in this report are those of the authors and should not be construed otherwise.
Footnotes
Previous Presentation: Portions of the manuscript were presented at the Veterans Affairs Health Services Research & Development (HSR&D) National Meeting on Mental Health and Substance Use Disorders; April 29, 2010; Little Rock, Arkansas. In addition, portions of the manuscript were presented at the Alzheimer's Association International Conference on Alzheimer's Disease (ICAD); July 13, 2010; Honolulu, Hawaii.
Conflicts of interest: Dr. Byers, Dr. Covinsky, and Dr. Barnes report no financial relationships with commercial interests. Dr. Yaffe reports having served as a consultant to Novartis, Inc. for reasons not related to the current project, and she serves on DSMB committees for Pfizer and for Medivation, Inc. The authors have no competing interests, including specific financial interests or relationships or affiliations relevant to the subject of this manuscript.
Author Contributions: Dr. Byers had full access to all the data in the study. She conducted the data analysis, and takes responsibility for the integrity of the data and the accuracy of the statistical results.
Contributor Information
Amy L. Byers, Department of Psychiatry, University of California, San Francisco and San Francisco Veterans Affairs Medical Center.
Kenneth E. Covinsky, Department of Medicine, University of California, San Francisco and San Francisco Veterans Affairs Medical Center.
Deborah E. Barnes, Department of Psychiatry, University of California, San Francisco and San Francisco Veterans Affairs Medical Center.
Kristine Yaffe, Departments of Psychiatry, Neurology and Epidemiology & Biostatistics, University of California, San Francisco and San Francisco Veterans Affairs Medical Center.
References
- 1.Byers AL, Yaffe K, Covinsky KE, et al. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67:489–496. doi: 10.1001/archgenpsychiatry.2010.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 3.Lapid MI, Rummans TA. Evaluation and management of geriatric depression in primary care. Mayo Clin Proc. 2003;78:1423–1429. doi: 10.4065/78.11.1423. [DOI] [PubMed] [Google Scholar]
- 4.Vahia IV, Meeks TW, Thompson WK, et al. Subthreshold depression and successful aging in older women. Am J Geriatr Psychiatry. 2010;18:212–220. doi: 10.1097/JGP.0b013e3181b7f10e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ownby RL, Crocco E, Acevedo A, et al. Depression and risk for Alzheimer Disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006;63:530–538. doi: 10.1001/archpsyc.63.5.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korczyn AD, Halperin I. Depression and dementia. J Neurol Sci. 2009;283:139–142. doi: 10.1016/j.jns.2009.02.346. [DOI] [PubMed] [Google Scholar]
- 7.Barnes DE, Alexopoulos GS, Lopez OL, et al. Depressive symptoms, vascular disease, and mild cognitive impairment. Arch Gen Psychiatry. 2006;63:273–280. doi: 10.1001/archpsyc.63.3.273. [DOI] [PubMed] [Google Scholar]
- 8.Wilson RS, Barnes LL, Mendes de Leon CF, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59:364–370. doi: 10.1212/wnl.59.3.364. [DOI] [PubMed] [Google Scholar]
- 9.Jorm AF. History of depression as a risk factor for dementia: an updated review. Aust N Z J Psychiatry. 2001;35:776–781. doi: 10.1046/j.1440-1614.2001.00967.x. [DOI] [PubMed] [Google Scholar]
- 10.Yaffe K, Blackwell T, Gore R, et al. Depressive symptoms and cognitive decline in nondemented elderly women: a prospective study. Arch Gen Psychiatry. 1999;56:425–430. doi: 10.1001/archpsyc.56.5.425. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg PB, Mielke MM, Xue QL, et al. Depressive symptoms predict incident cognitive impairment in cognitive healthy older women. Am J Geriatr Psychiatry. 2010;18:204–211. doi: 10.1097/JGP.0b013e3181c53487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becker JT, Chang YF, Lopez OL, et al. Depressed mood is not a risk factor for incident dementia in a community-based cohort. Am J Geriatr Psychiatry. 2009;17:653–663. doi: 10.1097/jgp.0b013e3181aad1fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panza F, Capurso C, D'Introno A, et al. Impact of depressive symptoms on the rate of progression to dementia in patients affected by mild cognitive impairment: the Italian Longitudinal Study on Aging. Int J Geriatr Psychiatry. 2008;23:726–734. doi: 10.1002/gps.1967. [DOI] [PubMed] [Google Scholar]
- 14.Ganguli M, Du Y, Dodge HH, et al. Depressive symptoms and cognitive decline in late life: a prospective epidemiological study. Arch Gen Psychiatry. 2006;63:153–160. doi: 10.1001/archpsyc.63.2.153. [DOI] [PubMed] [Google Scholar]
- 15.Lindsay J, Laurin D, Verreault R, et al. Risk factors for Alzheimer's Disease: a prospective analysis from the Canadian Study of Health and Aging. Am J Epidemiol. 2002;156:445–453. doi: 10.1093/aje/kwf074. [DOI] [PubMed] [Google Scholar]
- 16.Yaffe K, Edwards ER, Covinsky KE, et al. Depressive symptoms and risk of mortality in frail, community-living elderly persons. Am J Geriatr Psychiatry. 2003;11:561–567. [PubMed] [Google Scholar]
- 17.Mehta KM, Yaffe K, Langa KM, et al. Additive effects of cognitive function and depressive symptoms on mortality in elderly community-living adults. J Gerontol A Biol Sci Med Sci. 2003;58:M461–467. doi: 10.1093/gerona/58.5.m461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blazer DG, Hybels CF, Pieper CF. The association of depression and mortality in elderly persons: a case for multiple, independent pathways. J Gerontol A Biol Sci Med Sci. 2001;56:M505–509. doi: 10.1093/gerona/56.8.m505. [DOI] [PubMed] [Google Scholar]
- 19.Schulz R, Beach SR, Ives DG, et al. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 20.Whooley MA, Browner WS. Association between depressive symptoms and mortality in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1998;158:2129–2135. doi: 10.1001/archinte.158.19.2129. [DOI] [PubMed] [Google Scholar]
- 21.Covinsky KE, Kahana E, Chin MH, et al. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130:563–569. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 22.Callahan CM, Wolinsky FD, Stump TE, et al. Mortality, symptoms, and functional impairment in late-life depression. J Gen Intern Med. 1998;13:746–752. doi: 10.1046/j.1525-1497.1998.00226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fredman L, Schoenbach VJ, Kaplan BH, et al. The association between depressive symptoms and mortality among older participants in the Epidemiologic Catchment Area-Piedmont Health Survey. J Gerontol. 1989;44:S149–S156. doi: 10.1093/geronj/44.4.s149. [DOI] [PubMed] [Google Scholar]
- 24.Herrera-Guzman I, Gudayol-Ferre E, Herrera-Guzman D, et al. Effects of selective serotonin reuptake and dual serotonergic-noradrenergic reuptake treatments on memory and mental processing speed in patients with major depressive disorder. J Psychiatr Res. 2009;43:855–863. doi: 10.1016/j.jpsychires.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 25.Bragin V, Chemodanova M, Dzhafarova N, et al. Integrated treatment approach improves cognitive function in demented and clinically depressed patients. Am J Alzheimer's Dis Other Demen. 2005;20:21–26. doi: 10.1177/153331750502000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 27.Alexopoulos GS, Meyers BS, Young RC, et al. 'Vascular depression' hypothesis. Arch Gen Psychiatry. 1997;54:915–922. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- 28.Alexopoulos GS. Vascular disease, depression, and dementia. J Am Geriatr Soc. 2003;51:1178–1180. doi: 10.1046/j.1532-5415.2003.51373.x. [DOI] [PubMed] [Google Scholar]
- 29.Steffens DC, Krishnan KR, Crump C, et al. Cerebrovascular disease and evolution of depressive symptoms in the Cardiovascular Health Study. Stroke. 2002;33:1636–1644. doi: 10.1161/01.str.0000018405.59799.d5. [DOI] [PubMed] [Google Scholar]
- 30.Wolbers M, Koller MT, Witteman JCM, et al. Prognostic models with competing risks: methods and application to coronary risk prediction. Epidemiology. 2009;20:555–561. doi: 10.1097/EDE.0b013e3181a39056. [DOI] [PubMed] [Google Scholar]
- 31.May HT, Horne BD, Carlquist JF, et al. Depression after coronary artery disease is associated with heart failure. J Am Coll Cardiol. 2009;53:1440–1447. doi: 10.1016/j.jacc.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 32.VanCott AC, Cramer JA, Copeland LA, et al. Suicide-related behaviors in older patients with new anti-epileptic drug use: data from the VA hospital system. BMC Med. 2010;8:4. doi: 10.1186/1741-7015-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castilla-Puentes RC, Habeych ME. Subtypes of depression among patients with Alzheimer's disease and other dementias. Alzheimers Dement. 2010;6:63–69. doi: 10.1016/j.jalz.2009.04.1232. [DOI] [PubMed] [Google Scholar]
- 34.United States Department of Veterans Affairs. VA Vital Status Files [description online] [Accessed January 14, 2010]; Available at: http://www.virec.research.va.gov/DataSourcesName/VitalStatus/VitalStatus.htm.
- 35.Bauman KJ, Graf NL. Educational attainment: Census 2000 Brief (C2KBR-24) Washington, DC: U.S. Government Printing Office; 2003. [Google Scholar]
- 36.Zivin K, Kim HM, McCarthy JF, et al. Suicide mortality among individuals receiving treatment for depression in the Veterans Affairs Health System: associations with patient and treatment setting characteristics. Am J Public Health. 2007;97:2193–2198. doi: 10.2105/AJPH.2007.115477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bruce ML. Subsyndromal depression and services delivery: at a crossroad? Am J Geriatr Psychiatry. 2010;18:189–192. doi: 10.1097/JGP.0b013e3181cb87f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amore M, Tagariello P, Laterza C, et al. Subtypes of depression in dementia. Arch Gerontol Geriatr. 2007;44(1):23–33. doi: 10.1016/j.archger.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 40.Carney RM, Freedland KE, Miller GE, et al. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]