Abstract
Objective
To establish reference values for stair ascent and descent times in community dwelling ambulatory older adults, and to examine their predictive validity for functional decline.
Design
Longitudinal cohort study. Mean follow-up time was 1.8 year (maximum 3.2 y, total 857.9 person-years).
Setting
Community sample.
Participants
Older adults age 70 and older (N=513; mean age, 80.8±5.1y), without disability or dementia.
Interventions
Not applicable.
Main Outcome Measures
Time to ascend and descend 3 steps measured at baseline. 14 point Disability scale assessed functional status at baseline and at follow-up interviews every 2–3 months. Functional decline was defined as an increase in the disability score by 1-point during the follow-up period.
Results
The mean ± standard deviation (SD) stair ascent and descent time for three steps was 2.78 ±1.49 and 2.83 ±1.61 sec respectively. The proportion of self-reported and objective difficulty was higher with longer stair ascent and descent times (P<.001 for trend for both stair ascent and descent). Of the 472 participants with at least one follow-up interview, 315 developed functional decline with a 12-month cumulative incidence of 56.6% (95% confidence interval, CI, 52.1–61.3%). The stair negotiation time was a significant predictor of functional decline after adjusting for covariates including gait velocity (adjusted hazard ratio per one-second increase, aHR 1.12, 95% CI 1.04–1.21 for stair ascent time, aHR 1.15, 95% CI 1.07–1.24 for stair descent time). Stair descent time was a significant predictor of functional decline among relatively high-functioning older adults reporting no difficulty in stair negotiation (P=.001).
Conclusions
The stair ascent and descent times are simple, quick, and valid clinical measures for assessing the risk of functional decline in community dwelling older adults including high-functioning individuals.
Keywords: Rehabilitation, Activities of daily living, Aged
Stair negotiation is one of the most demanding and hazardous activities with more than 10% of fatal falls in older adults occurring while going down stairs.1 Self-reported ability to climb stairs is considered as a key marker of functional independence in older adults.1–3 Difficulty in climbing stairs in older adults predicted readmission to hospital within a month after being discharged from the emergency department.4 In hospital settings, stair-climbing ability is often used to decide whether a patient may be sent home or to a nursing facility.5,6
Stair negotiation is often assessed as one of the components of functional assessment scales.3,7–9 Stair climbing is assessed by self-report in the majority of these scales. The questionnaires for stair negotiation, however, are limited by unclear definitions (i.e. number of steps), lack of validation, or only assessing stair ascent and not descent.3 Moreover, while self-reported difficulty in stair negotiation may be a reliable and valid indicator,10 it is not a direct measure of this motoric activity and does not adequately capture the variability in performance seen on this task in older adults. Currently there exists no standard performance test of stair negotiation ability with age and gender norms and the potential importance of difficulty with stair descent1,10,11 as an indicator of functional status has been largely overlooked.
Several quantitative measures have been reported assessing stair negotiation.12–16 These measures have, however, limited use as reference measures due to inconsistency in the unit (i.e. stair negotiation speed, cm/sec or steps/sec),14–16 lack of validated norms,17,18 not distinguishing stair ascent and descent phases,13,17 or limited feasibility for low functioning individuals (involving a full flight of stairs at the fastest speed).12,13,17
Developing reliable and valid quantitative measures that are complementary to self-report is needed for better assessment of stair negotiation ability among older adults. The objective of this study was threefold; to establish reference values for stair ascent and descent in nondemented and nondisabled older adults living in the community, to assess the face validity of stair negotiation times with subjective and objective stair negotiation ability measures, and to examine the predictive validity of stair negotiation times for functional decline in older adults including high functioning individuals.
METHODS
Study Population
We conducted a prospective cohort study nested within the Einstein Aging Study. The primary aim of the Einstein Aging Study was to identify risk factors for dementia. Study design has been previously reported.19 Potential participants (aged 70 and older) identified from Bronx County population lists were invited for the study. Exclusion criteria included severe auditory or visual loss, being bed-bound, and institutionalization. Of the 577 participants enrolled between March 2006 and January 2009, 41 were not tested on the stairs protocol for the following reasons; joint pain (n=8), unsteadiness (n=17), tiredness (n=7), and refusal without providing reasons (n=9). We excluded 4 participants with disability (see definition below) and 19 with dementia20 leaving 513 participants eligible for this study. Follow-up for this study was through December 2010. All clinical and stair assessments were done in our research center using study protocols approved by the local institutional review board.
Clinical Evaluation
Research assistants elicited history of medical illness at study visits using structured questionnaires. Dichotomous rating (present or absent) of hypertension, diabetes, heart failure, angina, myocardial infarction, strokes, Parkinson’s disease, chronic obstructive lung disease, depression, and arthritis was used to calculate a summary illness index score (range 0–10) as previously described.21,22 Previous falls and status of fear of falling (yes or no) were recorded. Depressive symptoms were measured by the 15-item Geriatric Depression Scale,23 and cognitive status by the Blessed Information-Memory-Concentration Test.24 Gait velocity was measured using an instrumented walkway (457 × 90.2 × 0.64cm, GAITRitea).
Stair Negotiation
Prior to the stair test, all participants were asked whether they were willing to climb up and down three steps. If participants were not comfortable or not willing with the procedure, the test was not administered. To assess the stair negotiation times, participant stood with the research assistant at the base of a well-lighted, uncarpeted flight of stairs with handrails. Each step measured 18 cm in height, 26 cm in depth, and 110 cm in width. These dimensions are among the most frequently encountered in semi-public places and are within the stair dimensions recommended by the Occupational Safety and Health Standards,25 lending ecological validity to this test. Participants were instructed to climb the steps at their preferred speed using handrails if necessary. We used three steps, which was more preferable to our participants than a full flight of stairs (10 steps) as reported in our previous study.10 Participants were asked about difficulty in stair negotiation before performing stair negotiation using our previously validated questionnaire (Do you have difficulty climbing stairs? Do you have difficulty coming down stairs?).10 Stair ascent timing was started using a stopwatch once the participant began lifting their leading foot from the floor after the tester said “go”. When the participant placed both feet flat on the third step, the timing was stopped. After a brief rest, participants were requested to walk down. The stair descent timing started from the time when the leading foot began lifting from the third step and stopped when both feet were placed flat on the base of the stairs. Stair negotiation time was measured to the hundredth of a second with one trial for stair ascent and descent. The test-retest reliability for this measure was good (Pearson’s r=.94 for ascent time, r=.93 for descent time) in a subsample of 20 participants. The use of handrails and objective difficulty were noted by the tester. Testers intervened to assist the participants in case of safety concerns.
Assessment of Activities of Daily Living and Definition of Functional Decline
Participants were assessed for ADL at the baseline study visit, every 2 to 3 months via telephone interviews, and annual interviews at the research center using a validated disability scale.26 The following 7 ADLs were assessed: bathing, dressing, grooming, feeding, toileting, walking around home, and getting up from a chair. For each task, participants were asked: “At the present time, are you unable or do you need help from another person to complete the task?” If the response was “yes”, the task was scored 2. If the response was “no”, participants were asked a follow-up question, “Do you have difficulty in completing the task? The task was scored 1 for the response of “yes”, and 0 for the response of “no”. The disability score was calculated as a sum of the scores from 7 ADLs with maximum disability score of 14 (requiring help for all 7 ADLs) and minimum of 0. Disability was defined as inability or requiring personal assistance in any of the 7 ADLs. Functional decline was operationally defined as an increment of 1-point or more on the disability score during follow-up period. The 1-point increment could represent a participant who had no difficulty in all 7 ADLs at baseline reporting a new difficulty to perform any of the 7 ADLs or a participant who reported difficulty in ADLs at baseline transitioning to disability during follow-up.27,28 We also explored a more stringent alternate definition of functional decline defining it as an increment in disability score by 2-points or more over follow-up. The 2-point increment would correspond to developing a new disability or new difficulty in doing two or more ADLs over the follow-up.
Statistical Analysis
The mean and SD of the stair negotiation times were tabulated per 5-year age stratum for each sex. The association between the stair negotiation times and clinical characteristics were reported in univariate linear regression analysis. Data from the 472 participants with at least one follow-up interview were analyzed by the Kaplan-Meier method to estimate the cumulative probability of functional decline among tertiles of stair negotiation time. The timing of event was estimated as the follow-up interview date at which functional decline was reported for the first time. If participants had more than 6 months interval between interviews, their follow-up was censored at the interview prior to this interval. Out of a total of 3812 interviews, only 28 interviews (0.7%) from 28 participants had intervals of longer than 6 months. Sensitivity analysis including interviews of intervals longer than 6 months showed similar results as our main analysis, and are not reported.
Cox proportional-hazards regression analysis was performed to investigate whether stair negotiation time was an independent predictor of functional decline. Ascent and descent times were examined in separate models due to issues of collinearity. The covariates of clinical importance or with p values of <0.1 in the univariate analysis were included in the models. The final analysis included age, gender, ethnicity, illness index score, Blessed test score, depression score, fear of falling status, disability score, and gait velocity at baseline. Predictive validity of stair negotiation was also evaluated among subgroup of relatively high functioning individuals. High functioning status was defined using a recommended cutscore on gait velocity of 100 cm/sec or higher,29 and alternatively as no self-reported difficulty in stair negotiation. Proportionality assumption was checked for each variable using the Goodness-of-fit test based on the scaled Schoenfeld residual.30 All data analysis was performed using STATAb version 10.1.
RESULTS
Study Population and Clinical Covariates
The baseline characteristics of 513 participants are summarized in table 1. None of the participants had loss of balance, fell, or sustained injuries during the stair negotiation test. The mean (SD) age was 80.8 (5.1) years and 60.2% were women. Of the 513 participants, 48% reported a previous fall and 34% fear of falling at baseline. In the univariate analysis, stair ascent time was significantly longer with higher number of medical illnesses, depressive symptoms, and disability scores, lower gait velocity, and in women and those with fear of falling. Stair descent time showed a similar pattern of associations to stair ascent time, and additional associations with older age and non-white ethnicity. To account for the skewed distribution of stair negotiation time (skewed to the right, higher values), we also performed the univariate analysis with inverse transformation of stair negotiation times. In this analysis, older age became significantly associated with both stair ascent and descent time. The remaining results from this analysis were not materially different from the analysis without transformation. Hence, for ease of interpretation the remaining analyses reported below are based on untransformed values.
Table 1.
Demographic and medical characteristics of study population and regression coefficients in univariate analysis with stair ascent and descent time.
| Stair Ascent Time | Stair Descent Time | ||||
|---|---|---|---|---|---|
| Total (n=513) |
Regression coefficient (95% CI) |
P | Regression coefficient (95% CI) |
P | |
| Age | 80.8±5.1 | 0.021 (−0.004, 0.046) | .101 | 0.042 (0.015, 0.069) | .002 |
| Men (%) | 204 (39.8) | −0.363 (−0.625, –0.101) | .007 | −0.607 (−0.889, –0.326) | <.001 |
| Ethnicity (Non-White) (%) | 158 (30.8) | 0.179 (−0.101, 0.458) | .210 | 0.309 (0.006, 0.612) | .046 |
| Illness index summary score | 1.4±1.1 | 0.169 (0.047, 0.291) | .007 | 0.139 (0.006, 0.273) | .040 |
| Geriatric depression scale | 2.0±2.0 | 0.100 (0.036, 0.164) | .036 | 0.085 (0.015, 0.155) | .017 |
| Blessed test score | 1.8±2.0 | 0.042 (−0.022, 0.106) | .200 | 0.035 (−0.034, 0.105) | .318 |
| Disability score | 1.3±1.5 | 0.393 (0.312, 0.474) | <.001 | 0.456 (0.368, 0.543) | <.001 |
| Past fall (%) | 245 (47.7) | 0.159 (−0.099, 0.417) | .306 | 0.081 (−0.200, 0.362) | .572 |
| Fear of falling (%) | 174 (33.9) | 0.510 (0.241, 0.779) | <.001 | 0.608 (0.317, 0.900) | <.001 |
| Gait velocity (cm/sec) | 95.6±20.3 | −0.031 (−0.037, –0.025) | <.001 | −0.036 (−0.042, –0.029) | <.001 |
Values for continuous variables expressed as mean±standard deviation (SD).
Stair Ascent and Descent Time
Table 2 shows the mean values for stair negotiation times by gender and age groups. Overall correlation between stair ascent and descent time was high (Pearson’s r=.77). The stair ascent and descent times were greater with older age in men (P for trend=.040 for ascent and P for trend=.012 for descent). Among women, this pattern was shown for stair descent (P for trend=.024) but not for stair ascent.
Table 2.
Mean value for stair ascent and descent time by age groups.
| Stair Negotiation Time (sec) |
Men | Women | Overall (n=513) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 70–74 (n=26) |
75–79 (n=59) |
80–84 (n=68) |
≥85 (n=51) |
Total (n=204) |
70–74 (n=53) |
75–79 (n=101) |
80–84 (n=91) |
≥85 (n=64) |
Total (n=309) |
||
| Ascent | 2.09±0.66 | 2.48±1.11 | 2.60±1.19 | 2.83±1.80 | 2.56±1.31 | 2.91±1.64 | 2.83±1.63 | 2.83±1.57 | 3.22±1.45 | 2.92±1.58 | 2.78±1.49 |
| Descent | 1.98±0.81 | 2.29±0.90 | 2.60±1.25 | 2.74±1.64 | 2.47±1.25 | 2.75±1.61 | 3.0±1.86 | 2.93±1.68 | 3.69±1.81 | 3.08±1.78 | 2.83±1.61 |
Values expressed as mean±SD.
Association with Self Reported Difficulty and Use of Handrails
The proportion of self-reported stair negotiation difficulty was compared by tertiles of stair negotiation time (table 3). Similar pattern was shown in stair ascent and descent. The mean values ± SD of stair ascent and descent time were 3.16±1.64 and 3.60±2.01 sec for those reporting difficulty in stair negotiation compared to 2.41±1.16 and 2.43±1.15 sec for those without difficulty. The proportion of participants with self reported difficulty was 34.1% in the lowest tertile compared to 70.2% in the highest tertile of stair ascent time (P for trend<.001). Gender-specific tertiles showed similar pattern (34.1, 45.2, and 70.6% among the lowest, middle, and highest tertiles respectively for women, 32.9, 37.8, and 68.1% respectively for men, P for trend<.001 for both genders). Similar trend was shown for difficulty observed by the tester and use of handrails during the test.
Table 3.
Difficulty and Use of Handrails during Stair Negotiation among the Participants by Tertiles of Stair Ascent and Descent Time.
| Tertiles of Stair Ascent Time | Tertiles of Stair Descent Time | |||||||
|---|---|---|---|---|---|---|---|---|
| Lowest (n=173) |
Middle (n=169) |
Highest (n=171) |
P for trend | Lowest (n=173) |
Middle (n=169) |
Highest (n=171) |
P for trend | |
| Stair negotiation time (sec) | 1.73±0.25 | 2.36±0.20 | 4.25±1.75 | <.001 | 1.65±0.24 | 2.31±0.23 | 4.55±1.76 | <.001 |
| Difficulty reported by participants (%) | 59 (34.1) | 72 (42.6) | 120 (70.2) | <.001 | 34 (19.7) | 49 (30.0) | 97 (56.7) | <.001 |
| Difficulty observed by tester (%) | 4 (2.3) | 16 (9.5) | 105 (61.4) | <.001 | 4 (2.3) | 20 (11.8) | 105 (61.4) | <.001 |
| Use of handrails (%) | 75 (43.4) | 106 (62.7) | 149 (87.1) | <.001 | 67 (39.0) | 110 (65.1) | 151 (88.3) | <.001 |
Values for continuous variables expressed as mean± SD.
Stair Negotiation Time and Functional Decline
Four hundred and seventy-two participants with minimum one follow-up had a total of 3812 interviews (median, 8 interviews per participant). Mean overall follow-up time for the study cohort was 1.8 years (not censoring at functional decline) with maximum of 3.2 years and total 857.9 person-years follow-up time. Participants with no follow-up (n=41) did not differ from participants with follow-up in terms of age, gender, ethnicity, mean stair ascent (2.7±1.5 versus 2.8±1.4 sec), and stair descent times (2.7±1.5 versus 2.8±1.6 sec), however, showed higher depression scores (2.6 versus 1.9, P=.040), illness index (1.8 versus 1.4, P=.044) and higher prevalence of past falls (72.5 versus 45.3%) and fear of falling (50.0 versus 32.4%).
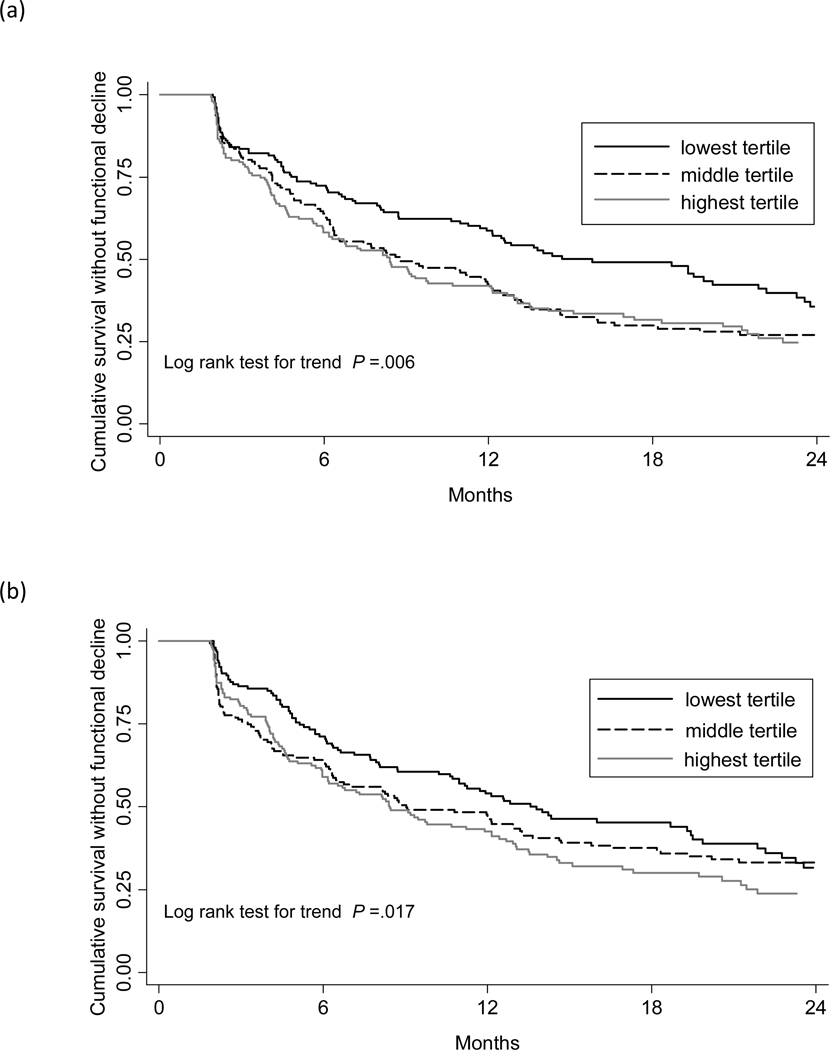
Of the 472 participants, 315 developed functional decline with a 12-month cumulative incidence of 56.6% [95% CI, 52.1–61.3%]. Mean follow-up time to incident functional decline was 11.4 months. Functional-decline-free-survival by the tertiles of stair ascent and descent times is presented in figure 1. There was an increasing trend noted in developing functional decline over 12-months from 45.7% (95% CI, 38.1–54.0%) in the lowest to 61.8% (95% CI, 53.9–69.7%) in the highest tertiles of the stair ascent time (log rank test for trend, P=.006). Similar pattern was shown for stair descent; 50.4% (95% CI, 42.5–58.8%) in the lowest and 62.5% (95% CI, 54.8–70.3%) in the highest tertiles (log rank test for trend, P=.017).
Figure 1.
Functional-decline-free survival among the participants in each tertile of stair ascent time (a) and stair descent time (b).
Cox proportional-hazards analysis showed that both stair ascent and descent times predicted functional decline after adjusting for covariates including gait velocity which was also a significant predictor (aHR of 1.12 per one-second increase in stair ascent time, 95% CI 1.04–1.21, aHR of 1.15 per one-second increase in stair descent time, 95% CI 1.07–1.24) (table 4).
Table 4.
Adjusted Hazard Ratio for Decline in ADL performance in Cox Proportional Hazards Regression Analysis
| Analysis with Stair Ascent Time | Analysis with Stair Descent Time | |||
|---|---|---|---|---|
| aHR (95% CI) | P | aHR (95% CI) | P | |
| Stair Ascent Time | 1.12 (1.04, 1.21) | .004 | N/A | |
| Stair Descent Time | N/A | 1.15 (1.07, 1.24) | <.001 | |
| Age | 1.01 (0.99, 1.03) | .487 | 1.01 (0.98, 1.02) | .628 |
| Men (reference-women) | 1.14 (0.89, 1.44) | .305 | 1.18 (0.93, 1.52) | .164 |
| Non-white (reference-white) | 0.91 (0.69, 1.18) | .463 | 0.89 (0.68, 1.16) | .391 |
| Illness index | 1.02 (0.91, 1.12) | .830 | 1.01 (0.91, 1.13) | .799 |
| Depression score | 1.07 (1.01, 1.15) | .023 | 1.09 (1.07, 1.16) | .016 |
| Blessed test score | 0.97 (0.91, 1.03) | 0.260 | 0.97 (0.92, 1.03) | .355 |
| Fear of falling | 1.24 (0.95, 1.61) | 0.108 | 1.23 (0.95, 1.60) | .117 |
| Disability score at baseline | 0.71 (0.64, 0.79) | <.001 | 0.70 (0.63, 0.78) | <.001 |
| Gait velocity at baseline | 0.99 (0.98, 1.00) | .004 | 0.99 (0.98, 1.00) | .012 |
Abbreviation: aHR, adjusted hazard ratio; CI, confidence interval.
Of the 472 participants, 156 showed functional decline using our alternate definition (increment of 2-points or more on the disability score) over the follow-up period. Only the stair descent time was a significant predictor for functional decline by this definition (aHR;1.15, 95% CI;1.06–1.27, P=.002) but not the stair ascent time (aHR;1.05, 95% CI;0.95–1.17).
Stair Negotiation Time and Functional Decline among High Functioning Older Adults
Among the 204 participants with gait velocity of 100 cm/sec or higher, stair descent time predicted functional decline (aHR of 1.24 per one-second increase, 95% CI 1.05–1.47, P=.011) and stair ascent time was of borderline significance (aHR of 1.15, 95% CI 1.00–1.32, P=.057). Among the 220 participants reporting no difficulty in stair ascent or descent, stair descent time was predicted functional decline after adjusting for covariates including gait velocity (aHR 1.17, 95% CI 1.01–1.37). Stair ascent time was not significant in this analysis (aHR 1.06, 95% CI 0.93–1.21). Stair descent time also predicted new difficulty in stair negotiation (ascent or descent) among 220 participants with no difficulty at baseline (aHR; 1.20, 95% CI; 1.02–1.42). Stair ascent time was not a significant predictor of subjective difficulty in stair negotiation.
DISCUSSION
We report reference values for stair negotiation times for three steps in community residing nondisabled and nondemented older adults. To our knowledge, this is the first report to provide reference values for quantitative stair negotiation in community dwelling old adults as well as by age and gender categories. The proportion of participants with subjective or objective difficulty and the proportion of those using rails during stair negotiation were higher among individuals with longer stair negotiation times supporting the face validity of this measure. Our subgroup analysis also shows high test-retest reliability for this simple clinical measure. Our findings show that the objective stair negotiation test is a simple, quick (takes less than 30 seconds), valid and reliable assessment of function in older adults that does not require specialized equipment or training.
Stair descent time was greater with older age in both genders and stair ascent time was greater with older age in men. Stair negotiation demands relatively higher effort of the knee extensors in the healthy old compared to young adults due to reduced maximum leg strength (percentage of maximum knee extensor momentum; 78% versus 54% for stair ascent, 88% versus 42% for stair descent).31 This in part may explain the association between the stair negotiation times and age. Impairments in vision, proprioception, balance, and cardiovascular health may also contribute to this association.1 In concordance with our previous study of self-reported difficulty in stair negotiation,10 fear of falling was associated with longer stair negotiation times. Lower self efficacy score in stair negotiation has been shown to be associated with slower stair climbing speed and cautious stair climbing behaviors.32
Both stair ascent and descent times were strong predictors of functional decline even after adjusting for multiple covariates including gait velocity supporting its incremental value in studying functional decline. The increasing cumulative incidence in functional decline from the lowest to the highest tertiles of stair negotiation indicates a dose-response effect of this measure.
Since stair negotiation is more challenging compared to walking on level surface, we hypothesized that stair negotiation may predict incident functional decline among high functioning individuals. Our results showed that stair descent time was a strong predictor and stair ascent time was of borderline significance for functional decline in this subgroup. Stair descent, but not ascent time also predicted new onset of subjective difficulty in stair negotiation. Stair descent time remained a predictor even when a more conservative definition for functional decline was used. These findings are in accord with our previous study10 reporting that self-reported difficulty in stair descent was associated with difficulty in a wider spectrum of ADLs than stair ascent.
Kinetic and behavioral differences between stair ascent and descent in part might explain the discrepant findings with regards to predicting functional decline.31,33 Older adults utilize nearly 90% of maximum capacity of knee extensor momentum for stair descent compared to 78% for stair ascent.31 Also, increased coactivation of knee extensors (agonist) and flexors (antagonist) during stair descent indicate that it is more challenging than stair ascent, therefore neuromotor impairment among older adults may be unmasked more during stair descent than ascent.31 During stair descent a larger separation between center of mass and center of pressure occurs34 compared to stair ascent reflecting higher demands on balance control mechanisms. Lower self efficacy scale scores were associated with stair descent compared to stair ascent indicating a greater contribution of psychological factors to stair descent.32 Our previous study10 showed that difficulty in stair descent but not in ascent was associated with previous falls suggesting that stair descent may be more robust in capturing negative outcomes compared to stair ascent.
Study Limitations
The sample is a community based sample but was not recruited as a representative population sample. To improve the reliability of our measures and safety of participants, we did not include individuals with disability or dementia. Therefore, our sample is likely healthier than general population, which might reduce generalizability. It might be expected that stair negotiation times might be longer in individuals with disability or that they might not be able to do these tasks.
CONCLUSIONS
The stair ascent and descent times are reliable and valid measures of assessing difficulty in negotiating stairs, a common activity at home and community settings. Stair descent time is a strong predictor of functional decline in community dwelling older adults including individuals with relatively high functional status. The stair negotiation time can be used as a quick and simple measure in clinical settings that does not require specialized equipment or training to assess functional status and predict functional decline in older adults.
Acknowledgments
Funding: Mooyeon Oh-Park is an Einstein Men’s Division Scholar partially supported through a National Institutes of Health ‘Clinical and Translational Science Award ‘(CTSA) grant UL1 RR025750 and KL2RR025749 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. The Einstein Aging Study (PI: R.B. Lipton) is funded by the National Institute on Aging (AG03949). Dr. Verghese is funded by the National Institute on Aging (RO1 AG025119).
Financial Disclosure: We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
SUPPLIERS
GAITRite system; CIR systems Inc, 60 Garlor Drive, Havertown, PA, USA
STATA Corp, 4505 Lakeway Drive, College Station, TX 77845.
REFERENCES
- 1.Startzell JK, Owens DA, Mulfinger LM, Cavanagh PR. Stair negotiation in older people: a review. J Am Geriatr Soc. 2000;48:567–580. doi: 10.1111/j.1532-5415.2000.tb05006.x. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 3.van Iersel MB, Olde Rikkert MG, Mulley GP. Is stair negotiation measured appropriately in functional assessment scales? Clin Rehabil. 2003;17:325–333. doi: 10.1191/0269215502cr628oa. [DOI] [PubMed] [Google Scholar]
- 4.Caplan GA, Brown A, Croker WD, Doolan J. Risk of admission within 4 weeks of discharge of elderly patients from the emergency department--the DEED study. Discharge of elderly from emergency department. Age Ageing. 1998;27:697–702. doi: 10.1093/ageing/27.6.697. [DOI] [PubMed] [Google Scholar]
- 5.Lin PC, Hung SH, Liao MH, Sheen SY, Jong SY. Care needs and level of care difficulty related to hip fractures in geriatric populations during the post-discharge transition period. J Nurs Res. 2006;14:251–260. doi: 10.1097/01.jnr.0000387584.89468.30. [DOI] [PubMed] [Google Scholar]
- 6.Stineman MG, Fiedler RC, Granger CV, Maislin G. Functional task benchmarks for stroke rehabilitation. Arch Phys Med Rehabil. 1998;79:497–504. doi: 10.1016/s0003-9993(98)90062-4. [DOI] [PubMed] [Google Scholar]
- 7.Mahoney FI, Barthel DW. Functional Evaluation: The Barthel Index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 8.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 9.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Verghese J, Wang C, Xue X, Holtzer R. Self-reported difficulty in climbing up or down stairs in nondisabled elderly. Arch Phys Med Rehabil. 2008;89:100–104. doi: 10.1016/j.apmr.2007.08.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bassett DR, Vachon JA, Kirkland AO, Howley ET, Duncan GE, Johnson KR. Energy cost of stair climbing and descending on the college alumnus questionnaire. Med Sci Sports Exerc. 1997;29:1250–1254. doi: 10.1097/00005768-199709000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Bean JF, Kiely DK, LaRose S, Alian J, Frontera WR. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88:604–609. doi: 10.1016/j.apmr.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Perron M, Malouin F, Moffet H. Assessing advanced locomotor recovery after total hip arthroplasty with the timed stair test. Clin Rehabil. 2003;17:780–786. doi: 10.1191/0269215503cr696oa. [DOI] [PubMed] [Google Scholar]
- 14.Bassey EJ, Fiatarone MA, O'Neill EF, Kelly M, Evans WJ, Lipsitz LA. Leg extensor power and functional performance in very old men and women. Clin Sci (Lond) 1992;82:321–327. doi: 10.1042/cs0820321. [DOI] [PubMed] [Google Scholar]
- 15.Masuda K, Kim J, Kinugasa R, Tanabe K, Kuno SY. Determinants for stair climbing by elderly from muscle morphology. Percept Mot Skills. 2002;94:814–816. doi: 10.2466/pms.2002.94.3.814. [DOI] [PubMed] [Google Scholar]
- 16.Tiedemann AC, Sherrington C, Lord SR. Physical and psychological factors associated with stair negotiation performance in older people. J Gerontol A Biol Sci Med Sci. 2007;62:1259–1265. doi: 10.1093/gerona/62.11.1259. [DOI] [PubMed] [Google Scholar]
- 17.Almeida GJ, Schroeder CA, Gil AB, Fitzgerald GK, Piva SR. Interrater reliability and validity of the stair ascend/descend test in subjects with total knee arthroplasty. Arch Phys Med Rehabil. 2010;91:932–938. doi: 10.1016/j.apmr.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verghese J, LeValley A, Hall CB, Katz MJ, Ambrose AF, Lipton RB. Epidemiology of gait disorders in community-residing older adults. J Am Geriatr Soc. 2006;54:255–261. doi: 10.1111/j.1532-5415.2005.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington (DC): APA; 1994. [Google Scholar]
- 21.Holtzer R, Verghese J, Wang C, Hall CB, Lipton RB. Within-person across-neuropsychological test variability and incident dementia. JAMA. 2008;300:823–830. doi: 10.1001/jama.300.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holtzer R, Verghese J, Xue X, Lipton RB. Cognitive processes related to gait velocity: results from the Einstein Aging Study. Neuropsychology. 2006;20:215–223. doi: 10.1037/0894-4105.20.2.215. [DOI] [PubMed] [Google Scholar]
- 23.de Craen AJ, Heeren TJ, Gussekloo J. Accuracy of the 15-item geriatric depression scale (GDS-15) in a community sample of the oldest old. Int J Geriatr Psychiatry. 2003;18:63–66. doi: 10.1002/gps.773. [DOI] [PubMed] [Google Scholar]
- 24.Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br J Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- 25. [accessed on 04/22/2011]; http://www.osha.gov/pls/oshaweb/owadispshow_document?p_table=STANDARDS&p_id=9716.
- 26.Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community-living older persons. J Gerontol A Biol Sci Med Sci. 2003;58:70–75. doi: 10.1093/gerona/58.1.m70. [DOI] [PubMed] [Google Scholar]
- 27.Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Fox M, Guralnik JM. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314–322. doi: 10.1046/j.1532-5415.2003.51104.x. [DOI] [PubMed] [Google Scholar]
- 28.Gill TM. Assessment of function and disability in longitudinal studies. J Am Geriatr Soc. 2010;58 Suppl 2:S308–S312. doi: 10.1111/j.1532-5415.2010.02914.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, Tylavsky FA, Brach JS, Satterfield S, Bauer DC, Visser M, Rubin SM, Harris TB, Pahor M. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 30.Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 31.Hortobagyi T, Mizelle C, Beam S, DeVita P. Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci. 2003;58:M453–M460. doi: 10.1093/gerona/58.5.m453. [DOI] [PubMed] [Google Scholar]
- 32.Hamel KA, Cavanagh PR. Stair performance in people aged 75 and older. J Am Geriatr Soc. 2004;52:563–567. doi: 10.1111/j.1532-5415.2004.52162.x. [DOI] [PubMed] [Google Scholar]
- 33.Reeves ND, Spanjaard M, Mohagheghi AA, Baltzopoulos V, Maganaris CN. The demands of stair descent relative to maximum capacities in elderly and young adults. J Electromyogr Kinesiol. 2008;18:218–227. doi: 10.1016/j.jelekin.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 34.Reeves ND, Spanjaard M, Mohagheghi AA, Baltzopoulos V, Maganaris CN. Influence of light handrail use on the biomechanics of stair negotiation in old age. Gait Posture. 2008;28:327–336. doi: 10.1016/j.gaitpost.2008.01.014. [DOI] [PubMed] [Google Scholar]