Abstract
Introduction
The principles of correction of thoraco-lumbar kyphotic deformity (TKLD) in ankylosing spondylitis (AS) are essentially centred on lordosing osteotomies such as pedicle subtraction closing wedge osteotomy (CWO), polysegmental posterior lumbar wedge osteotomies (PWO) and Smith Peterson’s open wedge osteotomy (OWO) of the lumbar spine. There have been no studies that compared the results of the three osteotomies performed by a single surgeon with a long-term follow-up.
Materials and Methods
A retrospective review of 31 patients with AS was performed: 12 patients underwent CWO, 10 had OWO, and 9 had PWO. Radiographic assessment was performed at 6, 12, 24, and 52 weeks and annually thereafter. Clinical assessment included blood loss, intensive care unit (ICU) stay, and surgical time recordings. All patients were assessed clinically at regular intervals and outcome measures recorded included Oswestry Disability Index (ODI), Visual Analogue Score (VAS) for pain, and SRS-22 (recorded in 23 patients).
Results
The mean age at surgery was 54.7 years (40–74 years) and mean duration of symptoms was 3 years (range, 5–8 years). Mean follow-up was 5 years (range, 2–10 years). There was no statistically significant difference between the three techniques with regard to mean duration of surgery and ICU stay. The mean duration of surgery was 7 h (range, 4–9 h) (OWO cases had shorter period than CWO and PWO cases, and the longest period was for CWO cases). The mean ICU stay was 3 days (range, 2–20 days) (the period of stay was shorter in general for OWO and slightly longer for CWO and PWO). Blood loss was expressed as percentage of estimated blood volume (EBV). The mean blood loss in PWO was 23 ± 15.4% (range, 9–36%), CWO was 28 ± 4.5% (range, 12–40%) and in OWO was 15 ± 11% (range, 13–99%). Mean correction of kyphosis was 38° (range, 25°–49°) with CWO, 28° with OWO (range, 24°–38°) and 30° with PWO (range, 28°–40°). In comparison to preoperative scores, statistically significant improvement was noted in all three groups in the postoperative period with regard to ODI, VAS and SRS-22 (p = 0.001, Wilcoxon signed-rank test).
Conclusion
Better radiographic correction was noted in the CWO and PWO groups, although this was associated with increased blood loss, multiple levels of instrumentation, and increased surgical time compared to OWO. A new safe technique of instrumentation using temporary malleable rods to prevent sagittal translation during the reduction manoeuvre is also described.
Keywords: Ankylosing spondylitis, Thoraco-lumbar kyphotic deformity, Instrumented lumbar osteotomy
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory seronegative arthropathy which primarily affects the axial skeleton [1]. The aetiology of this condition remains unknown, but it is known that the disease is an inflammatory condition affecting the ligamentous insertion into bone [2, 3]. Sacroiliac joint is one of the first joints to be involved and other joints of the axial skeleton get affected progressively [4]. The inflammatory process culminates in calcification of the involved ligaments leading to disabling ankylosis of the involved joints.
The incidence of AS is between 0.5 and 14 per 100,000 people per year, whereas the prevalence is between 0.1 and 1.4%. There is a male preponderance (male:female ratio being 2:1) and patients show characteristic symptoms and signs around the age of 30 years [5]. There appears to be a genetic relation to HLA-B27; AS is seen in 90–95% of HLA-B27 patients, whereas only 1–5% of individuals who are HLA-B27 positive develop the disease. The influence of other environmental factors in this condition has been hypothesized [6, 7].
Thoracolumbar kyphotic deformity (TKLD) in AS is a disabling condition affecting more than 30% of the patients with this condition [8]. Patients find it difficult to sit, stand and/or lie down comfortably. Their horizontal visual field is compromised and due to an overall loss of sagittal balance their efficiency in gait is severely compromised. Compression of the abdominal viscera by the inferior margins of the ribs and reduced diaphragmatic excursion further contributes to the morbidity experienced by these patients. The principles of correction of TLKD are essentially centred on lordosing osteotomies of the lumbar spine as thoracic deformity correction is limited by the ankylosed costovertebral joints [9–14]. The thoracic cord is less mobile and tolerant to handle in a relatively tight canal, thereby increasing the risk of neurological injury compared to the cauda equine in the capacious lumbar canal. Also, the degree of correction achieved would be greatest if a sagittal plane deformity is corrected at the base of the deformity. The more inferior the lordotic angular correction in the lumbar spine, greater would be the arc subtended at the superior end of the deformity thereby magnifying the correction achieved [12, 15, 16]. Also, if the correction is lower, the lever arm for correction of the axis for frontal view is larger and hence the force for correction is also significantly greater [14].
Three osteotomies have been advocated and extensively used by several authors—pedicle subtraction closing wedge osteotomy (CWO), polysegmental posterior lumbar wedge osteotomies (PWO) and Smith Peterson’s open wedge osteotomy (OWO). Currently, these three techniques have been used separately by different authors. The technique used for a particular case appears to be determined by the surgeons’ individual experience and familiarity with each of these techniques. A recent study indicated that the quality of bone in the middle column is important in determining the type of osteotomy [17]. As has been advocated in this study, the senior author (SMH) also recommends assessment of hardness of bone intra-operatively. If the bone is hard and could act as a hinge in corrective osteotomy then OWO could be performed with a low risk of neurological complications due to a fractured middle column. For these reasons, OWO can be performed with a relative degree of safety in younger patients with a good bone stock. OWO is also best avoided if the aorta is calcified, to minimize risk of catastrophic bleeding, especially if the osteotomy is planned at L2 or higher. In the setting of osteoporotic bone at the level of osteotomy CWO is the procedure of choice since the posterior wedge can be resected with relative ease. However, the degree of correction achievable here without disrupting the ALL thereby causing anterior hinge failure is usually between 30° and 35° for a single segment. Larger corrections require multiple level osteotomies. In our series, PWO were generally reserved for mild disease, when the discs are not completely calcified and the aorta is not atheromatous or calcified. These have generally been the criteria for choosing the type of osteotomy in the senior author’s series. There are no studies comparing the results of the three aforementioned osteotomies performed by a single surgeon.
Methods
A retrospective review of patients, with AS who underwent corrective lumbar osteotomy from 1985 to 2007, was performed. There were 31 patients (26 males, 5 females) with mean age of 54 years (range 40–74 years). Indications for surgery included loss of sagittal balance, loss of horizontal gaze and back pain (noted in 80% of patients). Loss of sagittal balance was defined as >8 cm horizontal distance between C7 plumb line and the postero-superior corner of S1 endplate as determined on long cassette lateral radiographs. All operations were performed by the senior author (SHM). 12 patients underwent CWO, 10 had OWO, and 9 had PWO. One patient had undergone conservative treatment for a previous spinal fracture.
Careful positioning and fibre-optic intubation was used in all patients before positioning prone on a spinal frame or on a combination of bolsters and pillows ensuring that the abdomen was hanging free. Spinal cord monitoring using wake-up test or sensory-evoked potentials was performed in the early cases and motor and sensory-evoked potentials in the later cases. A midline skin incision was made to expose the posterior elements. In early cases, short segment fixation (a combination of hook and rod system) was used in patients who had OWO (Fig. 1) and pedicle screws were inserted at desired levels when the system become available in early 1990s. The Mehdian pedicular system (Corin, Cirencester, UK) was used in 22 patients and 9 patients had varied instrumentation systems (Hook and rod system were used in 5 cases and 4 patients had Universal Spinal Instrumentation system—pedicle screw with threaded rods (Ulrich, Ulm, Germany). Lateral whole spine radiographs were obtained intra-operatively for a level check and to confirm screw positioning. OWO was performed at L2/L3 or L3/L4 level, CWO was done at L2 or L3 with instrumentation from lower thoracic spine (T10/11/12) to S1 (Fig. 2) and PWO was performed between L2 and L5 with instrumentation from again from lower thoracic spine (T10/11/12) to S1 (Fig. 3).
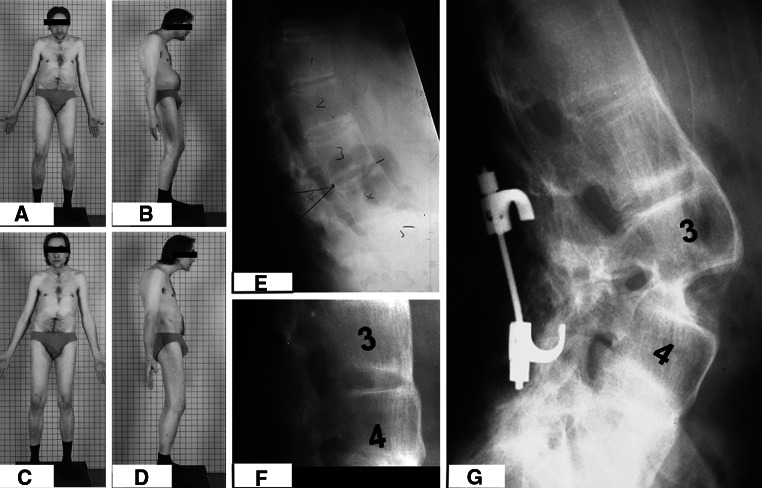
Fig. 1.
a, b The pre-operative photographs of a patient with AS and TKLD. Notice the protuberance of the abdomen on the lateral view. c, d The post-operative photographs following OWO technique. The patient worked as a cabinet maker and hence maximal correction was not performed to ensure that the patient had adequate horizontal gaze and also a functional degree of inferior vision to aid his profession. e The pre-operative radiographs of the same patient with TKLD, the opening wedge was planned at L3–4 interspace (f). f The follow-up radiograph with healed osteotomy site, correction was stabilized with hook and rod system
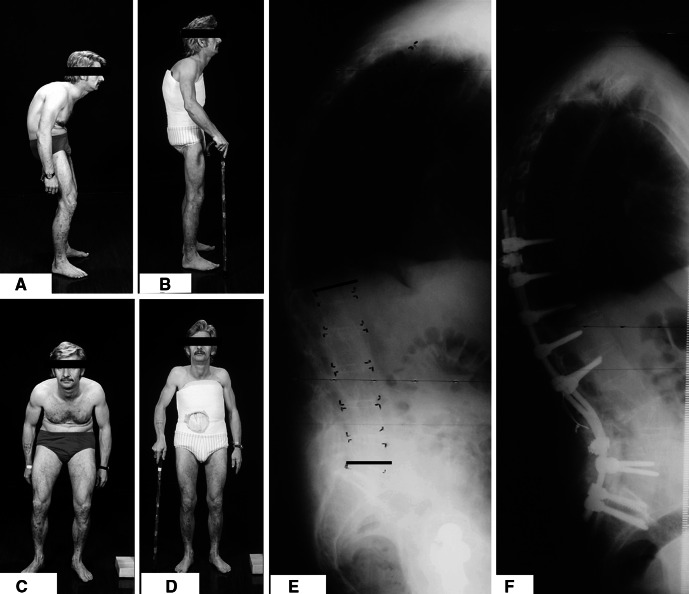
Fig. 2.
a, b The lateral pre- and post-operative photographs, respectively of an AS patient with TKLD, who underwent correction using the CWO technique. c, d The frontal photographs in the same patient pre- and post-op, notice the compressive effect on the abdomen by the inferior margins of the ribs which has been relieved following surgery. e The pre-operative lateral radiographs in the same patient, notice the TKLD and the loss of lumbar lordosis. f The post-operative lateral radiographs in the same patient, who underwent corrective osteotomy using CWO technique and instrumentation using pedicle screws and solid contoured rods
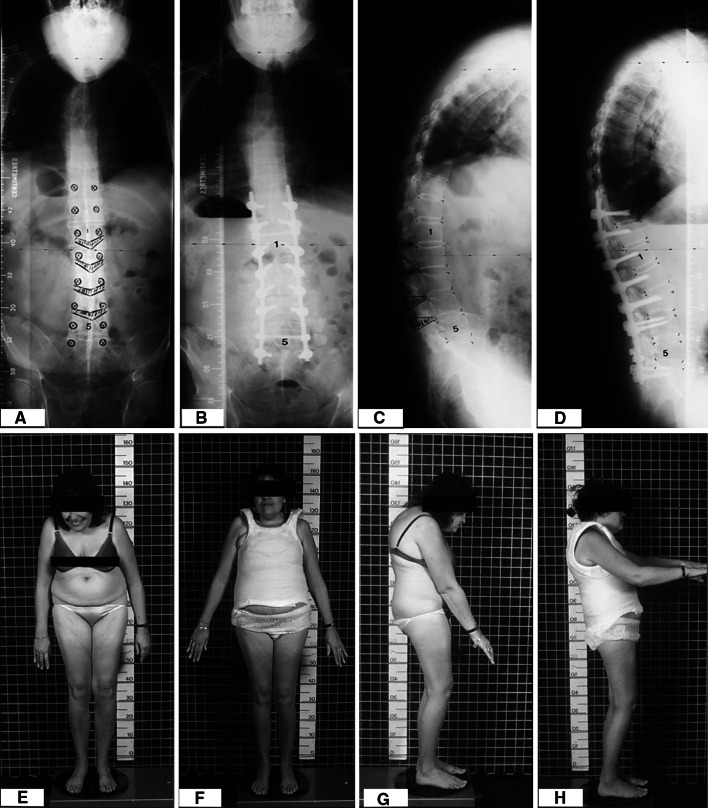
Fig. 3.
a, b The pre-operative antero-posterior whole spine radiographs, respectively, of another AS patient who underwent polysegmental wedge osteotomies (PWO). c, d The pre- and post-operative lateral radiographs in the same patient showing correction of her TKLD using PWO and instrumentation using pedicle screws and contoured solid rods. e, f The pre- and post-operative frontal photographs of the same patient, note that horizontal gaze has been restored. g, h The lateral photographs in the same patient
CWO consisted of removal of spinous process, lamina and pedicle to expose the thecal sac safely. Using curettes placed through the pedicle, decancellation of the vertebral body was performed to leave a thin shell of bone. Posterior cortical shell was fractured using Kerrison rongeurs. Correction was achieved by closure of posterior osteotomy without anterior column lengthening. In PWO, wedge osteotomies were created by the removal of superior and inferior articular processes bilaterally and also involved interlaminar spaces. In OWO, spinous processes, laminae, facet joints and pedicles at the desired level were removed to expose the thecal sac. Closure of osteotomy was performed by gentle manual extension.
In the initial 10 patients, correction manoeuvre involved manipulation using the fixation device and straightening of the flexed operating table that resulted in trunk extension. In the other 21 patients, the same technique was used with better control because malleable rods were used during correction to prevent sudden sagittal translation. After correction was achieved, the flexible rods were removed and replaced by contoured definitive rods.
Decortication of posterior elements was performed using Capner gouges or burr. Morcellised iliac crest autograft and local bone was used in all cases, however, in 10 recent cases, it was mixed with demineralized bone matrix. The wound was closed over two suction drains and all patients were treated in an intensive care unit following surgery. Patients were allowed out of bed as soon as was comfortable and were mobilized at 3–5 days after surgery. In the early years, a plaster jacket was used for up to 3 months, but later cases had a moulded thoraco-lumbo-sacral orthosis.
Radiographic assessment was performed using standard 36-in. long cassette and antero-posterior and lateral radiographs taken in the standing position. Radiographs were requested pre-operatively and post-operatively at 6, 12, 24, 52 weeks and annually thereafter. All radiographs were assessed by one of the authors who were independent of the operating team (RA and HVD). Parameters recorded included angle of lumbar lordosis, chin brow vertical angle (CBVA), sagittal vertical axis: horizontal distance of C7 plumb from the posterosuperior corner of L5/S1 disc and sacro-horizontal angle.
Clinical assessment included blood loss, intensive care unit (ICU) stay, and surgical time recordings. All patients were assessed clinically at regular intervals and outcome measures recorded included—Oswestry Disability Index (ODI), Visual Analogue Score (VAS) for pain, and SRS-22 (recorded in 23 patients). Appropriate statistical tests were used to test for significance of various clinical and radiological parameters.
Co-morbidities
Post-operatively, eight patients required total hip replacement and seven required corrective cervical osteotomy for severe cervicothoracic kyphotic deformity.
Results
The mean age at surgery was 54.7 years (40–74 years) and mean duration of symptoms was 3 years (range 5–8 years). Mean follow-up was 5 years (range 2–10 years). There was no statistically significant difference between the three techniques as regards mean duration of surgery and ICU stay. Mean duration of surgery was 7 h (range 4–9 h) (OWO cases had shorter period than CWO and PWO cases and the longest period was for CWO cases). Mean ICU stay was 3 days (range 2–20 days) (the period of stay was shorter in general for OWO and slightly longer for CWO and PWO). Blood loss was expressed as percentage of estimated blood volume (EBV). Mean blood loss in PWO was 23 ± 15.4% (range 9–36%), CWO was 28 ± 4.5% (range 12–40%) and in OWO was 15 ± 11% (range 13–99%). The clinical parameters are summarized in Table 1.
Table 1.
Clinical parameters
| CWO (mean ± SD) | OWO (mean ± SD) | PWO (mean ± SD) | |
|---|---|---|---|
| EBV | 28 ± 4.5% | 15 ± 11% (excluding outlier 99% in one case) | 23 ± 15.4% |
| Outcome measures | |||
| ODI | |||
| Pre-op | 48 ± 9.65 | 46.36 ± 7.89 | 47.4 ± 6.54 |
| Post-opa | 17.67 ± 5.58 | 15.64 ± 3.78 | 14.4 ± 3.5 |
| VAS | |||
| Pre-op | 7.08 ± 1.31 | 7.18 ± 1.17 | 7.3 ± 1.06 |
| Post-opa | 2.83 ± 0.83 | 2.55 ± 0.69 | 2.7 ± 0.67 |
aPost-op recordings are from 2-year follow-up
In comparison to pre-operative scores, statistically significant improvement was noted in all three groups in the post-operative period as regards ODI, VAS and SRS-22 (p = 0.001, Wilcoxon’s signed rank test). Mean ± SD pre-:post-op ODI in CWO, OWO and PWO was 48 ± 9.65:17.67 ± 5.58, 46.36±7.89:15.64 ± 3.78 and 47.4 ± 6.54:14.4 ± 3.5, respectively (Table 1). The mean pre-:post-op scores for VAS in CWO, OWO and PWO were 7.08 ± 1.31:2.83 ± 0.83, 7.18 ± 1.17:2.55 ± 0.69 and 7.3 ± 1.06:2.7 ± 0.67, respectively (Table 1). Table 2 shows the improvement noted in various domains of the SRS-22 and there was no significant difference between the three groups.
Table 2.
Improvement in SRS—22 domains
| CWO | OWO | PWO | |
|---|---|---|---|
| Pain | 17 ± 3.5 | 16 ± 4.5 | 14 ± 6 |
| Self-image | 18.4 ± 4.4 | 16.5 ± 3.5 | 17.6 ± 4.2 |
| Function | 17.5 ± 4.2 | 16 ± 3.3 | 17.2 ± 3.8 |
| Satisfaction | 8.2 ± 1.3 | 8.6 ± 1.7 | 7.7 ± 2.2 |
| Total score | 75 ± 14 | 72 ± 12.3 | 75 ± 15 |
Mean correction of kyphosis was 38° (range 25°–49°) with CWO, 28° with OWO (range 24°–38°) and 30° with PWO (range 28°–40°). Mean CBVA pre-:post-operatively in CWO, OWO and PWO was 35.33 ± 5.21:19.5 ± 1.51, 29.64 ± 5.35:11.45 ± 2.54 and 28.8 ± 5.01:12.8 ± 3.68, respectively. No change was seen in thoracic kyphosis in any group. The mean sacrohorizontal angle in CWO, OWO and PWO cases pre-:post-operatively were 9.33 ± 5.21:29.42 ± 7.27, 10.91 ± 2.43:24.82 ± 5.31 and 10.8 ± 1.69:32 ± 6.46, respectively. Sagittal vertical axis (cm) pre- and post-operatively were 14.5 ± 3.92:5.58 ± 3.34, 13.64 ± 3.44:4.45 ± 2.5 and 14 ± 4.22:7 ± 2.71 in CWO, OWO and PWO, respectively. The lumbar lordosis changed in the pre- and post-operative period in CWO, OWO and PWO from −15.42° ± 3.53°, −12.55° ± 2.98° and −13.3° ± 2.75° to −53.67° ± 4.12°, −31.64° ± 11.3° and −43.3° ± 5.58°, respectively (as summarized in Table 3).
Table 3.
Radiological parameters following corrective osteotomy
| CWO | OWO | PWO | |
|---|---|---|---|
| CBVA | |||
| Pre-op | 35.33 ± 5.21 | 29.64 ± 5.35 | 28.8 ± 5.01 |
| Post-opa | 19.5 ± 1.51 | 11.45 ± 2.54 | 12.8 ± 3.68 |
| Sacrohorizontal angle | |||
| Pre-op | 9.33 ± 5.21 | 10.91 ± 2.43 | 10.8 ± 1.69 |
| Post-opa | 29.42 ± 7.27 | 24.82 ± 5.31 | 32 ± 6.46 |
| Sagittal vertical axis (cm) | |||
| Pre-op | 14.5 ± 3.92 | 13.64 ± 3.44 | 14 ± 4.22 |
| Post-opa | 5.58 ± 3.34 | 4.45 ± 2.5 | 7 ± 2.71 |
| Lumbar lordosis (°) | |||
| Pre-op | −15.42 ± 3.53 | −12.55 ± 2.98 | −13.3 ± 2.75 |
| Post-opa | −53.67 ± 4.12 | −31.64 ± 11.3 | −43.3 ± 5.58 |
aPost-op values are from time of last follow-up minimum 2 years and average 5 years (range 2–10 years)
Complications
Table 4 lists the complications noted in this series. There was one intra-operative death of a patient who underwent OWO at the same level as a fracture sustained few years ago. During closure of the osteotomy, there was brittle failure of the bone in anterior vertebral body, significant adhesion and sagittal translation resulting in a sharp bony spike that caused aortic injury and catastrophic bleeding. After this case, the senior author started using malleable rods to prevent sagittal translation during the extension manoeuvre and no neurovascular sequelae have been noted since, in 21 patients, in whom this technique was used. 21 patients with a mild form of neuropraxia had recovered by 6 weeks. Superficial wound infection occurred in two patients and was treated with local wound care and antibiotics. Two patients required extension of instrumentation to sacrum.
Table 4.
List of intra-operative and post-operative complications
| Complication | OWO | CWO | PWO |
|---|---|---|---|
| Aortic injurya | 1 | 0 | 0 |
| L2/L3 nerve root palsya | 1 | 1 | 0 |
| Intra-operative dural tear | 2 | 1 | 1 |
| Superficial wound infection | 0 | 1 | 1 |
| Re-operation–epidural haematoma | 1 | 1 | 1 |
| Pseudarthrosis | 1 | 0 | 1 |
| Extension of instrumentation | 0 | 1 | 0 |
aMalleable rods not used during correction
Discussion
Corrective osteotomy for TLKD in AS helps the patient walk erect, improves balance and the gait efficiency. Forward vision is improved; the cervical spine assumes a more normal attitude thereby exhibiting an improved functional range of motion. The pressure of the abdominal organs on the diaphragm is relieved thereby increasing its excursion and the pulmonary vital capacity. Nutrition improves and patients experience a boost in their mental and social morale. Surgical osteotomy has also been reported to increase the patient’s chances of return to gainful employment [18]. Surgery has a big impact on the patient’s psyche and its a life changing event. If successful, surgery increases the patient’s mental abilities and unleashes a new life, socially [15]. Generally, surgery in AS is rewarding with good functional results [19]. Similar improvement in clinical outcomes was noted in our series. Although patients in the initial phase of the study did not have SRS-22 scores, similar improvement was noted in all domains in 21 patients in whom SRS-22 was recorded. A recent comprehensive review article, showed that corrective lumbar osteotomy for TLKD showed good outcome varying between 69 and 78% for the three different osteotomies based on the combined outcome scores from different studies [20]. They concluded that based on the existing data from several studies, it was not possible to determine the ideal method of corrective surgical treatment for TKLD in AS. One of the limitations may have been a lack of single surgeon case series to compare the results with all three types of osteotomies.
OWO was first described by Smith Peterson et al. [21]. The original technique involved osteotomies through the articular processes of L1, L2 and L3. The osteotomies were then closed by manual extension which resulted in the disruption of the anterior longitudinal ligament and opening of the anterior column. Around the same period, a two stage posterior—anterior opening wedge osteotomy was also described [22]. Over the years, several variations of this technique have been performed [10, 11, 15, 17, 18, 23–25]. However, elongation of the anterior column has been fraught with the risk of neurological and catastrophic vascular complications [11, 15, 26–28].
To overcome these complications, PWO was advocated [29]. Correction was achieved by closing multiple wedged osteotomies of the lamina and the articular processes. The anterior longitudinal ligament is not disrupted in this technique. This technique was thought to provide for more harmonious correction and better restoration of the lumbar lordosis. Hehne and Zielke [14] have advocated polysegmental wedged osteotomies with internal fixation.
CWO at a single level was described first by Scudese et al. [30]. Thomasen [31] described CWO in AS. In this technique lamina, articular processes, pedicles and a posterior wedge from the vertebral body are resected and closed with an anterior hinge. Thus, the anterior column is not lengthened making the procedure relatively safe. Different instrumentation techniques have been described for CWO for early stability and fusion [16, 31–33].
Secure fixation of the lumbar spine has been reported to influence results following lumbar osteotomy in AS [34]. Another study also showed that pedicle screw instrumentation in PWO yielded good results [35]. Initial cases in our series were performed using different forms of instrumentation [(5 Hook and rod, 4 Universal Spine Instrumentation Systems—pedicle screw with threaded rods (Ulrich, Ulm, Germany)]. The last 22 cases were all performed using pedicular instrumentation with solid rods. In agreement with the existing literature, instrumentation (providing for a rigid immobilization) facilitated early mobilization, rapid fusion and consistent good results. It was also noticed that a rigid fixation provided early pain relief and the degree of pain significantly improved with long-term follow-up probably due to spinal realignment. This has also has been reported in other series [17, 19]. As reported in earlier studies, with all three techniques the degree of lumbar correction achieved was maintained. However, sagittal balance deteriorated due to the active disease process and flexion deformities in other regions of the spine or hips. This necessitated total hip replacement in eight patients and corrective cervical osteotomy in seven patients, in our series. Loss of sagittal alignment due to flexing deformities in other regions during follow-up has also been noted in other series with medium to long-term follow-up.
In OWO, due to lengthening and opening up of the anterior column posterior implants are placed under considerable tension predisposing this form of osteotomy to a risk of non-union and hence eventual implant failure. This risk is not seen in CWO and PWO. However, in all three osteotomies, in order to achieve a good result, it is important to shift the gravity line of weight bearing as posteriorly as possible to place the osteotomy site under compression. Due to the nature of the disease, fusion however does not appear to be a problem in AS, especially with the newer stronger instrumentation systems. The author aims for extension of pedicle fixation to three to four levels above the osteotomy and routinely instruments inferiorly to the sacrum. The advantage in choosing L2 or L3 for osteotomy is that force concentration in prone positioning on the spinal table occurs at these levels, thereby providing a greater corrective force when the flexed table is extended and stays outside the conus. The degree of osteoporosis at the apical segments prevents satisfactory implant purchase and hence extension by a few segments cranially is preferred. Fusion to the sacrum in AS can cause problems with sitting on the floor due to a short distal lever arm [36]. However, this does not appear to be a problem in the western culture. Extension of instrumentation to the sacrum provides for a strong foundation and a rigid base for the long lever arm of correction. Implant failure or non-union was not noticed in any of our cases.
There was no difference in the surgical time and ICU stay between the three groups, but higher blood loss was noted in CWO and PWO groups. Two patients had transient neurological deficits and the overall complication rate is similar to that noted in previous reports [35, 37]. One unfortunate patient had catastrophic blood loss during correction of OWO. Our patient had sustained a fracture of the L3 vertebral body, which had been treated conservatively, 9 years before surgery. Postmortem examination confirmed aortic injury caused by a sharp bony spike lacerating the aorta which was adherent to the spine. A similar mechanism of spontaneous spinal fracture has been reported previously [38], and catastrophic bleeding due to rupture of the aorta during correction of deformity by a similar mechanism has also been reported in AS [39]. It is noteworthy, that in two patients who were noted to have neurological problems and one who had aortic injury, flexible rods were not used during correction. Several other authors have noted instances of neurologic problems leading to paraplegia, aortic ruptures, subluxation at the osteotomy site and mesenteric vessel thrombosis with paralytic ileus [9–12, 25, 27, 39, 40]. Mortality has been reported to be as high as 12%. [14].
In OWO, with careful patient selection, if the aorta is not calcified and the osteotomy level is below L2 lengthening of the anterior column can be performed relatively safely with a fairly low risk of neurovascular complications. Since the posterior restraining structures are resected prior to anterior column lengthening, a sudden instability is created when ALL disrupts in OWO. This can cause sagittal translation or if a fracture through the vertebral body occurs as in our case the bony spike can translate sagitally. If this uncontrolled sagittal translation occurs anteriorly, it can breach the aortic wall; if translation occurs posteriorly, it can cause neurological compromise. Although the ALL is thought to be intact in CWO and PWO, osteotomies at a single level aiming to achieve corrections greater than 35° are thought to be associated with some anterior hinge failure [20]. Hence, the risk of sagittal translation associated with the weakening of the anterior column, technically exists with all the three osteotomies, more so in OWO. To avoid these two complications, the senior author (SHM) advocates the use of malleable rods as a temporary stabilization. These flexible rods are fixed to the screws proximal to osteotomy site/sites and loosely fixed to all the screws distal to the osteotomy site/sites, therefore sagittal translation is prevented. This makes the extension manoeuvre more controlled and safe. Following the extension manoeuvre, the flexible rods can be tightened distally to provide temporary stabilization and these can then be replaced one side at a time with permanent rods. The temporary rods also act as an accurate template for contouring the stronger permanent rods. The senior author started using this flexible rod technique in 21 patients and no neurovascular sequelae have been noted since.
A meta-analysis of published studies on lumbar osteotomy in AS, reported that average correction was 3.8° lesser in CWO as compared to PWO and OWO [20]. However, in the current series, better radiographic correction was noted in CWO and PWO groups. This may be related to the degree of initial deformity, timing of surgery and mobility of intervertebral discs. The senior author prefers to use CWO and PWO as they result in good correction and are safer with lower risk of neurovascular sequelae. However, both these techniques are associated with increased blood loss and more levels of instrumentation. The senior author recommends the use of temporary flexible rods to prevent sagittal translation during the extension manoeuvre in all three types of osteotomies.
There appears to be a general decrease in the degree of severe TKLD in AS, perhaps due to better disease management and a greater awareness amongst general practitioners, leading to early referrals. This has lead to early surgery, with better corrections and good patient outcomes associated with lower risk of catastrophic neurovascular complications.
Conflict of interest
None.
References
- 1.Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379–1390. doi: 10.1016/S0140-6736(07)60635-7. [DOI] [PubMed] [Google Scholar]
- 2.Fox MW, Onofrio BM, Kilgore JE. Neurological complications of ankylosing spondylitis. J Neurosurg. 1993;78:871–878. doi: 10.3171/jns.1993.78.6.0871. [DOI] [PubMed] [Google Scholar]
- 3.Stafford L, Youssef PP. Spondyloarthropathies: an overview. Intern Med J. 2002;32:40–46. doi: 10.1046/j.1445-5994.2002.00132.x. [DOI] [PubMed] [Google Scholar]
- 4.Luken MG, Patel DV, Ellman MH. Symptomatic spinal stenosis associated with ankylosing spondylitis. Neurosurgery. 1982;11:703–705. doi: 10.1227/00006123-198211000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Braun J, Bollow M, et al. Prevalence of spondylarthropathies in HLA-B27 positive, negative blood donors. Arthritis Rheum. 1998;41:58–67. doi: 10.1002/1529-0131(199801)41:1<58::AID-ART8>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 6.Feldtkeller E, Khan MA. Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int. 2003;23:61–66. doi: 10.1007/s00296-002-0237-4. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurg Focus. 2008;24(1):E12. doi: 10.3171/FOC/2008/24/1/E12. [DOI] [PubMed] [Google Scholar]
- 8.Kubiak EN, Moskovich R, Errico TJ, Di Cesare PE. Orthopaedic management of ankylosing spondylitis. J Am Acad Orthop Surg. 2005;13(4):267–278. doi: 10.5435/00124635-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Goel MK. Vertebral osteotomy for correction of fixed flexion deformity of the spine. J Bone Joint Surg Am. 1968;50A:287–294. doi: 10.2106/00004623-196850020-00007. [DOI] [PubMed] [Google Scholar]
- 10.McMaster MJ, Coventry MB. Spinal osteotomy in ankylosing spondylitis: technique, complications, and long-term results. Mayo Clin Proc. 1973;48:476–487. [PubMed] [Google Scholar]
- 11.Adams JC. Technique, dangers and safeguards in osteotomy of the spine. J Bone Joint Surg Br. 1952;34-B:226–232. doi: 10.1302/0301-620X.34B2.226. [DOI] [PubMed] [Google Scholar]
- 12.Dawson CW. Posterior elementectomy in ankylosing arthritis of the spine. Clin Orthop. 1957;10:274–281. [PubMed] [Google Scholar]
- 13.Gerscovich EO, Greenspan A, Montesano PX. Treatment of kyphotic deformity in ankylosing spondylitis. Orthopedics. 1994;17:335–342. doi: 10.3928/0147-7447-19940401-07. [DOI] [PubMed] [Google Scholar]
- 14.Hehne HJ, Zielke K, Böhm H. Polysegmental lumbar osteotomies and transpedicled fixation for correction of long-curved kyphotic deformities in ankylosing spondylitis: report on 177 cases. Clin Orthop. 1990;258:49–55. [PubMed] [Google Scholar]
- 15.Camargo FP, Cordeiro EN, Napoli MM. Corrective osteotomy of the spine in ankylosing spondylitis. Experience with 66 cases. Clin Orthop. 1986;208:157–167. [PubMed] [Google Scholar]
- 16.Van Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Br. 1995;77-B:117–121. [PubMed] [Google Scholar]
- 17.Chang K-W, Chen Y-Y, Lin C-C, Hsu H-L, Pai K-C. Closing wedge osteotomy versus opening wedge osteotomy in ankylosing spondylitis with thoracolumbar kyphotic deformity. Spine. 2005;30(14):1584–1593. doi: 10.1097/01.brs.0000170300.17082.49. [DOI] [PubMed] [Google Scholar]
- 18.McMaster MJ. A technique for lumbar spinal osteotomy in ankylosing spondylitis. J Bone Joint Surg Br. 1985;67:204–210. doi: 10.1302/0301-620X.67B2.3980526. [DOI] [PubMed] [Google Scholar]
- 19.Halm H, Metz-Stavenhagen P, Zielke K. Results of surgical correction of kyphotic deformities of the spine in ankylosing spondylitis on the basis of the modified arthritis impact measurement scales. Spine. 1995;20(14):1612–1619. doi: 10.1097/00007632-199507150-00010. [DOI] [PubMed] [Google Scholar]
- 20.Van Royen BJ, De Gast A. Lumbar osteotomy for correction of treatment of thoracolumbar kyphotic deformity in ankylosing spondylitis. A structured review of three methods. Ann Rheum Dis. 1999;58:399–406. doi: 10.1136/ard.58.7.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg. 1945;27:1–11. [PubMed] [Google Scholar]
- 22.La Chapelle EH. Osteotomy of the lumbar spine for correction of kyphosis in a case of ankylosing spondylarthritis. J Bone Joint Surg. 1946;28:851–858. [PubMed] [Google Scholar]
- 23.Bossers GT. Columnotomy in severe Bechterew kyphosis. Acta Orthop Belg. 1972;38:47–54. [PubMed] [Google Scholar]
- 24.Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop. 1977;128:65–77. [PubMed] [Google Scholar]
- 25.Emnéus H. Wedge osteotomy of spine in ankylosing spondylitis. Acta Orthop Scand. 1968;39:321–326. doi: 10.3109/17453676808989465. [DOI] [PubMed] [Google Scholar]
- 26.Weatherley C, Jaffray D, Terry A. Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine. 1988;13:43–46. doi: 10.1097/00007632-198801000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Herbert JJ. Vertebral osteotomy for kyphosis, especially in Marie–Strumpell arthritis. J Bone Joint Surg Am. 1959;41A:291–302. [PubMed] [Google Scholar]
- 28.Law WA. Osteotomy of the spine. Clin Orthop. 1969;66:70–76. [PubMed] [Google Scholar]
- 29.Wilson MJ, Turkell JH. Multiple spinal wedge osteotomy. Its use in a case of Marie Strümpell spondylitis. Am J Surg. 1949;77:777–782. doi: 10.1016/0002-9610(49)90148-8. [DOI] [PubMed] [Google Scholar]
- 30.Scudese VA, Calabro JJ. Vertebral wedge osteotomy. Correction of rheumatoid (ankylosing) spondylitis. JAMA. 1963;186:627–631. doi: 10.1001/jama.1963.03710070029006. [DOI] [PubMed] [Google Scholar]
- 31.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop. 1985;194:142–152. [PubMed] [Google Scholar]
- 32.Jaffray D, Becker V, Eisenstein S. Closing wedge osteotomy with transpedicular fixation in ankylosing spondylitis. Clin Orthop. 1992;279:122–126. [PubMed] [Google Scholar]
- 33.Thiranont N, Netrawichien P. Transpedicular decancellation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine. 1993;18:2517–2522. doi: 10.1097/00007632-199312000-00023. [DOI] [PubMed] [Google Scholar]
- 34.Weale AE, Marsh CH, Yeoman PM (1995) Secure fixation of lumbar osteotomy. Surgical experience with 50 patients. Clin Orthop Relat Res (321):216–222 [PubMed]
- 35.van Royen BJ, de Kleuver M, Slot GH. Polysegmental lumbar posterior wedge osteotomies for correction of kyphosis in ankylosing spondylitis. Eur Spine J. 1998;7(2):104–110. doi: 10.1007/s005860050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim K-T, Suk K-S, Cho Y-J, Hong G-P, Park B-J. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine. 2002;27(6):612–618. doi: 10.1097/00007632-200203150-00010. [DOI] [PubMed] [Google Scholar]
- 37.Willems KF, Slot GH, Anderson PG, Pavlov PW, de Kleuver M. Spinal osteotomy in patients with ankylosing spondylitis: complications during first postoperative year. Spine. 2005;30(1):101–107. doi: 10.1097/00007632-200501010-00018. [DOI] [PubMed] [Google Scholar]
- 38.Rapp GF, Kernek CB. Spontaneous fracture of the lumbar spine with correction of deformity in ankylosing spondylitis. J Bone Joint Surg Am. 1974;56(6):1277–1278. [PubMed] [Google Scholar]
- 39.Klems H, Friedebold G. Rupture of the abdominal aorta following a corrective spinal operation for ankylopoietic spondylitis. Z Orthop Ihre Grenzgeb. 1971;108(4):554–563. [PubMed] [Google Scholar]
- 40.McMaster PE. Osteotomy of the spine for fixed flexion deformity. Pac Med Surg. 1965;73:314. [PubMed] [Google Scholar]