Abstract
We evaluated the reliability and validity of an adapted Korean version of the Roland–Morris Disability Questionnaire (RMDQ). Translation/retranslation of the English version of RMDQ was conducted, and all steps of the cross-cultural adaptation process were performed. The Korean version of the Visual Analog Scale (VAS) measure of pain, RMDQ, and the previously validated Oswestry Disability Index (ODI) were mailed to 100 consecutive patients with chronic lower back pain (LBP) of at least 3 months. Eighty-one patients responded to the first mailing of questionnaires and 63 of the first-time responder returned their second survey. The average age of the 63 patients (45 female, 18 male) was 47.8 years. Reliability assessment was determined by estimating kappa statistics of agreement for each item, the intraclass correlation coefficient (ICC), and Cronbach’s α. Concurrent validity was evaluated by comparing the responses of RMDQ with the results of VAS and responses of ODI by using Pearson’s correlation coefficient. The constructed Bland–Altman plot showed a good reliability. All items had a kappa statistics of agreement greater than 0.6. The RMDQ showed excellent test/re-test reliability as evidenced by the high ICC for 2 test occasions (ICC = 0.932, P < 0.001). Internal consistency was found to be very good at both assessments with Cronbach’s α (0.942 and 0.951 at first and second assessments, respectively). The RMDQ was correlated with the VAS (r = 0.692; P = 0.000 and r = 0.668; P = 0.000 at first and second assessments, respectively), and with the ODI (r = 0.789; P = 0.000 and r = 0.802; P = 0.000, respectively). The adapted Korean version of the RMDQ was successfully translated and showed acceptable measurement properties, and as such, is considered suitable for outcome assessments in the Korean speaking patients with LBP.
Keywords: Low back pain, Roland–Morris Disability Questionnaire, Korean version
Introduction
Low back pain (LBP) is a major health problem and can have a profound impact on individual functional activity. The aim of treatment is to improve patient function, and thus functional status is an important outcome variable in clinical trials that investigate LBP. During recent years, there has been a tendency to supplement objective assessments of the spine with subjective measures of functional status using validated questionnaires in patients with LBP.
A variety of outcome measures are used to assess LBP, and the Roland–Morris Disability Questionnaire (RMDQ) is one of the most common instruments used to assess the functional status of patients with LBP [16]. The RMDQ is a self-completed measure of disability, and was developed by selecting statements from the Sickness Impact Profile [3]. In particular, the phrase “because of my back” was added to relevant questions in the RMDQ to elicit back pain-specific responses. Studies have reported that the test/re-test reliability, validity and responsiveness of RMDQ are adequate [16, 17], and, it has been successfully adapted across cultures. Thus, the objectives of this study were to translate into the Korean language a culturally adapted version of the RMDQ and to validate this Korean version of the RMDQ in Korean LBP patients.
Materials and methods
The translation and adaptation processes were carried out by following published guidelines for the process of cross-cultural adaptation of self-report measures [1]. The translation procedure in this study had three stages, namely, forward translation, back translation, and an expert committee discussion. A pilot study was then performed to test whether the prefinal version could be understood correctly by Korean LBP patients. The final version was obtained by expert committee discussion and tested for its validity and reliability together with the Korean version of the Oswestry Disability Index (ODI) questionnaire [7].
The forward translation was completed by two native Korean translators. The first translator, also the author of this article, is an orthopedic surgeon, and the other is a professional translator, with no medical background, who was not initially informed of the purpose of the translation. The two translators’ versions and the original version were compared and discussed by the two translators and an orthopedic professor, until a synthesis of the translation was reached.
The back translation was completed by two bilingual translators whose native language was English. They independently translated the synthetic version into English. Both of these translators lacked medical background and were not informed or aware of the prior translation procedures.
All the versions of the translation, as well as the original, were put together and discussed by the four translators and an expert committee with three bilingual experts, two orthopedic professors and a Korean translation expert. This committee discussed the translation procedure and results until a consensus was reached on discrepancies. Accordingly, based on the synthetic forward translation, the prefinal version of RMDQ was created.
This prefinal version of the RMDQ was given to 30 Korean-speaking patients with chronic LBP of at least 3 months’ duration who were receiving one or more therapeutic interventions (non-steroidal anti-inflammatory drug medication and/or physical therapy) at another spine center. Subsequently, these patients were questioned regarding their understanding of the questionnaire items and their responses. These 30 patients included 18 females and 12 males with a mean age of 48.5 ± 6.3 years. The interviewer was asked to document any problems that occurred during the administration of the questionnaire. In addition, at the end of the interview each patient was asked to provide comments about the questionnaire and to identify any words that were difficult to understand. No patients declined to complete it and the majority of the patient correctly understood the questionnaire. On the basis of their comments, the final version was developed by the expert committee (see Appendix).
The Korean version of the Visual Analog Scale (VAS) measure of pain, RMDQ and ODI were mailed to 100 consecutive patients with chronic LBP of at least 3 months’ duration who were receiving one or more therapeutic interventions (non-steroidal anti-inflammatory drug medication and/or physical therapy) at another spine center. All patients had been previously investigated by physical and neurologic examination, spine radiographs, and laboratory tests had been performed to identify the non-mechanical causes of LBP. Patients suspected of having a non-mechanical LBP and those with neurologic deficit were excluded in the study. First mailing contained a consent form, a description of the study, the Korean versions of VAS measure of pain, RMDQ and ODI, and an addressed and stamped return envelope. Eighty-one patients (56 female, 25 male) responded to the first set of questionnaires. Sixty-three (45 female, 18 male) of the first-time respondents returned their second survey. The average age of the 63 patients was 47.8 ± 7.6 years. The average time between the first and the second mailings was 2 weeks.
Test–retest reliability was measured by comparing responses to the first and second administrations of RMDQ. Reliability was assessed using kappa statistics of agreement for each item and the intraclass correlation coefficient (ICC). Cronbach’s α was used to evaluate internal consistency. Concurrent validity was evaluated by comparing the responses of RMDQ with the results of VAS and responses of ODI by using Pearson’s correlation coefficient. All statistical analyses were performed with the SPSS version 16.0.
Results
A total of 81 native Korean-speaking patients with chronic LBP were enrolled in this study. Sixty-three patients completed the second assessment. None of the patients had undergone surgery. Neurological examinations and laboratory tests (complete blood count, erythrocyte sedimentation rate and C-reactive protein) were normal for all study subjects. Table 1 summarizes the demographic and clinical characteristics of the study population.
Table 1.
The demographic and clinical characteristics of the study population
| First assessment (n = 81) | Second assessment (n = 63) | |
|---|---|---|
| Age (years) | 48.7 ± 7.4 | 47.8 ± 7.6 |
| Education (years) | 13.1 ± 2.5 | 13.1 ± 2.7 |
| Pain duration (months) | 22.9 ± 10.7 | 23.8 ± 11.6 |
| VAS (mm) | 53.1 ± 18.5 | 51.9 ± 16.9 |
| ODI (%) | 22.6 ± 9.2 | 23.3 ± 8.6 |
| RMDQ | 9.7 ± 4.2 | 10.1 ± 3.6 |
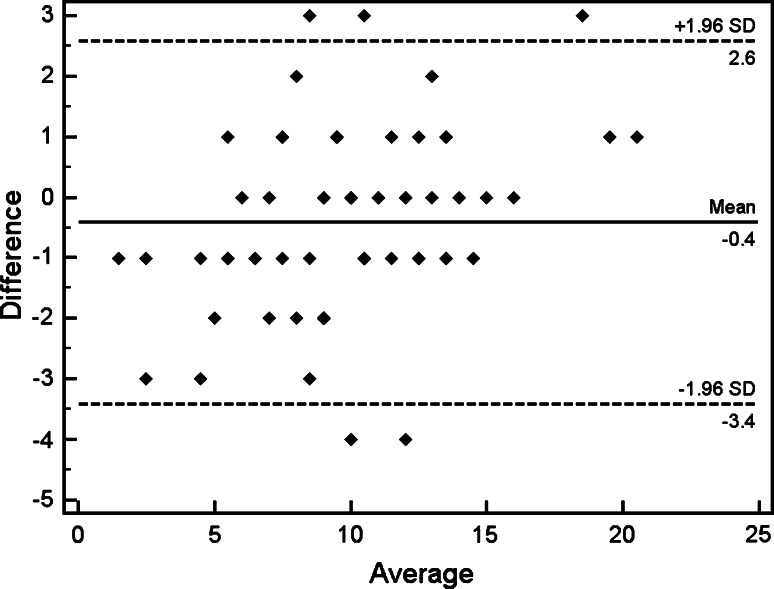
The constructed Bland–Altman plot for test/re-test agreement showed a good reliability (Fig. 1). All items had a kappa statistics of agreement greater than 0.6 and ranged from 0.72 to 0.92. The RMDQ showed excellent test/re-test reliability as evidenced by the high ICC for two assessments (ICC = 0.932, P < 0.001). In addition, internal consistency of RMDQ was found to be very good at both assessments with Cronbach’s α (0.942 and 0.951 at first and second assessments, respectively) (Table 2).
Fig. 1.
Bland Altman plot for test/re-test reliability of the Korean version of the Roland–Morris Disability Questionnaire between first and second assessments
Table 2.
Values of Cronbach α if the question was excluded
| The RMDQ | First assessment (n = 81) | Second assessment (n = 63) |
|---|---|---|
| Staying at home most of the time | 0.939 | 0.948 |
| Changing position frequently | 0.941 | 0.951 |
| Walking more slowly than usual | 0.937 | 0.949 |
| Not doing any of the jobs | 0.947 | 0.954 |
| Using a handrail to get upstairs | 0.947 | 0.954 |
| Lying down to rest more often | 0.948 | 0.954 |
| Holding on to something | 0.941 | 0.951 |
| Trying to get other people to do | 0.942 | 0.951 |
| Getting dressed more slowly | 0.938 | 0.948 |
| Standing for short periods of time | 0.943 | 0.950 |
| Trying not to bend | 0.942 | 0.951 |
| Getting out of chair | 0.947 | 0.955 |
| Back is painful | 0.937 | 0.948 |
| Turning over in bed | 0.941 | 0.951 |
| Appetite is not very good | 0.942 | 0.951 |
| Putting on my socks | 0.937 | 0.944 |
| Walking short distances | 0.943 | 0.951 |
| Sleeping less well | 0.941 | 0.950 |
| Getting dressed with help | 0.941 | 0.951 |
| Sitting down for most of the day | 0.942 | 0.952 |
| Avoiding heavy jobs | 0.947 | 0.955 |
| Being more irritable | 0.943 | 0.950 |
| Going upstairs more slowly | 0.939 | 0.947 |
| Stay in bed most of the time | 0.943 | 0.950 |
Concurrent validity was evaluated by comparing the responses to the RMDQ with the results of VAS by using the Pearson correlation coefficient and positive correlations between RMDQ and VAS were found for both for first and second assessments (r = 0.692; P = 0.000 and r = 0.668; P = 0.000, respectively). In addition, the correlation between the Korean version of the RMDQ and the Korean version of the modified ODI was used to test the construct validity and similarly, significant positive correlations were determined between these evaluations for both first and second assessments (r = 0.789; P = 0.000, and r = 0.802; P = 0.000, respectively).
Discussion
The objectives of this study were to produce a Korean version of RMDQ by translation and adaption. The Korean version of RMDQ appeared to be clearly understood and easily administered to the patients. The structure of the original RMDQ was not altered, and all of its 24 items were maintained. The results of this study indicate that the Korean version of the RMDQ is a reliable and valid instrument for measuring outcome in Korean LBP patients and its reliability levels were similar to those of the the French [4], German [19], Italian [13], Spanish [9], Tunisian [2], and Turkish versions [11].
Regarding internal consistency, Roland and Fairbank [15] recommended an acceptable range of 0.7–0.9. The Cronbach’s α values obtained from the Korean version of the RMDQ were 0.942 and 0.951 at first and second assessments, respectively, and were similar to those reported by other studies [2, 4, 9, 11, 13, 19]. This result shows that this translated version is reliable and has a low standard error of measurement.
The reproducibility of each of the 24 items was satisfactory with kappa statistics of agreement superior to 0.6 in our study. However, some authors have reported an average reproducibility of item 10 to see lower for other items. It was case of the French version with kappa value of 0.6 for item 10 and 0.45 for item 14 [4], and case of the Moroccan version with 0.47 for item 10 [12]. The results were explained by some patients answering “yes” to an item in the first visit and “no” in the second visit, and these patients probably had to wait for a longer time than others for consultation before being received for the interview, which perhaps was not the case at the second visit [12]. To avoid this bias, we mailed the Korean version of VAS for pain, RMDQ and ODI to 100 consecutive patients with chronic LBP. The agreement of all the items was very good in this study. In fact, an ICC of 0.932 is a very good measure of reliability of the Korean version of the RMDQ and is in accordance with other translated versions with ICCs ranging from 0.87 to 0.93 [4, 8, 9, 12].
Reliability of functional status questionnaires may be measured using an interval of 1–2 weeks between assessments, because during this time clinical status is unlikely to change appreciably in patients with chronic pain in the absence of a specific intervention [8], and thus we used this in the present study. Because this study was performed by survey with mail, the time of survey was relatively short, 18 patients of 81 first-time respondents dropped out of the second survey.
Our analysis of concurrent validity showed positive correlation between the Korean version of RMDQ and VAS, and analysis of construct validity showed a significant correlation between the Korean version RMDQ and ODI. In particular, disability scales correlated well with each other, which is consistent with the observed results in other studies [5, 10, 14, 18]. Our study showed the distribution of Korean version of RMDQ scores was greater than that of ODI. In order to reduce floor and ceiling effects, the Korean version of RMDQ could be recommended in Korean patients with relatively little disability and the Korean version of ODI in Korean patients with severe disability.
There were some limitations to this study. Although Short-form 36-Item Health Survey (SF-36) is a widely used health status measure, we compared the Korean version of RMDQ with ODI because the properties of the RMDQ and ODI were very similar. Although the Korean version of SF-36 has previously developed and tested at the Japanese institute [6], Korean surgeons are more familiar with Korean version of ODI than the SF-36.
To the authors’ knowledge, this Korean version of the RMDQ is the first condition-specific outcome instrument for LBP to be validated in a Korean population. The development and validation of multiple-language versions of existing validated questionnaires plays a key role in standardizing outcome measurements and increasing the statistical powers of clinical studies. The results of this study demonstrated that the RMDQ was successfully translated into Korean without losing the psychometric properties of the original version. Accordingly, the Korean version of the RMDQ appears to be a reliable and valid outcome measure for the assessment of functional status in patients with LBP. Thus, we recommend that this Korean version of the RMDQ can be utilized for future clinical studies in Korea.
Conflict of interest
None.
Appendix
The Korean version of Roland-Morris Disability Questionnaire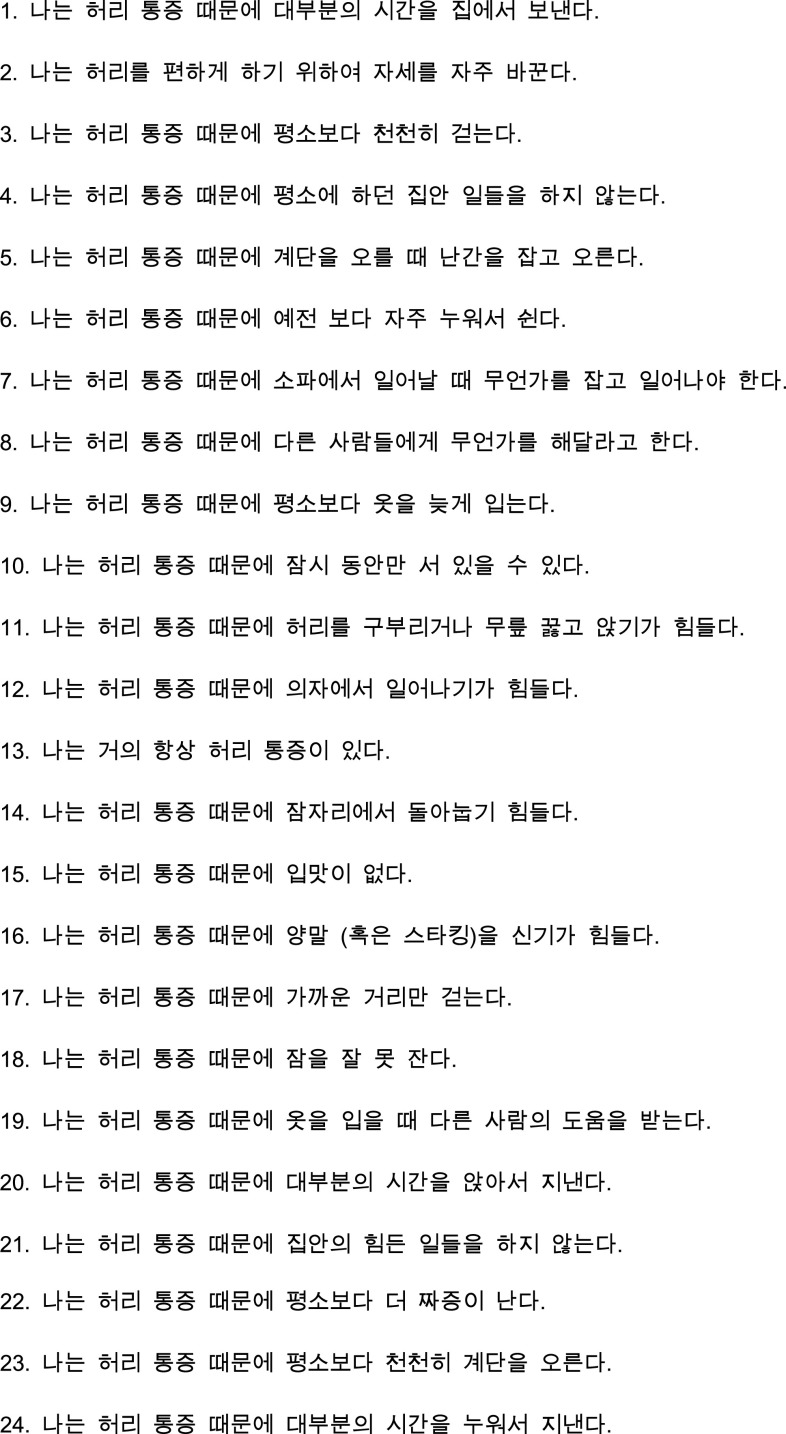
References
- 1.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 2.Bejia I, Younes M, Kamel BS, Letaief M, Touzi M, Soltani M, Bergaoui N. Validation of the Tunisian version of the Roland–Morris questionnaire. Eur Spine J. 2005;14:171–174. doi: 10.1007/s00586-004-0730-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bergner M, Bobbitt RA, Kressel S, Pollard WE, Gilson BS, Morris JR. The sickness impact profile: conceptual formulation and methodology for the development of a health status measure. Int J Health Serv. 1976;6:393–415. doi: 10.2190/RHE0-GGH4-410W-LA17. [DOI] [PubMed] [Google Scholar]
- 4.Coste J, Le Parc JM, Berge E, Delecoeuillerie G, Paolaggi JB. French validation of a disability rating scale for the evaluation of low back pain (EIFEL questionnaire) Rev Rhum Ed Fr. 1993;60:335–341. [PubMed] [Google Scholar]
- 5.Deyo R, Diehl A. Measuring physical and psychosocial function in patients with low-back pain. Spine. 1983;8:635–642. doi: 10.1097/00007632-198309000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patents of in Korea. Tohoku J Exp Med. 2004;203:189–194. doi: 10.1620/tjem.203.189. [DOI] [PubMed] [Google Scholar]
- 7.Jeon CH, Kim DJ, Kim SK, Kim DJ, Lee HM, Park HJ. Validation in the cross-cultural adaptation of the Korean version of the Oswestry Disability Index. J Korean Med Sci. 2006;21:1092–1097. doi: 10.3346/jkms.2006.21.6.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johansson E, Lindberg P. Subacute and chronic low back pain: Reliability and validity of a Swedish version of the Roland and Morris Disability Questionnaire. Scand J Rehabil Med. 1998;30:139–143. doi: 10.1080/003655098444066. [DOI] [PubMed] [Google Scholar]
- 9.Kovacs FM, Llobera J, Gil Del Real MT, Abraira V, Gestoso M, Fernandez C, KA Primaria Group Validation of the Spanish version of the Roland–Morris questionnaire. Spine. 2002;27:538–542. doi: 10.1097/00007632-200203010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Kroner-Herwig B, Jakle C, Frettloh J, Peters K, Seemann H, Franz C, Basler HD. Predicting subjective disability in chronic pain patients. Int J Behav Med. 1996;3:30–41. doi: 10.1207/s15327558ijbm0301_3. [DOI] [PubMed] [Google Scholar]
- 11.Kucukdeveci AA, Tennant A, Elhan AH, Niyazoglu H. Validation of the Turkish version of the Roland–Morris Disability Questionnaire for use in low back pain. Spine. 2001;26:2738–2743. doi: 10.1097/00007632-200112150-00024. [DOI] [PubMed] [Google Scholar]
- 12.Maaroufi H, Benbouazza K, Faik A, Bahiri R, Lazrak N, Abouqal R, Amine B, Hajjaj-Hassouni N. Translation, adaptation, and validation of the Moroccan version of the Roland–Morris Disability Questionnaire. Spine. 2007;32:1461–1465. doi: 10.1097/BRS.0b013e318060a63d. [DOI] [PubMed] [Google Scholar]
- 13.Padua R, Padua L, Ceccarelli E, Romanini E, Zanoli G, Bondi R, Campi A. Italian version of the Roland Disability Questionnaire, specific for low back pain: cross-cultural adaptation and validation. Eur Spine J. 2002;11:126–129. doi: 10.1007/s005860100262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rainville J, Ahern DK, Phalen L, Childs LA, Sutherland R. The association of pain with physical activities in chronic low back pain. Spine. 1992;17:1060–1064. doi: 10.1097/00007632-199209000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Roland M, Fairbank J. The Roland–Morris Disability questionnaire and the Oswestry disability questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Roland M, Morris R. A study of the natural history of back pain: 1. Development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Stratford PW, Binkley JM, Riddle DL, Guyatt GH. Sensitivity to change the Roland–Morris back pain Questionnaire: Part 1. Phys Ther. 1998;78:1186–1196. doi: 10.1093/ptj/78.11.1186. [DOI] [PubMed] [Google Scholar]
- 18.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 19.Wiesinger GF, Nuhr M, Quittan M, Ebenbichler G, Wolfl G, Fialka-Moser V. Cross-cultural adaptation of the Roland–Morris questionnaire for German-speaking patients with low back pain. Spine. 1999;24:1099–1103. doi: 10.1097/00007632-199906010-00009. [DOI] [PubMed] [Google Scholar]