Abstract
Background
Elevated scores on depression symptom questionnaires predict rehospitalization after acute myocardial infarction (AMI). Whether DSM-IV depressive disorders predict rehospitalization after AMI is unknown.
Methods and Results
Participants (n=766) in an ENRICHD ancillary study were classified by diagnostic interview as having no depression, minor depression, or major depression after AMI. Cardiac rehospitalizations were tracked for up to 42 months. Cox proportional hazards regression was used to model the effect of depressive disorder on time to first cardiac rehospitalization, controlling for mortality risk factors. Logistic regression was used to compare the accuracy with which rehospitalization could be predicted by depression diagnosis or by the Beck Depression Inventory (BDI). Secondary analyses examined the effects of depression on the cumulative number of all-cause rehospitalizations, length of stay, and emergency department visits. Compared to nondepressed patients, those with either major or minor depression were hospitalized sooner (minor: adjusted HR, 2.22; 95% CI, 1.59 to 3.08; P<.001; major: adjusted HR, 2.54; 95% CI, 1.84 to 3.53; P<.001), had more hospitalizations (minor: P<.001; major: P<.001) and emergency department visits (minor: P=.003; major: P<.001), and spent more days in the hospital (minor: P<.001; major: P<.001). The interview and questionnaire methods of assessing depression did not significantly differ in their overall accuracy of predicting rehospitalization.
Conclusions
Depressive disorders increase the risk of rehospitalization after AMI. Future work should focus on developing multivariable models to predict risk of rehospitalization after AMI, and depression should be included in these.
Keywords: myocardial Infarction, depression, depressive disorder, patient readmission
Heart disease remains the number one cause of death in the United States, with coronary heart disease (CHD) being responsible for one out of every six deaths in 2007(1). However, CHD mortality rates have declined in recent decades, leading to an increased focus on the health care and economic burdens of chronic coronary disease. Recent reports highlight the frequency and high cost of hospital readmissions related to acute myocardial infarction (AMI) and other manifestations of CHD. Of the patients who survive an index hospitalization for acute coronary syndrome (ACS), between 21 and 33% are rehospitalized within one year (2, 3). The estimated cost of hospitalization for ACS ranges from around $13,000 to almost $30,000 (3–6), and there is evidence that the cost of a readmission is at least as high as that of the index hospitalization (3). Rehospitalizations account for a majority of the annual cardiovascular-related expenditures in the first year following index admission for ACS (3, 4). Hospital readmissions also affect patients’ quality of life, and in younger patients who are still employed, readmissions result in lost work days and potential difficulty in maintaining employment. For all these reasons, it is important to identify factors that are associated with increased risk of rehospitalization among patients with coronary disease. The identification of risk factors that are potentially modifiable would be particularly useful.
Depression is an independent predictor of cardiac and all-cause mortality following ACS (7–9). There is also evidence that individuals with symptoms of depression are more likely to be rehospitalized within the first year after AMI (10–14). For instance, Frasure-Smith et al. (10) reported that in the first year after hospitalization for MI, patients with a Beck Depression Inventory (BDI) (15) score of 10 or higher were more likely to be readmitted and spent more days in the hospital compared to those who scored below 10. Similar findings have been reported by Parashar et al. (13) and Smolderen et al. (14) using a cutoff score of 10 on the Patient Health Questionnaire (16). However, these studies used self-report depression screening questionnaires rather than diagnostic interviews to identify depression. Carney et al. (17) reported that the standard cutoff score of 10 on the BDI failed to identify approximately 20% of the depressive disorders in a group of patients with coronary disease. The specificity of depression screening questionnaires is also limited in cardiac patients because some of the symptoms of depression, such as fatigue and poor appetite, overlap with symptoms of medical illness.
The current study investigated whether major and minor depressive disorders, assessed by a diagnostic interview, predict time to first cardiac rehospitalization during a 42-month follow-up after index hospitalization for AMI. To our knowledge, this is the first study to examine this relationship using Diagnostic and Statistical Manual-IV (DSM-IV) criteria for depression (18) rather than a self-report inventory of depressive symptoms. We also compared the discrimination ability of the BDI with that of the diagnostic interview, to determine whether one was a more accurate predictor of readmissions than the other. As a secondary aim, we examined the relationships between depression status and cumulative number of rehospitalizations, cumulative number of emergency department (ED) visits, and the cumulative length of hospital stay (LOS) across all hospitalizations during the follow-up period.
Methods
Participants and Data Collection
Patients were screened for eligibility to participate in the Enhancing Recovery and Coronary Heart Disease (ENRICHD) trial between October 1997 and January 2000 (19). The current sample is limited to patients who were admitted for acute myocardial infarction at one of the four ENRICHD clinical trial sites (Washington University, St. Louis, MO; Duke University, Durham, NC; Harvard University, Boston, MA; and Yale University, New Haven, CT) that participated in an ENRICHD ancillary study, the detailed methods of which have been previously reported (20). Patients were eligible to participate if they had evidence of AMI, as documented by cardiac enzymes and chest pain consistent with acute AMI, characteristic evolutionary ST-T changes, or new Q waves. Although the ENRICHD trial was limited to patients who met criteria for depression and/or low perceived social support, the ancillary study also included a comparison group of patients who consented to participate in ENRICHD and were otherwise eligible, but who did not meet study criteria for depression or low social support. Patients were excluded from the study if they (1) had another life-threatening medical illness, significant cognitive impairment, or another major psychiatric disorder; (2) lived too far away, were too ill, or were unable to participate for other logistical reasons; (3) were currently taking tricyclic or monoamine oxidase inhibitor antidepressants; or (4) refused to participate.
The Depression Interview and Structured Hamilton (DISH) (21) was used to determine depression status on the basis of the DSM-IV diagnostic criteria. The BDI, a 21-item self-report inventory of depressive symptoms, was used to assess severity of depression (15). To be eligible for the ENRICHD trial, patients had to meet DSM-IV criteria for a current major or minor depressive episode (18), or have a past history of major depression and meet the criteria for a current episode for at least seven days (instead of the DSM-IV defined 14 days). Patients who met the modified criteria for major or minor depression on the interview and who scored at least 10 on the BDI were enrolled. The present study included patients in both the usual care and the intervention arm of the ENRICHD trial. Control participants did not meet diagnostic criteria for major or minor depression or dysthymia, had no prior episodes of major depression, and scored less than 10 on the BDI. Controls and depressed patients were enrolled concurrently, but the control sample was limited to 120% of the depressed sample.
Medical record reviews were conducted to document history of coronary disease and revascularization, current medications, medical comorbidities, and major risk factors for coronary heart disease.
Follow-up assessments were conducted 6 months after enrollment and then annually, for up to 42 months. Study staff identified potential end points through follow-up visits, telephone calls, medical record surveillance, and physician contacts. All reported hospitalizations were confirmed through medical record review, and all reported deaths were confirmed by examination of death certificates. Cardiovascular rehospitalizations were the primary end point for this study.
The study was approved by the institutional review board at each study site, and all participants provided written informed consent.
Statistical Analysis
Chi-square tests and analysis of variance (ANOVA) models were fitted to compare the depression groups on demographic and medical characteristics at baseline.
The primary outcome, defined as the time to first cardiac rehospitalization during follow up, was censored on the date of the patient’s death or on the date of last contact if the patient was lost to follow-up. For time-to-event analyses, the origin of time was defined as the date of randomization for ENRICHD clinical trial participants, and as the enrollment date for nondepressed controls. Survival methods were used to examine the primary endpoint, and were carried out in two steps. First, univariate event times were estimated by the Kaplan-Meier method and then compared between groups with the log-rank test. Second, Cox proportional hazards regression was used to model the risk of rehospitalization associated with the presence of a depressive disorder, adjusted for the ENRICHD all-cause mortality risk score. A random frailty term for study site was included in the model to account for heterogeneity among study sites. A recent review (22) found very little consistency among 35 studies of patient characteristics that were associated with higher risk of post-AMI readmission. We therefore chose a priori to control for the ENRICHD risk score, which is a weighted composite index of medical characteristics (see Table 1) that has been shown to predict death or recurrent nonfatal MI in patients with AMI (23). It is composed of 11 variables that are likely to increase the risk of rehospitalization, including age, medical comorbidities, and markers of heart disease severity. At least one of the 11 constituent variables of the risk score was missing in approximately 40% of cases, although only 3.6% of the sample had more than 2 missing components. Multiple imputation was used to reduce the risk of bias in each statistical model that controlled for the risk score. The imputer’s model comprised 41 variables. We used SAS Proc MI to create 50 imputed datasets. Markovchain Monte Carlo (MCMC) methods were used to impute plausible values. We specified 1000 burn-in iterations and 100 run-in iterations, and used graphical methods (e.g., time plots of LVEF) to assess the stability of the process. Parameter estimates reported in the manuscript are based on the imputed data.
Table 1.
Demographic and medical characteristics by depression group (N=766)*
| Characteristic | No Depression (n=408) |
Minor Depression (n=195) |
Major Depression (n=163) |
P-value |
|---|---|---|---|---|
| Demographics | ||||
| Gender (% Female) | 131 (32.1) | 89 (45.6) | 84 (51.5) | <.001 |
| Caucasian | 322 (78.9) | 144 (73.9) | 114 (70.0) | .06 |
| Married | 312 (78.0) | 117 (62.2) | 86 (54.4) | <.001 |
| Education (> 12 years) | 304 (77.0) | 130 (69.5) | 108 (68.8) | .06 |
| Medical | ||||
| Heart Rate at Baseline (bpm) | 71.2 ± 12.4 | 73.0 ± 13.6 | 75.4 ± 12.6 | .002 |
| Systolic blood pressure (mmHg) | 122.2 ± 18.1 | 124.6 ± 20.9 | 121.7 ± 18.6 | .27 |
| Body Mass Index (kg/m2) | 28.4 ± 4.8 | 29.4 ± 5.9 | 29.5 ± 6.3 | .04 |
| Cigarette smoker (current) | 104 (26.1) | 69 (35.8) | 75 (46.6) | <.001 |
| Total Cholesterol (mg/dl) | 184.3 ± 47.3 | 199.1 ± 45.7 | 192.1 ± 45.7 | .007 |
| Time from MI to Baseline (days) | 17.1 ± 6.5 | 7.9 ± 6.1 | 8.4 ± 7.0 | <.001 |
| Post MI PTCA | 270 (67.3) | 107 (56.0) | 94 (58.4) | .01 |
| Thrombolytic therapy | 135 (33.6) | 59 (31.1) | 40 (25.0) | .14 |
| < 24 hr admit from index MI | 309 (76.5) | 153 (79.3) | 131 (81.9) | .35 |
| History hypercholesterdemia | 195 (49.1) | 123 (66.5) | 96 (61.2) | <.001 |
| Heart disease in 1st degree relatives | 268 (67.2) | 119 (64.0) | 110 (71.0) | .39 |
| History PVD | 22 (5.6) | 19 (10.4) | 33 (20.9) | <.001 |
| History CABG | 42 (10.4) | 21 (11.2) | 19 (12.0) | .87 |
| History PTCA | 41 (10.3) | 32 (17.2) | 30 (18.9) | .009 |
| History of Hypertension | 211 (52.4) | 114 (59.7) | 97 (61.0) | .09 |
| Charlson Comorbidity Index | 1.6 ± 1.8 | 2.1 ± 2.0 | 2.5 ± 2.2 | <.001 |
| ENRICHD All-Cause Mortality Risk Score1 | ||||
| Age (years) (766) | 61.1 ± 10.6 | 58.3 ± 12.3 | 55.3 ± 12.5 | <.001 |
| Diabetes mellitus (761) | 91 (22.3) | 56 (29.0) | 60 (37.5) | .001 |
| LVEF (<40%) (581) | 82 (23.0) | 41 (23.3) | 37 (24.5) | .93 |
| Killip class III-IV (725) | 17 (4.4) | 6 (3.3) | 15 (9.7) | .02 |
| Creatinine (≥ 1.3 mg/dl) (729) | 87 (22.3) | 26 (14.1) | 29 (19.0) | .07 |
| Post MI CABG (752) | 52 (13.0) | 32 (16.7) | 19 (11.8) | .36 |
| History CHF (690) | 16 (4.4) | 20 (11.4) | 32 (20.9) | <.001 |
| Previous AMI (743) | 81 (20.3) | 43 (23.0) | 33 (21.2) | .75 |
| History Stroke/TIA (741) | 23 (5.8) | 22 (11.8) | 17 (10.9) | .02 |
| Total Weighted Score (459) | 3.68 ± .88 | 3.65 ± 1.03 | 3.68 ± 1.10 | .96 |
| Medications | ||||
| Beta blocker | 332 (85.4) | 151 (79.5) | 124 (78.0) | .06 |
| ACE inhibitor | 197 (50.0) | 85 (44.7) | 77 (48.4) | .49 |
| Aspirin | 355 (90.1) | 175 (93.1) | 133 (84.7) | .03 |
| Depression | ||||
| Baseline BDI Depression Score | 3.9 ± 2.9 | 14.3 ± 5.4 | 21.4 ± 8.2 | <.001 |
| Probable # of Prior Major Depressive Episodes | .3 ± .9 | 3.0 ± 6.4 | 2.3 ± 3.6 | <.001 |
| History of Depression | 56 (16.1) | 186 (96.4) | 124 (76.5) | <.001 |
| History of Antidepressants | 7 (1.8) | 29 (15.3) | 22 (13.8) | <.001 |
| Family History of Depression | 47 (14.9) | 79 (44.4) | 62 (40.8) | <.001 |
Continuous variables are reported as mean ± SD; categorical variables represent number of patients (%).
Number in the last parenthesis represents the number of patients with observed data for that particular risk score element.
We fitted logistic regression models to compare the estimated area under the ROC curve of BDI total scores in relation to that of the DISH interview-based diagnosis (major or minor depression versus no depression) as predictors of rehospitalization. A covariate-adjusted c-statistic (c) was computed for each predictor. We used a BDI cutoff score of 10, which is the convention for clinically significant depressive symptoms, to compute c for the BDI. However, we also examined c at other cutoff scores.
To examine the effect of depression on secondary outcomes, we fitted Poisson regression models to the cumulative number of rehospitalizations and cumulative number of ED visits during the follow-up period. The cumulative length of hospital stay was extremely positively skewed. We therefore transformed this variable into a 3-level ordinal response (0 days, 1–5 days, 6 or more days), and fit it to a proportional odds model of the probability of response in the higher categories, i.e., longer cumulative LOS. All analyses of secondary outcome variables included the risk score and a variable that represented the length of known contact with the patient during follow up (measured in days).
We assessed each statistical model for any serious model violations. For the Cox models, we verified that the continuous predictor variables were linearly related to the log hazard, and that the hazard ratio was constant (proportional) over time. We assessed the latter by examining Schoenfeld residuals and adding an interaction (with time) term to the model. We also tested assumptions about outliers, influential observations, and the model’s goodness of fit. We assessed key assumptions for both the proportional odds and Poisson models, including the equality of slopes (proportional odds) and use of deviance residuals to determine whether the variance was proportional to the mean response, respectively. AIC and BIC statistics were used to assess overall model fit.
All statistical tests were two-sided and p-values were adjusted for multiple comparisons via a step-down Bonferroni procedure (24) to maintain a Type I error rate of 0.05 per comparison. All analyses were conducted using SAS 9.2 statistical software.
Results
A total of 766 patients were enrolled in the study, including 408 patients who were not depressed (ND), 195 with minor depression (md), and 163 with major depression (MD). As shown in Table 1, the groups differed on several medical and demographic characteristics. They also differed on the proportion of patients who had a subsequent cardiac hospitalization during the follow-up (ND: 81/408 [19.9%], md: 67/195 [34.4%], MD: 70/163 [42.9%]; P<.001), as well as on the number [percentage] of deaths (n=47) during follow up (ND: 14 [3.4%]; md: 17 [8.7%]; MD: 16 [9.8%]; P=.004). The ND (25.7 [8.5]), md (24.7 [8.3]), and MD (24.3 [8.3]) participants did not differ (P=.13) on mean length of follow up (in months).
Table 2 displays demographic and baseline medical characteristics by rehospitalization status. Patients who were female, not Caucasian, and who had 12 years of education or less were more likely to be rehospitalized. Additionally, those who were rehospitalized were more likely to have a history of peripheral vascular disease, coronary revascularization, and hypertension, and had higher systolic blood pressure, body mass index, and a higher ENRICHD all-cause mortality risk score.
Table 2.
Medical and demographic characteristics by verified cardiac rehospitalization (N=766)*
| Characteristic | Cardiac Rehospitalization | ||
|---|---|---|---|
| P-value | |||
| No (n=548) |
Yes (n=218) |
||
| Demographics | |||
| Gender (% Female) | 201 (36.7) | 103 (47.3) | .007 |
| Caucasian | 427 (77.9) | 153 (70.2) | .02 |
| Married | 377 (70.6) | 138 (65.1) | .14 |
| Education (> 12 years) | 399 (75.6) | 143 (67.8) | .03 |
| Medical | |||
| Heart Rate at Baseline (bpm) | 72.2 ± 12.7 | 73.6 ± 13.1 | .17 |
| Systolic blood pressure (mmHg) | 121.7 ± 19.1 | 125.2 ± 18.3 | .02 |
| Body Mass Index (kg/m2) | 28.6 ± 5.3 | 29.7 ± 5.8 | .02 |
| Cigarette smoker (current) | 173 (32.1) | 75 (35.2) | .41 |
| Total Cholesterol (mg/dl) | 190.0 ± 44.4 | 190.0 ± 52.9 | .99 |
| Time from MI to Baseline (days) | 13.5 ± 7.7 | 11.4 ± 8.2 | .001 |
| Post MI PTCA | 335 (62.0) | 136 (63.9) | .64 |
| Thrombolytic therapy | 173 (32.2) | 61 (28.5) | .33 |
| < 24 hr admit from index MI | 418 (77.3) | 175 (81.0) | .26 |
| History hypercholesterdemia | 296 (55.9) | 118 (56.5) | .88 |
| Heart disease in 1st degree relatives | 366 (69.1) | 131 (62.4) | .08 |
| History PVD | 42 (7.9) | 32 (15.6) | .002 |
| History CABG | 45 (8.4) | 37 (17.5) | <.001 |
| History PTCA | 60 (11.2) | 43 (20.5) | .001 |
| History of Hypertension | 288 (53.2) | 134 (63.2) | .01 |
| Charlson Comorbidity Index | 1.7 ± 1.7 | 2.6 ± 2.3 | <.001 |
| ENRICHD All-Cause Mortality Risk Score1 | |||
| Age (years) (766) | 59.4 ± 11.6 | 58.6 ± 11.9 | .43 |
| Diabetes mellitus (761) | 130 (23.8) | 77 (36.0) | <.001 |
| LVEF (<40%) (581) | 103 (21.2) | 57 (28.8) | .03 |
| Killip class III-IV (725) | 22 (4.2) | 16 (7.8) | .05 |
| Creatinine (≥ 1.3 mg/dl) (729) | 100 (19.1) | 42 (20.5) | .67 |
| Post MI CABG (752) | 87 (16.2) | 16 (7.5) | .002 |
| History CHF (690) | 32 (6.4) | 36 (18.7) | <.001 |
| Previous AMI (743) | 93 (17.5) | 64 (30.5) | <.001 |
| History Stroke/TIA (741) | 37 (6.9) | 25 (12.1) | .02 |
| Total Weighted Score (459) | 3.61 ± .90 | 3.85 ± 1.14 | .02 |
| Medications | |||
| Beta blocker | 441 (84.2) | 166 (77.6) | .03 |
| ACE inhibitor | 244 (46.2) | 115 (53.5) | .07 |
| Aspirin | 474 (90.5) | 189 (88.7) | .48 |
| Depression | |||
| Depression diagnosis | <.001 | ||
| No depression | 327 (59.7) | 81 (37.2) | |
| Minor depression | 128 (23.4) | 67 (30.7) | |
| Major depression | 93 (17.0) | 70 (32.1) | |
| Baseline BDI Depression Score | 9.1 ± 8.1 | 13.3 ± 9.9 | <.001 |
| Probable # of Prior Major Depressive Episodes | |||
| 1.5 ± 4.2 | 1.8 ± 3.8 | .39 | |
| History of Depression | 233 (46.7) | 133 (65.5) | <.001 |
| History of Antidepressants | 39 (7.4) | 19 (8.9) | .51 |
| Family History of Depression | 114 (24.8) | 74 (39.8) | <.001 |
Continuous variables are reported as mean ± SD; categorical variables represent number of patients (%).
Number in the last parenthesis represents the number of patients with observed data for that particular risk score element.
Figure 1 represents Kaplan-Meier estimates for time to first rehospitalization by depression status. The estimated time at which 25% of patients had at least one cardiac rehospitalization was 32.3 months in the ND group, 11.5 months in the md group, and 5.9 months in the MD group. Results of the unadjusted and adjusted Cox regression analyses on time to first rehospitalization are shown in Table 3. Compared to patients without depression, patients with major depression (unadjusted hazard ratio [HR], 2.69; 95% CI, 1.95 to 3.70; P<.001) or minor depression (unadjusted HR, 1.99; 95% CI, 1.44 to 2.76; P<.001) were at greater risk for cardiac rehospitalization. There was no significant difference in the risk of rehospitalization between patients with major depression and those with minor depression (HR, 1.35; 95% CI, 0.96 to1.88; P=.08). After controlling for the ENRICHD all-cause mortality risk score and a random frailty term for study site, the results were essentially unchanged (major versus nondepressed: adjusted HR, 2.54; 95% CI, 1.84 to 3.53; P<.001; minor versus nondepressed: adjusted HR, 2.22; 95% CI, 1.59 to 3.08; P<.001.) Additionally, we conducted a post hoc analysis controlling for gender, which differed significantly between patients who were rehospitalized and those who were not (see Table 2). Although the main effect for gender was marginally associated with time to first rehospitalization (adjusted HR, 1.29; 95% CI, .99 to 1.69; P=.06), the effects of depression remained relatively unchanged.
Figure 1.
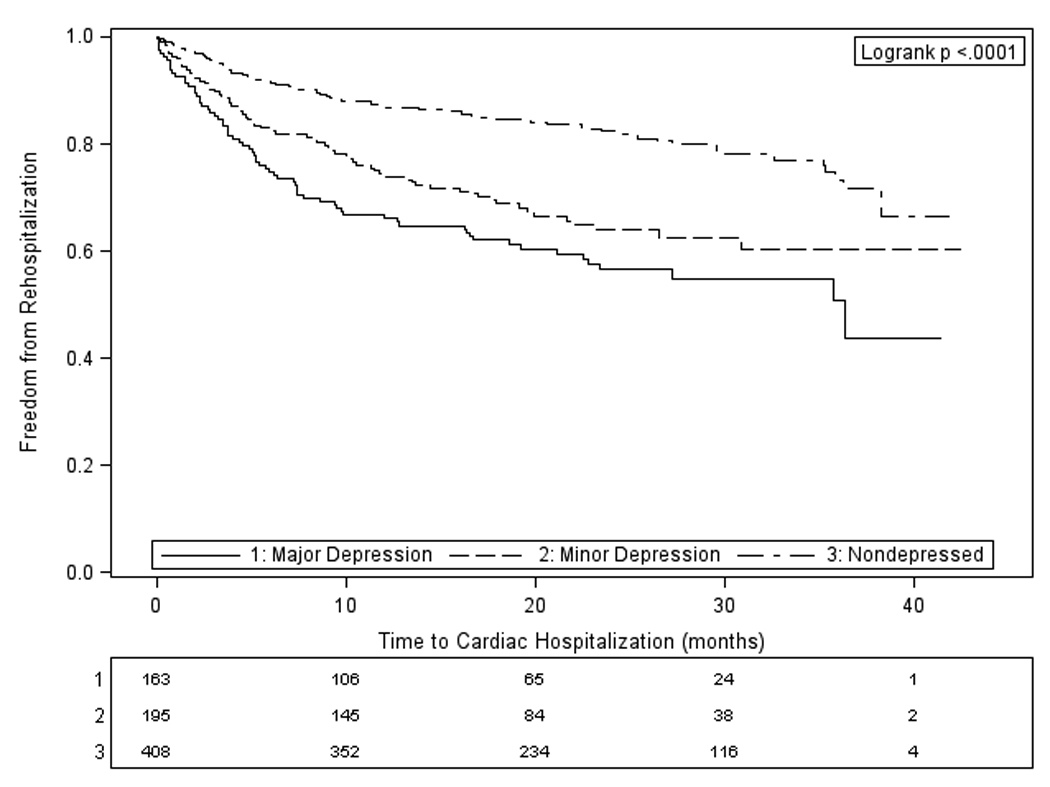
“Kaplan-Meier Plot” “With Number of Subjects at Risk”
The embedded table represents the number of patients in each depression group who have neither experienced a cardiac rehospitalization nor been censored. Reasons for censoring were death or loss to follow-up.
Table 3.
Effect of depression on time to first cardiac hospitalization
| Analysis Model Parameter |
Hazard Ratio (95% CI) |
P-value |
|---|---|---|
| 1Unadjusted | ||
| Major vs. No Depression | 2.69 (1.95, 3.70) |
<.001 |
| Minor vs. No Depression | 1.99 (1.44, 2.76) |
<.001 |
| Major vs. Minor Depression | 1.35 (0.96, 1.88) |
.08 |
| 2Adjusted | ||
| Major vs. No Depression | 2.54 (1.84, 3.53) |
<.001 |
| Minor vs. No Depression | 2.22 (1.59, 3.08) |
<.001 |
| Major vs. Minor Depression | 1.15 (.81, 1.62) |
.43 |
| ENRICHD All-Cause Mortality Risk Score | 1.27 (1.11, 1.45) |
<.001 |
Kaplan-Meier curves are provided in Figure 1.
The effect of depression is controlled for the imputed, ENRICHD all-cause mortality risk score and a random frailty term for study site.
We investigated whether there was any bias introduced by the high degree (40%) of missing data in at least one of the 11 constituent variables of the risk score covariate. We found that only one component of the risk score was missing in 30.7% of the sample; 2 components were missing in 6.1%; and ≥3 components were missing in 3.3%. The distributions of numbers of missing components were also quite similar across the ND, md, and MD groups. For example, only one component was missing in 32.4%, 30.3%, and 27% of the groups, and only 2 components were missing in 7.1%, 4.1%, and 6.1% of the groups, respectively. The predominant missing component was LVEF, which was missing in 24.2% of cases in the overall sample (25% ND, 23% md, and 23% MD). The rates of CV rehospitalizations of patients with LVEF data present vs. missing were 28.4% and 28.7%, respectively (P=.95). Thus, there are not any large imbalances in missingness between the depression groups or between the patients who were or were not rehospitalized. Tables 1 and 2 show the observed (before imputation) sample size for each component of the risk score.
The ROC curves are shown in Figure 2. The c-statistic for a BDI cutoff score of 10 (0.64; 95% CI, 0.60–0.68) and for DISH interview-based depression diagnosis (0.65; 95% CI, 0.61–0.69) were not significantly different (difference in c, 0.01; 95% CI, −0.00–0.03; P=.08). Other ROC parameters were estimated, comparing a BDI score of 10 or greater with DISH depression diagnosis. Sensitivity was 96.1%, specificity was 95.9%, positive predictive value was 95.4%, and negative predictive value was 96.5%. We also found excellent agreement (κ̂ = 0.92) between the two depression diagnostic tools. Finally, as an exploratory analysis, we examined the c-statistics for BDI cutoff scores of 5–20, to determine whether the conventionally used score of 10 provided the highest overall accuracy of prediction. The highest value of c was associated with a BDI cutoff of 15 (0.67, 95% CI, 0.62–0.71), suggesting a slight advantage in discrimination ability with a higher cutoff score.
Figure 2.
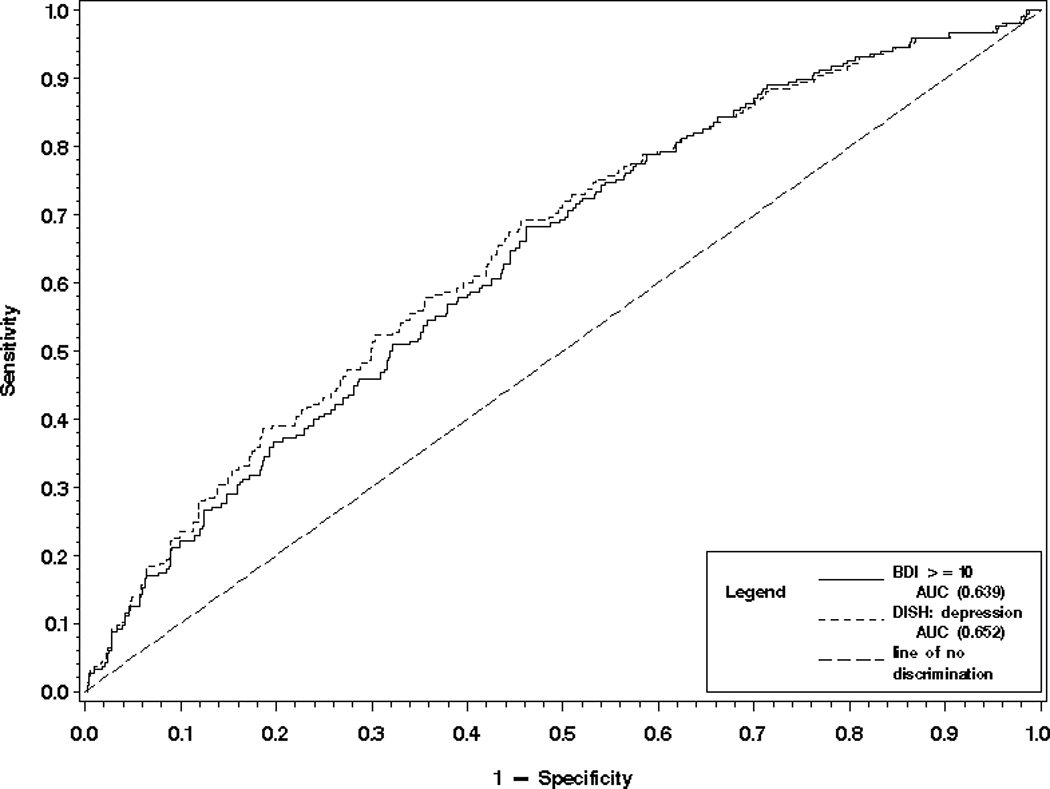
“ROC Curves Comparing the Overall Accuracy of BDI Score with DSM-IV Diagnosis as Predictors of Rehospitalization”
Keywords: AUC = area under curve = c-statistic
Poisson regression models revealed significant differences between the MD and ND groups, as well as between the md and ND groups in the cumulative number of all-cause rehospitalizations (both P<.001) and number of ED visits during the follow up (MD vs. ND: P<.001; md vs. ND: P=.003). Additionally, the MD and md groups differed significantly on the cumulative number of all-cause rehospitalizations (P=.04). Compared to the ND group, both MD (P<.001) and md (P<.001) patients had greater odds of having a longer cumulative length of hospital stay.
As a sensitivity analysis, we redefined the primary outcome as a composite endpoint of time to first rehospitalization or death, in order to account for any biases due to deaths which were censored in our primary analysis. The results were very similar to the primary analysis, with depression remaining a significant predictor of the composite endpoint after adjusting for mortality risk.
To determine whether the severity of clinical depression was related to the primary outcome, we examined the effect of self-reported depression on time to first rehospitalization among patients with major or minor depression (n=358). BDI score was significantly associated with time to rehospitalization (unadjusted HR = 1.02; 95% CI, 1.0 to 1.04; P=.02). Every one-point increase on the BDI was associated with a 2% increase in the risk of rehospitalization in the depressed subgroup.
Discussion
In this ENRICHD ancillary study, we found that patients who met the DSM-IV criteria for major or minor depression after an acute MI were rehospitalized significantly sooner for cardiac reasons than patients who were not depressed. Depressed participants also had higher total numbers of all-cause hospitalizations and ED visits during the 42 months following initial hospitalization for MI, and they spent significantly more total days in the hospital. These results remained significant after adjustment for well-established mortality risk factors. To our knowledge, this is the first study to use diagnostic interviews to examine the association between depressive disorders and the risk of rehospitalization after AMI. The results are consistent with those of previous investigations that used symptom questionnaires to assess depression (10–14). It is possible that symptom questionnaires may predict rehospitalization because of their modest specificity for clinical depression; it could be that among patients who go on to be rehospitalized, depression questionnaire scores are inflated by the presence of more severe heart disease. The present findings confirm that clinical depression actually does predict readmissions.
However, we also found that the diagnostic interview does not significantly improve the overall accuracy of prediction of rehospitalization, when compared to the BDI questionnaire. Although clinical diagnostic interviews are the gold standard for determining depression diagnostic status, they are more burdensome to administer than are self-report questionnaires due to their length and to the extensive training required of interviewers. Our findings suggest that it is not necessary to interview patients to determine whether they are at increased risk of rehospitalization due to depression, and that this determination can be made on the basis of a brief questionnaire such as the BDI. We believe this finding has important clinical implications, as these questionnaires are cost-effective and are easy to administer and interpret. Our results also show that the risk of rehospitalization increases along with the severity of depression, suggesting that depression inventory scores should be used in this context as continuous measures, and not artificially dichotomized at a cutoff score.
The latest report from the American Heart Association projects that by 2030, over 40% of adults in the U.S. will have some form of cardiovascular disease, and that the direct medical costs of cardiovascular disease will triple (25), assuming no significant changes in cardiovascular treatment and prevention. Reducing hospital costs among CHD patients is therefore a public health priority. However, a recent review of 35 studies (22) found no reliable predictors of post-AMI rehospitalization. A substantial body of research now shows the negative prognostic impact of depression in patients with AMI, and these adverse associations contribute to higher health care costs among depressed patients (10). In one study, the average daily cost of an AMI hospitalization in the United States was estimated to be $1,688 per day (4). In the present study, we found that nondepressed patients spent an average of 4.1 days in the hospital during the follow-up, while patients with major depression were in the hospital for an average of 13.4 days. This translates to an additional average cost of $15,698 for depressed patients. The current study and a number of others have found depression to be a significant predictor for hospital readmission. The fact that this result is consistent across different samples and assessment methods suggests that depression has a robust effect on the risk of rehospitalization after AMI. Nevertheless, depression remains underdiagnosed and is often untreated in this population (26).
Depression is a modifiable risk factor which contributes significantly to hospital costs. However, we do not yet know if treating depression would decrease rehospitalization rates, but some initial evidence suggests that it may. Cosette et al. (27) found that MI patients who experienced a decrease in distress following a brief intervention were less likely to be rehospitalized for cardiac and noncardiac causes, when compared to patients whose distress did not improve. At the least, treating physicians should be aware of the risk for rehospitalization associated with depression, and ensure that depressed patients receive appropriate treatment or a referral for depression care.
The mechanisms underlying depression’s effect on the likelihood of hospital readmission are unknown. Depression increases the risk of cardiac morbidity and mortality in patients with established CHD (28, 29), and this may be the single most important reason for its association with rehospitalization after AMI. Differences between depressed and nondepressed patients in help-seeking behaviors (30), health behavior and compliance (31), and perception of chest pain (32) may also play a role.
A limitation of this study is that our data were collected over ten years ago. It is possible that rehospitalization risks may have changed, such that we would not find the same result in a more recent study. However, our findings are consistent with those of similar investigations that have used more contemporary samples (13, 14). Additionally, we may not have controlled for all factors that could potentially affect hospitalization. The current literature is not consistent regarding patient characteristics associated with readmission, and more work needs to be done to empirically determine the most reliable predictors of readmission. Missing risk score data pose another limitation. The risk score’s constituent variables were obtained from chart reviews, not from data collected specifically for the study. Virtually all of the missing data were missing because they were simply not available in the clinical record. However, we did not find any evidence for systematic bias in our findings due to missing risk score data.
In summary, depression increases the risk of rehospitalization after AMI, resulting in a greater economic burden for patients as well as the health care system. This result is consistent whether depression is assessed by symptom inventory or by diagnostic interview. Given the high frequency and cost of hospital readmission after AMI, empirical development of risk prediction models should be a priority, and self-report depression measures should be included in them. Future work should also examine whether successful treatment of depression is associated with decreased hospitalizations and hospital stays, and therefore decreased health care costs.
What is Known
Depression is associated with adverse outcomes in patients with coronary artery disease
Whether DSM-IV depressive disorders (minor or major depression) predict rehospitalization after acute myocardial infarction (AMI) is unknown.
What this Article Adds
Minor and major depression increase the risk of rehospitalization and emergency department visits after AMI.
This result is consistent whether depression is assessed by symptom questionnaire or by a diagnostic interview
Multivariable models that predict the risk of rehospitalization after AMI should include depression.
Acknowledgments
Funding Sources: This research was supported in part by Grant No. 2 RO-1HL58946 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Maryland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures: None
References
- 1.Xu J, Kochanek KD, Murphy S, Tejada-Vera B. Deaths: Final Data for 2007. National Vital Statistics Reports. 2010;58 [PubMed] [Google Scholar]
- 2.Berenson K, Ogbonnaya A, Casciano R, Makenbaeva D, Mozaffari E, Lamerato L, Corbelli J. Economic consequences of ACS-related rehospitalizations in the US. Current Medical Research and Opinion. 2010;26:329–336. doi: 10.1185/03007990903479331. [DOI] [PubMed] [Google Scholar]
- 3.Menzin J, Wygant G, Hauch O, Jackel J, Friedman M. One-year costs of ischemic heart disease among patients with acute coronary syndromes: findings from a multi-employer claims database. Current Medical Research and Opinion. 2008;24:461–468. doi: 10.1185/030079908x261096. [DOI] [PubMed] [Google Scholar]
- 4.Johnston SS, Curkendall S, Makenbaeva D, Mozaffari E, Goetzel R, Burton W, Maclean R. The Direct and Indirect Cost Burden of Acute Coronary Syndrome. Journal of Occupational and Environmental Medicine. 2011;53:2–7. doi: 10.1097/JOM.0b013e31820290f4. [DOI] [PubMed] [Google Scholar]
- 5.Kauf TL, Velazquez EJ, Crosslin DR, Weaver WD, Diaz R, Granger CB, McMurray JJV, Rouleau JL, Aylward PE, White HD, Califf RM, Schulman KA. The cost of acute myocardial infarction in the new millennium: Evidence from a multinational registry. American Heart Journal. 2006;151:206–212. doi: 10.1016/j.ahj.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Camethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpem SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J. Heart Disease and Stroke Statistics-2011 Update A Report From the American Heart Association. Circulation. 2011;123:E18–E209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosomatic Medicine. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 8.Carney RM, Freedland KE. Depression in Patients with Coronary Heart Disease. American Journal of Medicine. 2008;121:20–27. doi: 10.1016/j.amjmed.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 9.van Melle JP, de Jonge P, Spijkerman TA, Tijssen JGP, Ormel J, van Veldhuisen DJ, van den Brink RHS, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis. Psychosomatic Medicine. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- 10.Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, Bourassa MG. Depression and health-care costs during the first year following myocardial infarction. Journal of Psychosomatic Research. 2000;48:471–478. doi: 10.1016/s0022-3999(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 11.Kurdyak PA, Gnam WH, Goering P, Chong A, Alter DA. The relationship between depressive symptoms, health service consumption, and prognosis after acute myocardial infarction: a prospective cohort study. Bmc Health Services Research. 2008;8:200. doi: 10.1186/1472-6963-8-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lauzon C, Beck CA, Huynh T, Dion D, Racine N, Carignan S, Diodati JG, Charbonneau F, Dupuis R, Pilote L. Depression and prognosis following hospital admission because of acute myocardial infarction. Canadian Medical Association Journal. 2003;168:547–552. [PMC free article] [PubMed] [Google Scholar]
- 13.Parashar S, Rumsfeld JS, Reid KJ, Buchanan D, Dawood N, Khizer S, Lichtman J, Vaccarino V. Impact of Depression on Sex Differences in Outcome After Myocardial Infarction. Circulation-Cardiovascular Quality and Outcomes. 2009;2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smolderen KG, Spertus JA, Reid KJ, Buchanan DM, Krumholz HM, Denollet J, Vaccarino V, Chan PS. The Association of Cognitive and Somatic Depressive Symptoms With Depression Recognition and Outcomes After Myocardial Infarction. Circulation-Cardiovascular Quality and Outcomes. 2009;2:328–337. doi: 10.1161/CIRCOUTCOMES.109.868588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 16.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 17.Carney RM, Rich MW, Tevelde A, Saini J, Clark K, Jaffe AS. Major depressive disorder in coronary artery disease. The American Journal of Cardiology. 1987;60:1273–1275. doi: 10.1016/0002-9149(87)90607-2. [DOI] [PubMed] [Google Scholar]
- 18.Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 19.Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, Czajkowski SM, DeBusk R, Hosking J, Jaffe A, Kaufmann PG, Mitchell P, Norman J, Powell LH, Raczynski JM, Schneiderman N. Effects of treating depression and low-perceived social support on clinical events after myocardial infarction - The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 20.Carney RM, Blumenthal JA, Stein PK, Watkins L, Catellier D, Berkman LF, Czajkowski SM, O'Connor C, Stone PH, Freedland KE. Depression, heart rate variability, and acute myocardial infarction. Circulation. 2001;104:2024–2028. doi: 10.1161/hc4201.097834. [DOI] [PubMed] [Google Scholar]
- 21.Freedland KE. Developoment of a structured interview for diagnosing depression in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study. Int J Behav Med. 2000;7:240. [Google Scholar]
- 22.Desai MM, Stauffer BD, Feringa HHH, Schreiner GC. Statistical Models and Patient Predictors of Readmission for Acute Myocardial Infarction A Systematic Review. Circulation-Cardiovascular Quality and Outcomes. 2009;2:500–507. doi: 10.1161/CIRCOUTCOMES.108.832949. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe AS, Krumholz HM, Catellier DJ, Freedland KE, Bittner V, Blumenthal JA, Calvin JE, Norman J, Sequeira R, O'Connor C, Rich MW, Sheps D, Wu C. Prediction of medical morbidity and mortality after acute myocardial infarction in patients at increased psychosocial risk in the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) study. American Heart Journal. 2006;152:126–135. doi: 10.1016/j.ahj.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Holm S. A Simple Sequentially Rejective Bonferroni Test Procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- 25.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PWF, Woo YJ on behalf of the American Heart Association Advocacy Coordinating Committee, Stroke C, Council on Cardiovascular Radiology and Intervention, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiopulmonary, Critical C, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on the Kidney in Cardiovascular Disease, Council on Cardiovascular Surgery and Anesthesia aICoQoCaOR. Forecasting the Future of Cardiovascular Disease in the United States: A Policy Statement From the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 26.Amin AA, Jones AMH, Nugent K, Rumsfeld JS, Spertus JA. The prevalence of unrecognized depression in patients with acute coronary syndrome. American Heart Journal. 2006;152:928–934. doi: 10.1016/j.ahj.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Cossette S, Frasure-Smith N, Lesperance F. Clinical implications of a reduction in psychological distress on cardiac prognosis in patients participating in a psychosocial intervention program. Psychosomatic Medicine. 2001;63:257–266. doi: 10.1097/00006842-200103000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Joynt KE, Whellan DJ, O'Connor CM. Depression and cardiovascular disease: Mechanisms of interaction. Biological Psychiatry. 2003;54:248–261. doi: 10.1016/s0006-3223(03)00568-7. [DOI] [PubMed] [Google Scholar]
- 29.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: Evidence, mechanisms, and treatment. Psychosomatic Medicine. 2004;66:305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- 30.Katon W, Berg AO, Robins AJ, Risse S. Depression - Medical Utilization and Somatization. Western Journal of Medicine. 1986;144:564–568. [PMC free article] [PubMed] [Google Scholar]
- 31.Carney RM, Freedland KE, Rich MW, Jaffe AS. Depression As A Risk Factor for Cardiac Events in Established Coronary Heart-Disease - A Review of Possible Mechanisms. Annals of Behavioral Medicine. 1995;17:142–149. doi: 10.1007/BF02895063. [DOI] [PubMed] [Google Scholar]
- 32.Ladwig KH, Roll G, Breithardt G, Borggrefe M. Extracardiac contributions to chest pain perception in patients 6 months after acute myocardial infarction. American Heart Journal. 1999;137:528–534. doi: 10.1016/s0002-8703(99)70502-8. [DOI] [PubMed] [Google Scholar]


