Abstract
MELD-based allocation of deceased donor livers allows exceptions for patients whose score may not reflect their true mortality risk. We hypothesized that OPOs may differ in exception practices, use of exceptions may be increasing over time, and exception patients may be advantaged relative to other patients. We analyzed longitudinal MELD score, exception, and outcome in 88,981 adult liver candidates as reported to UNOS from2002–2010.Proportion of patients receiving an HCC exception was 0–21.4% at the OPO-level and 11.9–18.8% at the region-level; proportion receiving an exception for other conditions was 0.0%–13.1% (OPO-level) and 3.7%–9.5%% (region-level).HCC exceptions rose over time (10.5% in 2002 vs. 15.5% in 2008, HR=1.09 per year, p<0.001) as did other exceptions (7.0% in 2002 vs. 13.5% in 2008, HR=1.11, p<0.001).In the most recent era of HCC point assignment (since April 2005), both HCC and other exceptions were associated with decreased risk of waitlist mortality compared to non-exception patients with equivalent listing priority (multinomial logistic regression OR=0.47 for HCC, OR=0.43 for other, p<0.001) and increased odds of transplant (OR=1.65 for HCC, OR=1.33 for other, p<0.001).Policy advantages patients with MELD exceptions;differing rates of exceptions by OPO may create, or reflect, geographic inequity.
Keywords: liver transplantation, organ allocation, MELD score
INTRODUCTION
Since February 2002, the Model of End-stage Liver Disease (MELD) score has been used to prioritize allocation of deceased donor livers. Although MELD was adopted to estimate the short-term (90-day) risk of waitlist mortality(1), it is believed to underestimate such risk for certain patients with non-normative conditions(2).Moreover, some diseases have low risk of short-term mortality, but require transplant before progression to the point of irreversible complications(3). As such, additional MELD points can be granted, and these patients ultimately receive priority based on the exception MELD rather than the calculated MELD.OPTN policies originally allowed exception points for certain Recognized Exceptional Diagnoses (REDs): hepatocellular carcinoma(HCC), hepatopulmonary syndrome(HPS), familial amyloidosis, and primary oxaluria. In June 2009, familial amyloidosis and primary oxaluria were removed from the list, and cholangiocarcinoma, cystic fibrosis, familial amyloid neuropathy, primary hyperoxaluria, and portopulmonary syndrome were added. Exceptions can also be awarded on a case-by-case basis for other, rarer conditions (non-RED exceptions) (4). Historically, the number of exception points allowed for diagnoses other than HCC has not been clearly defined (5, 6).
The assignment of MELD exceptions mitigates the risk of disadvantaging patients whose risk may not be fully captured by their calculated MELD, but creates the risk of assigning a higher priority than that warranted by the underlying health, therefore disadvantaging other patients. From 2004 to 2008, the proportion of patients on the waiting list with a MELD exception increased by 80%(7). The exception MELD score for patients with HCC, the most common exception diagnosis, was lowered in 2003 and again in 2005 in response to evidence that HCC patients were inappropriately favored (8, 9).
Recently, Washburn et al suggested that HCC patients are still advantaged under the current system based on differential dropout rates between a group of HCC patients and a group of non-exception patients (10) in the first year after listing. However, an "apples-to-apples" comparison, i.e. a head-to-head comparison of HCC patients whose waitlist priority is determined through exception points to patients whose priority is determined through equivalent lab scores, was not made. Furthermore, exceptions and MELD scores were treated as one-time events; HCC patients were analyzed as a single group, regardless of exception points (and regardless of when the exception was granted), and non-exception patients were analyzed based only on their initial MELD score. In reality, however, MELD scores change over time, most patients spend some time prioritized by calculated MELD and some time prioritized by exception MELD, and exception points change over time. Dichotomizing patients as "HCC exception" or "non-exception" creates time-dependent misclassification bias: the one-time (as opposed to a longitudinal) analysis limits any ability to account for differential patterns of MELD progression by disease or patient subgroups. Also, dropout rates of past the first year were not analyzed. Finally, patients with exceptions for conditions other than HCC were excluded, prohibiting any inference about the role of exceptions in other diseases.
The purpose of this study was to expand on the methodology and study population of these recent observations, thereby allowing more robust inferences about HCC exceptions, inferences about other exception conditions, and geographic comparisons. We constructed a rigorous statistical framework in which MELD progression could be modeled (accounting for the dynamic nature of MELD and exceptions over person-time instead of one-time measurements), head-to-head comparisons could be made, and both transplant rates and dropout rates could be compared. We used this framework to address the following goals: 1) to compare outcomes (transplant and mortality)in exception patients to outcomes in non-exception patients with equivalent allocation priority; 2) to analyze changes over time in the rates at which exceptions are granted; and 3) to compare geographic rates of exception, transplantation and death.
METHODS
Study Population
We analyzed data on deceased donor liver transplant waiting list registrants from a longitudinal dataset collected prospectively by UNOS/OPTN, analyzing candidates who enrolled on or after February 28, 2002. Data were administratively censored on February 26, 2010.Registrants added to the waiting list before February 28, 2002, registrants under 18 at registration, live donor recipients, and registrants who were ever Status 1 were excluded.
Person-Time
We use the term cMELD ("calculated MELD") to refer to an individual's MELD score as calculated from laboratory values (sometimes called "laboratory score" in other literature(9)); eMELD ("exception MELD") to refer to an individual's MELD score as granted by exception; and aMELD ("allocation MELD") to refer to the MELD score used to determine priority for allocation purposes (that is, aMELD=cMELD for non-exception patients and aMELD=max(cMELD,eMELD) for exception patients; sometimes called "match score" in other literature(9)).
We classified person-time as exception person-time when eMELD>cMELD for exception patients (i.e. the person-time when the exception points were relevant).Note that, under our definition, a person could contribute non-exception person-time even after an exception was granted, if cMELD≥eMELD for any amount of time (i.e. if the calculated MELD exceeded exception points).We further partitioned exception person-time based on whether or not the exception was granted for HCC. Among patients who were granted an exception, person-time accrued prior to granting of the exception was excluded from analysis. Person-time for which the cMELD score had not been reported in the UNOS-required manner (>1 year for cMELD≤10, >3 months for cMELD 11–18, >1 month for cMELD 19–24, and >7 days for cMELD>24) was interval censored.
Outcome Ascertainment
For each person-day of analysis, we classified the patient's outcome at 90 days, one year, and three years as either: decrease in aMELD, no change in aMELD, increase in aMELD, transplanted, or died. Patients were followed until the first occurrence of transplantation, death, or end-of-study. Removal from the waiting list for medical unsuitability, refusal of transplant, or deteriorating condition was treated as death for the purposes of this analysis; such treatment is particularly important for patients with conditions such as HCC, who may be removed from the list because they no longer qualify for transplantation due to disease progression, even in cases when short-term mortality risk is low(3, 11).Patients removed from the list for other reasons (transfer to another center, improved condition, transplantation at another center, removal in error) were censored at the time of removal.
90-Day Outcomes
Separately for non-exception person-time (time that a patient was prioritized by cMELD), HCC exception person-time (time that a patient with HCC was prioritized by eMELD), and other exception person-time (time that a patient with an exception for a condition other than HCC was prioritized by eMELD), we produced histograms of the distribution of person-days of aMELD, and heat maps showing the distribution of 90-day outcomes for each aMELD score. We tested the hypothesis that the probability of death or transplantation differed by exception status using baseline category multinomial logistic regression, with person-days as the unit of analysis and a clustered sandwich estimator of the standard error to account for correlation among repeated measurements of a single registrant. That is, for each patient-day i, we modeled the probability that 90-day outcome yiwould be equal to j (either death or transplant), given covariates Xi, as
| (12) |
This allowed a competing risk-type framework where each patient could only have one of several competing outcomes. The regression analysis included only time after April 2005, when the initial number of exception points for HCC was lowered from 24 to 22. Since more than 80% of aMELD values were in the range of 22–25 for HCC-exception person-time, we restricted the comparison of HCC exception person-time and non-exception person-time to aMELD values in that range, with indicator variables for each aMELD score other than 22 (the mode and median HCC eMELD exception value). Thus, person-time with aMELD lower than 22 or higher than 25 was not used for this comparison. Similarly, for the comparison of other exception person-time to non-exception person-time, we restricted the analysis to aMELD values in the range of 15–25.
Longer-Term Outcomes
The 90-day mortality metric may be inappropriate for patients with exceptions; for example, patients with HCC might initially survive longer, but lose transplant eligibility and have higher rates of death at longer time points. To test the hypothesis that longer-term outcomes differed by exception status, we produced additional multivariate logistic regression models of outcomes at 1 and 3 years.
Also, to better understand the fate of HCC patients after removal from the list for reasons other than patient death, we studied the survival of these patients after dropout for deteriorating patient health (or medical unsuitability). Since deaths after dropout are ascertained partly externally via the Social Security master death file, and may be reported after some delay, we administratively censored HCC dropouts at July 28, 2009, six months before the end of follow up in our dataset.
Exceptions Over Time
We analyzed changes over time in granting exceptions to new patients by constructing time-to-event models, with receipt of an exception as the outcome, censoring for any removal from the waiting list prior to receipt of an exception (e.g. transplantation, death). We plotted separate curves for HCC and other exceptions, stratifying by the year a patient was added to the waiting list. We used Cox regression to assess change in exception rates over time, adjusting for UNOS region. Additionally, we modeled odds over time of a patient receiving an exception within 1 year of listing, using a multilevel model with a random effect at the region level to account for differences in rates of exception by region.
OPO-Level and Region Level Models
To compare rates of transplantation by geographic area, we calculated for each OPO the probability that a given waitlist candidate would receive a transplant within 90 days of any given date. We calculated this probability as the number of person-days that fell ≤ 90 days before a transplant, divided by the number of person-days for which we had at least 90 days of follow-up. Similarly, we calculated for each OPO the probability that a candidate would die within 90 days of any given date. We then produced box plots of these probabilities, as well as a scatter plot of the proportion of registrants from each OPO that were granted an HCC or other exception. We computed the correlation coefficient of proportions of HCC and other exceptions to determine whether centers at some OPOs were more aggressive than others in seeking exceptions in general. We performed the same analyses by region.
Statistical Analysis
All statistical tests used a two-sided α of 0.05. Confidence intervals are reported as per the method of Louis and Zeger(13) as previously reported(14–16). All analyses were performed using STATA 11.0/MP for Linux (College Station, Texas).
RESULTS
Study Population
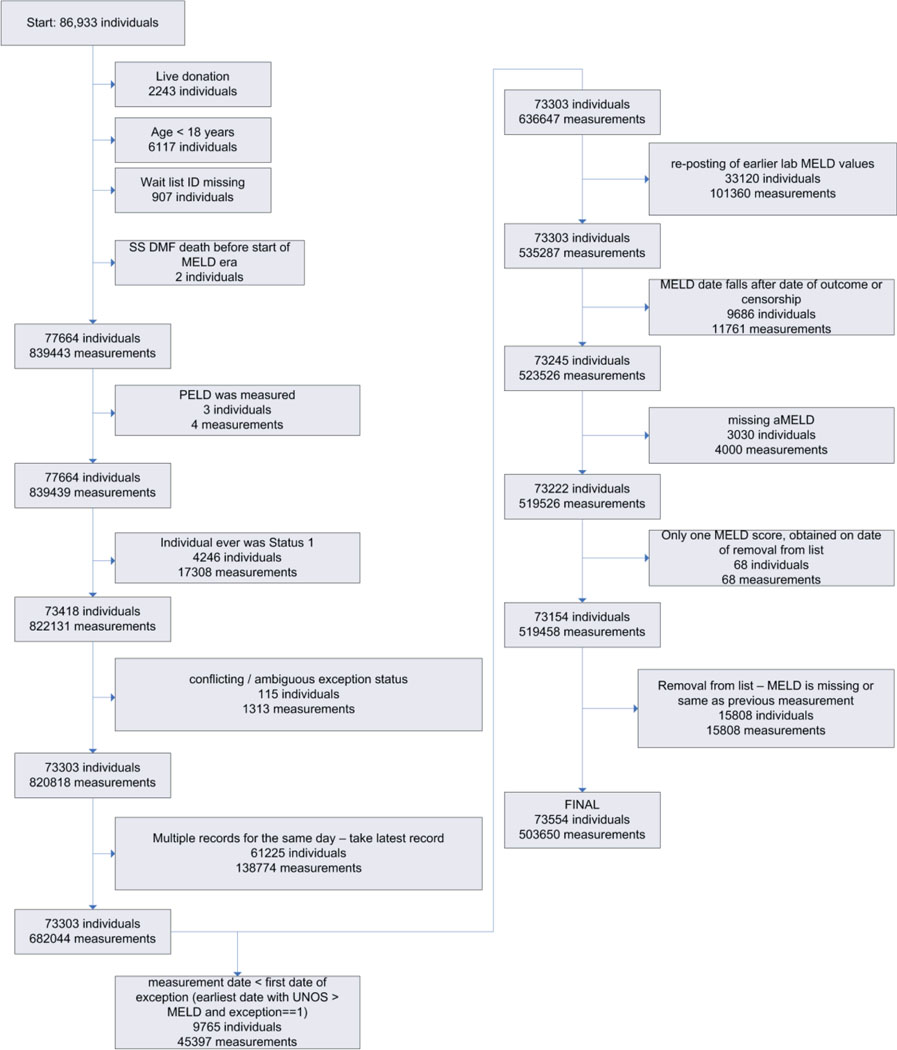
Over an 8 year period, there were 503,650 MELD measurements reported to UNOS, covering 22,337,938 person-days of 73,154 patients (Figure 1). At the patient level, 11,137(15.2%) received an HCC exception and 4,519 (6.2%) received an exception for other conditions. Median (IQR) age at listing was 53 (48–59) among patients contributing non-exception time, 56 (52–61) for HCC exception patients, and 53 (45–58) for other exception patients (Table 1).
Figure 1. Construction of the study population.
Table 1. Characteristics of the study population.
The proportion of patients with exceptions who received a liver transplant (72.4% for HCC exceptions, 70.8% for other exceptions) was much higher than for patients who did not receive an exception (44.6%). Similarly, the proportion of patients with exceptions who died (10.2% for HCC exceptions, 11.3% for other exceptions) was much lower than for non-exception patients (21.6%).
| Non-exception | HCC exception | Otherexception | Total1 | |
|---|---|---|---|---|
| Patients | 60,885 | 11,137 | 4,519 | 73,154 |
| N (%) male | 39,269 (64.5%) | 8,632 (77.5%) | 2,813 (62.2%) | 48,336 (66.1%) |
| Median (IQR) age at listing | 53 (48–59) | 56 (52–61) | 53 (45–58) | 54 (48–59) |
| Number (%) transplanted | 27,178 (44.6%) | 8,061 (72.4%) | 3,202 (70.8%) | 36,605 (50.0%) |
| Number (%) dropped out/died | 13,142 (21.6%) | 1,135 (10.2%) | 511 (11.3%) | 14,094 (19.3%) |
| Patient-days | 21,725,307 | 407,021 | 205,610 | 22,337,938 |
Values for column 4 may be less than the sum of columns 1 through 3 because some waiting list registrants contribute time in more than one category
Person-Time
Although 15,656 of 73,154 (21.4%) of patients received an exception, only 0.6 million of 22.3 million patient-days (2.7%) were considered exception person-time (eMELD>cMELD). This is because many exception patients contributed some non-exception person time after receiving an exception when cMELD≥eMELD (see methods); 3,385 of 15,656 exception patients (21.6%) had one or more days of non-exception person time after their exception was granted. Also, exception patients tended to remain on the waiting list for less time than most non-exception patients, thereby contributing less person time on the list than patients without exceptions. Of 42,444 non-exception patients who registered on or before February 28, 2008, 12,057 (28.4%) remained on the waiting list for at least two years; by contrast, of 11,090 exception patients who registered by that date, only 1,413 (12.7%) remained on the waiting list for at least two years.
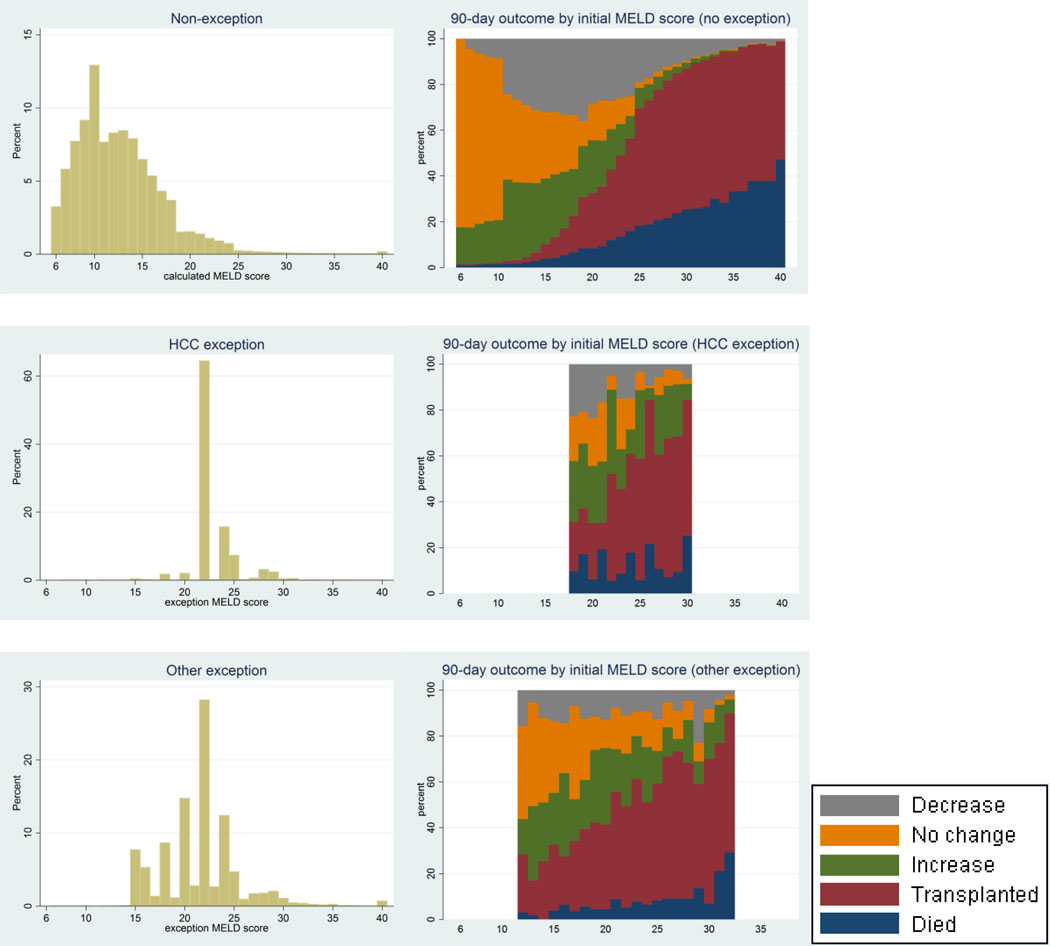
Median aMELD (IQR) for non-exception person-time was 12 (8–14); aMELD values were skewed to the right, with an aMELD at or below 22 for 99% of non-exception person-time (Figure 2, left panel). This reflects the fact that many non-exception patients listed for liver transplantation remained relatively healthy for years, with cMELD scores consistently below 10, whereas patients with higher cMELD scores tended to either die or be transplanted after a few weeks or months. In contrast, median (IQR) aMELD score for HCC and other exception patients was 22 (22–24) points and 22 (20–24) points respectively. aMELD for HCC exception time was exactly equal to 22 or 24 for over 80% of person days;aMELD for other exception time was more spread out over the range between scores 15 and 35. On exception patient-days, median (IQR) number of additional MELD points in excess of cMELD received for exceptions (i.e. eMELD-cMELD) was 12 (8–14) for patients with HCC exceptions and 9 (5–13) for patients with other exceptions.
Figure 2. Distribution of MELD scores, and 90-day outcomes by MELD score.
Left panel shows the distribution of person-days at each MELD score for non-exception person-time, HCC exception person-time, and other exception person-time. Right panel shows risk of various outcomes (MELD decrease, no change, MELD increase, transplantation, death) by MELD score for candidates without MELD determined by lab values (calculated meld/cMELD) and with by exception score (exception meld/eMELD), separately for HCC and other exceptions. Gray, orange, green, purple, and blue represent the risk of decrease, no change, increase, transplantation, and death respectively.
Outcome Ascertainment
During the study period, 47% of patients received a transplant and 20.5% dropped out (Table 1).Fewer patients with no exception (41.8%) received a transplant than patients with an HCC (72.6%) or other (71.6%) exception; conversely, more patients with no exception (22.8%) dropped out than patients with HCC (10.7%) or other (11.7%) exception. Patients with an exception constituted 21.4% of all patients but received 30.8% of all liver transplants.
90-Day Outcomes
For patients with no exception, 90-day rates of both transplantation and dropout/death increased steadily with increasing cMELD (Figure 2, right panel).Patients with an exception were much more likely to receive a transplant, and much less likely to die while waiting, than patients with an equivalent cMELD score. For example, 90-day probabilities of transplantation and of death were 30.8% and 12.0% respectively for patients with a MELD of 22 as calculated from lab values, but 38.0% and 4.4% respectively for patients with MELD of 22 due to HCC exception and 47.0% and 5.2% respectively for patients with MELD of 22 due to other exception.
Multinomial logistic regression confirmed the discrepancy in outcomes for patients with exceptions. Patients with a MELD assigned by HCC exception had much lower odds of 90-day death, and much higher odds of 90-day transplant, then patients with the equivalent MELD derived from laboratory values (OR = 0.400.460.53 for death, 1.611.751.89 for transplant, Table 2A). A similar advantage was observed for patients with MELD assigned by other exception, although the increase in odds of transplant was less pronounced than for HCC exception patients (OR = 0.300.390.53 for death, 1.211.371.55 for transplant). Restricting only to patient-days with aMELD of 22 (thus directly comparing outcomes of exception patients with MELD of 22 to outcomes for patients with the same allocation priority due to lab values), odds ratios were 0.410.470.54 (death) and1.521.651.81 (transplant) for HCC exceptions and 0.290.380.50 (death) and1.091.231.41 (transplant) for other exceptions.
Table 2. Transplantation and removal from the waiting list, comparing patients whose allocation priority is determined by exception points to those whose priority is determined from lab values.
Models are adjusted by UNOS score, as assigned by either lab MELD (non-exceptions) or exception score (exceptions), using indicator variables for each UNOS score other than 22, the most common value for exceptions. The models are restricted to a subset of UNOS scores as indicated; for example, the model for HCC exception compares exception person-time with eMELD between 22 and 25 to non-exception person-time with cMELD between 22 and 25.
| A | ||
|---|---|---|
| 90-day outcome | Odds ratio (exception MELD / calculated MELD) |
|
| Removal or death | Transplantation | |
| HCC exception, 22 ≤ UNOS score ≤ 25 | 0.410.470.53 | 1.531.651.79 |
| Other exception, 15 ≤ UNOS score ≤ 25 | 0.360.430.52 | 1.201.331.47 |
| B | |||
|---|---|---|---|
| 1-year outcome | Odds ratio (exception MELD / calculated MELD) |
||
| Removal or death | Transplantation | ||
| HCC exception, 22 ≤ UNOS score ≤ 25 | 0.620.710.82 | 2.142.382.65 | |
| Non-HCC exception, 15 ≤ UNOS score ≤ 25 | 0.530.640.77 | 1.681.912.19 | |
| C | |||
|---|---|---|---|
| 3-year outcome | Odds ratio (exception MELD / calculated MELD) |
||
| Removal from waiting list | Transplantation | ||
| HCC exception, 22 ≤ UNOS score ≤ 25 | 0.550.630.73 | 1.902.132.39 | |
| Non-HCC exception, 15 ≤ UNOS score ≤ 25 | 0.470.580.71 | 1.611.882.19 | |
Longer-Term Outcomes
Compared to patients with MELD assigned by laboratory values, patients with a MELD assigned by exception had lower odds of death at one year (OR=0.620.710.82 for HCC exception, 0.530.640.77 for other exception, Table 2B) and three years (OR=0.550.630.73 for HCC exception, 0.470.580.71 for other exception, Table 2C). These patients also had higher odds of transplant at one year (OR=2.142.382.65 for HCC exception, 1.681.912.19 for other exception) and three years (OR=1.902.132.39 for HCC exception, 1.611.882.19 for other exception).
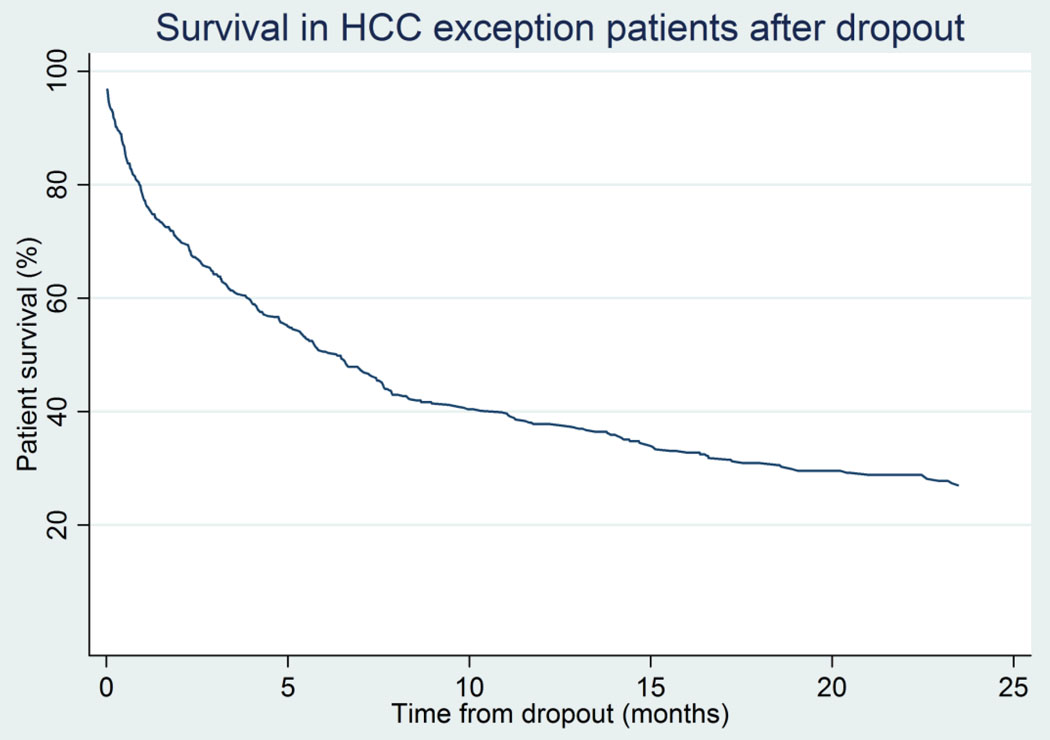
Of 1002 exception patients who dropped out through July 28, 2009, 503 (50.2%) dropped out for patient death. Among those 499 removed from the list for declining health, post-dropout mortality was 21.6% at 30 days, 35.8% at 90 days, 49.4% at six months, 62.2% at one year, and 73.0% at two years (Figure 3).
Figure 3. Survival of HCC exception patients after removal from the liver waiting list due to deteriorating health.
62% of HCC patients who dropped out due to deteriorating health died within one year.
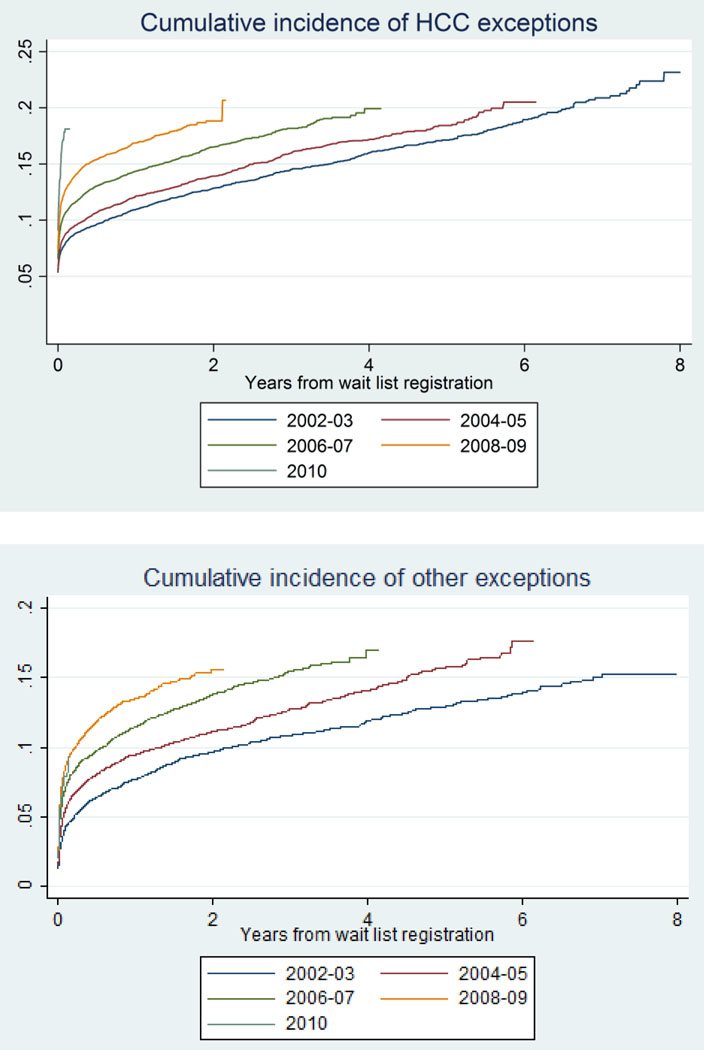
Exceptions over time
Rates of HCC and other exceptions increased for patients listed in more recent years (Figure 4). Cumulative incidence of HCC and other exceptions at one year was 10.5% and 7.0% respectively for patients registering in 2002, but rose to 15.5% and 13.5% respectively for patients registering in 2008. On average, adjusting for different rates of exception in different regions, the chance of receiving an HCC exception for a patient listing in a given year was 9% higher (HR=1.081.091.10) than that of a patient listing the year before, and the chance of receiving other exceptions was 11% higher (HR=1.091.111.12).The proportion of HCC exceptions granted for lesions beyond the Milan criteria increased from 2.7 in 2002 to 27.9% in 2008, then declining to 19.9% in 2010. In the multilevel analysis, adjusting for random region-level effects, odds of receiving an exception within a year of listing increased by 17% per year for HCC exceptions (OR=1.161.171.19) and 21% per year for other exceptions (1.191.211.23), respectively.
Figure 4. Cumulative incidence of HCC and other exceptions, stratified by year of waiting list registration.
Patients added to the waiting list in later years had a higher chance of being granted an exception, both for HCC and other exceptions.
OPO-Level and Region-Level Models
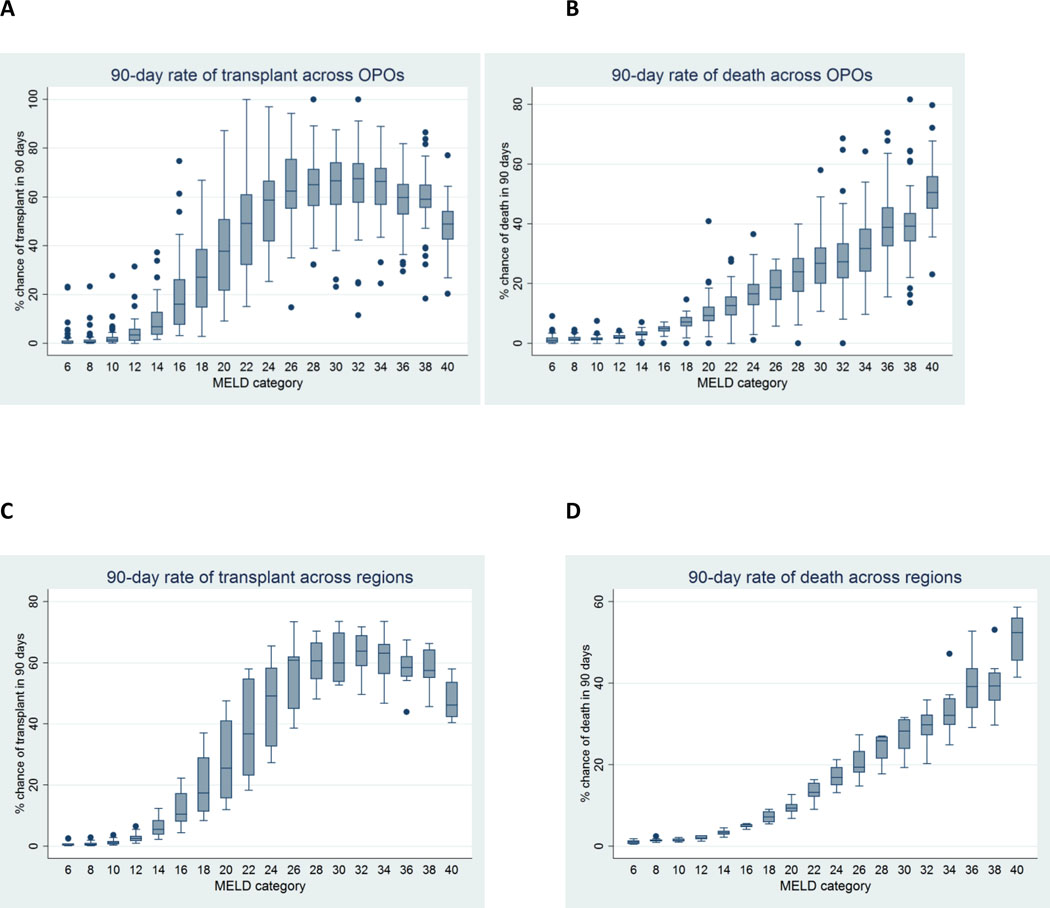
Probability of transplant within 90 days among patients of the same aMELD score varied widely across OPO, with a range of under 30% to over 90% for aMELD between 21–34 (Figure 5A). Variability was greatest at aMELD scores between 17–29.Probability of 90-day death while waiting was slightly more consistent across OPOs than probability of transplantation; nevertheless, the probability among patients with aMELD between 33–38 ranged from under 20% to over 80% (Figure 5B). Probability of 90-day outcome varied less at the regional level, although probability of transplant at a given aMELD score varied by a factor of 2 or more for aMELD values under 25 (Figure 5C–5D).
Figure 5. 90-day rates of transplantation and death while waiting, by initial allocation aMELD score, across OPOs (5A, 5B) and regions (5C, 5D).
Each box plot represents two aMELD points (e.g. the left most box represents aMELD scores of 6 or 7), except for the right most box which represents patients with an aMELD of exactly 40.
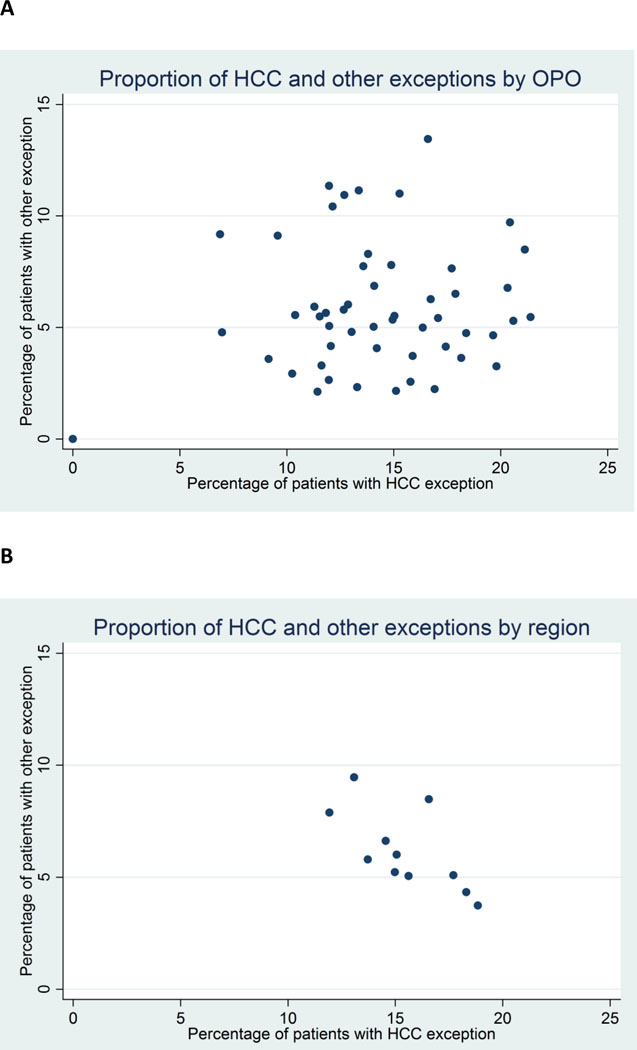
The proportion of patients per OPO receiving an HCC exception ranged from 0% to 21.4%, and the proportion of patients receiving other exceptions ranged from 0.0% to 13.1% (Figure 6A).Similarly, the proportion of patients per region receiving an HCC exception ranged from 11.9% to 18.8%, and the proportion of patients receiving other exceptions ranged from 3.7% to 9.5% (Figure 6B). There was no apparent relationship between rates of HCC and other exceptions per OPO (correlation coefficient = 0.14). However, regions with fewer HCC exceptions had, on average, more non-HCC exceptions (correlation coefficient = −0.67, Figure 6B).
Figure 6. Proportion of patients who received HCC and other exceptions, by OPO (6A) and region (6B).
HCC exceptions are more common than other exceptions. The proportion of HCC exception shows no apparent relation to the proportion of other exceptions at the OPO level (correlation coefficient = 0.14), but is inversely related to the proportion of other exceptions at the regional level (correlation coefficient=−0.67).
DISCUSSION
In this 8-year national study of patients awaiting liver transplantation, those who received a MELD exception dropped out at lower rates, and were transplanted at higher rates, than those with equivalent calculated MELD. This held true for both HCC and other exceptions. Furthermore, OPOs and regions differed in the proportion of patients who received exceptions, possibly accounting for some of the geographic heterogeneity in rates of transplantation and death on the waiting list, which varied considerably across OPO among patients of equivalent MELD score.
MELD exception points may be granted for patients whose mortality risk is believed to be greater than indicated by cMELD, or for patients who are at risk of an outcome other than mortality. In 2006, the MESSAGE conference identified two principles for non-mortality exceptions: the existence of a defined non-mortality endpoint (e.g. progression beyond Milan criteria in the case of HCC), and awarding of exception points based on estimated short-term risk of that endpoint(3). Although we lack data on non-mortality endpoints, lower rates of waitlist dropout in exception patients suggest either that the short-term risk of non-mortality negative outcome in exception patients is less than the mortality risk in non-exception patients with equivalent aMELD, or that some pretransplant negative outcomes in exception patients do not result in dropout.
Previous studies have suggested an advantage to patients with MELD exceptions relative to other patients on the waiting list. As previously mentioned, Washburn et al. identified lower dropout rates in HCC patients than in non-exception patients in the first year after registration. They compared HCC patients (who at some point received 22 eMELD points) to non-exception patients (who had initial cMELD< 21), but did not account for changes in MELD over time; as our models show, patients with low initial MELDs tend to have increased MELD scores over time, so the degree of advantage, if any, could not be estimated from their results. In 2004, Freeman et al compared the outcomes of non-exception patients in their first 90 days on the liver waiting list to outcomes of exception patients in their first 90 days after receiving their exception(9). Separately for HCC and other exceptions, they found patients with exceptions had roughly the same chance of transplant as non-exception patients with the same aMELD, but lower mortality risk. These findings contradict our findings that patients with exception points had higher chances of transplant than non-exception patients. However, their results were limited to the first 90 days after registration, did not adjust for MELD score, and used separate Cox regression techniques for each outcome, without accounting for transplant and death as competing risks. When mortality risk differs between groups, a Cox model of transplant rates censoring for death can be misleading because its fundamental assumption of uninformative censoringis violated(17). Voigt et al, analyzing applications for exception points (both granted and denied) found that cMELD predicted mortality better than requested eMELD, suggesting that lab values were better predictors of mortality than requested exception points in these patients(2).
Sulieman et al found lower risk of death in a cohort of 255 patients with HPS exceptions, as compared to a cohort of 32,358 non-exception patients (RR of mortality = 0.060.160.42); 92% of the HPS exception patients were transplanted as compared to only 46% of the non-exception patients(6). However, Krowka and Fallon noted that that standards of HPS diagnosis to determine exception points were unclear; the population of patients who received HPS exceptions may not be a good proxy for patients who truly have HPS(18). Previous work has shown increased mortality in cirrhosis patients with HPS, compared to cirrhosis patients without HPS(19). If misclassification in diagnosis accounts for such a large discrepancy, it is likely to be a problem for other exception diagnoses as well. Rodriguez-Luna et al reported in 2005 that the proportion of patients with a non-RED exception varied by region from 0.7% to 8.3%, and rates of approval for non-RED exception applications ranged from 28% to 75% (4). Similarly, Salvalaggio reported significant regional variation in exceptions for pediatric recipients (20).
We have shown that the proportion of registrants who receive an exception has increased for every year of registration since the start of the MELD era. Although this could in principle be due partly to new evidence over time that different diagnoses are deserving of an exception, a likely explanation is that clinicians have responded either to previous evidence that exception patients are favored, or to intuition that exception patients in their practice have better outcomes. The rise in exceptions over time can therefore be understood as a natural response to the incentive provided by the exception system. However, as the proportion of new registrants obtaining an exception increases, the disadvantage of patients who do not receive exceptions grows more severe.
Our analysis of exceptions other than HCC is limited by lack of data on the cause of these exceptions. After HCC, the next most common reason for a MELD exception, as captured by UNOS/OPTN, is "Other" with no further information. Additionally, although we hypothesize that different rates of exceptions by OPO may be partly attributable to differing aggressiveness in pursuing exceptions, we have no data on the rates of exception-eligible diagnoses among patients who do not receive an exception.
MELD is a useful indicator of risk of mortality due to liver failure, but it is not perfect, and without an exception policy, MELD-based allocation would fatally discriminate against patients whose risk is not reflected in their calculated MELD. However, a policy that unduly advantages patients who receive an exception leads to the same form of discrimination in the opposite direction, while creating further inequity by advantaging patients whose providers aggressively pursue exceptions. While MELD exceptions are often granted to avoid the risk of development of non-mortality outcomes in the longer term than that which is captured by MELD, the use of a MELD exception to skip over a patient with a relatively high risk of dying before receiving a subsequent liver offer merits serious consideration. In order to allocate deceased donor livers fairly, it is important to standardize exception policies, be judicious in the awarding of exceptions, and use mathematical models to assign exception points according to predicted risk.
ACKNOWLEDGEMENTS
The UNOS National Data Registry is supported in part by Health Resources and Services Administration contract 231-00-0115.This work was supported by grant number RC1DK086450 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The analyses described here are the responsibility of the authors alone and do not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
ABBREVIATIONS
- aMELD
allocation MELD (MELD score used for purposes of prioritization for liver allocation, whether calculated from lab values or through an exception)
- cMELD
calculated MELD (MELD score calculated from lab values)
- eMELD
exception MELD (exception score assigned to patients with a MELD exception)
- HCC
Hepatocellular carcinoma
- HPS
hepatopulmonary syndrome
- HR
hazard ratio
- IQR
interquartile range
- OPO
Organ Procurement Organization
- OPTN
Organ Procurement and Transplantation Network
- OR
odds ratio
- RED
recognized exception diagnosis
- RR
relative risk
- MELD
Model of End-stage Liver Disease
- UNOS
United Network for Organ Sharing
Footnotes
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Contributor Information
Allan B. Massie, Email: amassie@jhsph.edu.
Brian Caffo, Email: bcaffo@jhsph.edu.
Sommer Gentry, Email: gentry@usna.edu.
Erin Carlyle Hall, Email: erincarlylehall@gmail.com.
David Axelrod, Email: David.A.Axelrod@hitchcock.org.
Krista L. Lentine, Email: lentinek@slu.edu.
Mark A. Schnitzler, Email: schnitm@slu.edu.
Adrian Gheorghian, Email: agheorgh@slu.edu.
Paolo R. Salvalaggio, Email: salvalaggio@einstein.br.
REFERENCES
- 1.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 2.Voigt MD, Zimmerman B, Katz DA, Rayhill SC. New national liver transplant allocation policy: is the regional review board process fair? Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2004;10(5):666–674. doi: 10.1002/lt.20116. [DOI] [PubMed] [Google Scholar]
- 3.Freeman RB, Jr, Gish RG, Harper A, Davis GL, Vierling J, Lieblein L, et al. Model for end-stage liver disease (MELD) exception guidelines: results and recommendations from the MELD Exception Study Group and Conference (MESSAGE) for the approval of patients who need liver transplantation with diseases not considered by the standard MELD formula. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2006;12(12) Suppl 3:S128–S136. doi: 10.1002/lt.20979. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Luna H, Vargas HE, Moss A, Reddy KS, Freeman RB, Mulligan D. Regional variations in peer reviewed liver allocation under the MELD system. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2005;5(9):2244–2247. doi: 10.1111/j.1600-6143.2005.01008.x. [DOI] [PubMed] [Google Scholar]
- 5.Wiesner R, Lake JR, Freeman RB, Gish RG. Model for end-stage liver disease (MELD) exception guidelines. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2006;12(12) Suppl 3:S85–S87. doi: 10.1002/lt.20961. [DOI] [PubMed] [Google Scholar]
- 6.Sulieman BM, Hunsicker LG, Katz DA, Voigt MD. OPTN policy regarding prioritization of patients with hepatopulmonary syndrome: does it provide equitable organ allocation? American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2008;8(5):954–964. doi: 10.1111/j.1600-6143.2007.02124.x. [DOI] [PubMed] [Google Scholar]
- 7.Thuluvath PJ, Guidinger MK, Fung JJ, Johnson LB, Rayhill SC, Pelletier SJ. Liver transplantation in the United States, 1999–2008. Am J Transplant. 10(4 Pt 2):1003–1019. doi: 10.1111/j.1600-6143.2010.03037.x. [DOI] [PubMed] [Google Scholar]
- 8.Washburn K. Model for End Stage Liver Disease and hepatocellular carcinoma: a moving target. Transplant Rev (Orlando) 24(1):11–17. doi: 10.1016/j.trre.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 9.Freeman RB, Jr, Wiesner RH, Roberts JP, McDiarmid S, Dykstra DM, Merion RM. Improving liver allocation: MELD and PELD. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2004;4 Suppl 9:114–131. doi: 10.1111/j.1600-6135.2004.00403.x. [DOI] [PubMed] [Google Scholar]
- 10.Washburn K, Edwards E, Harper A, Freeman R. Hepatocellular carcinoma patients are advantaged in the current liver transplant allocation system. Am J Transplant. 10(7):1643–1648. doi: 10.1111/j.1600-6143.2010.03127.x. [DOI] [PubMed] [Google Scholar]
- 11.Roayaie K, Feng S. Allocation policy for hepatocellular carcinoma in the MELD era: room for improvement? Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2007;13(11) Suppl 2:S36–S43. doi: 10.1002/lt.21329. [DOI] [PubMed] [Google Scholar]
- 12.Agresti A. Categorical Data Analysis. Wiley-Interscience; 2002. [Google Scholar]
- 13.Louis TA, Zeger SL. Effective communication of standard errors and confidence intervals. Biostatistics. 2009;(1):1–2. doi: 10.1093/biostatistics/kxn014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Massie AB, Desai NM, Montgomery RA, Singer AL, Segev DL. Improving distribution efficiency of hard-to-place deceased donor kidneys: Predicting probability of discard or delay. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010;10(7):1613–1620. doi: 10.1111/j.1600-6143.2010.03163.x. [DOI] [PubMed] [Google Scholar]
- 15.Massie AB, Stewart DE, Dagher NN, Montgomery RA, Desai NM, Segev DL. Center-level patterns of indicated willingness to and actual acceptance of marginal kidneys. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010;10(11):2472–2480. doi: 10.1111/j.1600-6143.2010.03294.x. [DOI] [PubMed] [Google Scholar]
- 16.Massie AB, Zeger SL, Montgomery RA, Segev DL. The effects of DonorNet 2007 on kidney distribution equity and efficiency. Am J Transplant. 2009;9(7):1550–1557. doi: 10.1111/j.1600-6143.2009.02670.x. [DOI] [PubMed] [Google Scholar]
- 17.Putter H, Fiocco M, Geskus RB. Tutorial in biostatistics: competing risks and multi-state models. Statistics in medicine. 2007;26(11):2389–2430. doi: 10.1002/sim.2712. [DOI] [PubMed] [Google Scholar]
- 18.Krowka MJ, Fallon MB. Liver transplantation for hepatopulmonary syndrome (HPS): what is the MESSAGE? American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2008;8(5):911–912. doi: 10.1111/j.1600-6143.2008.02190.x. [DOI] [PubMed] [Google Scholar]
- 19.Fallon MB, Mulligan DC, Gish RG, Krowka MJ. Model for end-stage liver disease (MELD) exception for hepatopulmonary syndrome. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2006;12(12) Suppl 3:S105–S107. doi: 10.1002/lt.20971. [DOI] [PubMed] [Google Scholar]
- 20.Salvalaggio PR, Neighbors K, Kelly S, Emerick KM, Iyer K, Superina RA, et al. Regional variation and use of exception letters for cadaveric liver allocation in children with chronic liver disease. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2005;5(8):1868–1874. doi: 10.1111/j.1600-6143.2005.00962.x. [DOI] [PubMed] [Google Scholar]