Hypertension contributes significantly to cardiovascular mortality and morbidity in most parts of the world, and as a contributory modifiable risk factor is found to be second only to smoking.[1] The overall prevalence of hypertension in both developed (e.g. 28.7% in the USA) and developing world (e.g. 20% in India) is alarming.[2,3] The ever increasing prevalence is largely due to the so-called primary or essential hypertension which constitutes more than 90% of hypertensive population. Among those with hypertension, there is a small group described as secondary where a rare identifiable cause can be found and treated in manner that cures the patients. If renovascular and renal parenchymal causes are excluded, the possible cause of secondary hypertension would invariably lie in the endocrine system. In the past, the discussions encompassing the term “endocrine hypertension” would invariably be restricted to the adrenal gland. No doubt, the first or “big three” forms in this category, namely, pheochromocytoma, Cushing's syndrome, and Conn's syndrome, involve the adrenal gland.[4] A PUBMED search for articles using the terms “Endocrinology and Hypertension” strongly supports the observation made above [Figure 1]. Adrenal was the primary topic of discussion in more than one-half of the 100 oldest citations, published during late 1940s and early 1950s.There was not a single article in the category of Diabetes and Metabolic syndrome. Similar analysis of 100 latest citations using the same search term reveals that Diabetes and Metabolic syndrome category, with 40% of articles, has occupied the first place ahead of the adrenal, which is now in second place with 19% articles [Figure 1].
Figure 1.
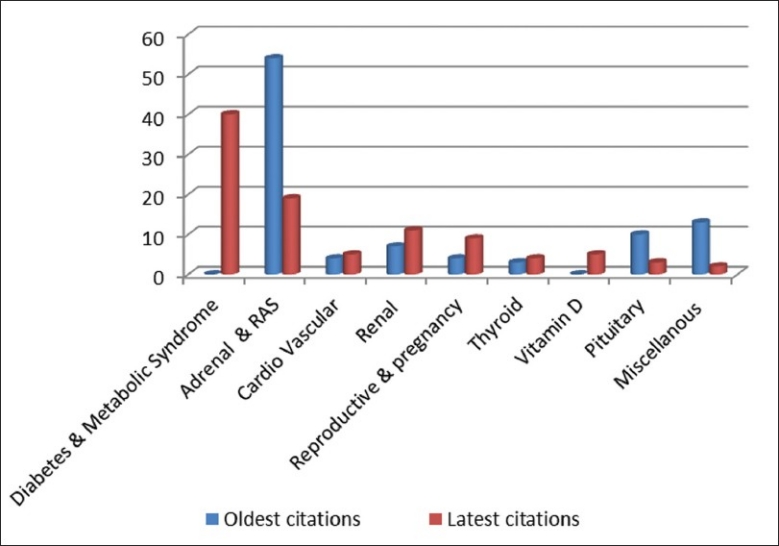
Break-up into different categories of 100 oldest and 100 latest citations from a PUBMED search using the search term “endocrinology and hypertension”
What do all these mean to an endocrinologist? Two decades ago, the role of an endocrinologist in managing hypertension remained pre-defined, i.e. to confirm the diagnosis and plan management in the small, but interesting sub-population of secondary hypertensive patients. Essential hypertension remained the domain of cardiologists and internists. The last two decades have seen an explosion of scientific information on the etio-pathogenesis of essential hypertension, specially related to the renin angiotensin aldosterone (RAS) axis. Discovery of tissue or local or nonclassical RAS has opened up newer insights to our understanding of the so-called primary hypertension. Further to this, research has indicated, amongst subjects with essential hypertension, the important role of aldosterone and mineralocorticoid receptors such as extra-adrenal aldosterone synthesis, impact of aldosterone on vascular and cardiac inflammation and fibrosis, and the action of glucocorticoid hormones at mineralocorticoid receptors.[5] Hence, it is high time that endocrinologists took a big leap forward to transcend the clear demarcation between secondary and primary hypertension and involve themselves extensively in discussions of the former. This supplement aims basically to address the changing paradigm of the endocrine perspective of hypertension and to redefine the role of an endocrinologist in this phase of transition. Hence, it is no wonder that this issue includes wide range of topics such as “pheochromocytoma” and “mineralocorticoid hypertension” which are hardcore endocrine to transitional topics such as “Management of diabetic hypertensive,” and “Essential hypertension in adolescents and children,” or even translational topics such as “Fetal origin of vascular ageing.”
The first review in this supplement takes the reader to a journey through the current basic understanding of BP control, the role of endothelial, neural and renal factors, and finally elaborating the endocrine mechanisms involved. It makes lot of sense to recapitulate certain things which gives a feeling of “Oh! I knew it so well” because they are bound to reappear in a more extensive and complex manner in the other articles in this supplement.
One topic which caught the imagination of research workers and clinicians alike before the last millennium ended is the imprint of the environment of the mother's womb on the expression in the post-natal life of certain genes that would eventually play a central role in the pathogenesis of the so-called lifestyle diseases including hypertension. The review titled “Fetal origin of vascular ageing” gives a critical appraisal of this interesting hypothesis.
By the time Prof. Jerome W. Conn[6] described a 34-year-old lady with a 7-year history of muscle spasms, temporary paralysis, tetany, and weakness, and a 4-year history of hypertension in his presidential address at the annual meeting of the Central Society for Clinical Research in Chicago, Illinois, October 29, 1954, he had the advantage of using a bioassay technique to measure sodium retention in adrenalectomized rats after intraperitoneal injection of human urine. The referred subject averaged 1333 μg deoxycorticosterone equivalent per day compared with normotensive controls at 61.4 μg per day. This helped Prof Conn to direct his surgical colleagues to do a bilateral adrenal excision (unlike exploratory laparotomy in the first case of pheochromocytoma, please see below) which later provided complete remedy to the patient. Conn studied this patient in the Metabolism Research Unit for 227 days before making a provisional diagnosis. Advances in hormone assays, nucleotide imaging and discovery of aldosterone antagonists have made the diagnosis and management of primary aldosteronism much easier. The topic of mineralocorticoid hypertension is extensively reviewed by Gupta in this issue, with special emphasis on the monogenic prototype of secondary hypertension caused by mineralocorticoid excess. Some aspects of this topic with special reference to children and adolescents find mention in the review by Bhavani.
Cushing's syndrome has remained an enigma for endocrinologists across the globe. Hypertension is present in about 80% of patients with this condition. Singh et al. initiate their review by introducing the reader to the clinically relevant issues pertaining to this enigmatic disease. The later part of their review takes on hypertension in Cushing's syndrome in a comprehensive manner. The article by Lila et al. aptly addresses the diagnostic dilemma of Cushing's syndrome and emphasizes the need for screening for hypercortisolism and advocates a stepwise protocol for arriving at the final diagnosis. Presence of comorbidities such as hypertension, hyperglycemia, obesity and hypokalemia make anesthesia during the surgical management of Cushing's syndrome a really a challenging task. The article by Domi makes a laudable effort to underscore some of the vital points in this regard.
In discussions of endocrine hypertension, pheochromocytoma has always attracted attention because of its strikingly unique presentation and dramatic change of events leading to complete cure following surgery. What seems to be so straightforward to the current generation of endocrinologists was not so to start with. It took more than 6 months for Charles Mayo and his team to evaluate, diagnose and finally discharge after a successful operation, a 30-year-old Catholic nun who happened to be the first properly described case of pheochromocytoma.[7] In the absence of a clear understanding of neuro-endocrine physiology and avenues for proper radiological or radio-nucleotide imaging, the pre-operative differential diagnoses as listed in the patient's medical record were vague and included conditions such as “generalized intermittent vascular spasm” and “paroxysmal tachycardia with vasomotor constriction and hypertensive crisis—cause unknown.” In a similar manner, the list of medications used to control the paroxysms of hypertension during pre-operative management also had a bizarre look and included quinidine, digitalis, amyl nitrate, sodium nitrate, sodium bromide, potassium iodide, morphine sulfate, atropine, histamine, chloral hydrate, typhoid vaccine, liver extract, choline, tincture of belladonna, and tobacco smoke. No wonder, none of these agents provided relief from the hypertensive spells.[8] Since then, our understanding of catecholamine physiology and suitable drugs to counter their excess has seen a revolutionary change. Garg et al. offer a comprehensive review on a vast topic like pheochromocytoma in a very lucid manner. While surgical approaches have become easier, anesthesia in pheochromocytoma surgery still remains a challenge. In this issue, Bajwa et al. have described the important and clinically relevant points to be undertaken during the pre-operative preparation as well as intra-operative and immediate post-operative phase. Justifying the myriads of presenting features of the tumor, two interesting cases of pheochromocytoma as a part of Von Hippel-Lindau (VHL) disease and diffuse neurofibromatosis find place in this supplement.
A sub-group of the family of endocrine hypertensive disorders has common characteristics of heritability and phenotype of mineralocorticoid excess. They are rare forms of secondary hypertension, but constitute a distinctly important category in the evaluation of pediatric patients with hypertension. These conditions are discussed in two articles in this supplement, complementing each other in their content: Gupta highlights the endocrine aspect, and Bhavani emphasizes the pediatric aspect.
In the “classic three” of endocrine hypertension, the causal role of adrenal gland is well documented. Although such concrete and anatomically definable definitive association is not there, hypertension in thyroid disorder is also well known. Hyperparathyroidism also has been associated with increased incidence of hypertension, the etiological mechanism of which is hitherto unknown. It is no wonder that no discussion on endocrine hypertension can be completed without mentioning these endocrine glands. The article by Chopra et al. will enlighten the reader in this aspect.
Vitamin D has traveled a long way since being considered merely as a “vitamin” to an omnipresent hormone involved in myriad of biological systems in human. In its new incarnation in this millennium, it has been implicated to be protective against the pathogenesis of certain important components of metabolic syndrome, including hypertension. A brief update is available in the review by Chopra et al. In their original article published in this supplement, Kota et al. provide evidence favoring an association of high blood pressure and increased RAS activity with hypovitaminosis D. The outcome of this study provides enough food for thought to the readers.
A number of articles in this supplement address issues beyond the domain of classical endocrine hypertension. As discussed earlier, this is a necessary step to redefine the role of endocrinology in so-called essential hypertension. The review of neuro-endocrine physiology by Chopra et al. will help the reader understand the pathophysiology of essential hypertension, in general, and the role of RAS, in particular. Essential hypertension in three populations, namely, pediatric, pregnant, and diabetic, is discussed in three reviews by Raj, Magon, and Ganesh and Viswanathan, respectively. The current understanding of hypertension indicates a polygenic etiopathogenesis, the major part of which remains ill-understood. Hence, a multi-pronged approach such as identifying the high-risk groups and countering various mechanisms in the etiopathogenesis at different levels is of paramount importance. The referred articles give ample insight in these aspects. There is no denying of the fact that Indians as a race are relatively more prone to develop the phenotypic changes of metabolic syndrome, that too in an earlier age. While the epidemic of diabetes mellitus amongst Indians has been highlighted in various publications, the other component of the so-called “twin epidemic,” i.e. hypertension, has not received adequate attention.[9] The SITE epidemic study which has been completed will provide answers in this aspect. This supplement has the privilege of offering the first article related to this study, describing the study rationale and research methodology.
The so-called “cardio-vascular endocrinology” is one area where significant translational research is going on. Hormones of the heart, such as natriuretic peptides (NPs), have traveled from the laboratory to the clinician's table. The origin of this science and the diagnostic, prognostic and therapeutic role of NPs are discussed in the review by Pandit in this supplement in a lucid manner.
Evaluation of endocrine hypertension, or for that matter, any sort of endocrine pathology revolves around competitive immunoassay with very high precision. But localization of a causative structural lesion requires highly sensitive and reasonably specific imaging tool. The advent of high-resolution ultrasonography (HRUSG), multislice and dynamic computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) have fulfilled such need to a great extent. The role of nuclear imaging in the evaluation of endocrine hypertension is immense. The review in this supplement authored by Das, Baruah and Baruah provides enough information and some beautiful images for the benefit of our readers.
REFERENCES
- 1.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Hajjar I, KotchenTA Trends in prevalence, awareness, treatment, and control of Hypertension in the United States, 1988-2000. JAMA. 2003;290:190–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 3.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai-The Chennai Urban Rural Epidemiology Study (CURES-52) J Assoc Phyicians India. 2007;55:326–32. [PubMed] [Google Scholar]
- 4.Karakoff LR. Endocrine Hypertension (guest editorial) Endocrinol Metab Clin N Am. 2011;40:17–9. [Google Scholar]
- 5.Carey RM. Overview of Endocrine Systems in Primary Hypertension. Endocrinol Metab Clin N Am. 2011;40:265–77. doi: 10.1016/j.ecl.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Conn JW. Presidential address. I. Painting background. II. Primary aldosteronism, a new clinical syndrome. J Lab Clin Med. 1955;45:3–17. [PubMed] [Google Scholar]
- 7.van Heerden JA. First encounters with pheochromocytoma.The story of Mother Joachim. Am J Surg. 1982;144:277–9. doi: 10.1016/0002-9610(82)90525-6. [DOI] [PubMed] [Google Scholar]
- 8.Young WF. Endocrine Hypertension: Then and Now. Endocr Pract. 2010;16:888–902. doi: 10.4158/EP10205.RA. [DOI] [PubMed] [Google Scholar]
- 9.Joshi SR, Parikh RM. India-diabetes capital of the world: now heading towards hypertension. J Assoc Physicians India. 2007;55:323–4. [PubMed] [Google Scholar]


