Summary points
Schistosomiasis, or bilharzia, is a common intravascular infection caused by parasitic Schistosoma trematode worms
It is prevalent in Africa, the Middle East, South America, and Asia
Acute schistosomiasis, or Katayama syndrome, can present as fever, malaise, myalgia, fatigue, non-productive cough, diarrhoea (with or without blood), haematuria (S haematobium), and right upper quadrant pain
Chronic and advanced disease results from the host’s immune response to schistosome eggs deposited in tissues and the granulomatous reaction evoked by the antigens they secrete
S mansoni, S japonicum, S intercalatum, and S mekongi cause intestinal disease; S haematobium causes urinary disease
Neuroschistosomiasis is arguably the most severe clinical syndrome associated with schistosome infection
Microscopic examination of excreta (stool, urine) is the gold standard diagnostic test but requires the adult worms to be producing eggs; serological tests can diagnose less advanced infections
Praziquantel 60 mg/kg in three doses over one day (S japonicum and S.mekongi); and 40 mg/kg in doses over one day (S mansoni, S haematobium, S intercalatum) remains the treatment of choice although others are being investigated
Preventive chemotherapy is with a single oral dose of praziquantel 40 mg/kg
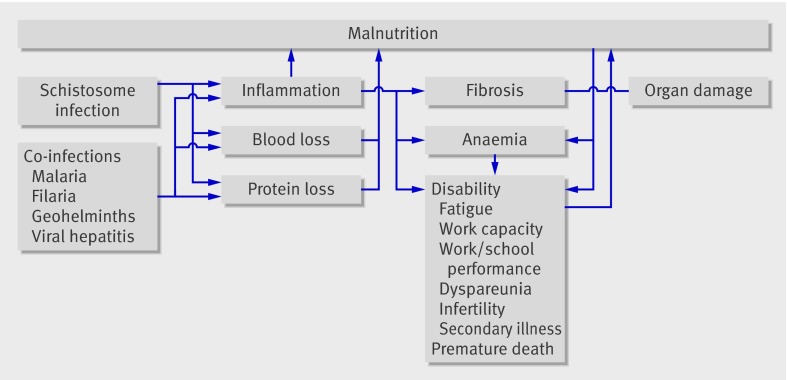
Schistosomiasis, or bilharzia, is a common intravascular infection caused by parasitic Schistosoma trematode worms.1 2 A systematic review and meta-analysis published in 2006 estimated that more than 200 million people are infected across Africa, Asia, and South America, and close to 800 million are at risk of infection.3 Meta-analyses have estimated that the current disease burden may exceed 70 million disability adjusted life years.4 5 The disease is also associated with anaemia, chronic pain, diarrhoea, exercise intolerance, and undernutrition, and female urogenital schistosomiasis may be a risk factor for HIV infection.4w15 Figure 1 shows the proposed pathway of schistosomiasis associated disease and disability derived from meta-analyses of disability-related outcomes.4
Fig 1 Proposed pathways of schistosomiasis associated disease and disability. Adapted from King et al4 with permission from Elsevier
Schistosome transmission requires contamination of water by faeces or urine containing eggs, a specific freshwater snail as intermediate host, and human contact with water inhabited by the intermediate host snail.1 2 Schistosomiasis transmission is highly dependent on environmental conditions, particularly those affecting the snail host. Climate change will alter aquatic environments and subsequently the transmission and distribution of waterborne diseases.6w2
In this review, we introduce the schistosome parasites and describe the pathophysiology and the clinical disease they cause. We discuss current diagnostic tools and the management of schistosomiasis, based on evidence from studies of both high and lower quality as well as information from current international guidelines.
Sources and selection criteria
Information for this clinical review was obtained from personal reference archives, personal experience, and extensive literature searches of the PubMed and Cochrane databases. We sourced English language papers that were fully published mainly between 2000 and September 2010 using appropriate index terms. Keywords included: “schistosomiasis”; “human schistosomiasis”; “schistosoma”; “schistosomiasis” with “diagnosis”, “treatment”, “acute”, “clinical”, “review”, and “meta analysis”; and “schistosoma” with “diagnosis”, “treatment”, “acute”, “clinical”, “review”, “meta analysis”; and “schistosome-induced pathophysiology clinical disease”.
Where and how is schistosomiasis acquired?
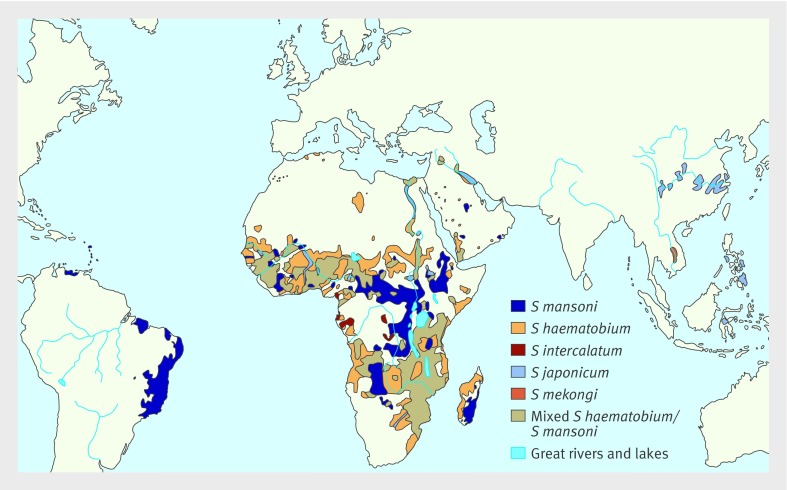
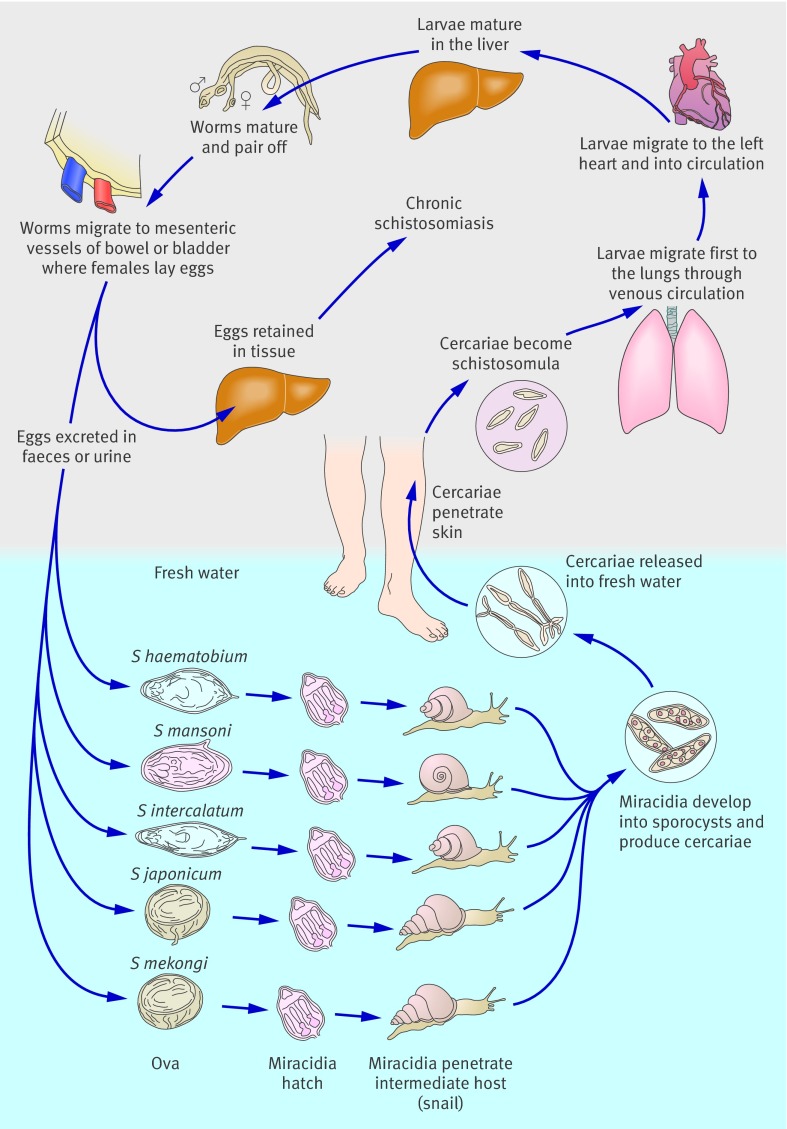
The global distribution of schistosomiasis is shown in figure 2, which is based on WHO statistics. 1The majority of infections with Schistosoma haematobium, Schistosoma mansoni and Schistosoma intercalatum are found in sub-Saharan Africa.1S mansoni remains endemic in parts of Brazil, Venezuela, and the Caribbean. Schistosoma japonicum infection occurs in the People’s Republic of China, the Philippines, and small pockets in Indonesia, despite substantial and largely successful control measures.1 2Schistosoma mekongi is found along the Mekong River in Cambodia and Lao People’s Democratic Republic (Laos).1 2 7 Infection is usually acquired through activities such as swimming, bathing, fishing, farming, and washing clothes. Important transmission sites include Lake Malawi and Lake Victoria in Africa, the Poyang and Dongting Lakes in China, and along the Mekong River in Laos. The life cycle of the schistosome is depicted in figure 3 . Intermediate snail hosts are more likely to inhabit still to moderately flowing fresh water and infection increases exponentially with length of time in contact with water, peaking at 30 minutes.w3
Fig 2 Global distribution of schistosomiasis. Adapted from Gryseels et al2 with permission from Elsevier.
Fig 3 Schistosome lifecycle. Freshwater molluscs act as intermediate hosts and higher order vertebrates as definitive hosts. Adult male and female worm pairs (slender female schistosome lies within the ventral gynaecophoric canal of the male) produce numerous eggs, most of which are deposited in the capillaries and tissues of the parasitised target organ and some of which are excreted via the urine or faeces. The shape of the eggs and the location of their excretion differentiate the various species. S haematobium inhabits the urinary system and the sacral and pelvic vessels, while intestinal schistosomes inhabit the intestinal mucosa. Some eggs are carried downstream in the portal circulation and, in the case of an S mansoni or S japonicum infection, are trapped in the liver. Once excreted, an ovum hatches in contact with fresh water and a free living motile miracidium is released to infect the specific freshwater snail intermediate host—with S mansoni this is generally Biomphalaria glabrata (Americas) or B pfeifferi (Africa). After about 30 days infected snails release free swimming cercariae in response to sunlight. These can penetrate the skin of the mammalian host within 12-24 hours, invade the lymphatic system, and enter the circulation via the lungs as maturing schistosomula.
What are the clinical features of schistosomiasis?
Schistosomiasis progresses in three distinct phases: acute, chronic, and advanced disease.
Early manifestations
Rash
A maculopapular eruption, comprising discrete erythematous raised lesions that vary in size from 1 cm to 3 cm, may arise at the site of percutaneous penetration by schistosome cercariae. (fig 4 ) Migrants or tourists infected for the first time may develop a skin reaction within a few hours, although a rash may appear up to a week later. This is less severe than, although similar to, “swimmers itch”, which is not a sequela of acute schistosomiasis but rather an immune reaction that develops in sensitised people when they are reinfected by species of schistosomes that do not colonise humans.1 2
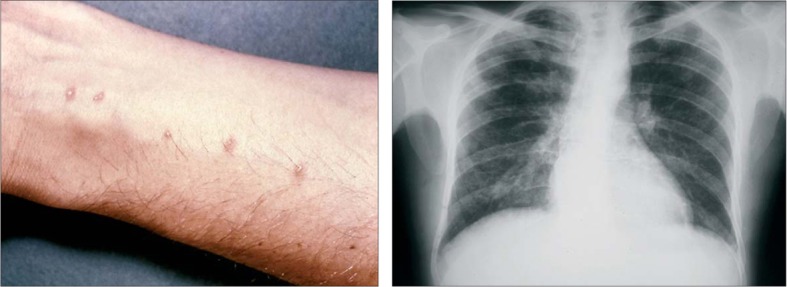
Fig 4 Clinical manifestations of acute schistosomiasis. Left: maculopapular rash (www.dpd.cdc.gov/dpdx/HTML/ImageLibrary/A-F/CercarialDermatitis/body_CercarialDermatitis_il2.htm). Right: chest radiograph showing pulmonary infiltrates. Reproduced from McManus et al13 with permission from the American Society for Microbiology.
Acute schistosomiasis (Katayama syndrome)
The symptoms of acute schistosomiasis are mediated by the immune complexw4-w7 and usually begin with the deposition of schistosome eggs into host tissues. Symptoms may include fever, malaise, myalgia, fatigue, non-productive cough, diarrhoea (with or without the presence of blood), haematuria (S haematobium), and right upper quadrant pain. Acute schistosomiasis is seen in people who are infected for the first time when travelling to endemic areas. In the case of S japonicum it is also associated with either a superinfection or a hypersensitivity reaction in previously infected people.8 Differential diagnoses include gastroenteritis, hepatitis A, B, and C, HIV, salmonellosis, and urinary tract infection.8
Chronic and advanced disease
Mature, patent, schistosome infections are associated with a chronic local inflammatory response to schistosome eggs trapped in host tissues, which may lead to inflammatory and obstructive disease in the urinary system (S haematobium) or intestinal disease, hepatosplenic inflammation, and liver fibrosis (S mansoni, S intercalatum, S japonicum and S mekongi).1 2 Immunopathological studies have shown that schistosomiasis results from the host’s immune response to schistosome eggs (fig 5 ) and the granulomatous reaction evoked by the antigens they secrete.1 2 9 10 Granulomas, which develop at the sites of maximal accumulation of eggs, destroy the eggs but result in fibrosis in host tissues.1 2w8-w12 Granuloma formation and the local inflammatory response mediated by CD4+ T-helper-2 lymphocytes help facilitate the passage of eggs into the lumen of the gut or urinary tract.w13
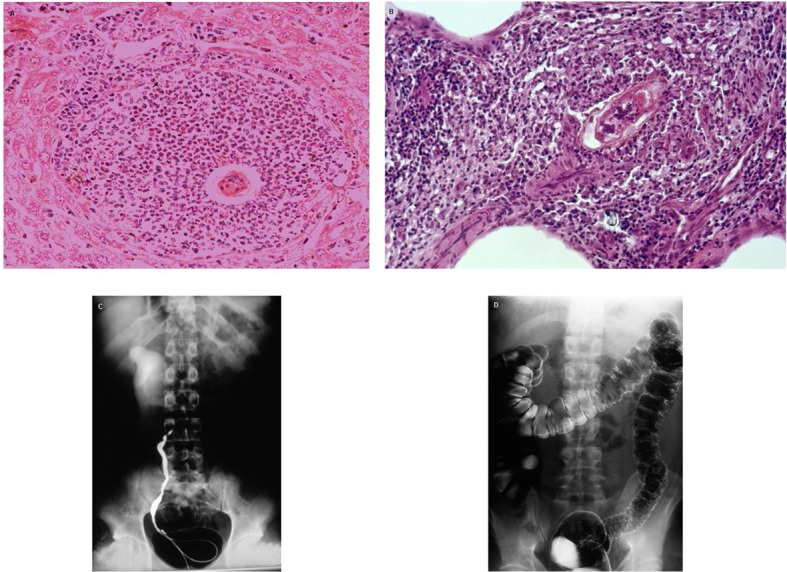
Fig 5 Chronic/advanced schistosomiasis pathology. (A) Characteristic perioval granuloma formed around S japonicum egg in mouse liver. (B) Granuloma formed around an S mansoni egg in human lung tissue. (C) Retrograde pyelogram showing right sided ureteric stricture due to infection with S haematobium. (D) Double contrast barium enema of a patient infected with S mansoni. The right side of the transverse colon (left of image) has a normal smooth mucosal lining. The left transverse colon, splenic flexure, and descending colon have a fine irregular granular mucosal surface, owing to numerous small lesions caused by deposition of schistosome eggs. The lesions result in inflammation and erosion of the mucosa. Reprinted from McManus et al13with permission from the American Society for Microbiology. Courtesy of the Wellcome Trust.
Gastrointestinal and liver disease
Eggs retained in the gut wall induce inflammation, hyperplasia, ulceration, micro-abscess formation, and polyposis. Symptoms of gastrointestinal disease include colicky hypogastric pain or pain in the left iliac fossa, diarrhoea (particularly in children) that may alternate with constipation, and haematochezia (blood in the faeces). Severe chronic intestinal disease may result in colonic or rectal stenosis. Colonic polyposis may manifest as a protein losing enteropathy. An inflammatory mass in the colon may even mimic cancer.1 2
Eggs of S mansoni and S japonicum embolise to the liver, where the granulomatous inflammatory response induces presinusoidal inflammation and periportal or clay-pipe-stem fibrosis,1 2 which population studies have shown are associated with sustained heavy infection and can take many years to develop.1 2w14-w19 Hepatomegaly, secondary to granulomatous inflammation, occurs early in the evolution of chronic disease. Periportal collagen deposits lead to the progressive obstruction of blood flow, portal hypertension, and ultimately varices, variceal bleeding, splenomegaly, and hypersplenism.1 Periportal fibrosis can be seen on ultrasonography, computed tomography, or magnetic resonance imaging and is characteristic of schistosomiasis.
Genitourinary disease
Urinary tract disease develops after infection with S haematobium and granulomatous inflammation in response to deposition of eggs in tissues.1 2w10 Haematuria, appearing 10-12 weeks after infection, is the first sign of established disease (fig 4). Dysuria and haematuria occur in early and late disease. Late disease manifestations also include proteinuria (often nephrotic syndrome), bladder calcification, ureteric obstruction, secondary bacterial infection in the urinary tract, renal colic, hydronephrosis, and renal failure.1 2w10 Structural abnormalities of the urinary tract may occur in children.1 2w20 Cystoscopy may reveal characteristic “sandy patches,” which are areas of roughened bladder mucosa surrounding egg deposits.1 2 Epidemiological studies have associated chronic urinary schistosomiasis with squamous cell carcinoma of the bladder in Egypt and other parts of Africa.w21-w25 In Egypt, the incidence of bladder cancer has decreased in line with decreasing prevalence of schistosomiasis over the past few decades.w26 w271 2S haematobium bladder squamous cell carcinomas tend to be well differentiated and metastasise locally.w21-w27 Nitrosamines, β-glucuronidase, and inflammatory gene damage have been proposed as possible carcinogenic factors.1 2w25 However, another explanation is that schistosomiasis lesions intensify the exposure of the bladder epithelium to mutagenetic substrates from tobacco or chemicals.1w22S haematobium causes genital disease in about a third of infected women.2 Vulval schistosomiasis may also facilitate the transmission of HIV, according to clinical findings; pathophysiological and immunological data, and epidemiological surveillance information.1 2 w24 w28 w29
Additional morbidity associated with schistosomiasis
Neuroschistosomiasis (fig 6 , box 1) is arguably the most severe clinical outcome associated with schistosome infection and includes signs and symptoms of increased intracranial pressure, myelopathy, and radiculopathy.1 2 11 12w30 Case studies suggest that neurological complications early in the course of infection are due to egg deposition following aberrant migration of adult worms to the brain or spinal cord. The mass effect of thousands of eggs and large granulomas in the brain or spinal cord underpin neuroschistosomiasis. Complications of cerebral disease include encephalopathy with headache, visual impairment, delirium, seizures, motor deficit, and ataxia; spinal symptoms comprise lumbar pain, lower limb radicular pain, muscle weakness, sensory loss, and bladder dysfunction.11 12 Myelopathy (acute transverse myelitis and subacute myeloradiculopathy) of the lumbosacral region is the most commonly reported neurological manifestation of both S mansoni and S haematobium infection, whereas acute encephalitis of the cortex, subcortical white matter, basal ganglia, or internal capsule is reportedly typical of S japonicum.11 12
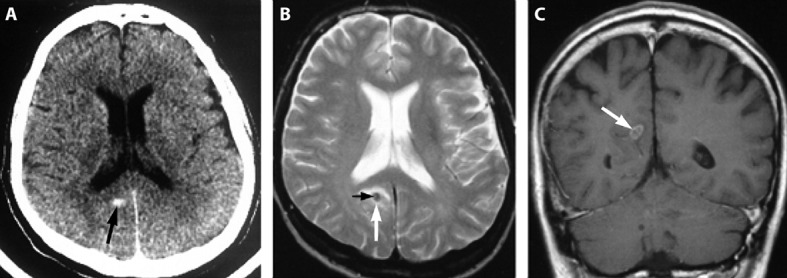
Fig 6 Pathology in neuroschistosomiasis. (A) Unenhanced axial CT scan shows small, oval, hyperdense lesion (black arrow) in the paraventricular zone, dorsal of the right posterior horn. (B) Axial T2-weighted (2437/90/1 [repetition time/echo time/excitations]) MRI shows hypointense lesion (white arrow) with small centrally located area of intermediate signal (black arrow). (C) Coronal contrast-enhanced T1-weighted (600/15/2) MRI shows oval lesion of intermediate signal (arrow) with ring-like and septum-like contrast enhancement. Reprinted from McManus et al13with permission from the American Society for Microbiology. Courtesy of the Wellcome Trust.
Box 1: Neuroschistosomiasis
Diagnosis
The finding of eggs in the stool or positive serology provides supportive but not direct evidence of schistosomal involvement in the central nervous system. A positive diagnostic finding coupled with neuroimaging and neurological symptoms should place neuroschistosomiasis high on the list of differentials. A definitive diagnosis can only be ascertained with histopathological study at biopsy or at necropsy, showing schistosome eggs and granulomas.
Signs and symptoms
Focal or generalised epilepsy (S japonicum)
Transverse myelitis (S mansoni and S haematobium)
Nystagmus
Speech disturbances
Motor weakness (hemiplegia, paraplegia, or quadriplegia)
Papilloedema
Lumbar pain and lower limb radicular pain (S mansoni and S haematobium)
Sensory loss (T12 to L1)
Bladder dysfunction
Neuro-imaging
Computerised tomography
Magnetic resonance imaging
Myelography
Management
Consult with a neurologist and an infectious disease physician
Treatment with corticosteroids and anticonvulsants within two months of infection
Praziquantel chemotherapy two months after known water contact
Population studies of children have shown that schistosome infection can cause growth retardation and anaemia, as well as possible cognitive and memory impairment, which limits their potential.1 2 13 Randomised controlled trials have shown that successful treatment in children leads to appreciable but incomplete catch-up growth and improvement in haemoglobin levels.1 2 13w26-w31 Schistosome infection seems to adversely affect maternal health and the unborn foetus. Chronic infection with S mansoni and (rarely) S haematobium, but not S japonicum, may cause pulmonary hypertension, cor pulmonale, glomerulonephritis, or transverse myelitis.w31-w36
How is schistosomiasis diagnosed?
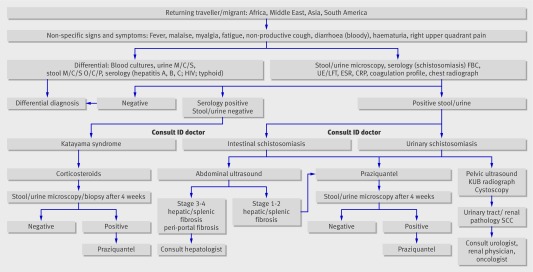
Box 2 outlines the approach to making a positive diagnosis of schistosomiasis including important questions to ask on medical history, specific signs to look for on physical examination, and relevant supportive laboratory and radiological investigations that should be undertaken. Figure 7 presents an algorithm for diagnosis and management. Microscopic examination of excreta (stool, urine) remains the gold standard test for diagnosis of schistosomiasis albeit with some limitations.1 Schistosome eggs are easy to detect and identify on microscopy owing to their characteristic size and shape with a lateral or terminal spine (fig 8 ). Wait at least two months after the last known freshwater contact before looking for eggs, as a patent infection takes this long to start producing eggs.1 2w37-w42
Fig 7 Diagnostic and treatment algorithm. M/C/S=microscopy/culture/sensitivity; O/C/P=ova/cysts/parasites; FBC=full blood count; UE/LFT=urea, electrolytes, and liver function test; ESR=erythrocyte sedimentation rate; CRP=C-reactive protein; ID doctor=infectious diseases doctor; KUB=kidney, ureter, and bladder; SCC=squamous cell carcinoma.
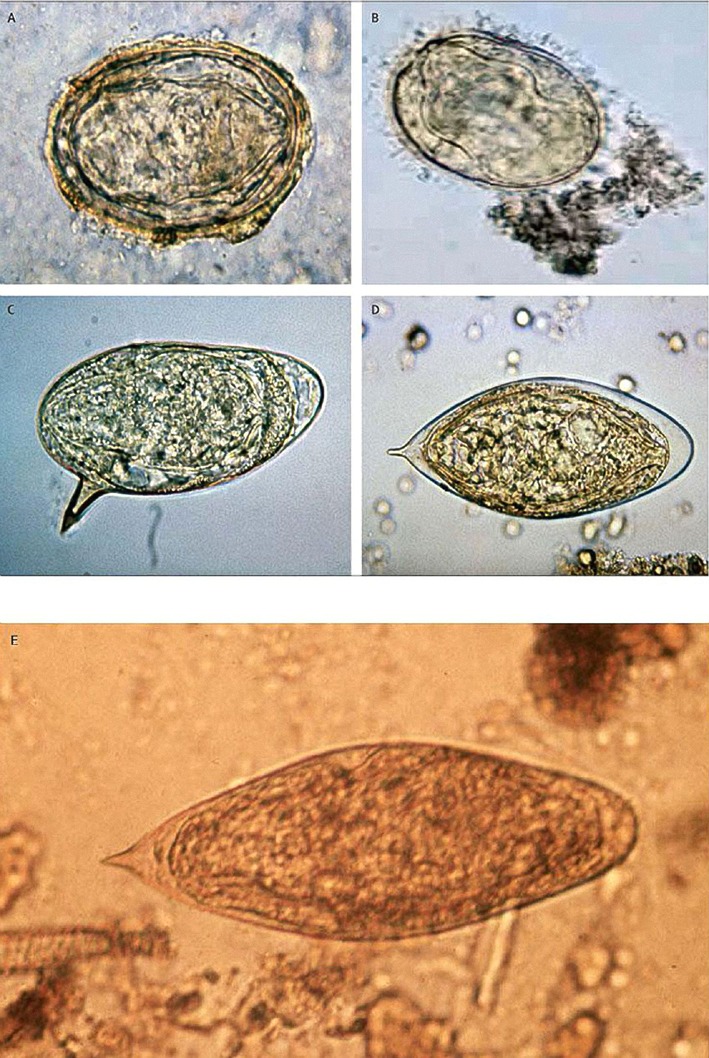
Fig 8 Schistosome eggs from species (A) S japonicum, (B) S mekongi, (C) S mansoni, (D) S haematobium,(E)S intercalatum. Courtesy of the Centers for Disease Control and Prevention, (A, C, D, and E) and www.dpd.cdc.gov/dpdx/HTML/ImageLibrary/Schistosomiasis_il.htm (B). Reproduced from Ross et al8 with permission from Elsevier.
Box 2: Key indicators for positive diagnosis of schistosomiasis
Medical history
Have you travelled to or emigrated from an endemic country recently? If so from where?
Have you been in contact with a freshwater source (such as lakes, rivers, or streams)?
(Patients returning/emigrating from Africa or the Middle East may have either intestinal or urinary schistosomiasis and those from Asia or South America may have intestinal schistosomiasis)
Physical examination
An urticarial rash (maculopapular lesions) may be present where the cercariae penetrated the skin (discrete erythematous raised lesions that vary in size from 1-3 cm)
On palpation of the abdomen, hepatomegaly (tender left lobe) and in about a third of patients splenomegaly may be detected
Auscultation of the lungs frequently detects dry or moist rales during the acute phase
Generalised lymphadenopathy may be present
Laboratory investigations
Stool/urine examination for schistosome eggs
Full blood count: eosinophilia (>80% of patients) with acute infections; anaemia and thrombocytopenia may be present in chronic and advanced schistosomiasis
Coagulation profile: prolonged prothrombin time, indicated by an increased international normalised ratio, may be evident in chronic and advanced cases
Urea, electrolytes, and liver function: raised urea and creatinine may be evident; and hyperglobulinaemia and hypoalbuminaemia may be present in chronic and advanced schistosomiasis
Serology: may be diagnostic in patients in whom no eggs are present, such as those with Katayama syndrome
Rectal or bladder biopsy for the identification of eggs may be performed if stool or urine are egg-negative but schistosomiasis is still suspected
Radiology
Chest radiograph: pulmonary infiltrates are common in acute cases (Katayama syndrome)
Abdominal ultrasound: can establish extent of liver and spleen pathology in intestinal schistosomiasis
Pelvic ultrasound: can establish extent of bladder, ureteral, and renal pathology in urinary schistosomiasis
S mansoni, S japonicum, S mekongi, and S intercalatum (intestinal schistosomiasis) are diagnosed by observing even a single egg in thick smears of stool specimens (2-10 mg) with or without suspension in saline. The extent to which eggs are shed varies and as many as three specimens may be needed to make a diagnosis in some patients. Formalin based techniques for sedimentation and concentration may increase the diagnostic yield1 in patients with a light infection, such as returned travellers.w43 The rapid, simple, and inexpensive Kato-Katz thick smear stool examination—recommended by WHO for intestinal schistosomiasis when the intensity of infection is high—is widely used in field studies, and requires 40-50 mg of faeces.14 It has specificity of 100% but its sensitivity varies with prevalence and intensity of infection, as well as with the number of stool specimens collected and slides prepared for microscopy.w44-w47 For example, one diagnostic studyw44 showed that the sensitivity increased from 85% for one stool to 100% for four stools, while anotherw45 showed that the sensitivity increased from 70% for one smear to 92% for four smears. Several population based studies have shown that mean egg burdens correlate with the mean severity of disease.1 2w46 w47 However, it is not necessary to quantify the egg burden in order to provide clinical care.
S haematobium eggs are released in urine and are detected by microscopy in a urine sample concentrated by sedimentation, centrifugation, or filtration and forced over a paper or nitrocellulose filter.1 2 A urine sample is ideally collected between 10 am and 2 pm to coincide with the maximum excretion of eggs. Self reported blood in the urine and microhaematuria on reagent strips indicates potential infection in those living in endemic areas.w48-w50
Specific and highly sensitive PCR based assays have been developed for the detection of schistosome DNA in faeces or sera and plasma.15 16 17 This approach has the potential to provide a test for diagnosing schistosomiasis in all phases of clinical disease, including the capacity to diagnose Katayama syndrome and active disease, and for the evaluation of treatment. The miracidium hatching test has been used by public health workers in China to rule out S japonicum infection.2w51 Eggs are concentrated by placing faeces in a nylon tissue bag suspended in distilled water. Miracidia that hatch are visualised macroscopically, and their presence is diagnostic of infection.
A biopsy of bladder or rectal mucosa may be considered for diagnosis in patients with a typical clinical presentation of schistosomiasis but with no eggs detectable in urine or faeces.2
Indirect methods for diagnosing schistosome infection using clinical, subclinical, or biochemical morbidity markers are not specific given the generalised presentation of schistosomiasis. Current indirect methods include the use of clinical assessment of the patient coupled with ultrasound, liver biopsy, and subsequent histological examination and the measurement of biochemical markers.1 2 Case studies have suggested that additional supportive laboratory evidence of schistosomiasis might include evidence of peripheral blood eosinophilia, anaemia (iron deficiency anaemia, anaemia of chronic disease, or macrocytic anaemia), hypoalbuminaemia, raised concentrations of urea and creatinine, and hypergammaglobulinaemia.1 2 Splenomegaly develops in some patients with pancytopenia.1 Biochemical markers of liver fibrosis (pro-collagen peptides type III and IV, the P1 fragment of laminin, hyaluronic acid, fibrosin, tumour necrosis factor αR-II, and sICAM-1) measured in serum have potential to provide a highly sensitive and cost-effective method for assessment of schistosome induced fibrosis.18w55-w54 A biopsy of the liver may be necessary in some patients with co-infection (eg with hepatitis virus).1 Liver involvement in patients with schistosomiasis may be suggested by the characteristic appearance of the organ on abdominal imaging.1 2
Antibody detection can be useful in a few specific circumstances, but its application is limited.1 2 19 A positive serological test may be diagnostic in patients who are not excreting eggs, such as those with Katayama syndrome. Serological testing can be useful in field studies for defining regions of low level endemicity, where individual patients have low egg burdens, and may also be beneficial for determining whether infection has re-emerged in a region after an apparently successful control programme. It is important for diagnosis in travellers. Commercially available immunodiagnostic kits are less sensitive than multiple faecal examinations and less specific, owing to antibody cross-reactivity with antigens from other helminths.1 19w55-w57 Most techniques detect IgG, IgM, or IgE against soluble worm antigen or soluble egg antigen by enzyme-linked immunosorbent assay (ELISA), indirect haemagglutination, or immunofluorescence.1 2 A cercarial antigen ELISA equivalent to the soluble egg antigen assay has been developed for serodiagnosis of schistosomiasis.20
Detection of circulating adult worm or egg antigens with labelled monoclonal or polyclonal antibodies in serum, urine, or sputum in infected individuals is another promising technique that may eventually supersede traditional diagnostic methods.1 2 A commercially produced diagnostic test—the urine circulating cathodic antigen strip—is available for detection of schistosomiasis.21 Surveillance studies and cross sectional surveys have shown that circulating cathodic antigen may be useful for screening for both S haematobium and S mansoni infections in the field but, to date, seems not to have sufficient sensitivity and/or specificity for definitive diagnosis.w58 w59
How is schistosomiasis treated?
Praziquantel
Randomised controlled trials have shown that praziquantel, a pyrazinoisoquinoline derivative, is a safe and effective oral drug that is active against all schistosome species.22 23 The drug is absorbed well but undergoes extensive first pass hepatic clearance. It is secreted in breast milk and is metabolised by the liver, and its metabolites (which are inactive) are excreted in the urine. The drug acts within one hour of ingestion although its precise action on adult worms is unknown. Laboratory studies have shown that it causes tetanic contractions and tegumental vacuoles, which cause worms to detach from the walls of veins and die. Schistosome calcium ion channels have been indirectly identified as the molecular target of praziquantel. In animal models, the presence of host antibodies is critical for efficacy.1 2 22 23
Randomised controlled trials have also shown that the effective praziquantel dosage regimen is 60 mg/kg orally in divided doses over one day (3 x 20 mg/kg doses 4-hourly or 2 x 30 mg/kg either 4-hourly or 6-hourly) for S japonicum and S mekongi, and 40 mg/kg orally in divided doses over one day (2 x 20 mg/kg doses 4-hourly) for S mansoni, S haematobium, and S intercalatum.1 7 19 22 23 24 (table). However, a single 40 mg/kg dose is administered with 66-95% efficacy for epidemiological studies and population-based preventive chemotherapy control programmes.2w60 Efficacy of 95-100% can be achieved with re-treatment four to six weeks later25 and this second dose is advisable, especially if eosinophilia and a high antibody titre persist after primary treatment. Praziquantel has few side effects other than transient nausea, dizziness, rash, and pruritus, which are thought to be associated with the consequences of worm death rather than the drug itself.1 2 22 23 It can be used to treat young children (>4 years old) and pregnant women if breastfeeding is discontinued on the day of treatment and for the next 72 hours.8 In patients with concurrent schistosomiasis and Taenia solium cysticercosis, praziquantel can cause irreparable eye lesions owing to the death of Taenia parasites in the ocular region, and it may also induce seizures and/or cerebral infarction owing to the intense inflammatory reactions that can be initiated by the dying Taenia cysts.w61
Treatment and prophylaxis for schistosomiasis. Adapted from Ross et al8 with permission from Elsevier
| Use in special groups | ||||||
|---|---|---|---|---|---|---|
| Drug | Dosage regimen | Pregnancy | Breast feeding | Children | Main contraindication | Comments |
| Praziquantel | S haematobium, S mansoni, S intercalatum, 40 mg/kg per day, two doses a day by mouth; S japonicum, S mekongi 60 mg/kg per day, three doses a day by mouth | Category B: usually safe, but benefits must outweigh risk | Discontinue breast feeding on day of treatment for up to 72 hours | Safe for age >4; not established for age <4 | Hypersensitivity, ocular cysticercosis | Used to treat all schistosomes. Usually well tolerated. Caution while driving or performing other tasks requiring alertness on the day of treatment or the day after |
| Artesunate | S haematobium, S mansoni, S intercalatum, S japonicum, S mekongi, prophylaxis: 6 mg/kg every 2-4 weeks by mouth | No data, not recommended | No data, not recommended | Safe | Hypersensitivity | Prophylactic against S haematobium, S mansoni, S japonicum. Antischistosomula properties |
| Corticosteroids (prednisone) | Adult: 1.5-2.0 mg/kg per day by mouth for 3 weeks. Paediatric: 0.05-2.0 mg/kg per day, three doses a day by mouth | Category C: unknown effect, not recommended | Unknown effect, not recommended | Safe | Immunosuppressant | Used for treatment of Katayama syndrome (within 2 months of water contact) and treatment for sequelae of neuroschistosomiasis |
| Anticonvulsants | Consult neurologist | Category D: not recommended | Benefits must outweigh risk | Safe | Hypersensitivity | Treatment of seizures associated with neuroschistosomiasis |
Experimental laboratory studies in mice have indicated, somewhat controversially, that resistance to praziquantel may be emerging in Africa, where there has been heavy exposure to the drug, and where, worryingly, there are reports of S mansoni and S haematobium infections that are not responsive.1w62 w63 Laboratory evidence suggests that drug tolerant schistosome worms may have an altered tegumental architecture, which could limit the effectiveness of the drug. So far, however, patients in many communities have undergone multiple courses of treatment over a period of 10 or more years without demonstrable loss of efficacy. Because worm reproduction in the mammalian host is sexual and the generation time is relatively long, resistance is likely to take many years to become an important clinical and public health issue. Nevertheless, resistance against praziquantel in the future cannot be ruled out and research should continue on developing alternative drugs—such as 4-phenyl-1,2,5-oxadiazole-3-carbonitrile-2-oxide, a new compound that has been shown to inhibit a crucial parasite enzyme, thioredoxin glutathione reductase).26
Adjuvant treatment
Corticosteroids (for example, prednisone 1.5-2.0 mg/kg per day for three weeks) are used to treat Katayama syndrome within two months of freshwater contact8w55 w64 (table) and for the treatment of schistosomal encephalopathy during the oviposition (egg laying) stage.11 12 Corticosteroids and anticonvulsants may be needed as adjuvants to praziquantel in neuroschistosomiasis, which needs specialised care.1 Corticosteroids help to alleviate acute allergic reactions and prevent mass effects caused by excessive granulomatous inflammation in the central nervous system. Anticonvulsants are used to treat seizures associated with cerebral schistosomiasis but lifelong use is rarely indicated (table). Surgery should be preserved for particular patients, such as those with evidence of medullary compression and for those who deteriorate, despite clinical treatment.11 12 A ventriculoperitoneal shunt and corticosteroids are required to treat hydrocephalus and intracranial hypertension in cerebral schistosomiasis.11 12
Other antiparasitic agents
Other drugs used to treat schistosomiasis are oxamniquine for S mansoni and metrifonate for S haematobium, but neither is effective against S japonicum.1 2 A recent randomised, exploratory open label trial of mefloquine-artesunate showed promising efficacy against S haematobium and further investigation of this approach is warranted.27
Praziquantel cannot be used for chemoprophylaxis because of its short half-life (1-1.5 hours) and because it cannot kill schistosomula (migrating larvae) that are three to 21 days old. Artemether is effective against juvenile schistosomes during the first 21 days of infection in animals and humans28 and, if given every two weeks, should kill all immature schistosomula. It has been used as a chemoprophylactic in schistosomiasis endemic areas for those at high risk of infection, such as flood relief workers and fishermen in China (table).29 The doses required are lower than those for the treatment of malaria, but it is unlikely that artemether will be used routinely in regions where malaria is endemic because of the risk of selecting artemether resistant Plasmodium falciparum. Randomised controlled trials have shown that combination therapy with praziquantel plus artemether is safe and results in higher rates of worm reduction than praziquantel alone.28 29 However, a randomised, double blind, placebo controlled trial that evaluated combined chemotherapy for acute schistosomiasis japonica in China failed to show improved treatment efficacy compared with praziquantel alone.24 Standard treatment with praziquantel was also more effective than artesunate with sulfalene plus pyrimethamine in the treatment of children with S mansoni infection in western Kenya.30 It is unclear, therefore, whether artemether based combination therapy has a role in the treatment of schistosomiasis.31 w65
What are the future challenges?
The challenge for researchers who aim to improve the diagnosis and management of schistosomiasis will be to find a way to respond to environmental changesw2 and to the threat of praziquantel resistance. New diagnostic procedures that are simple, rapid, and able to diagnose light infections (such as simple dipstick tests and PCR-based assays) need further development, as do new drugs that act effectively on both adult and larval schistosomes, and vaccines that target either the human host or, in the case of S japonicum or S mekongi, the animal reservoir hosts.
An integrated approach to the management of schistosomiasis32 w66 that offers treatment alongside measures to reduce transmission by snail control (focal mollusciciding and environmental modification), health education and promotion, improved sanitation, and vaccination is the key to sustainable long term control of schistosomiasis.32
Additional educational resources
Introduction to schistosomiasis (www.path.cam.ac.uk/~schisto/schistosoma/index.html)—Outline from the Schistosomiasis Research Group, University of Cambridge
Health topics: schistosomiasis (www.who.int/topics/schistosomiasis/en)—Information from the World Health Organization
Parasites—schistosomiasis (www.cdc.gov/ncidod/dpd/parasites/schistosomiasis/factsht_schistosomiasis.htm)—Fact sheet from the US Centers for Disease Control and Prevention
Schistosomiasis (www.medicinenet.com/schistosomiasis/article.htm)—Information for patients from MedicineNet
A patient’s perspective
I am a 26 year old driver from Yueyang, China. One Sunday last summer, I drove to the Dongting Lake and fished and swam for 30 minutes. Twenty five days later, I developed a fever and cough and had a distended abdomen and diarrhoea. I was tired and had little appetite. On the third day of fever I attended a private hospital in Yueyang city. A chest x ray suggested a lung infection. I was treated for four days with antibiotics and intravenous drips, but my condition did not improve. At another local hospital, I was diagnosed with acute schistosomiasis. I returned to Yueyang to attend a special schistosomiasis hospital. Schistosome eggs were found in my stool and my blood reacted to substances in schistosome eggs. X rays showed fluid in my left lung, and my liver and spleen were enlarged. Acute schistosomiasis was confirmed. I was told all my problems were caused by Schistosoma japonicum and its eggs. I was prescribed a drug called praziquantel and took the tablets three times a day after meals, three pills each time, for six days. My fever was highest (41.5ºC) on the second day of my course of praziquantel. A special injection to lower my temperature was given to me and it worked well. I was discharged from hospital two days after I finished taking the drug. My stool, re-checked 10 and 20 days later, showed no more eggs. After three months, I feel well now.
Mr Yang, Yueyang, Hunan Province, People’s Republic of China
We thank Mimi Kersting and Simon Forsyth for their graphical support.
Contributors: D Gray, A Ross, Y Li and D McManus conceived and prepared the manuscript. D Gray and D McManus finalised the article.
Funding: The authors’ studies on schistosomiasis have received financial support from various sources including: the UNICEF/UNDP/World Bank/WHO Special Program for Research and Training in Tropical Diseases; the National Health and Medical Research Council of Australia; the Wellcome Trust (UK); the Sandler Foundation (USA); the Dana Foundation (USA); and the National Institute of Allergy and Infectious Diseases.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: all authors had financial support from the National Health and Medical Research Council of Australia for the submitted work, no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned, externally peer reviewed.
Cite this as: BMJ 2011;342:d2651
Related links
bmj.com/archive
Web Extra. Extra material supplied by the author
Web reference list
References
- 1.Ross AGP, Bartley PB, Sleigh AC, Olds GR, Li Y, Williams GM, McManus DP. Schistosomiasis. N Eng J Med 2002;346:1212-9. [DOI] [PubMed] [Google Scholar]
- 2.Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet 2006;368:1106-18. [DOI] [PubMed] [Google Scholar]
- 3.Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis 2006;6:411-25. [DOI] [PubMed] [Google Scholar]
- 4.King CH, Dickman K, Tisch DJ. Reassessment of the cost of chronic helminthic infection: a meta-analysis of disability-related outcomes in endemic schistosomiasis. Lancet 2005;365:561-9. [DOI] [PubMed] [Google Scholar]
- 5.King CH, Dangerfield-Cha M. The unacknowledged impact of chronic schistosomiasis. Chronic Illness 2008;4:65-79. [DOI] [PubMed] [Google Scholar]
- 6.Mas-Coma S, Valero MA, Bargues MD. Climate change effects on trematodiases, with emphasis on zoonotic fascioliasis and schistosomiasis. Vet Parasitol 2009;163:264-80 [DOI] [PubMed] [Google Scholar]
- 7.Leshem E, Meltzer E, Marva E, Schwartz E. Travel-related schistosomiasis acquired in Laos. Emerg Infect Dis 2009;15:1823-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross AG, Vickers D, Olds GR, Shah SM, McManus DP. Katayama syndrome. Lancet Infect Dis 2007;7:218-24. [DOI] [PubMed] [Google Scholar]
- 9.Wynn TA, Thompson RW, Cheever AW, Mentink-Kane MM. Immunopathogenesis of schistosomiasis. Immunol Rev 2004;201:156-67. [DOI] [PubMed] [Google Scholar]
- 10.Burke ML, Jones MK, Gobert GN, Li YS, Ellis MK, McManus DP. Immunopathogenesis of human schistosomiasis. Parasite Immunol 2009;31:163-76. [DOI] [PubMed] [Google Scholar]
- 11.Carod-Artal FJ. Neurological complications of Schistosoma infection. Trans R Soc Trop Med Hyg 2008;102:107-16. [DOI] [PubMed] [Google Scholar]
- 12.Ferrari TC. Involvement of the central nervous system in the schistosomiasis. Mem Inst Oswaldo Cruz 2004;99:59-62. [DOI] [PubMed] [Google Scholar]
- 13.McManus DP, Gray DJ, Li YS, Feng Z, Williams GM, Stewart D, et al. Schistosomiasis in the Peoples’ Republic of China: the era of the Three Gorges Dam. Clinic Microbiol Rev 2010;23:442-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz N, Chaves A, Pellegrino J. A simple device for quantitative stool thick-smear technique for schistosomiasis mansoni. Rev Inst Med Trop Sao Paulo 1972;14:397-400. [PubMed] [Google Scholar]
- 15.Oliveira LM, Santos HL, Gonçalves MM, Barreto MG, Peralta JM. Evaluation of polymerase chain reaction as an additional tool for the diagnosis of low-intensity Schistosoma mansoni infection. Diagn Microbiol Infect Dis 2010;68:416-21. [DOI] [PubMed] [Google Scholar]
- 16.Wichmann D, Panning M, Quack T, Kramme S, Burchard GD, Grevelding C, Drosten C. Diagnosing schistosomiasis by detection of cell-free parasite DNA in human plasma. PLoS Negl Trop Dis 2009;3:e422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gomes LI, Dos Santos Marques LH, Enk MJ, de Oliveira MC, Coelho PM, Rabello A. Development and evaluation of a sensitive PCR-ELISA system for detection of Schistosoma infection in feces. PLoS Negl Trop Dis 2010;4:e664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ellis MK, Li Y, Hou X, Chen H, McManus DP. sTNFR-II and sICAM-1 are associated with acute disease and hepatic inflammation in schistosomiasis japonica. Int J Parasitol 2008;38:717-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergquist R, Johansen MV, Utzinger J. Diagnostic dilemmas in helminthology: what tools to use and when? Trends Parasitol 2009;25:151-6. [DOI] [PubMed] [Google Scholar]
- 20.Chand MA, Chiodini PL, Doenhoff MJ. Development of a new assay for the diagnosis of schistosomiasis, using cercarial antigens. Trans R Soc Trop Med Hyg 2010;104:255-8. [DOI] [PubMed] [Google Scholar]
- 21.Stothard JR, Sousa-Figueiredo JC, Standley C, Van Dam GJ, Knopp S, Utzinger J, et al. An evaluation of urine-CCA strip test and fingerprick blood SEA-ELISA for detection of urinary schistosomiasis in schoolchildren in Zanzibar. Acta Trop 2009;111:64-70. [DOI] [PubMed] [Google Scholar]
- 22.Doenhoff MJ, Cioli D, Utzinger J. Praziquantel: mechanisms of action, resistance and new derivatives for schistosomiasis. Curr Opin Infect Dis 2008;21:659-67. [DOI] [PubMed] [Google Scholar]
- 23.Cioli D, Pica-Mattoccia L. Praziquantel. Parasitol Res 2003;90:S3-S9. [DOI] [PubMed] [Google Scholar]
- 24.Hou XY, McManus DP, Gray DJ, Balen J, Luo XS, He YK, et al. A randomized, double-blind, placebo-controlled trial of safety and efficacy of combined praziquantel and artemether treatment for acute schistosomiasis japonica in China. Bull World Health Organ 2008;86:788-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Sleigh AC, Williams GM, Ross AG, Forsyth SJ, Tanner M, McManus DP. Measuring exposure to Schistosoma japonicum in China. III. Activity diaries, snail and human infection, transmission ecology and options for control. Acta Trop 2000;75:279-89. [DOI] [PubMed] [Google Scholar]
- 26.Sayed AA, Simeonov A, Thomas CJ, Inglese J, Austin CP, Williams DL. Identification of oxadiazoles as new drug leads for the control of schistosomiasis Nat Med 2008;14:407-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keiser J, N’Guessan NA, Adoubryn KD, Silué KD, Vounatsou P, Hatz C, et al. Efficacy and safety of mefloquine, artesunate, mefloquine-artesunate, and praziquantel against Schistosoma haematobium: randomized, exploratory open-label trial. Clin Infect Dis 2010;50:1205-13. [DOI] [PubMed] [Google Scholar]
- 28.Utzinger J, Xiao SH, Tanner M, Keiser J. Artemisinins for schistosomiasis and beyond. Curr Opin Investig Drugs 2007;8:105-16. [PubMed] [Google Scholar]
- 29.Xiao SH. Development of antischistosomal drugs in China, with particular consideration to praziquantel and the artemesinins. Acta Trop 2005;96:153-67. [DOI] [PubMed] [Google Scholar]
- 30.Obonyo CO, Muok EM, Mwinzi PN. Efficacy of artesunate with sulfalene plus pyrimethamine versus praziquantel for treatment of Schistosoma mansoni in Kenyan children: an open-label randomised controlled trial. Lancet Infect Dis 2010;10:603-11. [DOI] [PubMed] [Google Scholar]
- 31.Utzinger J, Tanner M, Keiser J. ACTs for schistosomiasis: do they act? Lancet Infect Dis 2010;10:579-81. [DOI] [PubMed] [Google Scholar]
- 32.Gray DJ, McManus DP, Li YS, Williams GM, Bergquist R, Ross AG. Schistosomiasis elimination: lessons from the past guide the future. Lancet Infect Dis 2010;10:733-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web reference list