Summary
Inhalation injury greatly increases the incidence of respiratory failure and acute respiratory distress syndrome. It is also the cause of most early deaths in burn victims. The aim of this research is to study the incidence, early diagnosis, complications, and management of inhalation injury and to discuss the relationship between inhalation injury and death in burn patients. The study included 130 burn patients (61 male and 69 female) with inhalation injury admitted to Menoufiya University Hospital Burn Center & Chest Department (Egypt) from January 2008 to January 2010. It was found that the presence of inhalation injury, increasing burn size, and advancing age were all associated with increased mortality (p < 0.01). The incidence of inhalation injury was 46.3% (the 130 patients came from a total number of 281 burn victims). The overall mortality rate among patients with inhalation injury was 41.5% (54/130) compared with 7.2% (11/151) among patients without inhalation injury. These statistics clearly indicate that inhalation injury was an important factor for predicting burn patient mortality. Approximately 80% of fire-related deaths are due not to the airway burn injury itself but to the inhalation of toxic products, especially carbon monoxide and hydrogen cyanide gases. Inhalation injury is generally caused by thermal burns, and is mostly confined to the upper airways. Major airway, pulmonary, and systemic complications occur after inhalation injury, and this increases the incidence of mortality among burn patients.
Keywords: INHALATION INJURY, MORTALITY
Abstract
Les lésions causées par l’inhalation sont responsables d’un incrément élevé de la fréquence de l’insuffisance respiratoire et du syndrome de détresse respiratoire aiguë. EIles sont également la cause de la plupart des décès précoces des patients brûlés. Le but de cette recherche est d’étudier la fréquence, le diagnostic précoce, les complications et la gestion des lésions par inhalation et de discuter la relation entre ce type de lésion et la mortalité. L’étude a inclus 130 patients brûlés (61 hommes et 69 femmes) atteints de lésions par inhalation hospitalisés au Centre des Brulés et au Service Thoracique de l’Hôpital Universitaire Menoufiya, Egypt, de janvier 2008 à janvier 2010. Les Auteurs ont constaté que la présence de lésions par inhalation, l’extension élevée de la surface brulée et l’âge avancé constituent des facteurs qui sont tous associés à une mortalité augmentée (p < 0,01). La fréquence globale des lésions par inhalation était de 46,3% (les 130 patients provenaient d’un nombre total de 281 victimes de brûlures). Le taux global de mortalité chez les patients atteints de lésions par inhalation était de 41,5% (54/130) contre 7,2% (11/151) chez les patients sans lésions par inhalation. Ces statistiques indiquent clairement que les lésions par inhalation ont constitué un facteur important pour prédire la mortalité chez les patients brûlés. Environ 80% des décès liés au feu sont dus non pas à la simple brûlure des voies aériennes mais à l’inhalation des produits toxiques, et en particulier des gaz du monoxyde de carbone et d’acide cyanhydrique. Les lésions par inhalation, provoquées dans la majorité des cas par les brûlures thermiques et normalement limitées aux voies respiratoires supérieures, peuvent avoir des complications majeures aux voies aériennes, comme aussi après les complications pulmonaires et systémiques, et elles provoquent un incrément de la mortalité des patients brûlés.
Introduction
Inhalation injury is an acute respiratory tract insult caused by steam or toxic inhalants such as fumes, gases, and mists. Inhalation injury may occur without cutaneous burn injury, though the two injuries usually occur together. Despite increasing clinical interest in the problem of inhalation injury over the last few decades, the pathophysiology of inhalation injury remains poorly understood and there have been few improvements in treatment. Inhalation injury continues to be one of the most serious associated injuries complicating the care of thermally injured patients. Prevention or early diagnosis and treatment of associated life-threatening complications are necessary to decrease its associated morbidity and mortality: airway injury is present in up to one-third of patients with major burns, and the risk of concurrent pulmonary damage is directly related to the extent of the body surface area burned.1
Inhalation injury greatly increases the incidence of respiratory failure and acute respiratory distress syndrome. It is also the cause of most early deaths in burn victims. The mortality rate following smoke inhalation ranges from 45 to 78%.2 Shirani et al. estimated that the burn-related death rate is 20% higher in patients with combined inhalation injury and cutaneous burns than in those with cutaneous burns alone.3
Smoke inhalation remains a serious and life-threatening problem. The heat generated during combustion can cause significant thermal injury to the upper airways. Particulate matter produced during combustion (soot) can mechanically clog and irritate the airways, causing reflex bronchoconstriction. The noxious asphyxiant gases released during thermal decomposition include carbon monoxide and hydrogen cyanide. Other by-products produced by the combustion of furniture and cotton (aldehydes) or rubber and plastics (chlorine gas, ammonia, hydrocarbons, various acids, ketones) also cause injury.4
Aim of the work
The aim of our research was to study the incidence, early diagnosis, complications, and management of inhalation injury and to discuss the relationship between inhalation injury and death in burn patients.
Patients and methods
This study includes all burn patients with inhalation injury admitted to Menoufiya Burn Unit, Plastic Surgery Department and Chest Department from January 2008 to January 2010. Each patient was subjected to the following procedures:
1. History taking
The patient’s name, age, sex, and past history of illness, chronic diseases or congenital diseases were recorded. Age is a valuable factor in forming a prognosis, such as in the case of very young or very old patients, in whom the prognosis is poor. The patients’ sex is important as females are more exposed to burns. Chronic diseases such as diabetes mellitus, ischaemic heart disease, or bronchial asthma can increase the mortality rate if associated with burns.
2. General examination
We measured vital signs at the time of admission (blood pressure, pulse rate, temperature) - blood pressure and pulse rate in order to know the degree of hypovolaemia and as a base line for the progress of fluid intake (whether enough or insufficient) and the level of consciousness to determine the degree of hypoxaemia.
3. Evaluation and assessment of inhalation injury
We suspect smoke inhalation injury in anyone who was trapped in a confined space or who lost consciousness during a fire, especially in the presence of large quantities of heavy smoke. Clinical manifestations vary among victims, depending on their susceptibility to injury and degree of exposure. Injury may be limited to the upper airways (e.g. nasopharyngeal irritation, hoarseness, stridor, cough) or may extend distally with tracheobronchial and alveolar destruction (e.g. dyspnoea, chest discomfort, haemoptysis). Inhalation injury is likely in the presence of facial and upper cervical burns, singed eyebrows and nasal vibrissae, bronchial breath sounds, wheezing, rales, cyanosis, and carbonaceous sputum (Figs. 1,2,3,4).
Fig. 1. Burned male patient with inhalation injury at moment of admission. Family used oil to deal with burn.
Fig. 2. Child with suspected inhalation injury with eyes closed because of severe face and lip oedema.
Fig. 3. Deep burn in face. History of entrapment in closed space, soot around mouth. Patient drowsy, face and lip oedema.
Fig. 4. Very deep burn in face, soot around mouth.
We assessed the extent of the burns and the degree of hypoxaemia in patients presenting with inhalation injury. Patients at low risk of injury and with no clinical symptoms can usually be observed for 4-12 h and then discharged, with close follow-up and instructions to return if symptomatic.
a. Investigations
In all patients admitted to our Department with clinically suspected inhalation injury, arterial blood gas analysis was a fundamental diagnostic test that was performed serially. Arterial hypoxaemia and reduced oxyhaemoglobin saturation (SaO2) accompany smoke inhalation, and the presence of hypoxaemia is therefore an indicator of inhalation injury, until it is proved otherwise. Initial measurement of PaO2 is thus an insensitive indicator. It was found that the onset of hypoxaemia could be delayed as much as 48 h in spite of the absence of clinical or X-ray findings of inhalation injury.
b. Chest X-ray
We performed serial chest X-rays in patients with suspected inhalation injury. Chest X-rays taken on the day of injury were unreliable as a means of determining pulmonary injury by smoke inhalation. However, we performed them on admission because they serve as a baseline for subsequent radiographs.
The chest X-rays were used in the follow-up of patients for the detection of atelectasis and more or less extensive peribronchial cuffing or oedema.
In our Department we performed X-rays for the detection of complications of several therapeutic interventions (e.g. endotracheal intubation, intravenous catheterization, and central venous line replacement).
c. Respiratory function tests
We used respiratory function tests as a bedside procedure for the early detection and quantitation of inhalation injury. These tests demonstrate the presence of airway obstruction.
d. Fiberoptic bronchoscopy
Fiberoptic bronchoscopy provides direct information about the entire respiratory system. In addition to its diagnostic functions, bronchoscopy has important therapeutic and investigative applications and is used to determine the severity of inhalation injury. The following grading was used:
Grade I: no laryngeal oedema
Grade II: minimal laryngeal oedema and erythema
Grade III: slight tracheal mucosal oedema and erythema
Grade IV: moderate tracheal mucosal oedema and erythema
Grade V: severe tracheal oedema and erythema
4. First aid and early management
This started when burn patients with inhalation injury came to our emergency room, where we performed first aid as follows:
Airways: we ensured patent airways.
Breathing: we checked for upper airway compromise, difficult breathing, stridor, and cough. We administered 100% oxygen because of the possibility of carbon monoxide inhalation in fires.
Circulation: patients were admitted to our burns unit according to our admission policy. When a patient arrives in the burns unit, there are two main problems. The first is severe pain, which may lead to neurogenic shock, and the second is fluid loss, which may lead to hypovolaemic shock.
The patient starts his journey of treatment from the dressing-room, where the dressing-room doctors and nurse start dressing him. We put the patient on a trolley in order to place him in a water container for the removal of dead skin and aspiration of bullae. We then paint the patient with Dermazine (silver sulphadiazine). During dressing, a venous line (cannula) is inserted in the patient and fluid therapy is started with 500 cc Ringer’s acetate; we also give the patient an analgesic. The patient is then weighed and the burn percentage is estimated for the purposes of fluid therapy with the Evans formula: 2 cc × body weight (kg) × burn percentage. If the burn more than 20% in children or more than 25% in adults, a urine catheter is inserted to record urine output, which must be 1 cc/kg body weight/h for adequate perfusion and fluid resuscitation.
In major burns, i.e. over 50% total body surface area (TBSA), we insert a central venous line (Swan-Ganz catheter) for continuous measurement of central venous pressure. We assess the patient for the presence of inhalation injury; if the patient is suspected of having inhalation injury a 100% oxygen mask is applied, followed by nebulized heparin.
5. Definitive treatment:
-
a. Fluid resuscitation
Fluid resuscitation: our unit follows the Evans formula (2 cc/kg/% burn lactated Ringer’s) and the patient is given a maintenance dose as 5% glucose. All fluids should be warm to avoid hypothermia.
-
b. Dressing
Dressing of the patient was performed twice daily by the open method with micronized silver sulphadiazine in a hydrophilic base (Dermazine) after hydrotherapy.
-
c. Medical treatment
Any patient with suspected inhalation injury received humidified oxygen. We used high-oxygen flow rates and a tight-sealed non-rebreathing-type face mask, which facilitated delivery of high levels of supplemental oxygen, thus helping to reverse the oxygenation defect created by ventilation-perfusion mismatch. The inhaled oxygen also helped in the displacement of CO from haemoglobin, decreasing the half-life of carboxyhaemoglobin from 4-6 h in room air to 40-60 min in 100% FiO2. It is recommended that oxygen therapy should be continued until acidosis is corrected, the carboxyhaemoglobin levels have fallen below 15%, and the neurological symptoms have ceased, which typically takes several hours.
We use the nebulized Farcolin bronchodilator because it relaxes bronchial smooth muscle by action on ß2 receptors, with little effect on cardiac muscle contractility. We give the following dose: adults (nebulizer), dilute 0.5 ml (2.5 mg) 0.5% inhalation solution in 1-2.5 ml saline every 6 h and according to the patient’s symptoms; paediatric <5 yr (nebulizer): dilute 0.25-0.5 ml (1.25-2.5 mg) 0.5% inhalation solution in 1-2.5 ml saline every 6 h and according to the patient’s symptoms.
We use bronchodilators with special care in cases of hyperthyroidism, diabetes mellitus, and cardiovascular disorders; the adverse effects include tachycardia, palpitations, tremor, insomnia, nervousness, nausea, and headache.
We add heparin to the nebulizer, and this plays an important role in breaking the cast and debris formed as a result of inhalation injury.
Corticosteroids like Decardon and Soliocortif are added to the medications because of their important role as anti-inflammatory elements.
6. Surgical intervention
In the circumferentially burned chest we performed an escharotomy to prevent restriction of chest expansion during respiration. This was done by means of two lateral incisions in the chest and a mid-line incision in the chest wall and two parallel incisions.
Tracheostomy was performed in patients with severe inhalation injury and airway obstruction in whom intubation was difficult.
Results
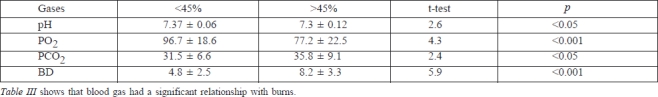
This study considered 130 burn patients (61 male, 69 female with inhalation injury admitted to Menoufiya University Hospital Burn Center and Chest Department from January 2008 to January 2010 (Tables I, II, III).
Table I. Mortality rate of patients with and without inhalation injury.
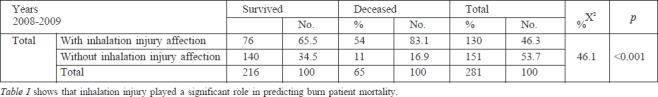
Table II. Mortality of patients with inhalation injury in relation to age.
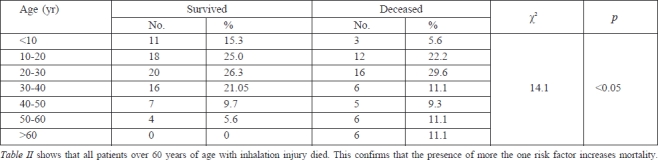
Table III. Blood gases of burn patients with inhalation injury in relation to burns percentage.
Discussion
Over the past 20 years, there has been remarkable improvement in the chances of survival of patients treated in burn centres. A simple, accurate system for objectively estimating the probability of death would be useful in counselling patients and making medical decisions. This remarkable success can be attributed to a number of therapeutic developments, including vigorous fluid resuscitation, the early excision of burn wounds, advances in critical care and nutrition, powerful topical and systemic antibiotics, and the evolution of specialized, multidisciplinary burn centres. It is over two decades since the first paper on inhalation injury was published.5 In an article published the following year it was reported that inhalation injury was an important factory - and possibly the primary factor - responsible for mortality in thermally injured patients.6 Although that may still be true today, many new things have been learned that have reduced the morbidity and mortality of burn patients who have sustained a concomitant inhalation injury.7 While some studies have reported that little progress has been made in reducing mortality associated with inhalation injury,8 others have noted significant progress,7 with improved techniques for ventilating patients,9 more aggressive fluid therapy, and better techniques for trachea bronchial toilet. Better understanding of the pathophysiology caused by cutaneous burns and smoke to the lung will lead to even further advances in the treatment of such lesions.10
The most commonly used predictors of mortality in burns are age, burn size, and inhalation injury. In the past, burns in over 80% TBSA that were mostly full-thickness were often considered fatal, especially in children and the elderly. In the past 15 years, advances in burn treatment have increased the survival rates of patients treated in specialized burns centres, while the following are significant predictors of increased mortality: larger burn size, the presence of inhalation injury, delayed intravenous access, lower admission haematocrit, lower base deficit on admission, higher serum osmolarity on arrival in hospital, sepsis, necessity of inotropic support, platelet count < 20,000, and ventilator dependency during the hospital course. It has been found that the patients most likely to die are the very young, those with limited donor sites, those who have inhalation injury, those with delayed resuscitation, and those with burn-associated sepsis or multi-organ failure.11
We conducted a review of all 130 burned patients with inhalation injury admitted from 2008 to 2010 to Menoufiya Burn Center, General Surgery Department, in Menoufiya University Hospital (Egypt).
Our study found that the presence of inhalation injury, increased burn size, and advanced age were all associated with increased mortality (p < 0.01). The incidence of inhalation injury in our study was 46.3% (130 patients out of 281 were identified as having inhalation injury). Overall mortality in patients with inhalation injury was 41.5% (54 out of 130) compared with 7.2% (11 out of 151) for those without inhalation injury. These statistical data clearly indicate that inhalation injury is an important factor in burn patient mortality prediction.
A study performed in Tokyo, Japan, to evaluate the impact of inhalation injury on burn patient mortality showed that between 1984 and 2002, of the 5560 patients admitted to 13 burn facilities of the Tokyo Burn Unit Association, 1690 patients (30.4%) had experienced inhalation injury. The overall in-hospital mortality rate of patients with inhalation injury was higher than that of those without inhalation injury (33.6% versus 8.1%), which is close to the ratio of 2.3 found in our study. It was found in the study that the results of the multivariate analysis indicated that inhalation injury, full- and partial-thickness burn size, and age were independent predictors of outcome (relative risk, 2.58 [2.03-3.29], 1.10 [1.09-1.11], 1.06 [1.06- 1.07], 1.05 [1.05-1.06], respectively). The authors concluded that inhalation injury was the most important predictor of overall mortality among burn patients in Tokyo.12
In a study conducted in Kansas University Medical Center, Burnett Burn Center, Kansas City, Kansas, USA, a retrospective review considered all patients aged yr 75 or older (n = 201) admitted to a university-based burn centre between 1972 and 2000. The variables examined were age, sex, TBSA, the Abbreviated Burn Severity Index, inhalation injury, time from burn to operative intervention, the number of surgical procedures, the number of premorbid conditions, and mortality. Mortality significantly increased with inhalation injury (p < 0.01). As we also we found in our study, the risk of fatality increased by 400% with inhalation injury.13
In a study of 710 burn patients in a Spanish burns centre it was found that the mortality rate among burn patients with inhalation injury was 66%.14
A retrospective study analysing 5264 patients treated in the burns centre at Gulhane Military Medical Academy in Turkey from 1 January 1986 to 31 December 1995 found that 134 of them presented inhalation injury, of whom 82% died.15 Our study found that 83.1% of burn patients with inhalation injury died. Three risk factors for death were identified: age over 60 years, more than 40% TBSA burned, and inhalation injury. The mortality formula they developed predicts 0.3%, 3%, 33%, or approximately 90% mortality, depending on whether zero, one, two, or three risk factors are present. The results of the prospective test of the formula were similar. A large increase in the proportion of patients who chose not to be resuscitated complicated comparisons of mortality over time.13
In another study the outcome of 1385 patients admitted to a burns unit over a 20-yr period was evaluated in relation to the presence of three major risk factors for death: age 60 years or over, total burned surface area 40% or more, and the presence of inhalation injury. Mortality was respectively 9.9%, 48.0%, and 90.5%, and it was found that nearly all the patients who died had at least one risk factor present. In the presence of three risk factors the prognosis following burns was particularly compromised.16
Our study found an overall burn patient mortality of 23.13% (65 out of 281).
In a study of all patients admitted to the Burns Unit in Alexandria Main University Hospital, Egypt, over a 1- year period (1999), the mortality rate was 33%.17
A retrospective analysis of 435 consecutive admissions to a regional burns unit in Saudia Arabia, over an 8-year period, found a case fatality rate 7.4%.18
The above-mentioned retrospective study analysing 5264 patients treated at Gulhane Military Medical Academy found an overall in-patient mortality rate of 18.2%.15
An analysis of mortality rates and related factors in Spanish burn centres, based on 710 patients treated between 1985 and 1988, found an overall mortality rate of 6.6%.14
The marked difference in mortality rate between this centre and our own burns centre is due to the fact that the average burn size was 14% TBSA in the Spanish centre.
Between 20 February 1987 and 13 July 1990, 844 patients were admitted to the Grady Memorial Hospital Burn Unit. The mortality rate was 8.5%.19 Half of the burns covered less than 10% TBSA, which explains the low mortality compared with that of our centre.
Any measure of outcome in a group of burn patients is useless and misleading unless the severity of injury is standardized. For many years, it was accepted that the extent of burn and the age of the patient were the two most important determinants of mortality probability in burn patients. It is now recognized that smoke inhalation is an important risk factor that must be included in the computation of mortality probability.
Inhalation injury greatly increases the incidence of respiratory failure and acute respiratory distress syndrome. It is also the cause of most early deaths in burn victims. The mortality rate following smoke inhalation ranges from 45% to 78%.2
Conclusions
Approximately 80% of fire-related deaths are due not to the burn injury to the airway but to inhalation of toxic products, especially carbon monoxide and hydrogen cyanide gases. Inhalation injury is generally caused by thermal burns, mostly confined to the upper airways. Major airway, pulmonary, and systemic complications occur with inhalation injury, which increases the incidence burn patient mortality.
Early detection and management of inhalation-related injury are absolutely essential. We therefore make the following recommendations:
Administer 100% humidified oxygen by facemask to burn patients with inhalation injury, once they have been admitted.
Burn patients with inhalation injury require more fluid than those with cutaneous burn alone; urine output and central venous pressure should be monitored to assess urine output.
Encourage central feeding as soon as possible.
Chest physiotherapy and postural drainage are essential to clear airways of cellular debris and soot.
Encourage extubated patient with inhalation injury to cough and breathe deeply; if intubated, use gentle suction to remove mucous, debris, and sloughed epithelium.
References
- 1.Shusterman D.J. Clinical smoke inhalation injury: Systemic effects. Occup Med. 1993;8:469–503. [PubMed] [Google Scholar]
- 2.Heimbach D.M., Waeckerle J.F. Inhalation injuries. Ann Emerg Med. 1988;17:1316–1320. doi: 10.1016/s0196-0644(88)80357-3. [DOI] [PubMed] [Google Scholar]
- 3.Shirani K.Z., Pruitt B.A., Mason A.D. The influence of inhalation injury and pneumonia on burn mortality. Ann Surg. 1987;205:82–87. doi: 10.1097/00000658-198701000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lahn M., Sing W., Nazario S. et al. Increased blood lead levels in severe smoke inhalation. Am J Emerg Med. 2003;21:458–460. doi: 10.1016/s0735-6757(03)00105-0. [DOI] [PubMed] [Google Scholar]
- 5.Herndon D.N., Adams T. jr, Traber D.L. Inhalation injury and positive pressure ventilation in a sheep model. Circ Shock. 1984;12:107–113. [PubMed] [Google Scholar]
- 6.Herndon D.N., Thompson P.B., Traber D.L. Pulmonary injury in burned patients. Crit Core Clin. 1985;1:79–96. [PubMed] [Google Scholar]
- 7.Rue L.W., Cioffi W.G., Mason A.D. et al. Improved survival of burned patients with inhalation injury. Arch Surg. 1993;128:772–778. doi: 10.1001/archsurg.1993.01420190066009. [DOI] [PubMed] [Google Scholar]
- 8.Sobel J.B., Goldfarb I.W., Salter H. et al. Inhalation injury: A decade without progress. J Burn Care Rehabil. 1992;13:573–580. doi: 10.1097/00004630-199209000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Cioffi W.G., Rue L.W., Graves T.A. et al. Prophylactic use of highfrequency percussive ventilation in patients with inhalation injury. Ann Surg. 1991;2134:575–580. doi: 10.1097/00000658-199106000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herndon D.N., Traber D.L., Traber L.D. The effect of resuscitation on inhalation injury. Surgery. 1986;100:248–251. [PubMed] [Google Scholar]
- 11.Wolf S.E., Rose J.K., Desai M.H. et al. Mortality determinants in massive pediatric burns. An analysis of 103 children with > or = 80% TBSA burns (> or = 70% full-thickness). Ann Surg. 1997;225:554–565. doi: 10.1097/00000658-199705000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suzuki M., Aikawa N., Kobayashi K. et al. Prognostic implications of inhalation injury in burn patients in Tokyo. Burns. 2005;31:331–336. doi: 10.1016/j.burns.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Lionelli G.T., Pickus E.J., Beckum O.K. et al. A three-decade analysis of factors affecting burn mortality in the elderly. Burns. 2005;31:958–963. doi: 10.1016/j.burns.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Benito-Ruiz J., Navarro-Monzonis A., Baena-Montilla P. et al. An analysis of burn mortality: A report from a Spanish regional burn centre. Burns. 1991;17:201–204. doi: 10.1016/0305-4179(91)90104-o. [DOI] [PubMed] [Google Scholar]
- 15.Brusselaers N., Hoste E.A., Monstrey S. et al. Outcome and changes over time in survival following severe burns from 1985 to 2004. Intensive Care Med. 2005;31:1648–1653. doi: 10.1007/s00134-005-2819-6. [DOI] [PubMed] [Google Scholar]
- 16.Turegun M., Sengezer M., Selmanpakoglu N. et al. The last 10 years in a burn centre in Ankara, Turkey: An analysis of 5264 cases. Burns. 1997;23:584–590. doi: 10.1016/s0305-4179(97)00081-8. [DOI] [PubMed] [Google Scholar]
- 17.Attia A.F., Reda A.A., Mandil A.M. et al. Predictive models for mortality and length of hospital stay in an Egyptian burns centre. East Mediterr Health J. 2000;6:1055–1061. [PubMed] [Google Scholar]
- 18.Al-Shlash S., Warnasuriya N.D., Al-Shareef Z. et al. Eight years’ experience of a regional burns unit in Saudi Arabia: Clinical and epidemiological aspects. Burns. 1996;22:376–380. doi: 10.1016/0305-4179(95)00169-7. [DOI] [PubMed] [Google Scholar]
- 19.Renz B.M., Sherman R. The burn unit experience at Grady Memorial Hospital: 844 cases. J Burn Care Rehabil. 1992;13:426–436. doi: 10.1097/00004630-199207000-00008. [DOI] [PubMed] [Google Scholar]






