Summary
Objective. We conducted a prospective study to identify the direct hospitalization cost of managing major acute burns in Lagos, Nigeria, and to determine the factors that influence the cost. Method. All consecutive and consenting patients seen and managed for major burns at the National Orthopaedic Hospital, Igbobi, Lagos, between 1 June 2007 and 31 May 2008 were recruited for the study. A special form designed for the study was used to collect the necessary data. Results. Fifty-two patients were seen during the study period (27 males and 25 females). The ages ranged from 2 months to 69 yr with a mean of 25.4 ± 17.1 yr. The length of hospital stay ranged from 0.3-12 months (mean, 3.2 ± 3.1 months). The average daily cost of treating a patient was ₦ (naira) 8,855 (₦1000 = €4.44) and the average overall cost was ₦209,303.70, with the costs of wound dressings, hospital admission, and surgery constituting respectively 29.5%, 25.7%, and 19.1% of the total amount spent. Conclusion. The length of hospital stay was prolonged in many patients and management methods should be reviewed to reduce this. The cost of managing burns is prohibitive for an average Nigerian. Efforts should be intensified to prevent burn injury and a Special Health Insurance policy should be established to finance burns management.
Keywords: MAJOR BURNS, HOSPITALIZATION AND COST OF CARE, LAGOS, NIGERIA
Abstract
But. Le but de notre étude prospective était d’établir le coût direct de l’hospitalisation pour la gestion des grands brûlés aigus à Lagos, au Nigeria, et de déterminer les facteurs qui influent sur le coût. Méthode. Tous les patients atteints de graves brûlures et traités consécutivement à l’Hôpital National d’Orthopédie, à Igbobi, Lagos, entre le 1er juin 2007 et le 31 mai 2008, ont été recrutés pour l’étude. Un formulaire préparé spécialement pour l’étude a été utilisé pour recueillir les données nécessaires. Résultats. Nous avons considéré 52 patients au cours de la période d’étude (27 mâles et 25 femelles). L’âge des patients variait de 2 mois à 69 ans (moyenne, 25,4 ± 17,1 ans). La durée de l’hospitalisation variait de 0,3 à 12 mois (moyenne, 3,2 ± 3,1 mois). Le coût quotidien moyen des soins pour traiter un patient a été de ₦8.855 (₦1000 = €4,44) et le coût moyen global était de naira 209,303.70 ; les coûts respectifs des pansements, de l’hospitalisation et des procédures chirurgicales constituaient 29,5%, 25,7% et 19,1% du montant total dépensé. Conclusion. La durée de l’hospitalisation a été prolongée chez de nombreux patients et il faut donc trouver un système de gestion capable de la diminuer. Le coût de la gestion des brûlures est prohibitif pour les citoyens nigériens moyens. Il faudra intensifier tous les efforts pour prévenir les brûlures et créer une spéciale police d’assurance maladie pour financer la gestion des brûlures.
Introduction
Burns are among the most devastating injuries, with long-term effects including economic ramifications. Burns occur with high frequency in the developing countries.1-4
Burn disasters have recently taken on epidemic proportions in Nigeria.3 The main factors involved are infrastructural deficiencies, including irregular electric power supply, together with adulteration of petroleum products and vandalization of petroleum pipelines.5,6 Other factors are ignorance, poor domestic and industrial safety practices, and the high incidence of road traffic accidents.7
The mjuries result in profound morbidity and high mortality. 1,3,8,9 Morbidity has been shown to be as high as 50% in some studies,8 with mortality ranging from 4.6 to 29%.10
The nanagement of major burns involves hospital stay, the use of medications and consumables, and surgical procedures. 11 The out-patient follow-up requires multispecialist clinic visits for varying periods.12 All of these have cost implications.
Studies from all over the world have highlighted the financial costs of burn care, making it obvious that burns present a major financial challenge.6,13 Cost is thus a major factor in burns management. However, there is a paucity of studies on the economic implications of burn care in Nigeria, and the enormous economic burden placed on burn patients and their relations is not appreciated.
We conducted a study to identify the direct hospitalization costs of early and late care to burn patients. Factors that influence the cost of management were also studied. We hope that the outcome of the study may influence the funding of burn care centres and also serve as a job audit for clinicians showing practices that are beneficial and cost-effective for the patients.
Methods
A prospective study was carried out of burn patients at the National Orthopaedic Hospital, Igbobi, Lagos (NOHIL), Nigeria, between 1 June 2007 and 31 May 2008.
NOHIL is a tertiary institution devoted to burns management, plastic surgery, orthopaedics, and trauma. It is located in the south-west of Nigeria.
Patients
All consenting patients presenting with burn injuries and their complications during the study period who satisfied the following criteria were recruited for the study:
* patients presenting with acute burn injuries and surviving for more than 72 h post-injury;
* patients presenting with post-burn ulcers and other complications that required reconstructive procedures, pressure garments, or other scar modifying agents;
* patients still being followed-up after reconstructive surgery for post-burn complications.
Definitions14
Conservative management means that no surgical operation was performed and that patients were managed with drug intake and regular dressing changes. Operations involved invasive procedures performed in the operating rooms under anaesthesia.
Blood transfusion was defined as the intravenous infusion of plasma, red blood cell suspension, whole blood, and other blood products.
Length of hospital stay was defined as the number of days between the day of admission and hospital discharge or death.
The cost per case is defined as the total direct cost paid to the hospital or spent for procurement of drugs and materials during the course of the management of the patient from admission to hospital discharge or death.
Discharge criteria included the resolution of acute burn injury, absence of infection, wound healing >90% in conservatively treated patients, the healing of donor sites and skin grafts in patients subjected to surgery, and adequate analgesia.
Data collection
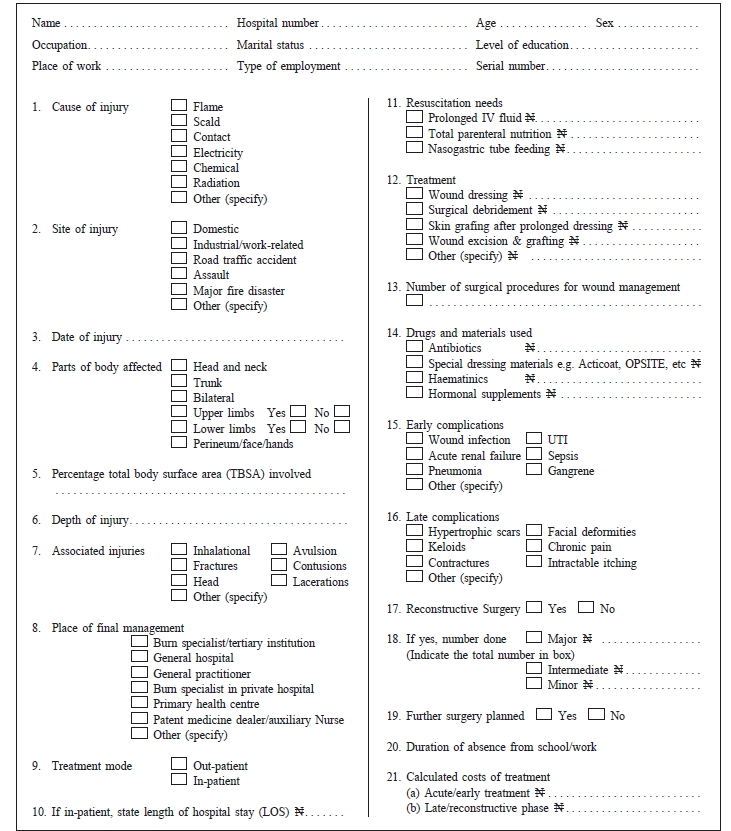
The study’s main instrument was a special form that reflected the various data of interest (Appendix). Consent was obtained from the Hospital Ethics Committee and the patients to carry out the study.
A special number-coded form was prepared and filled in for each patient during the course of treatment. Data regading cost were obtained from the relevant hospital departments and from the patients’ records.
Patient surveillance
Patient surveillance was started immediately after the patient was enrolled and continued throughout the period of the study.
Data analysis
The data of each patient were collected from the form at the conclusion of the study and stored in a computer. Analysis of the results was done with MS Excel and EPIINFO 2002 epidemiological and statistical software. The cases were classified into two groups: patients managed from the acute phase and those who were seen and managed later. The mean, standard deviation and frequency were calculated for the collected data.
Results
Demographics
A total of 52 patients were seen during the study period (27 males and 25 females, giving a male-to-female ratio of 1.1:1). The ages ranged from 2 months to 69 yr, with a mean (± standard deviation) of 25.4 ± 17.1 yr. Twenty-seven patients (51.9%) presented in the acute phase and 25 (48.1%) in the late phase. Twenty-nine patients (55.8%) were employed in the professions or as artisans and the remaining 44.2% had no earned income.
Aetiology of the burns
Flame was the commonest cause of burns (65.4%), followed by scalding (25.0%), chemicals (5.7%), and electricity (3.8%).
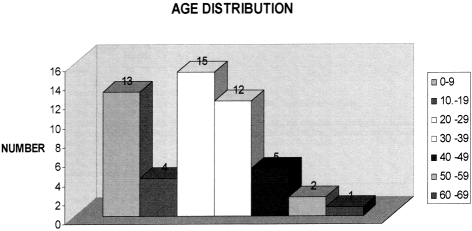
Distribution of patients by age
The age distribution of the patients is as shown in Fig. 1. The 20-29 yr age group was the most commonly affected, making up 28% of all the cases, followed by the 0-9 yr age group (23.1%).
Fig. 1. Patient age distribution.
Anatomical distribution of the injuries
Forty-three patients (83%) had burn injuries to the upper limbs. The trunk was affected in 65% of cases, the head and neck in 56%, and the lower limbs in 52%, while the perineum, face and hands were affected in 48%. Seven patients (13%) had all the regions involved.
Extent of burn injuries
The total body surface area involved ranged from 0.5 to 60% and the mean (± standard deviation) was 21.2 ± 14.3%. The injuries were mixed second- and third-degree thickness.
Associated injuries
Forty-seven patients (90.3%) sustained burns only, 5.7% had lacerations, and 4.0% had multiple injuries in addition to the burns.
Care providers during the acute phase management
Thirty patients (57.6%) were managed by burn specialists and 21 (40.4%) by general practitioners. One patient with chemical burns to the face and trunk was managed by an ophthalmologist. The majority (92.4%) of the patients were admitted into hospitals while the rest were managed on an out-patient basis.
Length of hospital day (LOS)
This ranged from 0.3 to 12 months with mean ± standard deviation of 3.2 ± 3.1 months. Thirty-nine (75%) patients were admitted for 0.3 to 5 months, 23.9% for 5.1- 10 months, and 1.9% for 12 months.
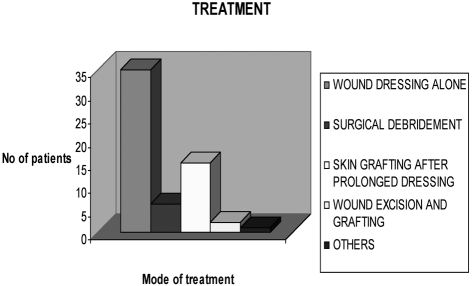
Modalities of burn wound management
Thirty-five patients (67.3%) were managed conservatively with continuous wound dressing alone until complete healing. Fourteen of these (26.9%) presented in the acute phase and 21 (40.4%) in the non-acute phase. Two (3.8%) had wound excision and early split-skin grafting, and 11 (21.2%) had split-skin grafting after contnuous wound dressing and spontaneous separation of the eschar (Fig. 2).
Fig. 2. Methods of treatment of cases seen in the acute phase.
All the 13 patients (25%) who had surgery for wound coverage were admitted during the acute phase.
Patients’ critical phase requirements
Thirty-five (67.3%) cases were managed routinely according to our Unit’s standard management protocol, i.e. intravenous fluid resurcitation with Ringer’s lactate infusion, analgesics, anti-tetanus immunoprophylaxis, prophylactic and later therapeutic antibiotic administrations as required, and regular wound dressing. Seventeen patients (32.7%) required prolonged intravenous fluid administration, 3.8% required nasogastric tube feeding, and 5.8% had total parenteral nutrition.
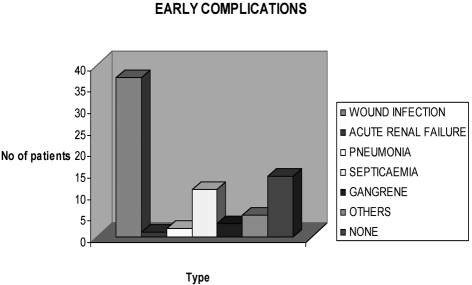
Complications developed by the patients
The early complications are shown in Fig. 3.
Fig. 3. Early complications in cases seen during the acute phase.
A total number of 16 patients (59.25%) out of those presenting in the acute phase had wound infections, resulting in an infection rate of 59.3 per 100 patients. Positive microbial cultures were obtained from the infected wounds from the fifth day of hospital admission, while all patients presenting in the non-acute phase had positive cultures on admission.
The late complications included hypertrophic scars in 30 patients (57.7%), contractures in 48.1%, and multiple complications in 48.0%.
Surgical procedures carried out
Most patients had multiple procedures. Thirty major operations, 29 intermediate, and 17 minor were carried out.
Direct financial implications of burns management
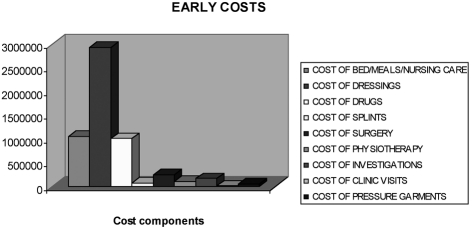
Direct cost of managing acute burns cases
A total of ₦5,665,000 was spent on the treatment of acute burn injuries, i.e. an average of ₦209,806 ± 77,397 for each of the 27 patients who were seen acutely, with a range of ₦14,470 to ₦2,206,950. The average cost per patient per day was ₦8,855. The breakdown of the expenses is shown in Fig. 4 and the cost per item in Table I.
Fig. 4. Distribution pattern of the costs of management of acute burns cases.
Table I. Cost in ₦ incurred per item in the management of acute burns cases.
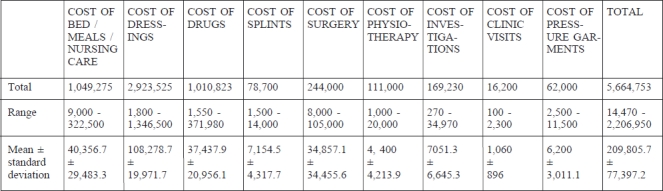
Fifty-two per cent was spent on wound dressings and 17.8% on drugs. Only 4.3% was spent on surgery.
Cost of the drugs used in the management of acute burn cases
The total cost of all antibiotics, including antimicrobial ointments, used in the management of the 27 patients in the early stage was ₦541,801, constituting 53.6% of the total cost of drugs (₦1,010,823). The total amount of all the intravenous fluids used was ₦187,000 (18.5% of the total cost), while haematinics cost ₦102,093 (10.1%). Analgesics and other drugs accounted for ₦70,757 (7%) and ₦109,168 (10.8%) respectively.
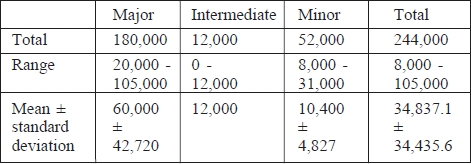
Cost of the surgical procedures carried out in acute burns cases
Table II shows the cost analysis for surgery in acute burns management. Seventy-four per cent of the early cost of surgery was for major procedures. These included escharectomies, fasciotomies, and tangential excisions with split-skin grafting. Intermediate and minor procedures accounted for 5% and 21% respectively.
Table II. Cost in ₦ of the surgical procedures carried out on acute burn patients.
Cost of nursing care and surgeon consultations
These were not quantifiable as these services were subsidized in the hospital where the study was conducted.
Late costs
For the 25 patients who presented late, a total of ₦5,219,000 was spent on the treatment of post-burn complications, an average of ₦208,762 ± 169,959, with a range of ₦13,050-738,940 (Fig. 5). Thirty-five per cent was spent on surgery. The cost per patient per day was not calculated as the particuliarities of post-burn reconstruction and rehabilitation of the patients studied involved a large number of out-patient activities.
Fig. 5. Distribution pattern of the cost in ₦ of managing burns in the non-acute phase.
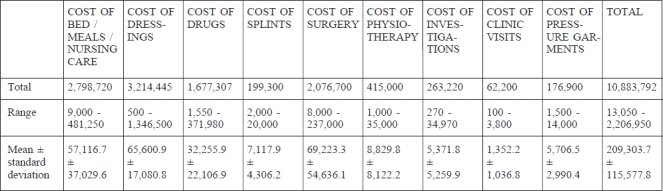
Total cost
A total of ₦10,884,000 was spent by the patients on the various modalities of treatment (Table III).
Table III. Total cost in ₦ of management of burns (acute and non-acute phases).
Discussion
In this study the younger age groups were found to be the most affected. This is consistent with the majority of previous studies.5,7-10,15,16 Small children are generally unaware of the dangers involved in their activities or in their environment, while older children are more active in their daily life and therefore more likely to be exposed to situations that could lead to burn injuries.
The two sexes were almost equally affected.. This is similar to the findings of Fadeyibi et al.14 in a previous study in the Lagos area. This finding is not unusual in an environment where the two sexes are almost equally involved in economy-related activities.
Flame was responsible for 63.5% of the injuries. Prolonged electric power outages have made the use of portable electricity generators very common. The equipment is often carelessly handled, causing fire disasters and burns in the process.14 Other factors that made flame accountable for many of the burns have been enumerated in previous studies from Nigeria.1,2,5,7-9
The average TBSA in the study was 21%, and 61.5% of the patients sustained third-degree burns. This is similar to findings from studies in other parts of Nigeria.2,5,7,10,16 The cost of burns treatment has been shown to correlate well with the severity of the injury.17 Extensive injuries are more difficult to manage. Deep wounds when managed conservatively take longer to heal. When such wounds are managed surgically, procedures may sometimes need to be staged.
Approximately 42% of the cases in the study were managed in the early stages by physicians not trained to manage major burns. Burns specialists are trained to anticipate, recognize, and appropriately treat burns and their complications as situations arise. The involvement of nonburn specialists may have been responsible for the morbidity and some of the complications that were found in this study. These may have contributed significantly to the cost.
The LOS in this study was quite high, with some patients staying in hospital for up to a year. The prolonged stay, during which time the patients paid various charges, contributed to management costs. Sixty-seven per cent of the patients were managed conservatively, waiting for the wounds to heal. Since 1947, when Cope et al.18 introduced early burn wound excision and autologous grafting, burn wound management has undergone radical changes. Thirddegree and some second-degree burns are now excised and skin-grafted as soon as the patients are haemodynamically stable.19-21 These procedures were found in one study to reduce LOS from 42 to 17 days in burns of equal size.22 The procedures decreased wound complications, sepsis, and LOS.20-22 Reduced LOS will also reduce the chances of nosocomial infections,14 thereby reducing morbidity and indirectly the cost of hospitalization.
The patients underwent multiple surgical procedures, the complicated nature of the injuries often requiring surgical procedures for appropriate management.14,20-22 These procedures contribute to the overall cost.
The average cost of the management of acutely injured burns patients in the study was ₦8,855 naira per day for an average total of ₦209,806 per patient. The cost of dressings, drugs, and hospital admission during the acute phase of management was considerable.
The local care of burn wounds has been found by various researchers to contribute significantly to the overall cost of burns management.23 Our finding is consistent with that of these previous studies. In the present study, local burn wound care involved regular cleansing with normal saline, application of silver-salt based topical antimicrobials, and coverage with dressings in layers. The wounds were extensive, hence many of these consumables were required at every wound cleansing and dressing session. Measures that can reduce the frequency of wound dressing may eventually reduce the overall cost of management.
The use of prophylactic antibiotics, pending the outcome of microbial studies on the wound swabs and biopsies, was normal practice during the study period. Our policy was based on previous experiences in the unit whereby most of the burn wounds were found to have been contaminated or infected at the time of presentation. The cost of medications, especially that of antibiotics, was proportionally high in this study. A nationwide standardized emergency medical/surgical referral system that ensures that emergency cases are appropriately revived, proper first-aid measures are commenced, and patients are taken to the appropriate healthcare facility in good time would reduce the incidence of wound infection, the need for prophylactic antibiotics, and overall drug use.
The cost of laboratory investigations during the treatment of the cases amounted to about 3.0% of the total cost of hospitalization and treatment. Good medical and surgical management of patients must be evidence-based. The various pathophysiological changes associated with major burns and the various complications that can develop during the treatment24 require adequate diagnostic supportive backup for the management team. The cost of investigating cases is offset by the reduction in morbidity and mortality.
The professional costs incurred due to nursing care services and repeated visits by the surgical teams were not available in this study. various routine and special procedures were carried out by the teams during the course of patient treatment. these included daily patient monitoring, the application of medication, and wound dressing. bedding and patient cleanliness were also taken care of or supervised by the nurses. other costs included regular consultation visits by the managing surgeon with his team to assess the patients’ state of health, prescribe for their needs, and perform any special procedures, including the securing of venous accesses, surgery, and the dressing of wounds, occasionally under sedation or general anaesthesia. all these procedures attract costs in health institutions that are not subsidized.
The cost of managing the cases seen in the non-acute phase of burn injury is shown in Fig. 5. Analysis of the cost implications in this set of cases is difficult and complex. Many of the procedures were performed at home by the patients and others had only indirect cost implications. However, the breakdown of the data showed that the cost of surgical procedures increased proportionally during the management of post-burn patients. Some of the procedures were carried out to correct the complications that developed during the acute phase management. Some such complications are avoidable if the patients are managed by burn specialists. Early wound excision with split-skin grafting and the use of splints, pressure garments, and physiotherapy could have made later reconstructive/aesthetic surgery unnecessary.
However, a comparative analysis of the costs of managing the two groups of patients seen in this study, i.e. those seen in the acute phase and those seen in the nonacute phase, could not be carried out. The patients seen in the non-acute phase were managed initially at different health care facilities with varying standards of patient management and non-standardized patient billing systems in most places. Records of the cost of management in these various centres were not available for most of the patients. The costs incurred during this study in this group were just part of the total costs of its entire management.
The total cost of managing the 52 patients was ₦10,884,000 i.e. an average of ₦209,303.70 per patient, while the cost of dressing materials used for the local wound care, of ward admission with bedding charges, and the fees for the various surgical procedures constituted respectively 29.5%, 25.7%, and 19.1% of the overall cost of the hospitalization and care of burns patients. Many burn victims in Nigeria are poor, the majority earning less than ₦500 a day, i.e. less than US$ 5, during the period of the study.24 An average Nigerian would thus have found it financially difficult to pay for the treatment of a patient with major burns.
The cost implications in this study can be compared with cost analyses from other studies globally. Kai-Yang et al.13 found that the average cost per case in Shanghai, China, was less than that in European and American studies. The Nigerian currency, the naira, was exchanging at the rate of ₦150 to US$ 1 and ₦230 naira to 1 British pound during the period of this study. Cases in this study included patients with extensive skin loss, wound sepsis, contractures, and various deformities, all of which required prolonged hospital admissions, intensive care, use of antibiotics, multiple surgeries, and various post-burn rehabilitation procedures. All of these have cost implications. The mean cost per case reported by Pressley et al.25 was $29,242 (₦4,386,300), and £1850 (₦425,500) by Griffith et al.26 for paediatric scalds. The costs of burn patient care are higher in Europe and America when these are compared with the findings in this study. However, the extent of the injuries and the types of management given to the patients in the American and British studies were not clearly stated. The reasons for the cost disparity between our studies and the other studies may include the modes of patient management, including the types of wound dressing materials used and the fact that health care services were subsidized by the government at the hospital where the present study was carried out. The LOS in this study was up to a year. This is considerable, when the indirect costs to the patients are considered.
The gold-mark for the management of deep burn wounds now is wound excision and split skin grafting.19,20 The advantages of this mode of wound management over the conservative approach have been mentioned. When wound dressings are required, various dressing materials, including biological dressings, biosynthetic materials, and varieties of nanocrystalline antimicrobial ointments, are used in Europe and America. These have been combined to reduce morbidity and mortality figures. All these are expensive and might have been responsible for the high cost in Europe and America. These materials were not used in the present study.
The limitations of the study include the fact that it was carried out in a single hospital. The management of patients in this hospital is subsidized, hence some facilities that should have been paid for were exempted. The cost implications may not be the same in private hospitals.
Conclusion
In conclusion, the study has shown that the direct hospitalization cost of the care of patients with acute burns may be considerable for the Nigerian patients but is however lower when compared on the global scale. The mode of patient management lags behind current international practice and should be improved in order to reduce the complications noted in the present study. Burn prevention measures should be intensified, more funds should be allocated to burn centres to upgrade the facilities and retrain personnel, and special health insurance policies should be put in place to finance burns management.
Appendix I
Special form for data collection on direct hospitalization cost of burns management in Lagos, Nigeria
References
- 1.Fadeyibi I.O., Jewo P.I., Saalu L.C. et al. Burn severity and postburn infertility in men. Burns. 2010;36:367–371. doi: 10.1016/j.burns.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Fadeyibi I.O., Omosebi D.T., Jewo P.I. et al. Mass burn disaster in Abule-Egba, Lagos, Nigeria from a petroleum pipeline explosion fire. Ann Burns Fire Disasters. 2009;22:97–103. [PMC free article] [PubMed] [Google Scholar]
- 3.Coker A.O., Fadeyibi I.O., Olugbile O.B. et al. A psychological morbidity study of patients with major burns seen at a Teaching Hospital in Lagos, Nigeria. Nigerian J Plastic Surgery. 2008;4:31–45. [Google Scholar]
- 4.Jeschke M.G., Chinks D., Finnerty C.C. et al. Pathophysiologic responses to severe burn injury. Ann Surgery. 2008;234:3–3. doi: 10.1097/SLA.0b013e3181856241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Datubo-Brown D.D., Kejeh B.M. Burn injuries in Port Harcourt. Burns. 1989;15:152–154. doi: 10.1016/0305-4179(89)90170-8. [DOI] [PubMed] [Google Scholar]
- 6.Onuba O., Udoidiok E. The problems and prevention of burns in developing countries. Burns. 1987;13:382–385. doi: 10.1016/0305-4179(87)90128-8. [DOI] [PubMed] [Google Scholar]
- 7.Sowemimo G.O.A. Burn injuries in Lagos. Burns. 1983;9:280–283. doi: 10.1016/0305-4179(83)90058-x. [DOI] [PubMed] [Google Scholar]
- 8.Gali B.M., Madziga A.G., Naaya H.U. Epidemiology of childhood burns in Maiduguri, North-Eastern Nigeria. Niger J Med. 2004;13:144–147. [PubMed] [Google Scholar]
- 9.Mabogunje O.A., Lawrie J.H. Burns in adults in Zaria. Burns. 1988;14:308–312. doi: 10.1016/0305-4179(88)90072-1. [DOI] [PubMed] [Google Scholar]
- 10.Mabogunje O.A., Khwaja M.S., Lawrie J.H. Childhood burns in Zaria, Nigeria. Burns. 1987;13:298–304. doi: 10.1016/0305-4179(87)90050-7. [DOI] [PubMed] [Google Scholar]
- 11.Eldad E., Stern Z., Sover H. et al. The cost of an extensive burn survival. Burns. 1993;19:235–238. doi: 10.1016/0305-4179(93)90157-4. [DOI] [PubMed] [Google Scholar]
- 12.Sheridan R.L., Hinson M.I., Liang M.H. et al. Long-term outcome of children surviving massive burns. JAMA. 2000;283:69–73. doi: 10.1001/jama.283.1.69. [DOI] [PubMed] [Google Scholar]
- 13.Kai-Yang L., Shi-Hui Z., Hong-Tai T. et al. The direct hospitalization costs of paediatric scalds: 2-year results of a prospective case series. Burns. 2009;35:738–745. doi: 10.1016/j.burns.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Fadeyibi J.O., Mustapha I.A., Ibrahim N.A. et al. Characteristics of paediatric burns seen at a tertiary center in a low-income country: A five-year (2004-2008) study. Burns. 2010 doi: 10.1016/j.burns.2010.09.015. ePub. [DOI] [PubMed] [Google Scholar]
- 15.Ahuja R.B., Battacharya S. Burns in the developing world and burns disastes. BMJ. 2004;329:447–449. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yiltok Y.T., Isamade E.S., Uba A.F. Outcome of burn patients managed in a general intensive care unit. Nig J Surg. 2005;11:1–4. [Google Scholar]
- 17.Wheeler J.R., Harrison R.V., Wolfe R.A. et al. The effects of burn severity and institutional differences on the costs of care. Med Care. 1983;21:1192–1203. doi: 10.1097/00005650-198312000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Cope O., Langhor J.L., Moore F.D. et al. Expeditious care of fullthickness burn wounds by surgical excision and grafting. Ann Surg. 1947;125:1–22. [PMC free article] [PubMed] [Google Scholar]
- 19.Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10:1103–1108. [PubMed] [Google Scholar]
- 20.Peck M.D., Heimbach D.M. Does early excision of burn wounds change the mortality? J Burn Care Rehabil. 1989;10:7–10. [PubMed] [Google Scholar]
- 21.Herndon D.N., Parks D.H. Comparison of serial debridement and auto grafting and early massive excision with cadaver skin overlay in the treatment of large burns in children. J Trauma. 1986;26:149–152. doi: 10.1097/00005373-198602000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Mzezewa S., Jonsson K., Aberg M. et al. A prospective study on the epidemiology of burns in patients admitted to the Harare burns unit. Burns. 1999;25:499–504. doi: 10.1016/s0305-4179(99)00041-8. [DOI] [PubMed] [Google Scholar]
- 23.Atiyeh B.S., Dham R., Kadry M. et al. Benefit cost analysis of moist exposed burn ointment. Burns. 2002;28:659–663. doi: 10.1016/s0305-4179(02)00075-x. [DOI] [PubMed] [Google Scholar]
- 24.Fadeyibi J.O., Jewo P.I., Opoola P. et al. Burns and fire disasters from leaking petroleum pipes in Lagos, Nigeria: An 8-year experience. Burns. 2011;37:145–152. doi: 10.1016/j.burns.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Pressley J.C., Trieu L., Kendig T. et al. National injury related hospitalization in children: Public versus private expenditures across preventable injury mechanisms. J Trauma. 2007;63(suppl. 3):510–519. doi: 10.1097/TA.0b013e31812f5ea7. [DOI] [PubMed] [Google Scholar]
- 26.Griffiths H.R., Thornton K.L., Clement C.M. et al. The cost of a hot drink scald. Burns. 2006;32:372–374. doi: 10.1016/j.burns.2005.10.025. [DOI] [PubMed] [Google Scholar]