Abstract
Human patient simulation (HPS) is used in health care education to enhance the transition from classroom learning to competent performance. It has been used frequently in nursing and medical schools and less often in pharmacy and other allied health professions. HPS is used to improve the development of pharmacy practice skills such as physical assessment, pharmacotherapy plan development, and monitoring plans. Engaging multiple health care disciplines in simulations enables participants to practice teamwork and communication skills that are essential in preventing errors and events of harm to patients. This article reviews current literature and use of simulation in pharmacy curricula for the development, enhancement, and assessment of pharmacy practice skills.
Keywords: human patient simulation, pharmacy practice, pharmacy curricula, teamwork, physical assessment
INTRODUCTION
The Accreditation Council for Pharmacy Education (ACPE) standards for the doctor of pharmacy (PharmD) degree state that “graduates must possess the basic knowledge, skills and abilities to practice pharmacy, independently, at the time of graduation.”1 Focus on communication skills, interprofessional teamwork, and patient safety in the healthcare setting has increased. The Lucian Leape Institute, in collaboration with the National Patient Safety Foundation, released a report that states “health professional education needs to be redesigned to equip students with the knowledge, skills, and attitudes they need to function safely and effectively in health care delivery in the 21st century.”2 The recommendations extend to all other health professionals related to integrating patient safety education and training throughout the entire curriculum. Pharmacists must develop effective practice skills that demonstrate the value of pharmacists to the healthcare team, regardless of the practice environment. Development of these skills early in pharmacy school is optimal to prepare students for advanced pharmacy practice experiences (APPEs), residency opportunities, and professional practice. Curricular change is difficult, but a paradigm shift is necessary.
Learning through classroom courses is only the first step for students in developing knowledge, experience, and competence. Repetition is one of the key factors in achieving competency, especially in practice skills, increasing accuracy, and building confidence in one's ability to perform the task well. Issenberg identified that the most important factor separating the elite performer from others is the amount of “deliberate practice” the individual obtains.3 Human patient simulation provides a standardized practice experience that closely mirrors actual patient care in that students experience healthcare team interactions, time pressure, and critical decision making, but in a safe environment with no potential for harm to the patient. This article reviews the literature on human patient simulation, focusing on its use in pharmacy education to provide students with opportunities for knowledge application and development of communication and teamwork skills.
ACCREDITATION AND HPS
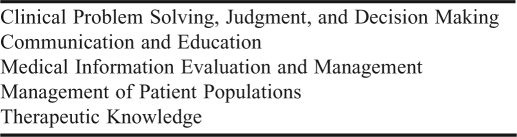
Guideline 1.3 of the ACPE's 2011 Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree states “The college or school's vision should include the development of pharmacy graduates who are trained with other health professionals to provide patient care services as a team.” Another similar recommendation promotes “development of interprofessional learning and collaborative practice in didactic and experiential education.” Guideline 14.5 discusses the option to use simulation as part of overall introductory pharmacy practice experiences (IPPEs). While not a requirement, simulation may be used to provide up to 20% (60 hours) of the student's required 300 hours of practice experience. For the purpose of satisfying IPPE expectations, ACPE defines simulation as the use of human patient simulation, medium fidelity manikins, standardized patients, standardized colleagues, role-play, and computer-based simulation. The use of interprofessional simulation experiences is encouraged. The American College of Clinical Pharmacy's (ACCP's) recommended competencies for a clinical pharmacist are grouped, with multiple components to each section (Table 1).4
Table 1.
American College of Clinical Pharmacy's Clinical Pharmacist Competency Groups
In June 2009, a task force was formed by the American Society of Health-System Pharmacists and ACPE and charged to describe competencies needed for entry-level practice in hospitals and health systems and to assist in identifying gaps in the readiness of graduating pharmacy students.5 The group used a survey tool that asked participants to rate each competency in relation to their expectation of new graduates as well as their perception of the importance of the competency in their practice setting. This was followed by a workshop in which the 150 participants shared when and how each competency was best taught (lecture courses, practice laboratory, or practice experiences). The task force identified 25 competencies, which were categorized into 4 groups: pharmacy systems, medication safety and quality, clinical applications, and professional practice. The recommendations included suggestions for placement in the curriculum, methods of assessment, and teaching methods for each of the 25 competencies. Many teaching and learning methods can be used to achieve the 25 competencies: patient cases, shadowing pharmacists or patient care teams, competitive internships, problem-based learning, mock pharmacy and therapeutics meetings, medication safety courses, drug usage evaluation projects, clinical skills days, root cause analyses, reflection, video clips, the use of manikins, and use of a simulation laboratory and group discussion.
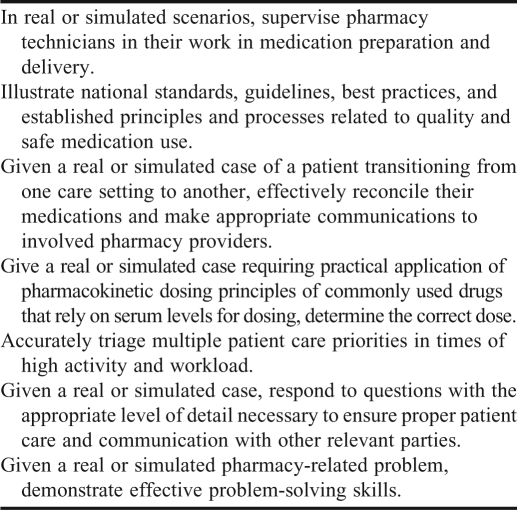
While many students obtain additional practice in clinical skills during postgraduate residencies or fellowships, the use of simulation in health care education is increasingly being used to provide and enhance students’ clinical skills prior to graduation. Of the 25 competencies defined, those that can be enhanced or achieved through simulation are defined in Table 2.
Table 2.
Competencies Defined as Amenable to Being Taught by Simulation
PREPARING STUDENTS FOR SIMULATION EXERCISES
Beaubien and Baker identified various levels of simulation (case studies, role plays, partial task trainers, and high fidelity human patient simulators) and provided guidelines and insight to maximize the use of simulation for training teamwork skills in health care.6 To decrease their apprehension, students or practitioners should complete an orientation exercise before participating in a simulation scenario. Repeated exposure to the simulation environment, including practicing basic physical assessment skills and observing the capabilities of the manikin (such as tongue swelling, seizure activity) will increase the learner's familiarity with the technology and decrease any apprehension about the human patient simulator and the simulation environment. In Mieure's study, which used simulation to teach advanced cardiac life support (ACLS) to pharmacy students, 90% of the students felt their clinical learning improved with HPS compared to standard lectures but 18% did not feel the simulation should be a graded experience because of the stress caused by having to perform.7 Anxiety can be lessened over time with increased familiarity with the simulator, the process, and the expectations. To lessen students’ anxiety, Tofil and colleagues8 offered an introduction to simulation course that focused on what to expect during the simulation visit. This kind of early exposure to the simulator through an exploration session is one method of familiarizing students with the capabilities and functions of the simulator and is critical to a successful simulation encounter.
DEBRIEFING FOR LEARNING
Key approaches to using simulation successfully include providing feedback and assessment through formal debriefing, repeating and practicing the same scenario, integrating simulation within the curriculum, having a controlled environment, and using multiple learning strategies. Debriefing can be the most important learning portion of the simulation experience. Fanning and Gaba discuss the objective of debriefing, how facilitators guide the reflection process and provide a safe learning environment, and the use of video review.9 A trained debriefer understands the need to guide learners to self-discover what went well and what could have been done better, as opposed to telling the learners this information. Reflecting on their own individual focus and decision-making process during the scenario helps the group learn how time pressure, unclear communication, conflict, and other factors increase the potential for error. Debriefing enables the participant to talk through their thought process and discover where they may have misunderstood or misinterpreted clinical signs or symptoms, jumped to an early conclusion, or otherwise erred in their thinking and decisions. Another important component of the debriefing is reviewing assessments conducted during the simulation.
SIMULATION TO TEACH TECHNICAL SKILLS, COMMUNICATION, AND TEAMWORK
Simulation, regardless of level of fidelity, can be used to increase students’ competence and confidence in both technical skills (eg, preparation and administration of medications, accurate blood pressure readings, administration of immunizations, etc) and non-technical skills, such as communication and teamwork behaviors. This section details some of the skills that can be taught, practiced, assessed, and mastered through HPS.
Product Preparation
In pharmacy, HPS can provide practice for developing competence in dosage calculations and product preparation. While students may practice calculations and medication preparation in a traditional classroom setting or skills laboratory, using simulation provides the realism of clinical practice such as time pressure and the need for interprofessional communication and teamwork to resolve discrepancies, for example, conflict resolution. Such a simulation can incorporate not only sterile product preparation, but application of knowledge of pharmacotherapeutics and patient assessment.
Mieure and colleauges conducted a study to provide students with experience applying pharmacotherapeutics (ACLS) knowledge; assessment and critical-thinking skills; and product preparation skills during a life-threatening cardiac event.7 Objectives of this workshop included preparation of medications for administration in a cardiac arrest situation (vasoactive and antiarrhythmic medications), calculation and recommendation of appropriate administration rates, and assessment of the patient's clinical status to anticipate potential interventions. In this study, the simulation session had a minimal impact on students’ grades, was 30 minutes long, and only 1 student per group performed preparation calculations. The student retention of knowledge gained during the HPS was not consistent with the perceived benefits of HPS, possibly because of the limited HPS experience or because a non-graded quiz was used as the assessment tool and administered several months after the experience. The authors suggested that repeated exposure to HPS should be used as in other studies. However, almost all students agreed or strongly agreed that the simulation experience enhanced their understanding of ACLS and the role of the pharmacist in a life-threatening event (99.2% and 98.3%, respectively). The majority also responded that they would like to see this type of experiential learning included in other sections of the pharmacy curriculum.
A study by Tofil and colleagues used an outpatient scenario and an inpatient scenario with an issue or concern designed to evoke assessment and treatment actions by the participants.8 The outpatient scenario involved an infant who developed acute respiratory distress requiring the administration of albuterol using a spacer and mask. The inpatient scenario was an infant presenting with supraventricular tachycardia (SVT) requiring the students to interpret the dysrhythmia and apply their knowledge of SVT and its treatment to prepare and administer adenosine. Although students’ scores on 2 components of a pre- and postintervention examination (signs and symptoms of pediatric respiratory distress and definitions related to the case) did not improve significantly, scores on the third section on applying knowledge did. Overall scores on the examination also improved significantly. The students liked the realism of the scenarios and being able to apply knowledge gained from classroom lectures to clinical decision-making.
A new advancement in HPS is drug recognition technology. This technology can be used to assess a pharmacy students’ ability to prepare and administer a drug correctly in an urgent care situation for example, as part of a health care team treating a patient who is experiencing a ventricular arrhythmia. The student is asked to calculate, prepare, and administer an amiodarone loading dose and infusion. Radiofrequency identification technology associated with the SimMan 3G (Laerdal)10 detects the drug, dose, and rate of administration, and automatically programs the patient to exhibit the appropriate physiologic response. The simulator also records this information, which allows the instructor to determine whether the student prepared the drug correctly and to debrief the group effectively after the scenario. This new technology will enable further studies related to the accuracy of students’ preparations, calculations, and administration of medications. Other simulation scenarios amenable to use of this technology include treatment of seizures, acute coronary syndrome, respiratory decompensation, and anaphylaxis.
Physical Assessment and Patient Monitoring
Proper training in patient assessment skills is foundational to the everyday practice of pharmacists. Collecting and evaluating patient information is necessary to make appropriate therapeutic treatment decisions. Spray and Parnapy11 found that 86% of 72 responding programs used a laboratory approach for student instruction in patient assessment, 70% used lectures, 11% used self-study, and 8% used a 3- to 7-day accelerated course (multiple methods could be selected). Of these programs that used only laboratory instruction, only 1 used patient simulation. The most common topics covered using simulation were pulmonary examination, followed by vital signs and cardiovascular assessment. Others include ear, eyes, nose, and throat (EENT), neurologic, gastrointestinal, and musculoskeletal assessment. An advantage of using a human patient simulator is the ability to provide students with standardized exposure to a diverse range of simulations such as skin rashes, extravasations, adverse drug reactions, drug-drug interactions, bowel sounds, and hemodynamics, as well as to infrequent or rare physiologic findings or events. Students can practice scenarios repeatedly to gain skill and confidence in their ability to recognize these events. Exposure to and practice of these types of scenarios in a simulated environment is much more realistic than reviewing a case on paper and much closer to what students will experience in professional practice. For example, exposing a student to a simulated patient who is developing an anaphylactic reaction (or drug-drug interaction) allows the student to experience the initial stress and inability to think or act quickly in a safe environment as opposed to an encounter with a standardized patient who could be harmed and whose clinical status may fluctuate from day to day.
After transition to a 6-year pharmacy curriculum in Japan, Tokunaga and colleagues12 introduced the use of HPS to assist pharmacy students with the acquisition of more extensive clinical skills, as pharmacists in Japan did not previously examine patients directly. After completing a simulation to improve their ability to monitor patients’ vital signs to identify drug treatment effects and adverse events, students’ understanding significantly improved (p<0.01) in the following areas: vital-sign monitoring devices, monitoring route of drug administration, rectal drug administration, and use of the spirometer/peak flowmeter and vital capacity measurement device.
Seybert and Barton assessed the use of simulation on students’ ability to complete accurate blood pressure measurements, demonstrate pharmacotherapy knowledge related to hypertensive therapy, and to assess student satisfaction with this method of teaching. Students were provided with the grading rubric, practiced blood pressure assessment for 15 minutes with the human patient simulator and given immediate feedback, and then completed a final practice skills evaluation for 10% of their final grade.13 The students’ clinical skills assessment of blood pressure significantly improved, with 21.5% of students obtaining an accurate reading at the first session and 97.6% of students at the third (final) session. A 5-question pre- and post-examination covering knowledge of the pharmacotherapy of hypertension demonstrated significant improvements in scoring (p < 0.05), as well as high levels of student satisfaction and increased competence. Based on the positive results of this study, the use of simulation was incorporated into a pharmacotherapy course.
In another study by Seybert and colleagues, simulation scenarios were used in a cardiovascular pharmacotherapy course to assess and develop clinical assessment, critical thinking, and problem-solving skills.14 The complexity of the simulations increased through the course, beginning with basic physical assessment skills, progressing to dysrhythmia recognition and treatment, and finally to a simulation in which the patient was experiencing a hypertensive crisis, acute myocardial infarction, atrial fibrillation, decompensated heart failure, or a ventricular dysrhythmia. Assessment included observation of the students’ communication skills, data collection skills, problem list prioritization, treatment and monitoring plan development, and documentation of the assessment and plan. Students’ scores on a 5-question pre- and post-simulation examination on dysrhythmia assessment and management all improved significantly (p < 0.05) with pre-simulation scores ranging between 4.5% and 24.7%, and post-simulation scores between 82% and 96.6%. There also was significant improvement in students’ scores on the myocardial infarction test questions relating to acute drug treatment and counseling points. Students confidence in their ability to care for patients improved significantly after completing the simulation (p < 0.05).
Critical Thinking Skills
Patient simulation has been used to assess and develop students’ critical-thinking skills. Event-based scenarios (a particular change in patient condition is designed to evoke certain reactions and behaviors by the participant) can be used to observe how a participant identifies changes in patient condition, selects and recommends a treatment, and monitors for adequate response to the therapy.15 Robinson and colleagues used HPS to expand the use of simulation beyond teaching physical assessment skills and acute patient care.16 They developed an ambulatory pharmacy simulation scenario to prepare pharmacy students for potential medical emergencies in the ambulatory pharmacy setting. In the scenario, a “patient” picking up his refills at the pharmacy developed symptoms of one of 5 acute conditions: acute chest pain, allergic reaction, asthma exacerbation, hypoglycemia, or stroke. The key learning objectives for students included rapid assessment, action, intervention, and appropriate follow-up instructions or referral. Ninety-three percent of the groups correctly identified the medical emergency, 89% initiated the appropriate treatment, and 87% of the students completed a competent SOAP (subjective, objective, assessment, plan) note. Of those who responded to a post-activity survey, 83% found this activity effective or very effective.
Two studies by Seybert describe the incorporation of HPS into a pharmacotherapy course and a dual-immersion elective acute care course. In the first, students were asked to assess an intensive-care unit patient, determine a primary diagnosis, and provide a pharmacotherapeutic plan with monitoring recommendations and SOAP note documentation. The average grade for the simulation was 88% and 93% of students felt that using simulation enabled them to apply knowledge learned in the course. The majority of students (66/94) felt very strongly that simulation training should be further incorporated into the pharmacy curriculum. In the second study, students viewed online self-study modules related to cardiology and critical care topics and then participated in simulations to develop and assess their ability to use critical-thinking skills and knowledge to solve problems related to cardiovascular disease. Students were evaluated in 4 areas: introduction to the patient, data collection and interpretation, pharmacotherapy and monitoring plan, and verbal presentation of the plan. Scores on 9 of 10 weekly posttests were significantly higher than those on pretests.
Communication and Teamwork Skills
Communication skills are critical to safe patient care, yet health professionals continue to experience difficulty with communication and clear and effective transfer of information from practitioner to practitioner. A large percentage of errors and events involve unclear, incomplete, or ambiguous communication. Ineffective communication has been identified as the most frequent root cause (65%-75%) in sentinel events (adverse events resulting in significant harm or death) reported to the Joint Commission.19 While there is some emphasis on developing these skills, the Lucian Leape Institute recommends more structured focus.
ACPE recommendations for interprofessional education and activities meshes nicely with efforts to train health care professionals to function effectively as a team, across the continuum of care. This will be easier to accomplish in some organizations than others, depending on the proximity to other health care professions schools and the willingness of leadership of each entity (ie, medical, pharmacy, nursing, and physician assistant schools) to reformat the curriculum to provide adequate time for these activities. Vyas and colleagues describe the use of HPS to supplement IPPEs in which fourth-year students participated in a 6-week high-fidelity patient simulation series where students worked with members of a patient care team (interdisciplinary) to care for patients with either asthma exacerbation, acute decompensated heart failure, and infective endocarditis with a subsequent anaphylactic reaction to the antibiotic.20 The objectives were to expose students to acute clinical situations that may not be presented during their IPPEs and to better equip them to serve effectively as a multidisciplinary team member. All student scores on a knowledge-based quiz demonstrated significant improvement post-simulation. Knowledge retention at 3 months was significantly higher among the students who participated in simulation than among those in the comparator group, and 76% of the students felt more confident providing recommendations to healthcare providers after the simulation session.
Fernandez used simulation in a pharmacotherapy course to teach interdisciplinary team skills.21 This study placed pharmacy students in a situation in which a patient with severely high blood pressure and a headache was being treated by a physician who ordered a non-formulary medication. The student team was expected to make a treatment recommendation to a nurse confederate as an order that included drug preparation and administration details. The pharmacy team was then expected to present their recommendation for treatment and monitoring to the patient's physician. This all was completed under time constraints and with a sense of urgency created by the patient repeatedly asking questions about how sick he was feeling. Over 98% of students agreed or strongly agreed that they learned material relevant to their current studies, and 90% felt they learned clinical patient care better using the HPS patient scenarios than through lectures.
Marken and colleagues found simulation to be an effective technique to teach interprofessional teams to engage in difficult conversations with patients.22 Using a simulated environment, interprofessional teams learned about the scope of each other's practice and how to effectively share information during the care process. The study used the Conscious Competence Learning model in which learners assess their competence at defined tasks at various points before and after a learning session. Participants’ scores improved for 6 of 9 skills related to patient conversations on partner violence and suicide. Potential barriers identified included the major time commitment for design and implementation, sustainability, and the lack of resources to replicate the program for all students.
Shrader and colleagues implemented a simulated interprofessional rounding experience in a clinical assessment course.23 Pharmacy, medical, and physician assistant students participated in this study with the following objectives: determine roles and responsibilities of an interprofessional healthcare team member in a simulated clinical environment, demonstrate effective teamwork skills in an interprofessional clinical environment, and deliver appropriate care to an unstable patient within an interprofessional healthcare team. Scenarios included a patient with gastrointestinal bleeding related to warfarin and a patient with digoxin toxicity and related cardiac arrhythmias. Each scenario had a medication error and drug interaction within the case. Overall, student satisfaction was high. In pre- and post-experience survey tools, there was significant improvement in items related to interprofessional attitudes and 3 of 4 items related to clinical confidence. This study using a multidisciplinary team working together may serve as a model for future simulation experiences.
Providing interprofessional experiences requires a coordinated effort and scheduling process. College and schools that are freestanding or not in close proximity to other disciplines may find it challenging to integrate interprofessional education and activities into their curriculum. Collaboration with current users of simulation in health care academia is highly recommended.
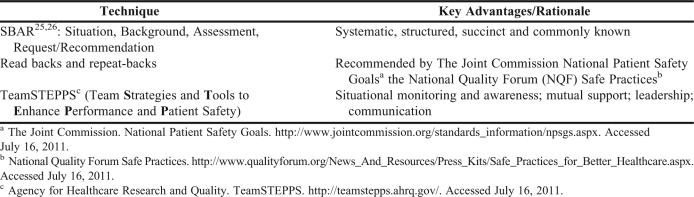
Examples of teamwork techniques amenable to use within simulation scenarios are included in Table 3. The systematic use of structured communication techniques such as SBAR (situation, background, assessment, and recommendation) is needed.24,25 The situation consists of a brief description of the current situation that is concerning such as a prescribed medication requires adjustment due to renal function or a severe drug-drug interaction exists. This is followed by the pertinent background information related to the patient. Presentation of a brief assessment of what the caller believes the problem to be is followed by a request or recommendation – usually to come examine the patient or request an order for testing or treatment.
Table 3.
Teamwork Techniques Amenable to Use Within Simulation Scenarios
“Read backs” and “repeat backs” are communication techniques recommended by The Joint Commission National Patient Safety Goals26 and the National Quality Forum Safe Practices.27 Repeating information back, especially for verbal orders or critical test results, provides an opportunity for the sender and receiver of information to clarify and confirm the information being exchanged.
Teamwork skills such as those outlined in team training programs such as TeamSTEPPS (Team Strategies and Tools to Enhance Performance and Patient Safety) are important components of any successful team intervention and should be included in any simulation scenario.28 TeamSTEPPS consists of 4 modules on various tools and techniques for optimizing teamwork in healthcare: effective leadership, situational monitoring and awareness, mutual support, and communication. Effective use of TeamSTEPPS within HPS should be observed and measured in each scenario.
Situational monitoring and awareness involves maintaining awareness of how an entire team is progressing towards a goal, which then enables early intervention and a change in care plan when needed. If a physician has requested epinephrine during a code and the nurse did not hear it, any team member is expected to call the information out to the nurse to confirm she has heard the order. Often a person is so focused on one task that they fail to see major changes right in front of them.
A team member may identify a colleague in need of help and offer assistance when that person may not have asked for help for fear of the perception that he or she could not get their workload completed effectively. This is also called mutual support. Combine situational awareness with mutual support within the team and the effectiveness, adaptability, and efficiency of the team improves significantly.
Effective leadership is an important characteristic of effective teams. Redirection of resources and the use of structured communication such as briefings prior to a procedure or debriefings after an event enable the team to have a common understanding of the upcoming procedure and to learn from situations in which improvement opportunities are identified. The use of a preoperative briefing tool and assessment of its effectiveness found that individuals overestimated their teamwork behaviors prior to implementation. Pre- and post-assessment mean scores demonstrated a significant improvement in teamwork behaviors.29
The last of the modules focuses on effective communication. The use of SBAR, call outs, and check backs are among the communication techniques reviewed within this module, all of which can be taught and practiced in teams. Pharmacy students and practitioners need to learn, understand, and practice these important teamwork concepts.
All of the safe behaviors and processes mentioned here can and should be included in all patient simulation scenarios. People tend to perceive they are more skilled than they actually are and the use of simulation provides an opportunity for self-recognition and practice to enable improvement in teamwork behaviors.
SUMMARY
Regulatory or accreditation bodies are encouraging the use of patient simulation in interprofessional education and clinical pharmacy practice activities. There is a broad range of simulation techniques that can be used, ranging from standardized patients to high-fidelity human patient simulators. While simulation typically has been used to develop participants’ skills in performing technical tasks, increasingly it is used as a setting in which to assess and develop teamwork and communication skills. While patient simulation scenarios can be time-consuming to develop, program, and execute, they provide a standardized experience for all students in a safe environment. Integration of patient simulation throughout the curriculum appears to be a key element to success, as practice over time allows students to develop expertise and competency.
Innovation and research continue to be needed in this area to define the benefits and lessons learned. There are many opportunities to continue to enhance pharmacy education with expansion of interprofessional simulation experiences, integration of safety science and simulation to sustain ongoing competencies, growth of existing faculty and trainees experience with this innovative teaching technique, and in situ simulations to encompass continuum of care.
There is a wealth of opportunity to augment learning and provide practice skill development for pharmacists by using simulation in a meaningful way. HPS is an ideal way for pharmacy educators to apply the Chinese proverb (popularized by Benjamin Franklin30): “Tell me and I forget. Teach me and I remember. Involve me and I learn.”
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf. Accessed September 21, 2011.
- 2.Lucian Leape Institute. Unmet needs: teaching physicians to provide safe patient care. National Patient Safety Foundation. http://www.npsf.org/download/LLI-Unmet-Needs-Report.pdf. Accessed September 21, 2011.
- 3.Issenberg SB, McGaghie WC, Petrusa ER, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–866. doi: 10.1001/jama.282.9.861. [DOI] [PubMed] [Google Scholar]
- 4.Burke JM, Miller WA, Spencer AP, et al. Clinical pharmacist competencies. Pharmacotherapy. 2008;28(6):806–815. doi: 10.1592/phco.28.6.806. [DOI] [PubMed] [Google Scholar]
- 5.ASHP-ACPE Task Force. Entry-level competencies needed for pharmacy practice in hospital and health-systems. http://www.ashp.org/DocLibrary/MemberCenter/Entry-level-Competencies.aspx. Accessed September 21, 2011.
- 6.Beaubien JM, Baker DP. The use of simulation for training teamwork skills in health care: how low can you go? Qual Saf Health Care. 2004;13(Suppl 1) doi: 10.1136/qshc.2004.009845. i51-i56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mieure KD, Vincent WR, Cox MR, et al. A high-fidelity simulation mannequin to introduce pharmacy students to Advanced Cardiovascular Life Support. Am J Pharm Educ. 2010;74(2):Article 22. doi: 10.5688/aj740222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tofil NM, Benner KW, Worthington MA, et al. Use of simulation to enhance learning in a pediatric elective. Am J Pharm Educ. 2010;74(2):Article 21. doi: 10.5688/aj740221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthcare. 2007;2(2):115–125. doi: 10.1097/SIH.0b013e3180315539. [DOI] [PubMed] [Google Scholar]
- 10.Laerdal product specifications. http://www.laerdal.com/us/doc/85/SimMan-3G. Accessed September 21, 2011.
- 11.Spray JW, Parnapy SA. Teaching patient assessment skills to Doctor of Pharmacy students: the TOPAS study. Am J Pharm Educ. 2007;71(4):Article 64. doi: 10.5688/aj710464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tokunaga J, Takamura N, Ogata K, et al. Vital sign monitoring using human patient simulators at pharmacy schools in Japan. Am J Pharm Educ. 2010;74(7):Article 132. doi: 10.5688/aj7407132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. Am J Pharm Educ. 2007;71(3):Article 48. doi: 10.5688/aj710348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seybert AL, Kobulinsky LR, McKaveney TP. Human patient simulation in a pharmacotherapy course. Am J Pharm Educ. 2008;72(2):Article 37. doi: 10.5688/aj720237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosen MA, Salas E, Wu TS, et al. Promoting teamwork: an event-based approach to simulation-based teamwork training for emergency medicine residents. Acad Emerg Med. 2008;15(11):1190–98. doi: 10.1111/j.1553-2712.2008.00180.x. [DOI] [PubMed] [Google Scholar]
- 16.Robinson JD, Bray BS, Willson MN, Weeks DL. Using human patient simulation to prepare student pharmacists to manage medical emergencies in an ambulatory setting. Am J Pharm Educ. 2011;71(1):Article 3. doi: 10.5688/ajpe7513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seybert AL, Laughlin KK, Benedict NJ, et al. Pharmacy student response to patient-simulation mannequins to teach performance-based pharmacotherapeutics. Am J Pharm Educ. 2006;70(3):Article 48. doi: 10.5688/aj700348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seybert AL, Kane-Gill SL. Elective course in acute care using online learning and patient simulation. Am J Pharm Educ. 2011;75(3):Article 54. doi: 10.5688/ajpe75354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Joint Commission. Improving America's Hospitals: The Joint Commission's annual report and quality and safety 2007. http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed September 21, 2011.
- 20.Vyas D, Wombwell E, Russel R, et al. High-Fidelity patient simulation series to supplement introductory pharmacy practice experiences. Am J Pharm Educ. 2010;74(9):Article l69. doi: 10.5688/aj7409169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernandez R, Parker D, Kalus JS, et al. Am J Pharm Educ. 2007;71(3):Article 51. doi: 10.5688/aj710351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marken PA, Zimmerman C, Kennedy C, et al. Human simulators and standardized pateints to teach difficult conversations to interprofessional health care teams. Am J Pharm Educ. 2010;74(7):Article 120. doi: 10.5688/aj7407120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shrader S, McRae L, King WM, Kern D. A simulated interprofessional rounding experience in a clinical assessment course. Am J Pharm Educ. 2011;75(4):Article 61. doi: 10.5688/ajpe75461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Joint Commission Journal on Quality and Safety. 2006;32(3):167–175. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- 25.Institute for Healthcare Improvement. http://www.ihi.org/knowledge/Pages/Tools/SBARTechniqueforCommunicationASituationalBriefingModel.aspx (Accessed October 23, 2011).
- 26.The Joint Commission. National Patient Safety Goals. http://www.jointcommission.org/standards_information/npsgs.aspx. Accessed September 21, 2011.
- 27.National Quality Forum Safe Practices. http://www.qualityforum.org/News_And_Resources/Press_Kits/Safe_Practices_for_Better_Healthcare.aspx. Accessed September 21, 2011.
- 28.Agency for Healthcare Research and Quality. TeamSTEPPS. http://teamstepps.ahrq.gov/. Accessed September 21, 2011. [DOI] [PubMed]
- 29.Paige JT, Aaron DL, Yang T, et al. Implementation of a preoperative briefing protocol improves accuracy of teamwork assessment in the operating room. Am Surgeon. 2008;74(9):817–823. [PubMed] [Google Scholar]
- 30.WisdomWord. Quotes by Benjamin Franklin. http://www.wisdomword.info/benjamin-franklin/ Accessed November 2, 2011.