Abstract
Renal coloboma syndrome (RCS), also called papillorenal syndrome, is an autosomal dominant condition characterized by optic nerve dysplasia and renal hypodysplasia. The eye anomalies consist of a wide and sometimes excavated dysplastic optic disc with the emergence of the retinal vessels from the periphery of the disc, frequently called optic nerve coloboma or morning glory anomaly. Associated findings may include a small corneal diameter, retinal coloboma, scleral staphyloma, optic nerve cyst and pigmentary macular dysplasia. The kidney abnormalities consist of small and abnormally formed kidneys known as renal hypodysplasia. Histologically, kidneys exhibit fewer than the normal number of glomeruli and these glomeruli are enlarged, a finding called oligomeganephronia. Consequences of the ocular malformations include decreased visual acuity and retinal detachment. Consequences of the renal hypodysplasia include hypertension, proteinuria and renal insufficiency that frequently progresses to end-stage kidney disease. High frequency hearing loss has been reported. Autosomal dominant mutations in PAX2 can be identified in nearly half of all patients with clinical findings suggestive of RCS, however, the majority of published cases have mutations in PAX2, thus biasing the known information about the phenotype.
In brief
Renal coloboma syndrome (RCS) is an autosomal dominant condition characterized by optic nerve dysplasia, often described as a coloboma and renal hypodysplasia.
Optic nerve malformations include optic nerve coloboma, optic nerve dysplasia, morning glory anomaly and cystic malformation of the optic nerve. Other eye malformations may include retinal coloboma, microphthalmia and macular dysplasia. Iris coloboma is not typically observed.
Renal and urinary tract malformations include renal hypodysplasia, vesicoureteral reflux and in severe cases, can present in utero with oligohydraminos, severe renal hypodysplasia or aplasia.
In 50% of patients who have characteristic eye and kidney malformations, mutations in one copy of PAX2 can be identified.
Isolated renal hypoplasia is an allelic condition. Nearly 10% of children with renal hypodysplasia will have point mutations in PAX2 and for some, on subsequent eye examination, subtle characteristic eye abnormalities may be identified.
Patients with characteristic eye abnormalities should undergo evaluation of both kidney structure and function.
Patients with renal hypodysplasia should undergo an ophthalmologic evaluation for eye findings characteristic of RCS.
Affected individuals require management by specialists in nephrology and ophthalmology.
Introduction
Renal coloboma syndrome (RCS) also known as papillorenal syndrome describes a condition consisting of optic nerve dysplasia (frequently described as a coloboma) and renal malformations (OMIM 120330). The inheritance pattern is autosomal dominant. The first clear description of RCS was made by Weaver et al1 in 1988 in two brothers who had end-stage kidney disease with interstitial nephritis and optic nerve colobomas. In 1995, the association of RCS with autosomal dominant mutations in the transcriptional regulator, PAX2, was made in a two generation family with optic nerve colobomas, vesicoureteral reflux and renal dysplasia.2, 3 Later that year, an autosomal dominant mutation in PAX2 was identified in the family described by Weaver et al4 confirming the association of PAX2 with RCS.
There are differences of opinion regarding the name of this condition between observers. RCS is the more common appellation in PubMed with 131 citations identified using the search term ‘Renal Coloboma syndrome' and 18 citations identified using the search term ‘Papillorenal syndrome' (PubMed search was performed November 26, 2010). The difference in nomenclature derives from differences in opinion regarding the description of the eye phenotype. To many ophthalmologists, the eye findings fall under the phenotype called ‘coloboma',5 meaning a condition that results from failure of the optic fissure to close during eye development. To others, the optic nerve findings should be described using the more general term, ‘dysplasia'6 with the preference for ‘papillorenal' syndrome where the word ‘papilla' refers to the optic papilla. In animal models, specifically mouse and zebrafish, Pax2/pax2a is expressed in the optic fissure; homozygous mutations lead to optic fissure closure defects and heterozygous mutations lead to similar defects as observed in human patients.7
Clinical Overview
Clinical findings of RCS occur primarily in the ocular and renal systems with reported auditory and central nervous system findings in individual cases. Organ specific findings correspond to tissue-specific PAX2 expression during early embryonic development; the eye, the inner ear, the midbrain/hindbrain, the spinal cord and the urogenital system.7, 8, 9, 10, 11
Ocular findings
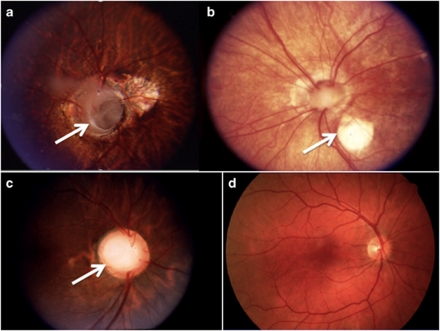
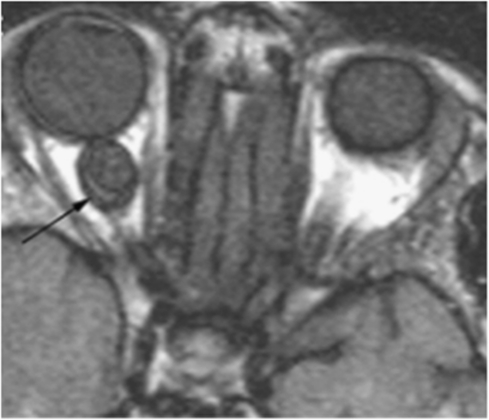
Eye findings reported in RCS have been reported in 85 patients who have mutations in PAX2.9, 12 The characteristic eye findings include an enlarged optic disc with blood vessels that emerge from the periphery of the disc (optic nerve head) rather than the center of the disc (Figure 1). The disc can be deeply excavated and dysplastic with grey gliotic tissue emerging from the center of the disc. The retinal blood vessels are tortuous and increased in number compared with normal. Reported named findings include optic nerve dysplasia, optic disc coloboma and morning glory anomaly. Associated abnormalities include retinal coloboma, scleral staphyloma, small corneal diameters, optic nerve cyst (Figure 2) and microphthalmia.12, 13, 14 Iris colobomas have not been identified to date in patients with mutations in PAX2.15 Foveal hypoplasia as well as macular abnormalities have been observed.12, 16, 17
Figure 1.
Fundus photographs from three patients with renal coloboma syndrome (a–c) and a normal retina for comparison (d). (a) Left retina from a patient with RCS and PAX2 mutation c.76dup.14 The arrow denotes a deeply excavated optic disc. (b) Right retina from a patient with RCS and PAX2 mutation c.76delG.14 The arrow denotes a retinal defect, however, the defect is temporal rather than nasal. (c) Right retina from a patient with PAX2 mutation c.76dup.13 The optic disc is enlarged and excavated. In all three retinae from patients with renal coloboma syndrome the retinal vessels emerge from the edge of the disc rather than the center. (d) A normal retina for comparison. Note that the typical optic nerve is smaller, compact and the retinal vessels emerge from the center of the disc.
Figure 2.
MRI of an optic nerve cyst in an affected patient with PAX2 mutation c.76dup denoted by the black arrow.14
Visual acuity ranges from normal to significant visual impairment with blindness. Nystagmus has been documented in a number of reports.3, 12, 16, 18 Anisometropic visual acuity has been reported with some as extreme as 20/20 in one eye and light perception in the other.12 Strabismus has been reported but may or may not be part of the syndrome. Many patients exhibit myopia of various degrees.3, 5, 14, 18 A recent report in a single patient identified calcified keratopathy, possibly secondary to renal failure and posterior lens luxation.19 Other sequelae include retinal detachment. Visual loss may be progressive over time (unpublished) but the mechanism of late onset loss is unknown.
Renal findings
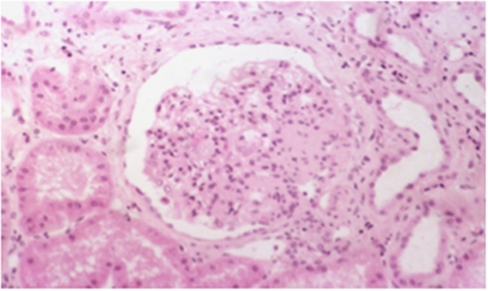
Renal malformations or insufficiency are identified in nearly all patients with RCS and are frequently identified before the eye malformations.5, 20 Renal findings in individuals with mutations in PAX2 include renal hypoplasia,3 renal hypodysplasia,21 multicystic dysplastic kidney,22 oligomeganephronia23 and horseshoe kidney.24 Renal hypoplasia and hypodysplasia describes small malformed kidneys that have fewer glomeruli that at some point may develop end-stage kidney disease. In studies of children identified for renal hypodysplasia, 10% will have mutations in PAX2.21, 25, 26 Multicystic dysplastic kidney has been identified in 10% of reported cases. Oligomeganephronia refers to kidneys where nephron number is strikingly reduced with structurally intact nephrons except for compensatory glomerular hypertrophy.23 Ultrasound findings show increased echogenicity as well as small size for age.3 Histologic findings can include glomerulosclerosis and mesangial fibrosis1, 13 (Figure 3).
Figure 3.
Histologic image of a single glomerlus from a patient with PAX2 mutation c.76dup exhibiting mesangial fibrosis and glomerulosclerosis.13
End-stage renal disease (ESRD) or renal failure can occur at any time, even within the same family with identical mutations in PAX2. ESRD may present prenatally with severely hypoplastic or aplastic kidneys and oligohydramnios resulting in fetal loss.18, 27 ESRD has been identified shortly after birth3, 18 and can occur as late as the seventh decade.12, 18 A single case of a surviving infant with Potter sequence, optic nerve malformations and a PAX2 mutation has been reported.28
Other renal findings include proteinuria, hypertension and vesicoureteral reflux. Vesicoureteral reflux may be an associated finding and although the majority may undergo spontaneous resolution, severe cases may be complicated by recurrent urinary tract infections and hydronephrosis necessitating surgical intervention.3, 18, 22
Auditory system
High frequency hearing loss presenting in childhood can be identified in up to 10% of affected individuals.9 High frequency hearing loss is unusual in childhood. In embryogenesis, Pax2 expression is critical for cochlear development and loss of Pax2 expression in the otic placode in knockout mice results in complete loss of cochlear development.29 The high frequency hearing loss in RCS appears to be a significant recurrent observation rather than related to age-related hearing loss.
Other clinical associations
Ligamentous laxity has been observed in a number of patients, but the underlying mechanism is uncertain.3, 14, 18 Chiari 1 malformation has been identified in a single patient with a PAX2 mutation.14 There are three reported individuals with developmental disability, although the majority of patients with PAX2 mutations have normal intellect.13, 19, 30
Allelic Conditions
Mutations in PAX2 have been identified in patients with isolated renal hypoplasia. In a series of 20 patients with renal hypoplasia, two were identified to have mutations in PAX2,25 one were subsequently found to have an optic nerve coloboma. In a study of children with renal hypoplasia, six out of ninety-nine probands were identified to have mutations in PAX2.21 In a recent survey of 20 children and young adults with congenital malformations of the urinary tract (CAKUT), two probands were identified to have PAX2 mutations and one subsequently was found to have optic nerve abnormalities.26
Diagnostic Criteria
Formal diagnostic criteria for RCS have not been established, however, in our clinical experience, patients who have the classical findings of optic nerve dysplasia or coloboma as well as renal hypodysplasia, nearly half will have mutations in PAX231 (Bower and Schimmenti, unpublished observations). It is recommended that patients with renal hypodysplasia be evaluated by an ophthalmologist for retinal examination with an eye for optic nerve malformations characteristic of RCS. Conversely, patients with optic nerve dysplasia should undergo additional evaluation consisting of blood pressure measurement, electrolytes, BUN/creatinine, urine analysis to evaluate for proteinuria and a renal ultrasound.
Differential Diagnosis
The differential diagnosis of RCS includes conditions where colobomas and renal anomalies have been identified. CHARGE syndrome (coloboma, heart malformations, atresia choanae, retardation of growth and development, genital anomalies, ear and hearing abnormalities) has overlap in that retinal and optic nerve colobomas are found.32 Patients with RCS do not have craniofacial abnormalities or cognitive difficulties typical of CHARGE syndrome. Oligomeganephronia is a common histologic finding in renal hypodysplasia and is not pathognomonic for RCS. Other conditions with renal hypodysplasia include deletions of distal 4p, branchio-oto-renal syndrome and mutations in HNF1beta.33, 34 There is significant overlap with eye findings in patients with PAX6 mutations, but renal anomalies are lacking.35 Patients with COACH or Joubert syndrome can have both colobomas and renal dysplasia leading to end-stage renal disease, however, patients with RCS will not have developmental disability, cerebellar hypoplasia, cerebellar dysfunction and hepatic dysfunction. Cat eye syndrome, or tetraploidy 22q, can have clinical overlap, however, typical iris colobomas are not typically observed.
Management
Management centers around sub-specialty care for the renal and ophthalmologic problems associated with RCS. Evaluations of affected patients should include biochemical tests of renal function, renal ultrasound, urine analysis with attention to proteinuria, blood pressure measurements and evaluation for vesicouretal reflux if clinically indicated. Long-term follow-up by a nephrologist is indicated for management of proteinuria, hypertension and prevention of complications associated with declining renal function and management of dialysis and transplantation when needed. Affected individuals should have close ophthalmologic management to prevent complications associated with retinal detachment. Low vision experts may be necessary to care for those patients with significant visual impairment. Audiologic evaluation for hearing loss is indicated as high frequency hearing loss may interfere with verbal communication.
Genetic Testing
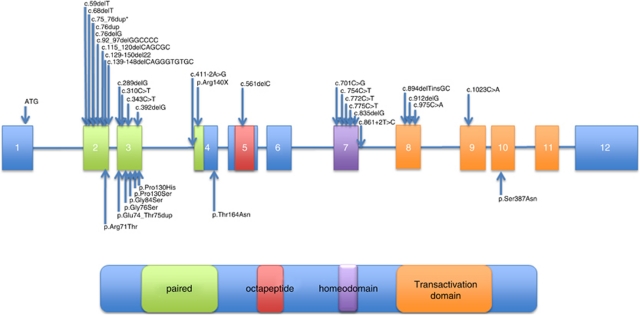
To date, PAX2 mutations have been the only identified genetic cause associated with RCS. The majority of mutations are deletions or duplications of a single nucleotide, missense mutations, nonsense mutations or small deletions or duplications of two or more nucleotides occurring in exons 2, 3 and 4 encoding the paired domain.36 The most prevalent mutations are frame shift mutations leading to a premature stop occurring in exons encoding the paired domain (Figure 4). Missense, nonsense and frameshift mutations have been reported. Genotype/phenotype correlations between mutations in the paired domain have not been identified.37 Mutations that occur in the exon 7, 8 and 9, may have a more severe renal phenotype than eye phenotype,24, 38 but there is significant variability of the phenotype even within single families.
Figure 4.
Illustration of the genomic structure of PAX2 from chromosome 10q24 covering nucleotides 102 505 468–102 589 697 (hg19 assembly). Exons 2, 3 and part of 4 (green) encode the paired domain of the PAX2 protein illustrated below. The octapeptide domain (pink), truncated homeodomain (purple) and transactivation domain (orange) are indicated. Published mutations are noted by arrows over their corresponding exons. The asterisk denotes the recurrent mutation c.76dup. Mutation notation has been updated from original publications. Each mutation has been reported for the first time in the following references: 2, 4, 5, 12, 13, 14, 15, 16, 20, 21, 22, 23, 24, 25, 27, 30, 37, 38, 52. This figure is not drawn to scale.
The most common recurrent mutation is an insertion of a guanine residue in a string of seven guanines in exon 2, c.76dup and has been reported numerous times. This mutation occurs in a string of seven guanines in exon 2, a mutational hotspot; most mutations are de novo and have occurred worldwide in various ethnic groups. Deletions as well as two base pair (GG) duplications have been reported.4, 14, 20
Only three large genomic abnormalities of PAX2 have been reported. There is a single report of a large genomic rearrangement resulting from a translocation occurring between exons 3 and 4 resulting in a phenotype consistent with RCS.39 A single patient who presented with renal malformations but had a normal eye examination was identified to harbor a 7.9 Mb deletion at 10q24 encompassing the PAX2 locus.40 Recently, a small deletion of PAX2 locus was identified by high-resolution array CGH41 in a patient with both renal and ocular findings of RCS. A systematic evaluation of patients with a RCS phenotype for genomic abnormalities has not yet been reported.
The current literature suggests that point mutations within the coding region of the PAX2 gene may not be the only cause of RCS. In a series of 17 patients with a phenotype consistent with RCS, point mutations in PAX2 were identified in nearly half.31
Genetic Counseling
Mutations in PAX2 are inherited in an autosomal dominant manner although de novo mutations are not uncommon.13 Affected individuals have a 50% chance of passing on RCS with each pregnancy. Gonosomal mosaicism has been observed in an unaffected parent who had affected children.20 Prenatal diagnosis or pre-implantation genetic testing is possible if the mutation in a family has been identified.
Animal Models
Animal models and studies in early retinal development provide evidence to suggest that PAX2 and its role in optic fissure formation and closure are important in understanding the observed eye abnormalities in RCS. Ocular development begins with the paired formation of optic vesicles from the lateral forebrain. Ventral infolding of the optic vesicle allows development of the optic stalk proximally and optic cup distally with formation of a ventral groove called the optic fissure. The optic fissure provides a conduit and guidance for entrance of vascular cells into the retina and an exit for the retinal axons. The term ‘coloboma' describes ocular defects where a hole or gap is observed, presumably from failure of closure of the optic fissure.42 In both mice and zebrafish, homozygous mutations in Pax2/pax2a result in failed optic fissure closure and a defect resembling chorioretinal coloboma, whereas studies in Pax2 haploinsufficient mice demonstrate that the optic fissure fails to extend into the optic stalk with a dysplasic optic disc.43, 44 This suggests that in the presence of a PAX2 mutation, the observed optic malformations result from optic fissure defects and supports the notion that the observed abnormalities in RCS should be considered in the continuum of malformations described as coloboma.
Retinal vascular malformations may be secondary to optic fissure malformation and result from abnormal PAX2 expression. In the developing mouse optic stalk, Pax2 expressing astrocytes migrate into the optic stalk ahead of entering vascular cells and serve as a guide or scaffold to the developing vasculature.45
In zebrafish, both homozygosity for pax2a null and hypomorphic alleles result in midbrain/hindbrain anomalies with loss of the isthmus, a structure orthologous to the midbrian/hindbrain of mammals.46 Homozygous embryos have optic fissure closure defects and die within a few days from hatching due to severely impaired renal function.
The role of Pax2 in kidney and gonadal structure development has been studied in mouse models. In mice and other amniotes, the pronephros, the nephric duct and subsequent mesonephros arise from paraxial mesoderm. The definitive kidney, or metanephros arises from the interaction of the ureteric bud, a caudal outpouching of the nephric duct with the overlying mesenchyme. Branching of the ureteric bud within the metanephric blastema results in the formation of the definitive kidney structure.47 Pax2 expression appears critical for formation of the nephric duct and the ureteric bud as homozygous knockout mice fail to develop kidneys, ureters and genital tracts.48
The mechanisms of renal hypoplasia and vesicoureteral reflux has been sought in mouse models. Favor et al (1995) described a mouse model, Pax21Neu with the identical common human allele c.76dup. In the heterozygous state, Pax21Neu mice have similar eye and kidney abnormalities as human patients with RCS.49 In this model, heterozygous mice have significantly smaller kidneys with fewer glomeruli and show increased rates of apoptotic cell death compared with wild-type controls demonstrating that Pax2 prevents cell death and reduced Pax2 dosage results in increased cell death, smaller kidneys and fewer glomeruli.38 Furthermore, in studies of heterozygous mice using a green fluorescent protein reporter for cells of the nephric duct, reduced branching of the ureteric bud within the metanephros leads to fewer, and apparently larger, glomerulae. This suggests a major role for Pax2 in ureteric bud branching and supports observations that Pax2 is necessary for mesenchymal to epithelial transformation that occurs within the metanephros.50, 51 Heterozygous Pax21Neu mice exhibit a high rate of vesicouteral reflux with the associated complication of hydroureter, hydronephrosis and urinary tract infections. The ureteric bud emerges further caudal compared with controls, implants for a shorter distance within the bladder wall and exhibits a higher rate of malformations such as duplicated collecting system.50
Conclusions And Future Directions
RCS is an autosomal dominant condition characterized by optic nerve coloboma or dysplasia and renal hypodysplasia. Mutations in PAX2 may be identified in nearly half of all patients with this condition. Recognition of this rare condition will allow for improved diagnosis and management.
Future areas for research development include identification of the genetic basis of RCS in phenotypically affected patients who are not identified to have point mutations in PAX2. Development of testing algorithms that include methods for identification of deletions at the PAX2 locus and studies to identify other loci associated with RCS are two priority areas of clinical research.
Further research is needed to understand the longitudinal course of RCS, particularly long-term visual outcome. Basic science research in both mouse and fish models are needed to determine the role of Pax2/pax2a in optic fissure development and the role of PAX2 in retinal vasculature patterning.
Acknowledgments
I thank all the individuals and families who have given of themselves to further our understanding of renal coloboma syndrome and conditions associated with mutations in PAX2. I would like to express my appreciation to colleagues, most cited in this review; each has worked to increase our understanding of renal coloboma syndrome. I would also like to thank the two anonymous reviewers for their thoughtful comments.
The author declares no conflict of interest.
References
- Weaver RG, Cashwell LF, Lorentz W, Whiteman D, Geisinger KR, Ball M. Optic nerve coloboma associated with renal disease. Am J Med Genet. 1988;29:597–605. doi: 10.1002/ajmg.1320290318. [DOI] [PubMed] [Google Scholar]
- Sanyanusin P, Schimmenti LA, McNoe LA, et al. Mutation of the PAX2 gene in a family with optic nerve colobomas, renal anomalies and vesicoureteral reflux. Nat Genet. 1995;9:358–364. doi: 10.1038/ng0495-358. [DOI] [PubMed] [Google Scholar]
- Schimmenti LA, Pierpont ME, Carpenter BL, Kashtan CE, Johnson MR, Dobyns WB. Autosomal dominant optic nerve colobomas, vesicoureteral reflux, and renal anomalies. Am J Med Genet. 1995;59:204–208. doi: 10.1002/ajmg.1320590217. [DOI] [PubMed] [Google Scholar]
- Sanyanusin P, McNoe LA, Sullivan MJ, Weaver RG, Eccles MR. Mutation of PAX2 in two siblings with renal-coloboma syndrome. Hum Mol Genet. 1995;4:2183–2184. doi: 10.1093/hmg/4.11.2183. [DOI] [PubMed] [Google Scholar]
- Chung GW, Edwards AO, Schimmenti LA, Manligas GS, Zhang YH, Ritter R., III Renal-coloboma syndrome: report of a novel PAX2 gene mutation. Am J Ophthalmol. 2001;132:910–914. doi: 10.1016/s0002-9394(01)01231-4. [DOI] [PubMed] [Google Scholar]
- Parsa CF, Silva ED, Sundin OH, et al. Redefining papillorenal syndrome: an underdiagnosed cause of ocular and renal morbidity. Ophthalmology. 2001;108:738–749. doi: 10.1016/s0161-6420(00)00661-8. [DOI] [PubMed] [Google Scholar]
- Puschel AW, Westerfield M, Dressler GR. Comparative analysis of Pax-2 protein distributions during neurulation in mice and zebrafish. Mech Dev. 1992;38:197–208. doi: 10.1016/0925-4773(92)90053-m. [DOI] [PubMed] [Google Scholar]
- Nornes HO, Dressler GR, Knapik EW, Deutsch U, Gruss P. Spatially and temporally restricted expression of Pax2 during murine neurogenesis. Development. 1990;109:797–809. doi: 10.1242/dev.109.4.797. [DOI] [PubMed] [Google Scholar]
- Schimmenti LA. Genetic and developmental basis of renal coloboma (papillorenal) syndrome. Expert Rev Ophthalmol. 2009;4:135–144. [Google Scholar]
- Terzic J, Muller C, Gajovic S, Saraga-Babic M. Expression of PAX2 gene during human development. Int J Dev Biol. 1998;42:701–707. [PubMed] [Google Scholar]
- Tellier AL, Amiel J, Delezoide AL, et al. Expression of the PAX2 gene in human embryos and exclusion in the CHARGE syndrome. Am J Med Genet. 2000;93:85–88. doi: 10.1002/1096-8628(20000717)93:2<85::aid-ajmg1>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Schimmenti LA, Manligas GS, Sieving PA. Optic nerve dysplasia and renal insufficiency in a family with a novel PAX2 mutation, Arg115X: further ophthalmologic delineation of the renal-coloboma syndrome. Ophthalmic Genet. 2003;24:191–202. doi: 10.1076/opge.24.4.191.17229. [DOI] [PubMed] [Google Scholar]
- Schimmenti LA, Cunliffe HE, McNoe LA, et al. Further delineation of renal-coloboma syndrome in patients with extreme variability of phenotype and identical PAX2 mutations. Am J Hum Genet. 1997;60:869–878. [PMC free article] [PubMed] [Google Scholar]
- Schimmenti LA, Shim HH, Wirtschafter JD, et al. Homonucleotide expansion and contraction mutations of PAX2 and inclusion of Chiari 1 malformation as part of renal-coloboma syndrome. Hum Mutat. 1999;14:369–376. doi: 10.1002/(SICI)1098-1004(199911)14:5<369::AID-HUMU2>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Cunliffe HE, McNoe LA, Ward TA, Devriendt K, Brunner HG, Eccles MR. The prevalence of PAX2 mutations in patients with isolated colobomas or colobomas associated with urogenital anomalies. J Med Genet. 1998;35:806–812. doi: 10.1136/jmg.35.10.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higashide T, Wada T, Sakurai M, Yokoyama H, Sugiyama K. Macular abnormalities and optic disk anomaly associated with a new PAX2 missense mutation. Am J Ophthalmol. 2005;139:203–205. doi: 10.1016/j.ajo.2004.07.021. [DOI] [PubMed] [Google Scholar]
- Samimi S, Antignac C, Combe C, Lacombe D, Renaud Rougier MB, Korobelnik JF. Bilateral macular detachment caused by bilateral optic nerve malformation in a papillorenal syndrome due to a new PAX2 mutation. Eur J Ophthalmol. 2008;18:656–658. doi: 10.1177/112067210801800430. [DOI] [PubMed] [Google Scholar]
- Ford B, Rupps R, Lirenman D, et al. Renal-coloboma syndrome: prenatal detection and clinical spectrum in a large family. Am J Med Genet. 2001;99:137–141. doi: 10.1002/1096-8628(2000)9999:999<00::aid-ajmg1143>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Beby F, Roche O, Cochat P, et al. New ocular phenotype associated with a mutation in the PAX2 gene. Eye (Lond) 2010;24:1293–1294. doi: 10.1038/eye.2009.330. [DOI] [PubMed] [Google Scholar]
- Amiel J, Audollent S, Joly D, et al. PAX2 mutations in renal-coloboma syndrome: mutational hotspot and germline mosaicism. Eur J Hum Genet. 2000;8:820–826. doi: 10.1038/sj.ejhg.5200539. [DOI] [PubMed] [Google Scholar]
- Weber S, Moriniere V, Knuppel T, et al. Prevalence of mutations in renal developmental genes in children with renal hypodysplasia: results of the ESCAPE study. J Am Soc Nephrol. 2006;17:2864–2870. doi: 10.1681/ASN.2006030277. [DOI] [PubMed] [Google Scholar]
- Fletcher J, Hu M, Berman Y, et al. Multicystic dysplastic kidney and variable phenotype in a family with a novel deletion mutation of PAX2. J Am Soc Nephrol. 2005;16:2754–2761. doi: 10.1681/ASN.2005030239. [DOI] [PubMed] [Google Scholar]
- Salomon R, Tellier AL, Attie-Bitach T, et al. PAX2 mutations in oligomeganephronia. Kidney Int. 2001;59:457–462. doi: 10.1046/j.1523-1755.2001.059002457.x. [DOI] [PubMed] [Google Scholar]
- Taranta A, Palma A, De Luca V, et al. Renal-coloboma syndrome: a single nucleotide deletion in the PAX2 gene at Exon 8 is associated with a highly variable phenotype. Clin Nephrol. 2007;67:1–4. doi: 10.5414/cnp67001. [DOI] [PubMed] [Google Scholar]
- Nishimoto K, Iijima K, Shirakawa T, et al. PAX2 gene mutation in a family with isolated renal hypoplasia. J Am Soc Nephrol. 2001;12:1769–1772. doi: 10.1681/ASN.V1281769. [DOI] [PubMed] [Google Scholar]
- Negrisolo S, Benetti E, Centi S, et al. PAX2 gene mutations in pediatric and young adult transplant recipients: kidney and urinary tract malformations without ocular anomalies Clin Genet 2010. doi: 10.1111/j.1399-0004.2010.01588.xe-pub ahead of print 29 October 2010). [DOI] [PubMed]
- Martinovic-Bouriel J, Benachi A, Bonniere M, et al. PAX2 mutations in fetal renal hypodysplasia. Am J Med Genet A. 2010;152A:830–835. doi: 10.1002/ajmg.a.33133. [DOI] [PubMed] [Google Scholar]
- Tagami M, Honda S, Morioka I, Matsuo M, Negi A. Bilateral optic disc anomalies associated with PAX2 mutation in a case of potter sequence. Case Report Ophthalmol. 2010;1:94–98. doi: 10.1159/000321625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres M, Gomez-Pardo E, Gruss P. Pax2 contributes to inner ear patterning and optic nerve trajectory. Development. 1996;122:3381–3391. doi: 10.1242/dev.122.11.3381. [DOI] [PubMed] [Google Scholar]
- Miyazawa T, Nakano M, Takemura Y, et al. A case of renal-coloboma syndrome associated with mental developmental delay exhibiting a novel PAX2 gene mutation. Clin Nephrol. 2009;72:497–500. doi: 10.5414/cnp72497. [DOI] [PubMed] [Google Scholar]
- Dureau P, Attie-Bitach T, Salomon R, et al. Renal coloboma syndrome. Ophthalmology. 2001;108:1912–1916. doi: 10.1016/s0161-6420(01)00722-9. [DOI] [PubMed] [Google Scholar]
- Pagon RA, Graham JM, Jr, Zonana J, Yong SL. Coloboma, congenital heart disease, and choanal atresia with multiple anomalies: CHARGE association. J Pediatr. 1981;99:223–227. doi: 10.1016/s0022-3476(81)80454-4. [DOI] [PubMed] [Google Scholar]
- Sikora P, Zajaczkowska M, Katska E, Niedzielska G. [A nineteen year observation of a boy with branchio-oto-renal syndrome and chronic renal failure] Pol Merkur Lekarski. 2001;10:291–293. [PubMed] [Google Scholar]
- Bohn S, Thomas H, Turan G, et al. Distinct molecular and morphogenetic properties of mutations in the human HNF1beta gene that lead to defective kidney development. J Am Soc Nephrol. 2003;14:2033–2041. doi: 10.1097/01.asn.0000078808.70309.c4. [DOI] [PubMed] [Google Scholar]
- Azuma N, Yamaguchi Y, Handa H, et al. Mutations of the PAX6 gene detected in patients with a variety of optic-nerve malformations. Am J Hum Genet. 2003;72:1565–1570. doi: 10.1086/375555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles MR, Schimmenti LA. Renal-coloboma syndrome: a multi-system developmental disorder caused by PAX2 mutations. Clin Genet. 1999;56:1–9. doi: 10.1034/j.1399-0004.1999.560101.x. [DOI] [PubMed] [Google Scholar]
- Devriendt K, Matthijs G, Van Damme B, et al. Missense mutation and hexanucleotide duplication in the PAX2 gene in two unrelated families with renal-coloboma syndrome (MIM 120330) Hum Genet. 1998;103:149–153. doi: 10.1007/s004390050798. [DOI] [PubMed] [Google Scholar]
- Porteous S, Torban E, Cho NP, et al. Primary renal hypoplasia in humans and mice with PAX2 mutations: evidence of increased apoptosis in fetal kidneys of Pax2(1Neu) +/− mutant mice. Hum Mol Genet. 2000;9:1–11. doi: 10.1093/hmg/9.1.1. [DOI] [PubMed] [Google Scholar]
- Narahara K, Baker E, Ito S, et al. Localisation of a 10q breakpoint within the PAX2 gene in a patient with a de novo t(10;13) translocation and optic nerve coloboma-renal disease. J Med Genet. 1997;34:213–216. doi: 10.1136/jmg.34.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benetti E, Artifoni L, Salviati L, et al. Renal hypoplasia without optic coloboma associated with PAX2 gene deletion. Nephrol Dial Transplant. 2007;22:2076–2078. doi: 10.1093/ndt/gfm187. [DOI] [PubMed] [Google Scholar]
- Raca G, Jackson CA, Kucinskas L, et al. Array comparative genomic hybridization analysis in patients with anophthalmia, microphthalmia, and coloboma. Genet Med. 2011. [DOI] [PMC free article] [PubMed]
- Gregory-Evans CY, Williams MJ, Halford S, Gregory-Evans K. Ocular coloboma: a reassessment in the age of molecular neuroscience. J Med Genet. 2004;41:881–891. doi: 10.1136/jmg.2004.025494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alur RP, Vijayasarathy C, Brown JD, et al. Papillorenal syndrome-causing missense mutations in PAX2/Pax2 result in hypomorphic alleles in mouse and human. PLoS Genet. 2010;6:e1000870. doi: 10.1371/journal.pgen.1000870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otteson DC, Shelden E, Jones JM, Kameoka J, Hitchcock PF. Pax2 expression and retinal morphogenesis in the normal and Krd mouse. Dev Biol. 1998;193:209–224. doi: 10.1006/dbio.1997.8794. [DOI] [PubMed] [Google Scholar]
- Chan-Ling T, McLeod DS, Hughes S, et al. Astrocyte-endothelial cell relationships during human retinal vascular development. Invest Ophthalmol Vis Sci. 2004;45:2020–2032. doi: 10.1167/iovs.03-1169. [DOI] [PubMed] [Google Scholar]
- Lun K, Brand M. A series of no isthmus (noi) alleles of the zebrafish pax2.1 gene reveals multiple signaling events in development of the midbrain-hindbrain boundary. Development. 1998;125:3049–3062. doi: 10.1242/dev.125.16.3049. [DOI] [PubMed] [Google Scholar]
- Dressler GR. Advances in early kidney specification, development and patterning. Development. 2009;136:3863–3874. doi: 10.1242/dev.034876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres M, Gomez-Pardo E, Dressler GR, Gruss P. Pax-2 controls multiple steps of urogenital development. Development. 1995;121:4057–4065. doi: 10.1242/dev.121.12.4057. [DOI] [PubMed] [Google Scholar]
- Favor J, Sandulache R, Neuhauser-Klaus A, et al. The mouse Pax2(1Neu) mutation is identical to a human PAX2 mutation in a family with renal-coloboma syndrome and results in developmental defects of the brain, ear, eye, and kidney. Proc Natl Acad Sci USA. 1996;93:13870–13875. doi: 10.1073/pnas.93.24.13870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murawski IJ, Myburgh DB, Favor J, Gupta IR. Vesico-ureteric reflux and urinary tract development in the Pax21Neu+/− mouse. Am J Physiol Renal Physiol. 2007;293:F1736–F1745. doi: 10.1152/ajprenal.00221.2007. [DOI] [PubMed] [Google Scholar]
- Rothenpieler UW, Dressler GR. Pax-2 is required for mesenchyme-to-epithelium conversion during kidney development. Development. 1993;119:711–720. doi: 10.1242/dev.119.3.711. [DOI] [PubMed] [Google Scholar]
- Cheong HI, Cho HY, Kim JH, Yu YS, Ha IS, Choi Y. A clinico-genetic study of renal coloboma syndrome in children. Pediatr Nephrol. 2007;22:1283–1289. doi: 10.1007/s00467-007-0525-z. [DOI] [PubMed] [Google Scholar]