Abstract
Introduction
Although cardiovascular diseases (CVD) are the leading cause of death among Americans, significant disparities persist in CVD prevalence, morbidity, and mortality based on race and ethnicity. However, few studies have examined risk factor reduction among the poor and ethnic minorities.
Methods
Community-based participatory research (CBPR) study using a cluster randomized design — African-American church congregations are the units of randomization and individuals within the congregations are the units of analysis. Outcome variables include dietary change (Diet History Questionnaire), level of physical activity (7-Day Physical Activity Recall), lipoprotein levels, blood pressure, fasting glucose, and hemoglobin A1c.
Results
Eighteen (18) church congregations were randomized to either a health maintenance intervention or a control condition. Complete data were obtained on 392 African-American individuals, 18 to 70 years of age, predominantly employed women with more than a high school diploma. Treatment and intervention groups were similar at baseline on saturated fat intake, metabolic equivalent of tasks (METS) per day, and other risk factors for CVD.
Conclusions
The GoodNEWS trial successfully recruited and evaluated CVD-related risk among African-American participants using a CBPR approach. Several logistical challenges resulted in extending the recruitment, preliminary training, and measurement periods. The challenges were overcome with the assistance of a local community consultant and a professional event planner. Our experience supports the need for incorporating non-traditional community-based staff into the design and operational plan of CBPR trials.
Keywords: Community-based participatory research, Cardiovascular diseases, Health behavior, Risk factors, Health disparities
1. Introduction
Cardiovascular diseases (CVD) are the leading cause of death among Americans in all racial and ethnic categories [1]; they account for 37.3% of all deaths and 58% when measured as a contributing cause [2]. However, significant disparities persist in the prevalence, morbidity, and mortality associated with CVD and their major risk factors based on race and ethnicity [3]. Compared to whites, blacks and Hispanics/Mexican Americans have a higher risk of developing disease and experiencing adverse CVD-related health outcomes [3], and blacks have a higher prevalence of stroke [4] and stroke mortality [5], and a higher overall mortality rate from CVD [3] and coronary heart disease [1]. Additionally, blacks have a higher prevalence of established risk factors for disease, including hypertension, diabetes, obesity, and physical inactivity [3,4,6].
The NIH recognizes that reducing risk factor prevalence –rather than disease treatment – is the most desirable strategy for reducing coronary heart disease morbidity, disability and mortality in high-risk populations [7]. Established risk factors for CVD include high blood pressure, high blood cholesterol, diabetes, tobacco use, physical inactivity, poor nutrition and obesity [5,8]. Modest but sustained changes in lifestyles related to these factors can lead to rapid and substantial decreases in CVD risk [9,10].
Although lifestyle modifications are known to reduce CVD in white, middle-class populations, they have not been widely tested among the poor and ethnic minorities [11]. Studies are needed examining lifestyle change in low income and minority communities, which appreciate the range of relevant factors in these communities [12], and address the social and behavioral factors that contribute to disease, disability and death [13]. Successful community-based disease prevention interventions and risk-reduction approaches must also balance the needs of researchers with the needs of communities’,[14] utilize local resources [15], and tailor the interventions to fit the at-risk target population [16]. By combining the efforts of researchers and community members prevention research can be translated into actions that will benefit those at risk in the target community [17].
The GoodNEWS (Genes, Nutrition, Exercise, Wellness, and Spiritual Growth) Trial is a community-based participatory research (CBPR) study for reducing risk factors for CVD among African-American individuals, using a Lay Health Promoter (LHP) approach in the faith-based organization (FBO) setting. CBPR promotes community ownership of a project by involving community stakeholders in all phases of research from problem definition through project completion [17–20]. Participatory research ensures that intervention strategies are culturally appropriate [21], contributes to building trust between researchers and communities [22], is effective for studying community-based lifestyle factors [23,24], and contributes to resolution of urban and rural health problems [25,26]. LHP programs are based on natural helping, and build on a community’s existing social networks and social relationships [27]. Social networks can improve community and individual health since social relationships are strongly related to physical and psychological well-being[27], and natural helping strategies can successfully develop networks or incorporate existent networks into interventions designed to improve community and individual health [28]. FBOs are another community resource for preventing disease in high-risk populations; in the United States churches and religious organizations – especially in African-American communities –have a long history of participating in community-based initiatives and health collaborations [29–33]. Studies support the importance of FBOs as an ally in community-based prevention [34] and the effectiveness of lifestyle education in the congregational setting [35].
The present trial responds to the need for testing the effectiveness of supportive environments on producing lasting health behavior changes in minority communities [36,37]. Our study will increase what is known about community-based prevention programs in general and FBO-based LHP models in particular. The project’s most significant contribution is testing a means for maintaining comprehensive lifestyle change among adults with multiple CVD risk factors, through a community and academic partnership. The present paper describes the study design, recruitment, baseline measurement and training procedures, and randomization and analysis guidelines. The discussion provides insight into the challenges of conducting a randomized trial in the community-based setting, and a summary of lessons learned and modifications that were made in response to the conditions encountered during initial program implementation phase of the project.
2. Methods
2.1. Study design and analysis
2.1.1. Study aims
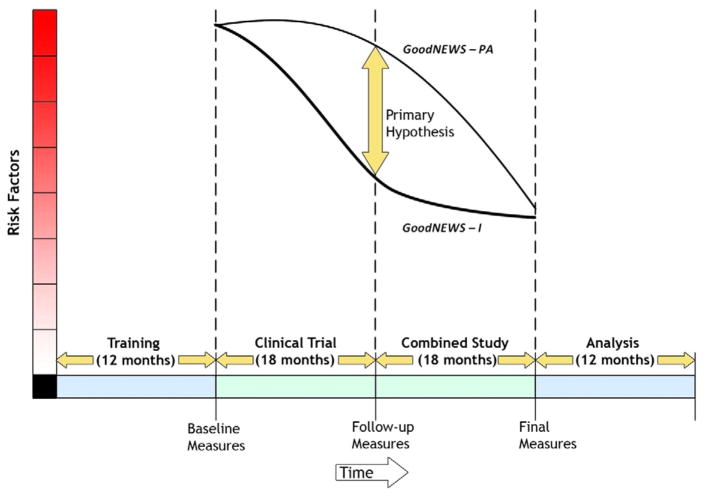
The primary aim of The GoodNEWS Trial is to assess the effect of a health promotion program combined with a maintenance intervention among African-American individuals, on increasing levels of physical activity and dietary change. The secondary aim is to determine the effect of the intervention on lipoprotein levels, blood pressure, fasting glucose, and hemoglobin A1c (HbA1c). Participating congregations are randomized to either a health education program with a maintenance intervention (GoodNEWS-I) or a health education program alone with limited staff contact and a monthly newsletter (GoodNEWS-PA). At the end of the 18 months, the GoodNEWS-PA group will be invited to join the GoodNEWS-I group, and both groups will be followed in a combined study for another 18 months (GoodNEWS-C). Primary data collection will occur at baseline, 18, and 36 months (see Fig. 1). The study received full board approval from the University of Texas Southwestern Medical Center at Dallas Institutional Review Board (IRB).
Fig. 1.
Timeline, measurement, and primary hypothesis. This figure illustrates the GoodNEWS timeline including primary hypothesis and measurements.
2.1.2. Study hypotheses and outcomes
The primary hypothesis is that GoodNEWS-I participants will significantly increase physical activity and healthy eating behavior after 18 months, compared to GoodNEWS-PA participants. The secondary hypothesis is that lipoprotein and glucose levels, blood pressure, and HbA1c will be significantly improved over baseline in the GoodNEWS-I group and that these changes will be significantly greater than those in the GoodNEWS-PA group. After 36 months final data will be analyzed from the GoodNEWS-C group controlling for initial group assignment.
The two primary outcomes are: 1) a reduction in saturated fat dietary intake as measured by Diet History Questionnaire (DHQ), and, 2) an increase in energy expenditure in kcal/kg/day as measured by 7-Day Physical Activity Recall (PAR). It is expected that at the end of 18 months, GoodNEWS-I participants will reduce saturated fat intake by 3.2 g/day and increase physical activity by 1.1 kcal/kg/day compared to GoodNEWS-PA participants. Changes in lipoprotein levels, blood pressure, fasting glucose, and HbA1c are expected to be significantly improved among GoodNEWS-I participants compared to baseline and in comparison with GoodNEWS-PA participants (Table 1).
Table 1.
Outcomes and instruments.
| Outcome measures | Test/instrument | Timing |
|---|---|---|
| Primary outcomes | ||
| Physical activity | 7-Day PAR | |
| Dietary changes | Diet History Questionnaire (DHQ) | |
| Secondary outcomes | ||
| Cardiovascular risk factors | Blood pressure | Baseline 18-months 36-months |
| Total cholesterol, HDL (high density lipoprotein cholesterol), LDL (low density lipoprotein) and triglycerides | ||
| Glucose level | ||
| Hemoglobin A1C (diabetics only) | ||
| Anthropometrics measurements | Body Mass Index (BMI) | |
| Waist circumference |
2.1.3. Measurement instruments
The DHQ is a food frequency questionnaire developed by the National Cancer Institute to measure an individuals’ usual dietary intake over the past year [38]. It assesses dietary behaviors, portion size, and frequency for intake of 124 foods items and dietary supplements. The 7-Day PAR estimates an individuals’ typical activity pattern by asking participants to recall the amount of time spent in sleep and in moderate, hard and very hard activities during the previous 7 days [39]. Values are recorded in metabolic equivalent tasks (METS), and its reliability and validity are well established [40]. Fasting capillary blood from a finger stick was tested for glucose, HbA1c, and lipid levels — the DSL 2000 was used for HbA1c testing and the Cholestech LDX was used for the lipid panel and glucose levels. Capillary blood testing was selected over venipuncture to reduce the risk of missing tests due to participant apprehension.
2.1.4. Sample size and power estimates
The primary outcome for sample size and power estimates is physical activity response in kcal/kg/day, based on the 7-Day PAR. A net difference of 1.1 kcal/kg/day is expected between groups based on the results observed in Project PRIME [41]. We estimate dietary changes to be a 3.2 gram decrease of saturated fat on the DHQ. Twenty sites, each with 20 participants, provide greater than 80% power to detect an effect size of 0.30 with an intraclass correlation of 0.015. An effect size of 0.30 is a 3.2% difference for energy expenditure and 15% for saturated fat [42]. Since an attrition rate of 15% is expected, the enrollment target was 23 participants at each site.
2.1.5. Randomization
A cluster randomized design is used with church congregations as the units of randomization (clusters) and individual participants as the units of analysis. The original study design specified 20 congregations stratified on the basis of congregation size and then randomly assigned to either GoodNEWS-I (treatment) or GoodNEWS-PA (control). However, the randomization plan was amended to reflect the level of engagement or interest in completing the study measurements among congregations’ members. Pairs of churches were created based on two factors: 1) the number of study participants who initially signed a letter of commitment to participate in the study, and, 2) a percentage value reflecting the number of study participants in a church who showed up to participate in measurement and data gathering divided by the number of church members who had initially signed the letter of commitment to participate. The revised randomization plan and stratification strategy resulted in pairs of churches with roughly equivalent numbers of study participants, and with comparable levels of motivation to participate in the study as reflected in the percentage of those who signed up to participate and were motivated to not only sign up but to also follow through on their commitment by coming to the measurement event. The paired churches were randomized by coin flip to either the treatment or control arm (Table 2).
Table 2.
Enrollment of Participants and Randomization of Churches.
| Church | Approx. cong. size | Signed commitment letter | Signed informed consent | Consented (at-event) | Attended measurement event | Signed letter and attended (%) | Completed measurements | Randomization pairing |
|---|---|---|---|---|---|---|---|---|
| Church 1 | 3,500 | 54 | 50 | 7 | 45 | 83 | 45 | 1 |
| Church 2 | 200 | 38 | 35 | 6 | 33 | 87 | 33 | 1 |
| Church 3 | 500 | 47 | 41 | 0 | 34 | 72 | 34 | 2 |
| Church 4 | 500 | 38 | 33 | 2 | 32 | 84 | 32 | 2 |
| Church 5 | 11,000 | 43 | 24 | 6 | 24 | 56 | 24 | 3 |
| Church 6 | 200 | 30 | 23 | 3 | 23 | 77 | 23 | 3 |
| Church 7 | 200 | 22 | 22 | 6 | 18 | 82 | 18 | 4 |
| Church 8 | 150 | 28 | 19 | 1 | 19 | 68 | 19 | 4 |
| Church 9 | 100 | 26 | 19 | 0 | 18 | 69 | 18 | 5 |
| Church 10 | 700 | 35 | 28 | 6 | 23 | 66 | 23 | 5 |
| Church 11 | 250 | 30 | 24 | 2 | 21 | 70 | 20 | 6 |
| Church 12 | 200 | 30 | 26 | 2 | 17 | 57 | 17 | 6 |
| Church 13 | 200 | 35 | 21 | 6 | 14 | 40 | 14 | 7 |
| Church 14 | 2,500 | 18 | 13 | 1 | 13 | 72 | 13 | 7 |
| Church 15 | 2,000 | 47 | 34 | 12 | 30 | 64 | 27 | 8 |
| Church 16 | 350 | 24 | 14 | 3 | 9 | 38 | 9 | 8 |
| Church 17 | 100 | 26 | 15 | 3 | 14 | 54 | 14 | 9 |
| Church 18 | 100 | 13 | 10 | 1 | 9 | 69 | 9 | 9 |
| TOTALS | 584 | 451 | 67 | 396 | 67 | 392 | N/A |
2.1.6. Data analysis
Analyses at the conclusion of the 18-month trial will take into account the lack of independence (correlation) among individuals within a site (congregation). This dependence will be incorporated into a mixed model to obtain proper variance estimates [43]. Site will be included in the multilevel analyses as a random effect [44]. In all analyses there is one between factor (group assignment variable — GoodNEWS-I or GoodNEWS-PA) and a within factor (data collection time — baseline or 18-month follow up) where the within factor is nested within site.
The primary analysis will compare the two arms but only for the first two time points (baseline and 18-month follow up), where group difference is of primary interest. A secondary analysis will be performed consisting of the same group but across all three time periods. The group by time interaction is the outcome of interest in this analysis. If the interaction is statistically significant then graphical procedures and post-hoc analyses will be used to clarify the interaction. Analyses will be performed using SAS Proc Mixed (SAS Institute, Cary, NC) v. 9 or higher [42].
The two analyses will be performed separately for the two primary outcome measures. Post-hoc analyses will consist of the same analyses performed on each of the secondary measures. For post-hoc analyses an alpha of 0.025 will be used to reduce the probability of a Type I error without overly inflating the Type II error. In the present paper, Chi-square analysis is performed to test for associations between categorical variables and group assignment, and the t-test is used for testing for differences on the continuous variables between the two groups.
2.2. Program components and implementation
2.2.1. Setting
The GoodNEWS trial is a faith-health collaborative study [45] located in the congregational setting in an area known as South Dallas and the Southern Sector. The Southern Sector of Dallas has the largest concentration of poverty, female-headed households, and unemployed males, and has disproportionately higher levels of morbidity and mortality when compared to other sectors of the city. It is predominantly African-American and – as in most African-American communities – the Church is considered the most important social institution in the community. Churches play a leadership role on issues ranging from education, health, and social justice, to matters of economic and community development.
2.2.2. GoodNEWS training program and theoretical framework
The GoodNEWS program uses a “train the trainer” approach; two (2) Lay Health Promoter’s (LHPs) from each congregation receive health education training, and then teach the information and skills to their congregation members. The program is curriculum based, and is built on social cognitive theory (SCT), wellness principles, and health promotion theory. Consistent with SCT, the program corrects misperceptions about chronic disease, educates participants about the value of health, explains how specific behaviors are related to health outcomes, and promotes practicing the skills needed for adopting healthier behaviors [46,47]. As a wellness program, the curriculum emphasizes the importance of healthy living rather than concepts of illness avoidance [48,49]. Its content is multidimensional, emphasizing the physical, mental, intellectual, social, environmental and spiritual dimensions of health [48,50]. The wellness model exists in numerous forms and our model substitutes environmental health for occupational health in order to emphasize participants’ need to overcome the “place-based” effects of living in low-income neighborhoods [51,52]. Finally, consistent with health promotion theory, the GoodNEWS curriculum teaches lifestyle principles, defined as consistent patterns of interrelated behaviors, based on cultural heritage, social relationships, geographic and socioeconomic circumstances, and personality [53]. According to health promotion theory, supportive environments have the greatest impact on producing lasting lifestyle changes [53]. The proposed project tests the effectiveness of a supportive environment on producing lasting health behavior changes in minority communities [37].
In addition to wellness principles, the curriculum addresses basic anatomy and disease processes, and the relationship between living styles and cardiovascular disease (Table 3 shows the nine core training modules). The LHPs are taught the social concepts related to health, namely, that health depends on factors within (what we eat and drink) and beyond (social and political policies) the individual’s immediate control. They are also taught the parallel concepts from science — wellness depends on a balance between genetic functions (internal dimensions) and the environmental context (external dimensions). By blending social and scientific concepts related to health, the GoodNEWS approach teaches participants how to send healthy messages to their genes, by participating in healthy lifestyles within the limitations of their external conditions or environment. The training program consists of about 24 h of didactic and interactive workshop sessions delivered on two consecutive weekends. LHPs completing the training program participate in a graduation ceremony and receive a Certificate of Program Completion.
Table 3.
Nine core lay health promoter training modules.
| Number | Title and content |
|---|---|
| 1 | Understanding cardiovascular disease |
| 2 | Healthful living principles |
| 3 | Nutrition principles |
| 4 | Physical fitness and activity |
| 5 | Spirituality and health |
| 6 | Mental health principles |
| 7 | Social and environmental health |
| 8 | Health resources in the community |
| 9 | Health ministry development |
2.2.3. Intervention and study groups
Once LHPs complete the GoodNEWS training program, congregations are randomized to one of two conditions —GoodNEWS-I or GoodNEWS-PA. All LHPs regardless of group assignment work within their congregation to develop a GoodNEWS Health Ministry (committee) and a GoodNEWS Wellness Club for engaging a sample of interested congregation members in health promotion activities. These “Wellness Club Members (WCMs)” do not belong to a physical health club structure, but are committed members of the congregation connected to one another by their common desire to improve their health through lifestyle events sponsored by their congregation’s GoodNEWS Health Ministry. The wellness clubs are intended to be “health clubs without walls” where people can come together to learn health promotion and disease prevention skills, and then work together to develop activities and programs in their congregation.
The LHPs from congregations randomized to GoodNEWS-I participate in a monthly education seminar series for presenting and discussing information related to community-based CVD health promotion and accessing community-based health resources (Table 4). Seminars provide an opportunity for LHPs, physicians and other health professionals, and representatives from community service organizations, to participate in a community-based dialog sharing multiple perspectives about the requirements for preventing CVD. GoodNEWS-I LHPs and WCMs also participate in quarterly health education events such as healthy activities challenges, health screening events, community walks, health and prayer breakfasts, and other activities for reducing CVD risk. They also have access to the members-only GoodNEWS website for sharing information about group activities and events, links to local and national patient education resources, GoodNEWS training modules, healthy recipes and physical activity tips, and an electronic version of the GoodNEWS quarterly newsletter (The Faith-Health Connection).
Table 4.
Content of intervention vs. control group.
| Area | Activities | Intervention | Control |
|---|---|---|---|
| Measurement | Baseline | Yes | Yes |
| Structured program support | Congregational assessment survey | Yes | Yes |
| Monthly lay health promoter meetings with structured health education curriculum | Yes | No | |
| Quarterly health education events | Yes | No | |
| Community engagement | Lay Health Promoters and Pastors eligible for GoodNEWS advisory board | Yes | Yes |
| Community Health Revival to share success stories, celebrate program | Yes | Yes | |
| Contact with program team | Monthly correspondence | Yes | Yes |
| Monthly newsletter | Yes | Yes | |
| Access to community resources recommended by team | Yes | Yes | |
| Access to program main website | Yes | Yes | |
| Access to program website intervention-group only area | Yes | No | |
| Measurement | 18-month follow-up | Yes | Yes |
NOTE: All program activities will be open to both groups after 18-month follow-up measurements.
The GoodNEWS-PA LHPs and WCMs receive a monthly generic newsletter prepared by program staff and investigators, which is relevant to the health needs of the community. The LHPs also receive a monthly phone call from the GoodNEWS program coordinator in order to keep them interested and engaged in the project and to answer questions. Similar to the GoodNEWS-I LHPs, the GoodNEWS-PA LHPs are asked to promote health and develop health programs in their congregations’ for 18 months, before being asked to join the combined study.
2.2.4. Recruitment
2.2.4.1. Congregation and Lay Health Promoter (LHP) recruitment
Consistent with the tenets of CBPR, the recruitment plan was developed through discussion among program staff and the GoodNEWS Pastors Advisory Council (PAC), a group of local Church Pastors who had participated in GoodNEWS pilot studies from 2002 to 2005. Congregations were recruited through personal contacts of the PAC members, radio advertisements, personal appearances by program staff on radio talk shows, and membership lists from local religious organizations and conferences. An independent recruitment consultant who lived in and had connections throughout the target community, implemented and supervised the recruitment strategy.
After broadly disseminating information about the program throughout the target area congregations, Pastors from the target area congregations were invited to a luncheon at the local African-American Museum where the GoodNEWS training program and study were explained. Interested Pastors were asked to sign a Memorandum of Understanding (MOU) outlining the responsibilities of the congregation and program staff during the study period. They were also asked to designate two members of their congregation to be trained as Lay Health Promoters (LHPs), and to forward the names and contact information of these individuals to the program staff within 2 weeks. In order to guide their selection, Pastors were provided with a document describing LHP qualifications and responsibilities; for example, LHPs must be knowledgeable about and active in the congregation, dedicated to their own personal health improvement, have good organizational skills, value confidentiality, and be committed to the welfare of others. Pastors also made a commitment to participate in a one-half day Saturday morning workshop, for providing them with training in the basics of cardiovascular health and the role of the Church in health promotion.
2.2.4.2. Sampling and recruitment
The first official responsibility of the LHPs after completing training was to administer a Congregational Health Assessment among a convenience sample of congregation members. The assessments are a paper and pencil tool in the form of a six-page booklet, consisting of three sections: general demographics, personal and family medical history, and a section asking members their preferences for the types of health promotion programs in which they would participate if they were available in their congregation. They are administered during a 15-minute pause in the Sunday worship service with instructions given by the Pastor and the LHPs. A report based on the aggregated results of the assessment and describing the primary health problems and program preferences of the congregation members, was developed by the program staff and is shared by the LHPs with the Pastor and other church leaders.
The program coordinator and health educator then collaborated with the LHPs to develop a GoodNEWS Recruitment Toolkit for enrolling individual congregation members into the study. The toolkit consisted of documents providing information about the study, an overview of how to contact congregation members and conduct a GoodNEWS program information session, frequently asked questions, and assorted promotional materials and incentives for congregation members to participate in the program. All of the toolkit materials were contained in a small colorful box printed with the GoodNEWS logo, and they were distributed to the LHPs on a designated evening at one of the participating churches that was centrally located and well known throughout the community.
The project coordinator met once with potential study participants recruited by the LHPs at each church during the month preceding the baseline measurements. The purpose of the meetings was uniformity in the consent process and answering questions about the project. Those church members interested in participating signed Letters of Commitment (Table 2). Those who were interested but not able to attend the informed consent sessions at the church meetings were allowed to go through the consent process on the day of the baseline measurements. Reminder strategies to catch up with this second wave of participants were used to enhance attendance at the baseline measurement event. These strategies consisted of announcements by the Pastors and LHPs, postcards, and phone calls. Once congregation members completed baseline measurements, they were designated as Wellness Club Members (WCMs), and the objective of the study was for the LHPs to share health information on an ongoing basis with the WCMs and develop programs in their congregation that would be directed at improving the health of their WCMs. The only inclusion/exclusion criteria for becoming a WCM (e.g. study participant) were motivation to participate in the 36-month project (18-month clinical trial and 18-month maintenance period) and belonging to one of the congregations in the study.
2.2.5. Measurement
2.2.5.1. Planning the measurement event
Baseline measurement planning was directed by a community-event planner, with the assistance of the project coordinator and program staff. The measurement event planning began approximately 4 months in advance of the measurement event, by developing a planning document and timeline outlining logistics related to: event venue, supplies and equipment, recruiting volunteers and staffing, training and coordination, expenses and payment scheduling, transportation, child care, and marketing and communications. The timeline outlined the specific activities and logistics, responsible party, start date for planning and finish date for completing, and the status updated on a weekly basis.
2.2.5.2. Location and dates of measurement
Measurement was based at Friendship West Baptist Church, a mega-church that was also participating in the study. The Church is well known throughout the City of Dallas, has modern and updated meeting space, is centrally located and accessible by car or bus, and was available at a reasonable cost for four measurement dates. Measurement events were conducted between 7:30 a.m. and 12:30 p.m. on two Saturdays (September 13, 2008 and September 20, 2008) and two Wednesdays (September 17, 2008 and September 24, 2008), in order to provide alternative measurement times for participants’ time conflicts due to work and home care responsibilities. A back-up measurement event was also conducted on October 8th, 2008 at Community Missionary Baptist Church, a large congregation participating in the study.
2.2.6. Volunteer recruitment and training
Recruitment of volunteers to assist with baseline data gathering was the combined responsibility of the project coordinator, the co-investigators in charge of measurements, and the LHPs. Recruitment efforts began three (3) months in advance of the measurement events, through electronic messages and word of mouth. Electronic reminders were sent 4 weeks before the measurement events requesting participation in one of two training sessions for those volunteers signing up for the measurement stations. The purpose of the training was to have a standardized approach to data collection. Each session started with a general description of the objectives of the study to impress upon the volunteers that they were participating in a research study as opposed to a health fair. Volunteers were asked to select a single station – blood pressure, blood draw, weight and height, diet history, or physical activity – to receive training. Once one of the stations was chosen, the group of volunteers received instructions on how to operate the equipment or questionnaire at that particular station and how to record the results. Each station was directed by one of the project’s co-investigators, who developed a training protocol and certification process for their station’s volunteers. While the exact certification process differed for each station depending on the level of knowledge and experience required of the volunteers, volunteers at all stations had to successfully perform the station function in front of the director in order to be certified for the measurement event.
3. Results
3.1. Recruitment
3.1.1. Recruitment of congregations
Fig. 2 shows a timeline displaying the sequence of church enrollment, individual participant enrollment, and randomization. By April 2008, 23 congregations had enrolled in the project and signed commitment letters to attend the LHP training program. Thirteen congregations’ LHPs completed the training program; 10 did not show up and a second training program was scheduled the following month for this group. Five of those not showing up initially and two additional congregations completed the training for a total of 20 congregations. Two congregations elected to discontinue participation after receiving training, leaving a total of 18 GoodNEWS participating congregations. Participating congregations range in size from 100 to 11,000 members. The mean congregation size is 1153 members and the median is 225 members.
Fig. 2.
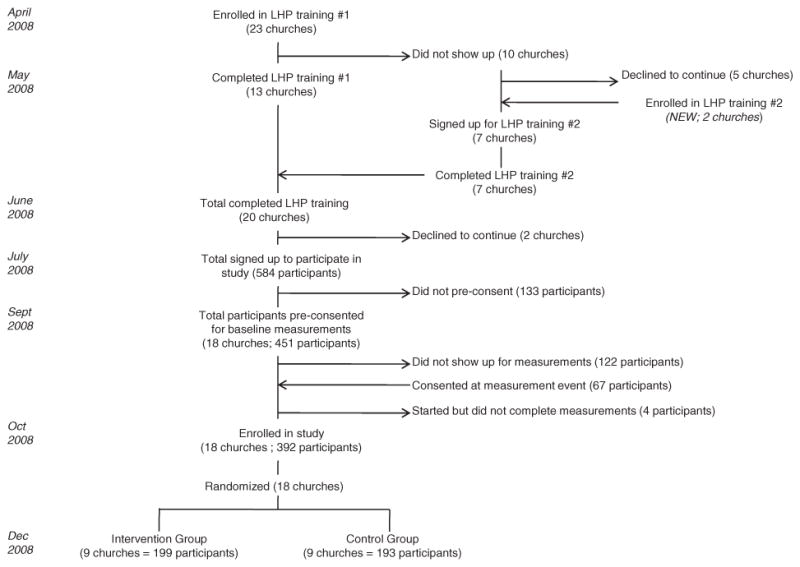
Recruitment of congregations and Lay Health Promoters down to participants. The figure illustrates the recruitment process for the GoodNEWS congregations and lay health promoters from April 2008 to December 2008.
3.1.2. Recruitment of patients
A total of 584 individuals originally signed letters of commitment for enrolling as study participants (e.g. Wellness Club Members) in their respective congregations (Fig. 2). Four hundred and fifty one (451) gathered at the 18 churches and consented to participate in the study during the month preceding the baseline measurement events. Of these 451 potential participants, 122 did not show up for the measurements. However, 67 additional participants did show up, signed a consent form, and participated in the measurement event. Although measurements were started on 396 participants, 4 of them provided only partial data leaving a total of 392 participants who completed all baseline measurements during 5 days (three Saturdays and two Wednesdays). Each church contributed between 9 and 45 consenting individuals (Table 2). Ten of the churches contributed 20 individuals or less.
3.1.3. Recruitment of volunteers
One hundred-twenty eight (128) individuals volunteered to assist with conducting the five (5) measurement events and ninety-three (93) of these attended one of the two training sessions. Most volunteers (N=75) were students, residents, fellows, and faculty members from the Schools of Medicine, Nursing, and Nutrition at UT Southwestern Medical Center. They administered blood pressure, point of care testing, anthropometrics, and the diet history and physical activity questionnaires. Fifty-three (53) volunteers from churches and the community volunteered to participate in event registration, child care, and facilitators for guiding participants through five measurement stations. Thirty-five (35) volunteers showed up at the measurement event without previous training; they were trained (and certified when appropriate) early in the morning before evaluation of participants began and were paired with a volunteer who attended the formal training session. All volunteers and study staff were identified by a T-shirt with the GoodNEWS study logo and an identification badge.
3.2. Baseline measurements
Three hundred and ninety six (396) individuals participated in the measurement event, and three-hundred ninety-two (392) completed all of the baseline assessments including: demographics, health beliefs, history of cardiovascular risk factors, nutrition, physical activity, anthropometrics, blood pressure, and point of care testing for lipids, glucose, and HbA1c. Most participants were African-American women in their late thirties to early sixties, employed, and with more than a high school diploma (Table 5). The groups were similar for the primary outcome variables saturated fat intake and metabolic equivalent of tasks (METS) per day, and other risk factors for CVD.
Table 5.
Baseline characteristics of intervention vs. control group.
| Category | Variable | Intervention (N=199) | Control (N=193) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Gender | Male | 36 (18.09) | 48 (24.87) | 0.1019 |
| Female | 163 (81.91) | 145 (75.13) | ||
| Race/ethnicity | Black/African-American | 197 (99.49) | 190 (98.96) | n/a |
| Marital status | Married | 89 (44.72) | 111 (57.51) | 0.1907 |
| Unmarried | 110 (55.28) | 82 (42.49) | ||
| Education | High school or less | 61 (30.65) | 47 (24.35) | 0.4691 |
| Some college | 58 (29.15) | 72 (37.31) | ||
| College degree | 80 (40.20) | 74 (38.34) | ||
| Employment | Employed | 145 (72.86) | 134 (69.43) | 0.4691 |
| Not employed | 54 (27.14) | 59 (30.57) | ||
| Primary variables | ||||
| METS per day* | 34.74 (4.28) | 34.87 (5.25) | 0.7851 | |
| Food energy (kcal) | 1968.8 (1584.8) | 2035.2 (1559.2) | 0.3259 | |
| Protein (g) | 83.14 (63.97) | 72.94 (55.00) | 0.0933 | |
| Total fat (g) | 83.53 (65.59) | 76.28 (62.56) | 0.2671 | |
| Saturated fat (g)* | 26.14 (23.33) | 23.69 (20.24) | 0.2708 | |
| Cholesterol | 253.59 (227.15) | 217.95 (189.25) | 0.0945 | |
| Total trans fatty acids | 5.60 (5.03) | 5.13 (4.75) | 0.3404 | |
| Secondary variables | ||||
| Average systolic blood pressure* | 128.11 (20.41) | 126.21 (18.40) | 0.4046 | |
| Average diastolic blood pressure* | 79.23 (10.08) | 79.88 (9.81) | 0.5789 | |
| High-density lipoprotein* | 47.31 (16.15) | 46.72 (15.22) | 0.3280 | |
| Low-density lipoprotein* | 109.70 (41.55) | 109.90 (39.59) | 0.2729 | |
| Triglyceride* | 123.10 (76.68) | 117.80 (88.92) | 0.4202 | |
| Total cholesterol* | 178.86 (44.72) | 180.90 (42.00) | 0.7064 | |
| Hemoglobin A1C* | 6.16 (1.02) | 6.17 (1.36) | 0.2144 | |
| Body Mass Index* | 34.57 (8.11) | 33.49 (8.26) | 0.2589 | |
| Waist-to-hip ratio | 0.88 (0.07) | 0.87 (0.08) | 0.6150 | |
4. Discussion
In the GoodNEWS trial we have used a CBPR approach for reducing the risk of CVD among African-American individuals in the congregational setting. Our experience provides valuable lessons related to four specific challenges we encountered conducting a clinical trial in the community setting. Typically, CBPR challenges tend to revolve around the interpersonal dynamics of reconciling academic and community priorities — e.g. developing equitable social relationships between researchers and community stakeholders, building trust between the partners, sharing power, and developing open communication [54,55]. However, since the GoodNEWS program has existed in the target community since 2003, the academic-community partners had already developed a robust partnership by the time the trial began in 2007 and the challenges tended to be more related to actually implementing the trial rather than developing or navigating relationships.
The first challenge faced by the team was recruiting congregations to participate in the study. The original recruitment plan proposed: 1) identifying eligible congregations using an existing directory of 800 area congregations as the sampling frame, 2) sending a program brochure and letter of invitation from the GoodNEWS Pastor’s Advisory Council (PAC) to the Pastors of eligible congregations, 3) contacting Pastors with a phone call from program staff and a follow-up phone call from a member of the PAC, and, 4) extending an invitation to an informational luncheon, where the program and the study would be described and interested Pastors could sign a letter of intent to participate. However, the process took almost twice as long to complete as we had planned; many times Pastor’s beyond the immediate circle of our PAC member friendships requested face-to-face meetings before coming to an informational session, we had difficulty getting our information on the agenda of local church congregation associations since the agendas were sometimes made several months in advance, and holidays such as Thanksgiving and Christmas fell in the middle of the recruitment period.
In light of the slower than expected pace of recruitment, we contracted with a local community consultant to help us revise our recruitment plan. The consultant began contacting congregations on our behalf, arranged for the principal investigator and senior research nurse (who were already well known in some segments of the community) to appear on local radio shows to discuss the project, and arranged for local community newspapers to run feature stories on the project. Although the revised strategy was ultimately successful, in retrospect – even though the program staff had strong existing relationships in the community – we would have likely saved time and improved efficiency by contracting with a local social networking consultant at the outset of the recruitment period.
The second unanticipated complication was the need to conduct two LHP training sessions, rather than only the one that had been planned originally. Only 13 of the 23 (57%) congregations recruited and scheduled to participate in the training program actually did participate as scheduled, and five of the ten who did not participate eventually declined continued participation altogether. Most of the reasons given for not participating in the scheduled training were related to personal problems encountered by the LHPs themselves, such as loss of a family member, illness, or some other unforeseen circumstance, or a feeling that they had overcommitted and did not realize the full extent of their commitment. Although, LHPs and their Church Pastors’ had been informed repeatedly in person, on the telephone, and through email, it was clear that some of the participants still did not have a clear understanding of the program requirements.
The need for extending recruitment and conducting a second training program produced both negative and positive effects. On the negative side, it contributed to another recruitment-related delay to the project timeline. However, on the positive side it allowed the project team to become very familiar with the training materials and to begin working together more closely before randomization and putting the intervention in place. The delay contributed to bonding the team members more closely together, and to developing a positive team culture related to addressing and overcoming the challenges of working with people in the real-world community setting. In future programs we plan to convene all of the community partners’ leaders – LHPs, Pastors, and other relevant church staff – to fully understand each other’s commitments and responsibilities. Although we had explained these components with the Pastor and the LHPs in the group setting, the extra time needed for conducting individual meetings in congregations, might be more efficient and less time consuming in the long run than extending the recruitment process and conducting another LHP training session.
The third challenge we encountered was related to planning the community-based measurement events, which was more complicated than originally envisioned. Since the events were based in the community, they required storage space for the measurement materials – including refrigeration – throughout the four-week measurement period. Additionally, separate rooms were needed for each measurement station, kitchen facilities were needed for providing a light breakfast since fasting glucose measurements were obtained, accessibility by car and bus was needed (along with parking), and crowd flow inside the event venue. When the program staff began planning the event it became clear to us that we would need the advice of a professional event planner familiar with the target community and suitable venues. The relatively modest amount of funding required for contracting with an event planner is highly recommended; the arrangement allowed the project staff to focus measurement planning needs while allowing the event planner to focus on the community and venue interface. The major consideration we learned from the event planner is the importance of developing a crowd-flow plan for a five-hour event when a large group of participants is expected to arrive at the same time, and when some of them will require immediate measurement and breakfast related to their medication schedule. Event planners are trained in and experienced with anticipating and accommodating these needs, and the joint planning between an experienced community event planner and CBPR project manager provided an excellent partnership for conducting a highly efficient community-based measurement event.
The final challenge that was not anticipated by the event planner or the research team was the need for conducting an additional measurement event beyond the four that were already schedule. We expected that two Saturday and two Wednesday events, would allow sufficient time and planning for all enrolled WCMs to attend regardless of conflicting schedules. The additional measurement event was needed even after advertising the measurement dates for 3 months in advance through personal meetings at the churches attended by program staff, telephone calls to the LHPs who then contacted by phone their respective WCMs, announcements in the church bulletins, announcements by the Pastor from the pulpit on Sunday mornings, and bi-weekly emails delivered to those who enrolled during their churches’ recruitment events. Our experience indicates that participants need to be instructed even more thoroughly about their roles and responsibilities, and the instruction needs to be reinforced beyond providing event reminders.
The experience of the GoodNEWS trail indicates that it is necessary when conducting community program and measurement events, to schedule back-up or contingency events as part of the planning process. Research requirements – no matter how well explained, planned, executed, or important from the research perspective – do not easily fit into the planning calculus and timeline of community members. Our experience also supports the need for incorporating non-traditional community-based staff into the design and operational plan of CBPR trials, including a community recruitment consultant and event planner. Even though two members of the core project team were actually from the target community, having a consultant and event planner from within the target community provides even greater insight into the pace and process of integrating a clinical trial into the community context and greatly improves efficiency.
Acknowledgments
The authors would like to thank Ms. Froswa Booker-Drew and Ms. Charlene Edwards for their contributions to this project, as well as Nicole Beltran, MBA for her capable and significant contribution to manuscript oversight and preparation. We would also like to acknowledge the contribution of the GoodNEWS Advisory Board, the Pastor’s Advisory Council, the Wellness Club Members, and the following participating congregations and their Pastors: Beth-Eden BC, Bible Way BC, Changing Directions Christian Center, Community Missionary BC, Concord Missionary BC, First CME, Friendship West BC, Goodwill BC, Greater Harvest Church of God in Christ, Heartline Ministries, Mt. Moriah Missionary BC, New Friendship BC, New Millennium Bible Fellowship, New Mt. Moriah Missionary BC, Northpark Missionary BC, Singing Hills BC, St. Matthew C.I.L. Missionary BC, Tabernacle Missionary BC, Promised Land Missionary BC, Cornerstone BC, Faith Cumberland Presbyterian, Faith Memorial, Frazier Berean BC, Greater New Zion BC, St. Mark BC, True Lee Missionary BC, Warren Avenue Christian, Warren United Methodist, and Zion Chapel Primitive BC. Finally, the GoodNEWS Lay Health Promoters have worked tirelessly and at great personal expense of their time and talent, to implement the GoodNEWS program in a way that will reduce the risk of CVD among their fellow congregants and we are very grateful to them for their efforts.
Footnotes
Funding was provided by the National Heart, Lung and Blood Institute (NHLBI) of the National Institutes of Health (NIH), Grant number: RO1 HL087768.
References
- 1.Clark LT. Issues in minority health: atherosclerosis and coronary heart disease in African Americans. Med Clin North Am. 2005;89(5):977–1001. doi: 10.1016/j.mcna.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 2.Heart Disease and Stroke Statistics - 2006 Update. Dallas, Texas: American Heart Association; 2006. [Google Scholar]
- 3.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–41. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 4.Bravata DM, Wells CK, Gulanski B, Kernan WN, Brass LM, Long J, et al. Racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke. 2005;36(7):1507–11. doi: 10.1161/01.STR.0000170991.63594.b6. [DOI] [PubMed] [Google Scholar]
- 5.Racial/ethnic and socioeconomic disparities in multiple risk factors for heart disease and stroke–United States, 2003. MMWR. 2005;54(5):113–7. [PubMed] [Google Scholar]
- 6.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165(18):2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 7.NIH. Addressing Health Disparities: The NIH Program of Action. 2005. [Google Scholar]
- 8.DHHS. Preventing Chronic Diseases: Investing wisely in health. 2005. [Google Scholar]
- 9.Haskell WL. Cardiovascular disease prevention and lifestyle interventions: effectiveness and efficacy. J Cardiovasc Nurs. 2003;18(4):245–55. doi: 10.1097/00005082-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation July. 2006;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. [DOI] [PubMed] [Google Scholar]
- 11.Brenner B. Implementing a community intervention program for health promotion. Soc Work Health Care. 2002;35(1–2):359–75. doi: 10.1300/J010v35n01_02. [DOI] [PubMed] [Google Scholar]
- 12.Farris RP, Haney DM, Dunet DO. Expanding the evidence for health promotion: developing best practices for WISEWOMAN. J Womens Health. 2004;13(5):634–43. doi: 10.1089/1540999041281098. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Intervention Strategies from Social and Behavioral Research. Washington: National Academy of Sciences; 2000. [Google Scholar]
- 14.Wandersman A. Community science: bridging the gap between science and practice with community-centered models. Am J Community Psychol. 2003;31(3–4):227–42. doi: 10.1023/a:1023954503247. [DOI] [PubMed] [Google Scholar]
- 15.Merzel C, D’Afflitti J. Reconsidering community-based health promotion: promise, performance, and potential. Am J Public Health. 2003;93 (4):557–74. doi: 10.2105/ajph.93.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorensen G, Emmons K, Hunt MK, Johnston D. Implications of the results of community intervention trials. Annu Rev Public Health. 1998;19:379–416. doi: 10.1146/annurev.publhealth.19.1.379. [DOI] [PubMed] [Google Scholar]
- 17.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 18.Giachello AL, Arrom JO, Davis M, Sayad JV, Ramirez D, Nandi C, et al. Reducing diabetes health disparities through community-based participatory action research: the Chicago Southeast Diabetes Community Action Coalition. Public Health Rep. 2003;118(4):309–23. doi: 10.1016/S0033-3549(04)50255-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Israel BA, Parker EA, Rowe Z, Salvatore A, Minkler M, Lopez J, et al. Community-based participatory research: lessons learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environ Health Perspect. 2005;113(10):1463–71. doi: 10.1289/ehp.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minkler M, Blackwell AG, Thompson M, Tamir H. Community-based participatory research: implications for public health funding. Am J Public Health. 2003;93(8):1210–3. doi: 10.2105/ajph.93.8.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Fallon LR, Dearry A. Community-based participatory research as a tool to advance environmental health sciences. Environ Health Perspect. 2002;110(Suppl 2):155–9. doi: 10.1289/ehp.02110s2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corbie-Smith G, Ammerman AS, Katz ML, St George DM, Blumenthal C, Washington C, et al. Trust, benefit, satisfaction, and burden: a randomized controlled trial to reduce cancer risk through African-American churches. J Gen Intern Med. 2003;18(7):531–41. doi: 10.1046/j.1525-1497.2003.21061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ammerman A, Corbie-Smith G, St George DM, Washington C, Weathers B, Jackson-Christian B. Research expectations among African American church leaders in the PRAISE! project: a randomized trial guided by community-based participatory research. Am J Public Health. 2003;93(10):1720–7. doi: 10.2105/ajph.93.10.1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sloane DC, Diamant AL, Lewis LB, Yancey AK, Flynn G, Nascimento LM, et al. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med. 2003;18(7):568–75. doi: 10.1046/j.1525-1497.2003.21022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Angell KL, Kreshka MA, McCoy R, Donnelly P, Turner-Cobb JM, Graddy K, et al. Psychosocial intervention for rural women with breast cancer: The Sierra-Stanford Partnership. J Gen Intern Med July. 2003;18(7):499–507. doi: 10.1046/j.1525-1497.2003.20316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox CE, Morford TG, Fine A, Gibbons MC. The Johns Hopkins Urban Health Institute: A collaborative response to urban health issues. Acad Med. 2004;79(12):1169–74. doi: 10.1097/00001888-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Israel BA, McLeroy KR. Social networks and social support: implications for health education. Introduction Health Educ Q. 1985;12(1):1–4. doi: 10.1177/109019818501200101. [DOI] [PubMed] [Google Scholar]
- 28.Eng E, Young R. Lay health advisors as community change agents. Fam Community Health. 1992;15:24–40. [Google Scholar]
- 29.Chatters LM, Levin JS, Ellison CG. Public health and health education in faith communities. Health Educ Behav. 1998;25(6):689–99. doi: 10.1177/109019819802500602. [DOI] [PubMed] [Google Scholar]
- 30.Foege WH, O’Connell U. A Role for America’s Religious Communities. Chicago: 1990. [Google Scholar]
- 31.Hale WD, Richard GB. Building Healthy Communities Through Medical -Religious Partnerships. Baltimore London: Catherine J. McGinniss Family Foundation; 2000. [Google Scholar]
- 32.Thomas SB, Quinn SC, Billingsley A, Caldwell C. The characteristics of northern black churches with community health outreach programs. Am J Public Health. 1994;84(4):575–9. doi: 10.2105/ajph.84.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tuggle RM. It is well with my soul. Washington D.C: Magnificent Publications, Inc; 2000. [Google Scholar]
- 34.Sutherland M, Hale CD, Harris GJ. Community health promotion: The church as partner. J Primary Prevent. 1995;25(16):201–17. doi: 10.1007/BF02407340. [DOI] [PubMed] [Google Scholar]
- 35.Oexmann MJ, Thomas JC, Taylor KB, O’Neil PM, Garvey WT, Lackland DT, et al. Short-term impact of a church-based approach to lifestyle change on cardiovascular risk in African Americans. Ethn Dis. 2000;10(1):17–23. [PubMed] [Google Scholar]
- 36.Ades PA, Kottke TE, Miller NH, McGrath JC, Record NB, Record SS. Task force #3–getting results: who, where, and how?. J Am Coll Cardiol; 33rd Bethesda Conference; 2002. pp. 615–30. [DOI] [PubMed] [Google Scholar]
- 37.Benjamin EJ, Smith SC, Jr, Cooper RS, Hill MN, Luepker RV. Task force #1–magnitude of the prevention problem: opportunities and challenges. J Am Coll Cardiol; 33rd Bethesda Conference; 2002. pp. 588–603. [DOI] [PubMed] [Google Scholar]
- 38.Diet History Questionnaire. 2007. [Google Scholar]
- 39.Blair SN, Haskell WL, Ho P, Paffenbarger RS, Jr, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 40.Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exer. 1997;29(6 Suppl):S1–S205. [PubMed] [Google Scholar]
- 41.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281(4):327–34. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 42.Donner A, Klar N. Statistical considerations in the design and analysis of community intervention trials. J Clin Epidemiol. 1996;49(4):435–9. doi: 10.1016/0895-4356(95)00511-0. [DOI] [PubMed] [Google Scholar]
- 43.Feng Z, Diehr P, Peterson A, McLerran D. Selected statistical issues in group randomized trials. Annu Rev Public Health. 2001;22:167–87. doi: 10.1146/annurev.publhealth.22.1.167. [DOI] [PubMed] [Google Scholar]
- 44.Singer J. Using SAS PROC MIXED to Fit Multilevel models, Hierarchical Models, and Individual Growth Models. J Educ Behav Stat. 1998;24(4):323–55. [Google Scholar]
- 45.DeHaven MJ, Hunter IB, Wilder L, Walton JW, Berry J. Health programs in faith-based organizations: are they effective? Am J Public Health. 2004;94(6):1030–6. doi: 10.2105/ajph.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–84. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 47.Kuhajda MC, Cornell CE, Brownstein JN, Littleton MA, Stalker VG, Bittner VA, et al. Training community health workers to reduce health disparities in Alabama’s Black Belt: the Pine Apple Heart Disease and Stroke Project. Fam Community Health. 2006;29(2):89–102. doi: 10.1097/00003727-200604000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Carmody K, Berge Z. Elemental analysis of the online learning experience. Int J Educ Dev. 2005;1(3) [Google Scholar]
- 49.Myers JE, Sweeney TJ, Witmer JM. The Wheel of Wellness Counseling for Wellness: A Holistic Model for Treatment Planning. J Couns Dev. 2000;78:251–66. [Google Scholar]
- 50.Hettler W. Wellness: Encouraging a lifetime pursuit of excellence. Health Values. 1984;8:13–7. [PubMed] [Google Scholar]
- 51.Morland K, Wing S, ez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–9. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 52.Sallis JF, Hovell MF, Hofstetter CR, Elder JP, Hackley M, Caspersen CJ, et al. Distance between homes and exercise facilities related to frequency of exercise among San Diego residents. Public Health Rep. 1990;105(2):179–85. [PMC free article] [PubMed] [Google Scholar]
- 53.Green L, Kreuter M. Health Promotion Planning: An Educational and Environmental Approach. 2. Mountain View: Mayfield Publishing Co; 1991. [Google Scholar]
- 54.Seifer SD, Sisco S. Mining the challenges of CBPR for improvements in urban health. J Urban Health. 2006;83(6):981–4. doi: 10.1007/s11524-006-9112-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Strickland CJ. Challenges in community-based participatory research implementation: experiences in cancer prevention with Pacific Northwest American Indian tribes. Cancer Control. 2006;13(3):230–6. doi: 10.1177/107327480601300312. [DOI] [PubMed] [Google Scholar]