Abstract
Context
Although depression frequently co-occurs with substance abuse, few individuals entering substance abuse treatment have access to effective depression treatment.
Objective
The Building Recovery by Improving Goals, Habits and Thoughts (BRIGHT) study is a community-based effectiveness trial that compared residential substance abuse treatment to residential treatment plus group cognitive behavioral therapy (CBT) for depression delivered by substance abuse treatment counselors. The authors hypothesized that intervention clients would have improved depression and substance use outcomes as compared to clients receiving usual care.
Design
A nonrandomized controlled trial using a quasi-experimental intent-to-treat design in which four sites were assigned to alternate between the intervention and usual care conditions every four months over a two-and-a-half-year period.
Setting
Four treatment programs in Los Angeles County
Participants
1,262 clients were screened for persistent depressive symptoms (Beck Depression Inventory-II (BDI-II) >17). 299 clients were assigned to receive either usual care (N=159) or usual care plus the intervention (N=140). Follow-up rates at three and six months after the baseline interview were 88.1% and 86.2% for usual care and 85.7% and 85.0% for the intervention group.
Intervention
Sixteen two-hour group sessions of CBT for depression
Main Outcome Measures
Change in depression symptoms, mental health functioning, and days of alcohol and substance use.
Results
BRIGHT clients reported significantly fewer depressive symptoms (p<0.001 at three and six months) and had improved mental health functioning (p<0.001 at three-months and p<0.01 at six months). At six months, BRIGHT clients reported fewer drinking days (p<0.05) and fewer days of problem substance use (p<0.05) on days available.
Conclusions
Providing group CBT for depression to clients with persistent depressive symptoms receiving residential substance abuse treatment is associated with improved depression and substance use outcomes. These results provide support for a new model of integrated care.
Introduction
Depression and substance abuse are the second and fourth most common mental disorders1, 2 and are leading causes of disability, reduced quality of life, and adverse social consequences.3 Frequently occurring together, individuals with co-occurring depression and substance abuse rarely receive treatment for both disorders.4 The consequences of this unmet need are great. Individuals with co-occurring depression and substance abuse overutilize high-cost, crisis-oriented services, and the interactive nature of the two disorders leads to poorer depression and substance abuse treatment outcomes than when only one disorder is treated.5, 6
There is a growing consensus that for the large group of individuals whose psychiatric symptoms do not remit with abstinence, treatment for both the substance abuse and mental disorder should be provided, and the treatments should be integrated at the clinical interface.7, 8 Despite the need for effective treatments, there is little research on psychosocial treatments for patients with co-morbid depression and substance use disorders.
Group cognitive behavioral therapy (CBT) is an effective treatment for depression.9, 10 The Building Recovery by Improving Goals, Habits and Thoughts (BRIGHT) study was a non-randomized community-based effectiveness trial11 that developed and evaluated a 16-session group CBT for depression. The intervention was designed to be feasible for use in residential substance abuse treatment settings and to be delivered by typical substance abuse counselors. The BRIGHT study compared the effectiveness of residential treatment to residential treatment plus the BRIGHT intervention. We hypothesized that clients receiving the intervention would have improved depression and substance use outcomes.
Methods
We used a non-randomized, quasi-experimental design in which cohorts of clients at each of the study sites received either residential treatment as usual (UC) or residential treatment enhanced with the BRIGHT intervention (BRIGHT) provided by trained substance abuse counselors over a two-and-a-half-year enrollment period. Study sites were the four residential sites operated by Behavioral Health Services (BHS), one of the largest publicly-funded substance abuse treatment providers in Los Angeles County.
Study Design
We used an alternating assignment process. During the first four-month period, all eligible clients from the largest site were assigned to the experimental condition (BRIGHT), while all eligible clients from the other three smaller sites were assigned to the comparison condition (UC). After four months this assignment pattern alternated and all clients from the three smaller sites were assigned to the experimental condition, while clients from the largest site were assigned to UC. This alternating pattern continued over a two-and-a-half-year enrollment period with the intervention delivered a total of 15 times. In the last year of the study for logistical reasons we centralized the delivery of the intervention at a single site; instead of the outpatient counselors travelling to the residential sites, intervention clients were transported to a single site to receive the intervention. While a randomized design would have been a stronger test of causality, the logistics of a randomized design were not feasible.
Participants and Enrollment
Study recruitment began in August 2006 and ended in January 2009. During that period a total of 1,262 clients were screened for eligibility and 299 clients with persistent depressive symptoms were enrolled (Figure 1). We defined persistent symptoms as symptoms that were measured on two separate occasions after at least two weeks of sobriety. Clients were first screened by residential staff using the Patient Health Questionnaire (PHQ-8)12 14 days after entering treatment. Clients with a score 5 or greater (corresponding to at least mild depression symptoms) were asked whether research staff could contact them. Fifty-nine percent of the clients screened at two weeks scored five or greater on the PHQ-8. Next, the research team conducted a second screening to determine eligibility; 9% of the sample refused the second screening or their contact information was lost, and 5% were discharged from the program before the second screening. Inclusion criteria at the second stage were 1) Beck Depression Inventory-II (BDI-II) scores >17, indicative of moderate to severe depressive symptoms,13, 14 2) the ability to speak and understand English, and 3) receiving residential treatment. Exclusion criteria included a positive screen for a self-reported bipolar disorder 15, schizophrenia (one item from the Healthcare for Communities Psychoticism screener) and cognitive impairment 16. We did not enroll clients on federal probation or parole, as we were unable to obtain permission from the Federal Parole Board.
Figure 1.
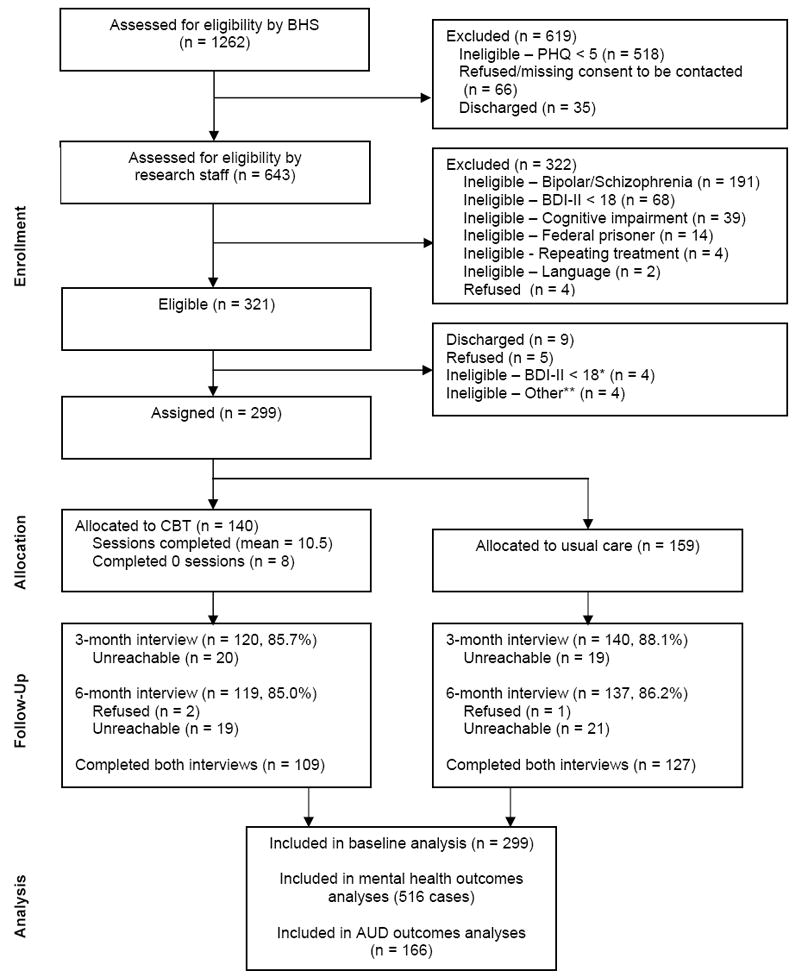
Study Enrollment Process
* If more than a 2 week period passed between the assessment for eligibility by research staff and the baseline interview, clients were re-assessed for persistent depressive symptoms using the BDI-II.
** If client had other known commitment (e.g., court date, pregnancy, specialty group) that would prevent them from attending intervention, they were deemed ineligible.
Twenty-four percent of those assessed were eligible for the study. Participants were enrolled 3-4 weeks after admission to residential treatment. Intervention clients started the BRIGHT group within 2 weeks after study enrollment. The study was approved by the RAND Corporation Institutional Review Board and all subjects provided written informed consent.
Assessments
Subjects completed a semi-structured baseline interview which included an assessment of a current depressive disorder using the Composite International Diagnostic Interview (CIDI).17 We selected the CIDI as it does not require clinical training to administer or score. We used the Addiction Severity Evaluation Indices which gathers information over the past-12 month period to assess alcohol and drug use severity.18 The Timeline Followback Method (TLFB)19 was used to capture past 30-day alcohol frequency and intensity, and questions from the Addiction Severity Index (ASI) were used to capture past 30-day use of the following substances: heroin, methadone, other opiates/analgesics, barbiturates, sedatives/hypnotics/tranquilizers, cocaine, amphetamines, cannabis/marijuana, hallucinogens, inhalants and polydrug use. The TLFB and ASI have been shown as reliable and valid measures of alcohol and drug use.20-24
We measured functioning using the Short Form-12 version 2 (SF-1225). We also measured demographic characteristics, along with mental health and substance abuse treatment utilization. Race/ethnicity was asked using the categories that conformed to the National Institutes of Health reporting standards. Primary outcomes were change in depression symptoms using the BDI-II and mental health functioning measured using the mental health composite score of the SF-12. Primary substance use outcomes included percent of days of alcohol and substance used out of days available for use (e.g., not institutionalized). Participants received $20 for completing the baseline interview. Extensive contact information and likely places the participant might be found if s/he were to leave treatment were collected to aid in participant tracking.
Three months after the baseline interview, the first follow-up interview was administered by survey field staff, corresponding to the conclusion of the intervention. Because at this time intervention clients were asked additional questions about their experience with the intervention, interviewers were not blind to study condition. At that time, new detailed tracking information was obtained. Three months later (i.e., approximately 6 months after the baseline interview and 3 months after intervention completion) a second follow-up interview was administered. Participants received $30 for completing the 3-month and the 6-month post-baseline interviews. In both these interviews, baseline measures of study outcomes were repeated.
Intervention condition
The BRIGHT intervention is a group CBT for depression for clients in substance abuse treatment. It consists of 16 two-hour sessions, divided into 4 modules: Thoughts, Activities, People and Substance Abuse. We adapted the intervention from an existing CBT for depression manual.9, 26, 27 Our adaptation sought to improve the intervention’s appropriateness for clients in residential treatment and to increase the likelihood that substance abuse counselors could successfully implement the intervention. We integrated examples dealing with alcohol and substance abuse, added the fourth module to focus on the connections between thoughts, behaviors, mood and substance abuse, and added guidance and structure to the sessions. In addition, we added a 45-min individual “orientation” session prior to the start of group, designed to increase motivation and retention, and which included elements of motivational interviewing28 and role induction29. The BRIGHT group was delivered two times per week; thus, the intervention lasted 8 weeks. Enrollment into the group was semi-open, and new clients could enter the group at the beginning of each of the 4 modules. Previous work indicated that effectiveness was independent of initial treatment focus.30 While participating in the BRIGHT group, other BHS group commitments were reduced accordingly (i.e., BRIGHT participation counted as two BHS groups per week), suggesting that all clients should have received the same number of group sessions per week.
Intervention Dosage
Clients who were assigned to BRIGHT attended a mean of 10.5 sessions (SD=5.5) and 69% attended at least half of the 16 sessions
Counselor Training and Fidelity
To reduce contamination, the intervention was provided by BHS outpatient counselors who traveled to the residential sites to deliver the two-hour intervention and then returned to their outpatient settings. Outpatient counselors had no contact with UC clients and only interacted with residential staff to coordinate care for intervention clients. We trained 5 counselors who had an average of 4 years of experience as counselors; none had specialty mental health credentials. Four counselors were certified by the state of California as substance abuse counselors. Counselors received two days of didactic training, followed by practice leading the intervention once in their outpatient setting coupled with weekly supervision from a licensed clinical psychologist, followed by an additional one-day booster training prior to delivering the intervention to study participants.
To encourage fidelity, sessions were coded for adherence and competence, with results provided back to the supervisors to inform ongoing supervision. All sessions were digitally recorded and 33% of sessions (N=80) were coded by at least one trained rater using measures adapted for this intervention. The adherence measure is specific to each session and requires ratings on a 4-point scale (ranging from 0 to 3) of how adequately group leaders covered each session element. A score of 2 or higher indicates adequate adherence to each session element. The 12-item competence measure was adapted from the Cognitive Therapy Adherence and Competence Scale.31 Items are rated on a 7-point scale (0-6), with an average score of 4 indicating competent CBT delivery. To account for the high proportion of items with high prevalence and for possible disagreement between raters with respect to baseline rates of each measure, we estimated interrater reliability using the prevalence-adjusted bias-adjusted kappa (PABAK)32 based on 33 double-coded sessions (13% of all delivered sessions). PABAK estimates ranged from 0.33-0.88 for adherence items (average=0.68) and 0.15-0.94 (average 0.58) for competence items, indicating moderate to substantial agreement among the three raters.33 The average adherence rate was 94% across all coded sessions, suggesting high adherence to the treatment. The average competence score, across all coded sessions was 4.1, indicating counselors were competently delivering CBT.31
Usual Care
We conducted annual site visits to assess organizational functioning and determine whether usual care treatment differed across sites. We conducted focus groups with assessment, admission and counseling staff. Afterwards, we administered a pen and paper questionnaire 34,35 that staff completed anonymously to assess organizational functioning. We also conducted yearly, semi-structured qualitative interviews with agency administrative leaders to ascertain information about staffing and training across sites. Findings from the organizational functioning surveys suggested that overall the sites did not significantly differ from each other or across the study years.36 We also learned that all staff were required to receive the same agency-wide training. Treatment (i.e., usual care) across the sites was standardized, clients experienced similar enrollment procedures and participated in individual substance abuse treatment counseling, group therapy, vocational skills training, AA/NA/CA meetings, recreational therapy, and family services. Residential staff were instructed to follow their usual mental health care procedures of referring clients with severe mental health conditions to a community mental health provider for evaluation. These results suggested that it may be appropriate to aggregate the data across sites in our analyses of client outcomes.
Data Analysis
We analyzed outcomes using an intent-to-treat approach, in which data from all enrolled participants were analyzed. We compared baseline characteristics of clients assigned to the BRIGHT and UC conditions using chi-squared tests for categorical characteristics and t-tests for continuous variables. Respondents and non-respondents of both follow-up surveys were also compared. Our primary mental health outcomes were the BDI-II score and SF-12, which we examined at 3-months and 6-months post-baseline. Each mental health outcome was modeled using mixed effects regression modeling. Random client effects accounted for the non-independence, or clustering, of outcomes repeatedly observed for clients at 3-months and 6-months post-baseline. A multiple membership modeling approach was used to account for the clustering of outcomes among those who attended group CBT sessions together given the semi-open enrollment, which involved including random CBT session effects in the model and estimating the client-specific session effect as an average of the random session effects for those sessions attended by the client.37, 38 The baseline value corresponding to the outcome was entered into the model as a covariate and centered to have mean zero to allow for interpreting other model coefficients as the effect for a client with average covariate values. For the models of BDI-II and SF-12, an indicator variable of intervention assignment, follow-up wave (3 months or 6 months post-baseline), and an interaction of these two measures were included as predictor variables. Intervention effects on BDI-II and SF-12 at 3- and 6-month post-baseline interviews were estimated from these coefficients and tested using two-sided t-tests, while the overall intervention effect over the full follow-up period was tested using a likelihood ratio test.39
We used a sensitivity analyses, conducted to test whether controlling for site changed the statistical significance of treatment effect estimates, to confirm that data across sites could be aggregated for analysis. We also calculated the proportion of clients in each study condition whose depressive symptoms were minimal (BDI-II<=13)13 and compared the proportion with minimal symptoms in each condition at the two follow-up points.
Our primary substance use outcomes were number of days used alcohol of days available, and self-reported use of problem substances on days available for use (i.e., when client was not institutionalized) during past 30 days. We examined these outcomes only at the 6-month follow-up because the majority of subjects (70%) were institutionalized (mostly in the residential treatment program) at the 3-month post-baseline time point. Analyses of percent of days used alcohol or percent days used problem substance out of days available were performed only on clients with any days available for use in the 30-day window (65% of the sample). We conducted a chi-squared test to compare the percent of clients in BRIGHT versus UC having zero days available for use to assess the comparability of AOD users in BRIGHT versus UC. We compared 6-month post-baseline AOD use measures for BRIGHT versus UC conditions using t-tests, as the estimated the variance component for CBT session attendance from the mixed regression model was zero and regression diagnostics of regression models that included baseline AOD use as covariates indicated severe violations of key model assumptions that were not corrected by data transformations.40
Results
Baseline Characteristics
No statistically significant differences between the UC and BRIGHT condition were found on demographic, mental health, or substance use characteristics. Participants were ethnically diverse (22% African American, 34% Caucasian, 30% Hispanic, 14% other/mixed) and 52% were male. The average age was 36.2 (SD =10.3) years old. Most clients were single (81.6%) with 11.9 (SD = 2.0) years of education. Most were unemployed (83.6%) and 18.4% reported being arrested in the month prior to treatment entry.
Mean BDI-II scores were in the clinically severe range (mean = 33.5, SD = 9.2) and 45.8% had a past-12 month depressive disorder. Mental health functioning (SF-12) scores were almost two standard deviations below the population norm (mean = 31.9, SD = 11.0). Nineteen percent of the cohort reported taking antidepressant medication, and 13% reported receiving individual psychotherapy in the month prior to entering residential treatment.
Sixty-six percent of the sample reported problem alcohol use. The mean number of drinks on a drinking day was 7.1 (SD = 8.7). The sample reported using a problem substance 16.3 days (SD = 11.9) in the month prior to entering treatment. The most commonly reported substance was amphetamines (36.8%), followed by cocaine (20.4%), alcohol (15.4%), and heroin (12.4%). The mean ASI alcohol evaluation index score was 54.1 (SD = 9.8) and the mean ASI drug evaluation index score was 47.5 (SD = 7.5). Evaluation indices are transformed such that mean = 50 and SD = 10, indicating that the substance abuse severity of the sample is typical to other patients entering substance abuse treatment.20
Two-hundred sixty (87.0%) and 256 clients (85.6%) completed 3- and 6-month post-baseline surveys. Response rates for clients in UC versus BRIGHT did not significantly differ at either wave (p = 0.55 and p = 0.77, respectively). Responders were not significantly different from non-responders at either wave with respect to baseline characteristics. Treatment effects did not significantly vary across the four sites.
Depression outcomes
At the 3- and 6-month post-baseline interviews, BRIGHT clients reported significantly fewer depressive symptoms; Table 1 shows the difference between BRIGHT and UC clients on average BDI-II score at each follow-up. The intervention was associated with increased overall mental health functioning. Figures 2 and 3 show the change over time of these two measures for the intervention and comparison conditions, conditional on a client starting at baseline with average scores on these measures. Inclusion of antidepressant medication use as a covariate did not alter the statistical significance of these treatment effects. Clients in the two conditions did not differ in terms of their self-reported receipt of individual counseling for a mental or emotional problem outside of substance abuse residential treatment at the 3- and 6-month post-baseline interviews (3 months: CBT = 21% vs. UC = 28%, p = 0.20; 6-months: CBT = 19% vs. UC = 26%, p = 0.29). At 3-months post-baseline, BRIGHT clients had depressive symptoms in the ‘mild’ range (mean BDI-II = 15.6), while UC clients were in the ‘moderate’ range (mean BDI-II = 21.9). Symptoms continued to decrease in both conditions at 6-months post-baseline.
Table 1.
Effect of group cognitive behavioral therapy versus usual care on outcomes
| Intervention effect at: | Variance components for random effects: | |||||
|---|---|---|---|---|---|---|
| 3 months | 6 months | LLstat (2 df) | Intercept (client) | Session | Residual | |
| Mental health outcomes | ||||||
| Change in Beck Depression Inventory-II score | -6.3**** | -5.6*** | 16.3*** | 64.2**** | 106.2 | 72.3**** |
| Change in Short Form-12 version 2 mental health score | 6.3*** | 4.6** | 16.3*** | 47.7**** | 94.3 | 92.2**** |
| Substance use outcomes | ||||||
| Change in percent of days used alcohol on days available for clients with at least one day available to use, past 30 days | n/a | -8.9* | n/a | n/a | 0 | 800.6**** |
| Change in percent of days used problem substance on days available for clients with at least one day available to use, past 30 days | n/a | -11.6* | n/a | n/a | 0 | 975.3**** |
p<0.0001;
p<0.001;
p<0.01;
p<0.05.
LLstat: log-likelihood ratio statistic for testing the total intervention effect for outcomes examined at 3- and 6-months.
Figure 2.
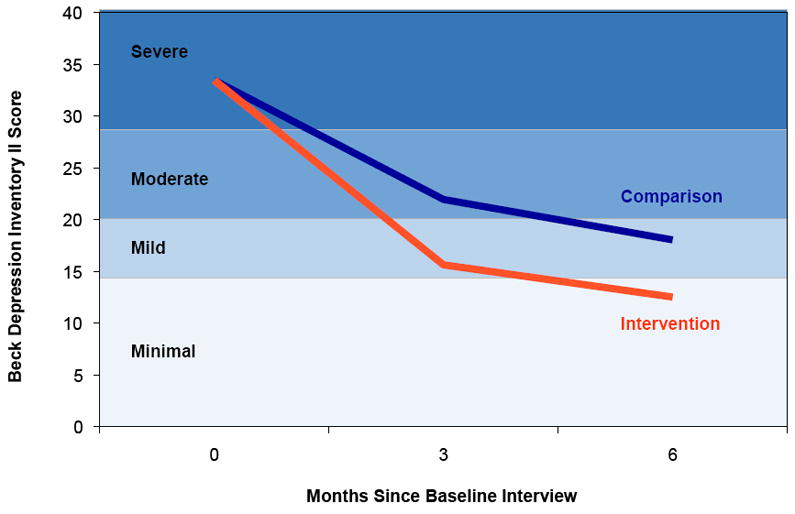
Conditional change in BDI-II score over time
Figure 3.
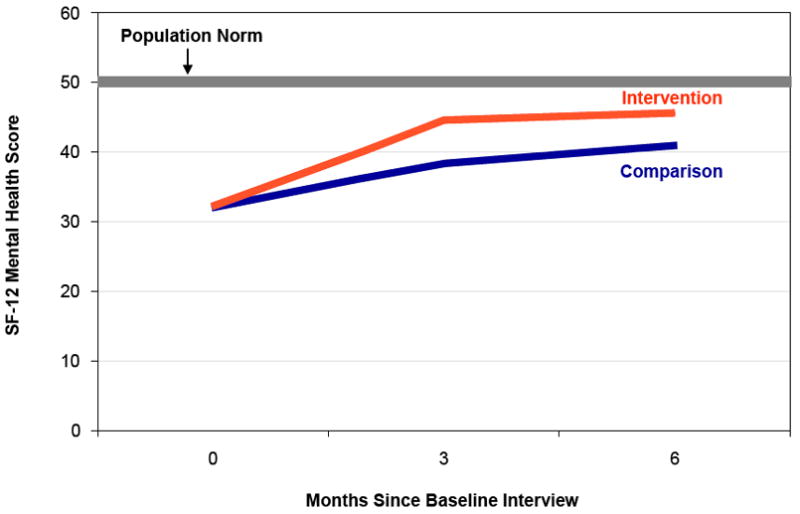
Conditional change in SF-12 mental health score over time
At both the 3-month and 6-month post-baseline interviews, more BRIGHT clients had minimal symptoms, as compared to the UC group (3-months: 55.8 % vs. 33.6%; p<0.001; 6-months: 63.9% vs. 43.8%, p<.0.001).
In addition to BRIGHT clients reporting significantly fewer depressive symptoms than UC clients, it is also notable that all clients reduced their depressive symptoms from baseline. The mean BDI-II score of BRIGHT clients went from 33.5 to 12.5 at 6-months and UC client scores went from 33.5 to 18.1, using the sample mean estimated from the model.
Substance Use Outcomes
The UC and BRIGHT conditions had similar percentages of clients having no days available for substance use at 6 months (36% vs. 34%, p=0.63). Among the clients with days available, BRIGHT clients reported fewer drinking days at 6-months and fewer days of problem substance use compared to UC (Table 1). The percent days of substance use for BRIGHT and UC groups at each follow-up is shown in Figure 4.
Figure 4.
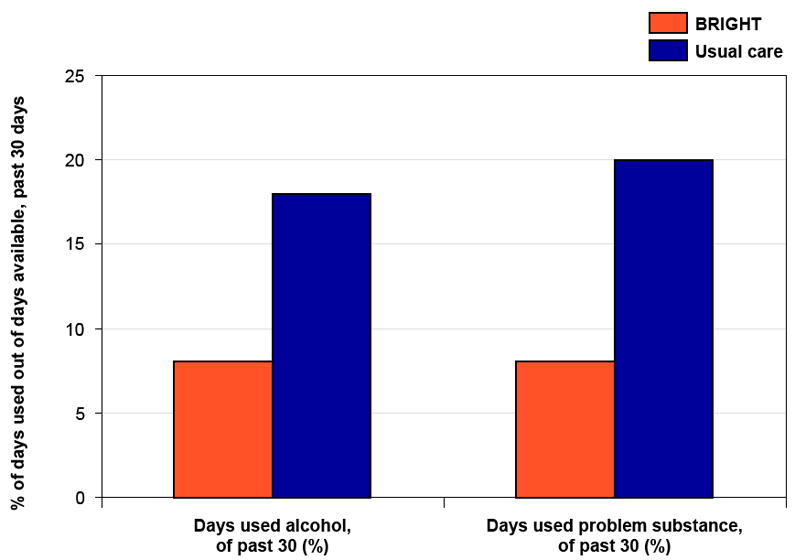
Substance use at 6 months
Discussion
The BRIGHT trial has several important findings. We show that providing group CBT for depression to clients with persistent depressive symptoms receiving residential substance abuse treatment is associated with better improvement in both depression and substance use outcomes. While all clients in our study, regardless of study condition, reduced their levels of depressive symptoms, intervention clients experienced greater decreases and their mental health functioning approached population norms. Among clients who had the opportunity for substance use at the 6-month post-baseline interview, intervention clients reduced their use by more than half compared to UC clients. It is notable that despite being a specific treatment for depression, the intervention was associated with clinically and statistically significant improvements in both mental health and substance use outcomes.
Few studies focus on the treatment of individuals with depression entering substance abuse treatment, and the majority of these examine pharmacotherapy.41 To our knowledge, this is the first large-scale trial of a psychosocial treatment for depression provided within standard substance abuse treatment, and adds to the small literature on effective treatments for individuals with co-occurring affective and substance use disorders. Apart from one study of interpersonal psychotherapy with 26 patients and another study of individual CBT with 35 patients, previous studies of psychosocial treatments have all included pharmacotherapy provided by a psychiatrist, a resource unavailable to most publicly funded substance abuse providers.42-45 While the CBT study found that individual CBT significantly lowered both drinking outcomes and depressive symptoms among alcoholics, the sample was less severely ill– e.g., baseline BDI-II was greater than or equal to 10, (versus 17) and only a single participant met criteria for major depression.42 Our findings extend these findings to include a group format, drug users in addition to alcoholics, and clients with severe depressive symptoms.
Our study addresses a critical need to develop and test integrated models of care suitable for the public-sector substance abuse treatment system. Lack of access to efficacious depression treatment for substance abusers is an important public health problem. Rates of current major depression are 2-4 times higher among substance abusers than in the general population,1, 46 affecting 15-35% of people seeking substance abuse treatment.47 Persons with co-morbid depression and substance use disorders experience greater impairment48 and worse outcomes than persons with only one of these disorders.49-51 Although current guidelines state that services for individuals with co-morbid substance use and mental disorders should be available regardless of setting, studies have shown that few public sector substance abuse treatment organizations are able to provide for the mental health needs of individuals with comorbid disorders.52, 53 Fewer than 9% of U.S. adults with a probable co-occurring disorder were able to access both mental health and substance abuse treatment.54
Public-sector programs typically do not provide mental health services because few substance abuse providers have qualified mental health professionals on staff,8, 55 and most do not have the funding mechanisms or resources to hire mental health professionals. In order to increase access and improve outcomes for individuals with comorbidity, interventions that use available resources need to be developed and evaluated. Because BRIGHT was implemented using typical substance abuse counselors, we address a critical limitation of the current system.8 A cost analysis will be reported elsewhere. The study demonstrates that it is possible to develop the capacity of substance abuse programs to deliver evidence-based mental health care by enhancing the skills and expanding the clinical roles of substance abuse counselors. If more broadly implemented, this approach could increase access to effective mental health care for the many individuals who enter the substance abuse treatment system with co-occurring persistent depressive symptoms. Moreover, because most substance abuse treatment occurs in a group format, our adaptation of group CBT for depression is consistent with providers’ expectations of what a usable treatment looks like.
Results from our study should be generalizable to the large population of individuals with persistent depressive symptoms entering residential treatment. Our study population included diverse cultures and ethnicities, and study sites were geographically spread across Los Angeles County. Participants were typical of clients enrolled in public-sector treatment, as most were single, unemployed, and indigent. To increase generalizability, we included clients with a range of severity and disorders, and had few exclusion criteria. About half had a current major depressive disorder. We also included individuals on medication as long as they continued to experience depressive symptoms. Given the difficulty of distinguishing between a substance-induced depressive disorder and an independent depressive disorder, initiating a treatment that is effective for both and which does not have the liability of medication side effects is advantageous.
The observed rates of CBT treatment attendance and completion in the absence of external incentives suggest that both clients and staff perceived the treatment to be acceptable and that the intervention is feasible. For example, we relied on the residential staff, who did not receive any training or exposure, to ensure that clients assigned to the BRIGHT condition received the intervention. In practice, this meant they had to remind clients, reschedule appointments, and ensure clients were on time. In addition, residential staff had to keep track of clients entering treatment in order to screen and enroll all eligible clients. Continued support for screening and client participation in the intervention was demonstrated by our low refusal rates and attendance in the intervention groups. Consistent with the improvement in outcomes, counselors without previous exposure to CBT for depression or to other depression treatments were able to deliver the treatment with acceptable levels of adherence and competence.
Our study has several limitations. Despite our efforts to develop and evaluate a treatment tied to the available resources of substance abuse providers, additional resources were required. Counselors went through significant training and weekly supervision by a PhD level psychotherapist, which may be more training and supervision than public programs can provide. BRIGHT was led by two counselors and the group size was limited to 10 which also increases the resources needed. We did not conduct a randomized trial, although our quasi-experimental study design, in which sites were assigned to alternate between the intervention and usual care conditions, minimized the chance of unmeasured site or subject characteristics influencing outcomes, and we did not observe differences by either site or intervention status. In the last year of the study we centralized the delivery of the intervention; clients were transported to a single site to receive the intervention. While this could have resulted in contamination, there were no differences in treatment attendance or outcomes associated with this change, and we continued to see a difference between our intervention and comparison conditions. We tested BRIGHT in a residential setting in which clients were expected to stay 3-6 months, and it is unknown whether the intervention will be feasible in 28-day programs or effective in outpatient settings. Small residential programs may not have sufficient clients to support a group. More work is needed to test the feasibility of BRIGHT in different settings.
We did not confirm self-report with urinalysis or a clinical interview and the lack of more thorough screening for co-morbid conditions is a limitation. Follow-up assessments were also unblinded to treatment allocation. Subjects may have under-reported their substance use or depression, although previous studies suggest the validity of self-reported mental health and substance abuse outcomes in similar populations, and the measures we used are based on previously-validated scales.21, 22, 56-59 We do not know whether the treatment influenced both depression and substance abuse directly, or whether the improvements in depression led to the improvements in substance use. This is an important area for further study. While all clients should have received the same amount of total residential treatment, it is probable that BRIGHT clients perceived themselves to be receiving increased clinical attention.
Taken together, our results provide support for a new model of integrated care suitable for substance abuse programs. Integration exists on a continuum, ranging from the co-location of mental health and substance abuse providers to integrated treatment teams staffed by experts in both disciplines. However co-location has not been shown to be effective,7 and integrated treatment teams are expensive to deliver and may not be cost-effective for individuals with less severe mental disorders. Future studies should include longer follow-up times and address the challenges of more broadly implementing this model of integrated care.
Acknowledgments
We would like to acknowledge the contributions of Suzanne Wenzel (RAND Corporation and University of Southern California School of Social Work), Suzanne Perry (RAND Corporation) Susan Ridgely (RAND Corporation), Stephanie Woo (Pepperdine University), and Ricardo Muñoz (University of California San Francisco, San Francisco General Hospital, San Francisco State University). We would also like to acknowledge the helpful contributions of Lynn Polite and Jacob Solomon.
We would also like to acknowledge Shirley Summers (Behavioral Health Services) and Behavioral Health Services outpatient counselors Conswaila Jackson, Elizabeth Macias, Sabrina Navarette, James B. Thompson, and Pamela Webber-Sandres.
Grant support: This research was funded by 1R01AA014699-01A2
Footnotes
Previous presentation: Portions of this have been previously presented at the International Conference on the Treatment of Addictive Behaviors, Santa Fe, NM: February 2010 by Sarah B. Hunter. The presentation was titled, “Group CBT for depression in substance abuse treatment: How does it work?”
Financial disclosures:Dr. Katherine Watkins reports no competing interests
Dr. Sarah Hunter reports no competing interests
Dr. Kimberly Hepner reports no competing interests
Dr. Susan Paddock reports no competing interests
Erin de la Cruz reports no competing interests
Annie Zhou reports no competing interests
Jim Gilmore reports no competing interests
I, Katherine E. Watkins, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Katherine E. Watkins, RAND Corporation, Santa Monica, CA; kwatkins@rand.org
Sarah B. Hunter, RAND Corporation, Santa Monica, CA; sarah_hunter@rand.org
Kimberly A. Hepner, RAND Corporation, Santa Monica, CA; kimberly_hepner@rand.org
Susan M. Paddock, RAND Corporation, Santa Monica, CA; susan_paddock@rand.org
Erin de la Cruz, RAND Corporation, Santa Monica, CA; edelacru@rand.org
Annie J. Zhou, RAND Corporation, Santa Monica, CA; zhou@rand.org
Jim Gilmore, Behavioral Health Services Inc., Los Angeles, CA; jgilmore@bhs-inc.org
References
- 1.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004 Aug;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–768. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD, editors. The global burden of disease: A comprehensive assessment of mortality and disability from disease, injuries, and risk factors, in 1990 and projected to 2020. Cambridge, MA: Harvard School of Public Health, on behalf of the WHO and the World Bank; 1996. [Google Scholar]
- 4.Clark HW, Power AK, Le Fauve CE, Lopez EI. Policy and practice implications of epidemiological surveys on co-occurring mental and substance use disorders. J Subst Abuse Treat. 2008 Jan;34(1):3–13. doi: 10.1016/j.jsat.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 5.Boden MT, Moos R. Dually diagnosed patients’ responses to substance use disorder treatment. J Subst Abuse Treat. 2009;37(4):335–345. doi: 10.1016/j.jsat.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grella CE, Stein JA. Impact of program services on treatment outcomes of patients with comorbid mental and substance use disorders. Psychiatr Serv. 2006;57(7):1007–1015. doi: 10.1176/appi.ps.57.7.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burnam A, Watkins KE. Substance abuse with mental disorders: Specialized public systems and integrated care. Health Aff (Millwood) 2006;25(3):648–658. doi: 10.1377/hlthaff.25.3.648. [DOI] [PubMed] [Google Scholar]
- 8.Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: issues and prospects. J Subst Abuse Treat. 2008 Jan;34(1):36–47. doi: 10.1016/j.jsat.2006.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muñoz RF, Mendelson T. Toward evidence-based interventions for diverse populations: The San Francisco General Hospital prevention and treatment manuals. J Consult Clin Psychol. 2005 Oct;73(5):790–799. doi: 10.1037/0022-006X.73.5.790. [DOI] [PubMed] [Google Scholar]
- 10.Oei TP, Dingle G. The effectiveness of group cognitive behaviour therapy for unipolar depressive disorders. J Affect Disord. 2008 Apr;107(1-3):5–21. doi: 10.1016/j.jad.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 11.Hohmann AA, Shear KM. Community-based intervention research: Coping with the ‘noise’ of real life in study design. Am J Psychiatry. 2002;159(2):201–207. doi: 10.1176/appi.ajp.159.2.201. [DOI] [PubMed] [Google Scholar]
- 12.Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. J Am Med Assoc. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 13.Beck A, Steer R, Brown G. BDI-II, Beck Depression Inventory: manual. 2. Boston: Harcourt Brace; 1996. [Google Scholar]
- 14.Buckley TC, Parker JD, Heggie J. A psychometric evaluation of the BDI-II in treatment-seeking substance abusers. J Subst Abuse Treat. 2001 Apr;20(3):197–204. doi: 10.1016/s0740-5472(00)00169-0. [DOI] [PubMed] [Google Scholar]
- 15.Sloan K, Kivlahan D, Saxon A. Detecting bipolar disorder among treatment-seeking substance abusers. Am J Drug Alcohol Abuse. 2000;26(1):13–23. doi: 10.1081/ada-100100587. [DOI] [PubMed] [Google Scholar]
- 16.Dennis ML, White MK, Titus JC, Unsicker JI. Short Blessed Scale Exam. Global Appraisal of Individual Needs: Trainer’s Training Manual and Resources (July 2006 version) Bloomington, IL: Chestnut Health Systems; 2006. [Google Scholar]
- 17.Walters E, Kessler R, Nelson C, Mroczek D. Composite International Diagnostic Interview (CIDI) 2.1. Geneva, Switzerland: World Health Organization (WHO); 1998. [Google Scholar]
- 18.McLellan A, Carise D, Coyne T. Addiction Severity Index (ASI) 5. Philadelphia, PA: Treatment Research Institute; 2005. [Google Scholar]
- 19.Sobell LC, Sobell MB. Alcohol timeline followback users’ manual. Toronto: Addiction Research Foundation; 1995. [Google Scholar]
- 20.Alterman AI, McDermott PA, Cook TD, Metzgera D, Rutherford MJ, Cacciola JS, Lawrence S, Brown J. New scales to assess change in the addiction severity index for the opioid, cocaine, and alcohol dependent. Psychol Addict Behav. 1998;12(4):233–246. [Google Scholar]
- 21.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. J Consult Clin Psychol. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 22.Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behav Res Ther. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- 23.Sobell LC, Sobell MB. Validity of self-reports in three populations of alcoholics. J Consult Clin Psychol. 1978 Oct;46(5):901–907. doi: 10.1037//0022-006x.46.5.901. [DOI] [PubMed] [Google Scholar]
- 24.Sobell LC, Sobell MB. Convergent validity: An approach to increasing confidence in treatment outcome conclusions with alcohol and drug abusers. In: Sobell LC, Sobell MB, Ward E, editors. Evaluating alcohol and drug abuse treatment effectiveness: Recent advances. New York: Pergamon Press; 1980. [Google Scholar]
- 25.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996 Mar;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Lewinsohn P, Munoz R, Youngren M, Zeiss A. Control Your Depression. New York, NY: Prentice Hall Press; 1986. [Google Scholar]
- 27.Muñoz R, Ippen C, Rao S, Le H, Dwyer E. Manual for Group Cognitive-Behavioral Therapy of Major Depression: A Reality Management Approach. San Francisco: Cognitive Behavioral Depression Clinic, San Francisco General Hospital, University of California, San Francisco; 2000. [Google Scholar]
- 28.Miller WR, Rollnick S. Motivational Interviewing. New York: Guilford; 1991. [Google Scholar]
- 29.Stark MJ, Kane BJ. General and specific psychotherapy role induction with substance-abusing clients. Int J Addict. 1985;20(8):1135–1141. doi: 10.3109/10826088509056355. [DOI] [PubMed] [Google Scholar]
- 30.Drapkin ML, Tate SR, McQuaid JR, Brown SA. Does initial treatment focus influence outcomes for depressed substance abusers? J Subst Abuse Treat. 2008 Oct;35(3):343–350. doi: 10.1016/j.jsat.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barber JP, Liese B, Abrams MJ. Development of the Cognitive Therapy Adherence and Competence Scale. Psychotherapy Research. 2003;13(2):205–221. [Google Scholar]
- 32.Byrt T, Bishop J, Carlin J. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46:423–429. doi: 10.1016/0895-4356(93)90018-v. [DOI] [PubMed] [Google Scholar]
- 33.Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 34.Lehman WE, Greener JM, Simpson DD. Assessing organizational readiness for change. J Subst Abuse Treat. 2002 Jun;22(4):197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- 35.Simpson D. Organizational readiness for stage-based dynamics of innovation implementation. Res Soc Work Pract. 2009;19(5):541–551. [Google Scholar]
- 36.Hunter SB. Group CBT for depression in substance abuse treatment: how does it work?. International Conference on the Treatment of Addictive Behaviors; Santa Fe, NM. 2010. [Google Scholar]
- 37.Browne WJ, Goldstein H, Rasbash J. Multiple membership multiple classification (MMMC) models. Stat Modelling. 2001 July 1;1(2):103–124. [Google Scholar]
- 38.Carey K. A multilevel modeling approach to analysis of patient costs under managed care. Health Econ. 2000;9:435–446. doi: 10.1002/1099-1050(200007)9:5<435::aid-hec523>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 39.Fitzmaurice G, Laird NM, Ware J. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- 40.Weisberg S. Applied Linear Regression. 3. Hoboken, NJ: Wiley/Interscience; 2005. [Google Scholar]
- 41.Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37(2):127–137. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. J Consult Clin Psychol. 1997 Oct;65(5):715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hesse M. Integrated psychological treatment for substance use and co-morbid anxiety or depression vs. treatment for substance use alone. A systematic review of the published literature. BMC Psychiatry. 2009;9(1):6. doi: 10.1186/1471-244X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Markowitz J, Kocsis J, Christos P, Bleiberg K, Carlin A. Pilot study of interpersonal psychotherapy versus supportive psychotherapy for dysthymic patients with secondary alcohol abuse or dependence. J Nerv Ment Dis. 2008;196(6):468–474. doi: 10.1097/NMD.0b013e31817738f1. [DOI] [PubMed] [Google Scholar]
- 45.Tiet Q, Mausbach B. Treatments for patients with dual diagnosis: a review. Alcohol Clin Exp Res. 2007;31(4):513–536. doi: 10.1111/j.1530-0277.2007.00336.x. [DOI] [PubMed] [Google Scholar]
- 46.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of Major Depressive Disorder: Results From the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 47.Grant B. The influence of cormorbid major depression and substance use disorder on alcohol and drug treatment: Results of a national survey. Natl Inst Drug Abuse Res Monogr Ser. 1997;172:4–15. [PubMed] [Google Scholar]
- 48.Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders: Findings from the Australian National Survey of Mental Health and Well Being. Drug Alcohol Depend. 2002;68(3):299–307. doi: 10.1016/s0376-8716(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 49.Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59(4):375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 50.Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Sokero TP, Isometsa ET. Severity and comorbidity predict episode duration and recurrence of DSM-IV major depressive disorder. J Clin Psychiatry. 2004 Jun;65(6):810–819. doi: 10.4088/jcp.v65n0612. [DOI] [PubMed] [Google Scholar]
- 51.Watkins KE, Paddock SM, Zhang L, Wells KB. Improving care for depression in patients with comorbid substance misuse. Am J Psychiatry. 2006 Jan;163(1):125–132. doi: 10.1176/appi.ajp.163.1.125. [DOI] [PubMed] [Google Scholar]
- 52.Ducharme LJ, Knudsen HK, Roman PM. Availability of integrated care for co-occurring substance abuse and psychiatric conditions. Community Ment Health J. 2006 Aug;42(4):363–375. doi: 10.1007/s10597-005-9030-7. [DOI] [PubMed] [Google Scholar]
- 53.Gil-Rivas V, Grella CE. Treatment services and service delivery models for dually diagnosed clients: variations across mental health and substance abuse providers. Community Ment Health J. 2005 Jun;41(3):251–266. doi: 10.1007/s10597-005-5000-3. [DOI] [PubMed] [Google Scholar]
- 54.Watkins KE, Burnam A, Kung FY, Paddock S. A national survey of care for persons with co-occurring mental and substance use disorders. Psychiatr Serv. 2001 Aug;52(8):1062–1068. doi: 10.1176/appi.ps.52.8.1062. [DOI] [PubMed] [Google Scholar]
- 55.Grella CE, Gil-Rivas V, Cooper L. Perceptions of mental health and substance abuse program administrators and staff on service delivery to persons with co-occurring substance abuse and mental disorders. J Behav Health Serv Res. 2004 Jan-Mar;31(1):38–49. doi: 10.1007/BF02287337. [DOI] [PubMed] [Google Scholar]
- 56.Brown J, Kranzler HR, Del Boca FK. Self-reports by alcohol and drug abuse inpatients: factors affecting reliability and validity. Br J Addict. 1992 Jul;87(7):1013–1024. doi: 10.1111/j.1360-0443.1992.tb03118.x. [DOI] [PubMed] [Google Scholar]
- 57.Rush AJ, Carmody TJ, Ibrahim HM, Trivedi MH, Biggs MM, Shores-Wilson K, Crismon ML, Toprac MG, Kashner TM. Comparison of self-report and clinician ratings on two inventories of depressive symptomatology. Psychiatr Serv. 2006 Jun;57(6):829–837. doi: 10.1176/ps.2006.57.6.829. [DOI] [PubMed] [Google Scholar]
- 58.Weiss RD, Najavits LM, Greenfield SF, Soto JA, Shaw SR, Wyner D. Validity of substance use self-reports in dually diagnosed outpatients. Am J Psychiatry. 1998 Jan;155(1):127–128. doi: 10.1176/ajp.155.1.127. [DOI] [PubMed] [Google Scholar]
- 59.Zimmerman M, Coryell W, Wilson S, Corenthal C. Evaluation of symptoms of major depressive disorder. Self-report vs. clinician ratings. J Nerv Ment Dis. 1986 Mar;174(3):150–153. doi: 10.1097/00005053-198603000-00004. [DOI] [PubMed] [Google Scholar]


