Abstract
Complete catheter-tissue contact and permanent tissue destruction are essential for efficient radio-frequency ablation (RFA) during cardiac arrhythmia treatment. Current methods of monitoring lesion formation are indirect and unreliable. The purpose of this study is to evaluate the feasibility of using optical coherence tomography (OCT) catheter to image endocardial wall in actively beating hearts through percutaneous access. We reported the first in vivo intracardiac OCT imaging through percutaneous access with a thin and flexible OCT catheter. This is a critical step toward image-guided RFA in a clinical setting. A cone-scanning forward-viewing OCT catheter was advanced into beating hearts through percutaneous access in four swine. The OCT catheter was steered by an introducer to touch the endocardial wall. We are able to acquire high quality OCT images in beating hearts, observe the polarization-related artifacts induced by the birefringence of myocardium, and readily evaluate catheter-tissue contact. The observations indicate that OCT could be a promising technique for in vivo guidance of RFA.
Keywords: optical coherence tomography, radiofrequency catheter ablation, percutaneous access
Catheter-based radio-frequency ablation (RFA) through percutaneous access is commonly practiced in interventional electrophysiology therapeutic procedures to treat cardiac arrhythmias.1, 2 The goal of catheter RFA is to disrupt abnormal electrical pathways by creating thermal lesions on the endocardial surface of heart, destroying tissue that induces or supports the abnormal pathway. Currently, monitoring of lesion formation is accomplished through indirect means, such as tissue temperature, impedance, and electrograms, which are unreliable for predicting lesion formation because of varied catheter-tissue contact and blood flow around electrodes.3 Physicians do not have in situ guidance to visualize catheter-tissue contact, monitor the successful formation of a lesion or identify critical structures to avoid unintentional damage. Our group has explored the potential of using optical coherence tomography (OCT) to perform real-time guidance and monitoring of RFA therapy.4, 5, 6 We have shown that OCT can monitor catheter-tissue contact and lesion formation through catheter-based endocardial and epicardial OCT imaging of excised tissue on the bench4, 6 and in vivo via an open-chest animal study.5 However, to test the feasibility of intracardiac OCT in a clinical setting, it is important to verify that if diagnostic-quality OCT images can be acquired through remote percutaneous access in the actively beating heart. For percutaneous access, the OCT catheter must be thin enough to be passed through a standard introducer and flexible enough to be remotely steered to access the endocardial wall at various locations in the heart. In this paper, we report the first in vivo intracardiac OCT imaging through percutaneous access in adult female swine using a newly fabricated OCT catheter.
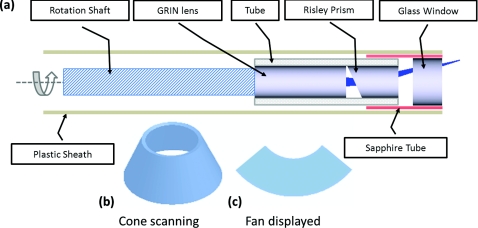
The newly fabricated OCT catheter for in vivo imaging through percutaneous access was based on our previously proposed cone-scanning forward-viewing concept.5, 6 The new design is simpler, smaller in diameter, and rigid length, which allows imaging endocardium through percutaneous access. The schematic of the new fabricated OCT catheter is shown in Fig. 1a. The light beam conducted through the optical fiber is first focused by a gradient-index lens and then deflected by a Risley prism. The focused light spot on the tissue is about 15 μm at full-width at half maximum. All rotating parts were housed in a biocompatible plastic sheath with a tube and a glass window attached at the end of the sheath. The tube served as a bearing to facilitate rotation. The sheath is disposable and can be easily replaced after a single use. The finished OCT catheter has an outer diameter of 2.3 mm (∼7.5 F) and a length of 2 m. A spectral domain OCT system described previously was adapted to acquire OCT images at 10 frames/s with 4500 A-lines per frame at an axial resolution of 15 μm.5, 6 The cone-shaped image can be visualized with true aspect ratio in a fan-shaped display [Fig. 1c].
Figure 1.
Schematic of the cone-scanning forward-viewing OCT catheter with 2.3 mm outer diameter and 12 mm rigid length at the tip (a). The image is acquired in a cone shape (b) but displayed in a fan shape (c).
To demonstrate the feasibility of imaging endocardial tissue through percutaneous access, we performed in vivo imaging in four swines weighing between 38 and 45 kg in the Experimental Interventional Catheterization Laboratory at Case Western Reserve University. The study protocol was reviewed and approved by the Institutional Animal Care and Use Committee of Case Western Reserve University. During the procedure, the swine was anesthetized, underwent endotracheal intubation and mechanical ventilation. The heart rate was maintained at approximately 98 beats/min and was continually monitored during the study. First, a steerable introducer with 8.5 F internal diameter (St. Jude Agilis) was advanced into the heart under fluoroscopic guidance via the right internal jugular vein. Next, the OCT catheter with ∼7.5 F outer diameter was inserted through the introducer. The OCT catheter is very flexible so that it could be steered to access different parts of the endocardial tissue by manipulating the steerable introducer. Similar studies were performed on a total of four swine. OCT images were continuously acquired and displayed in real-time during the catheter placement and selectively recorded at various locations in the right atrium and ventricle.
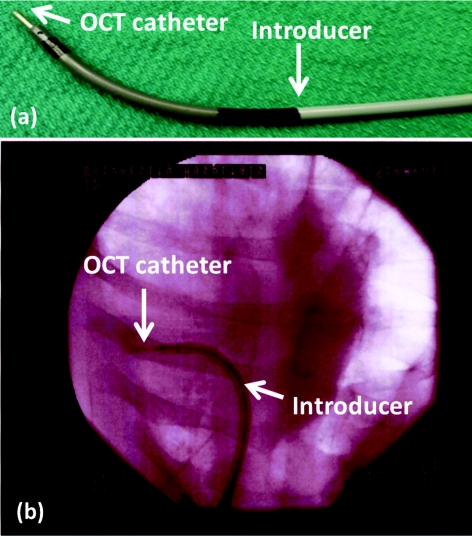
By manipulating the steerable introducer, the OCT catheter was bent and manipulated to contact with the endocardial wall to acquire images. Figure 2a shows a photograph of the steerable introducer with the OCT catheter emerging from the tip. Figure 2b is a fluoroscopic image recorded during in vivo OCT imaging in the beating heart through percutaneous access, where the OCT catheter was significantly bent for imaging.
Figure 2.
(a) Photograph of the steerable introducer with an OCT catheter inserted (arrow); (b) fluoroscopic image recorded during in vivo OCT imaging. The OCT catheter was bent and placed in contact against the endocardial wall.
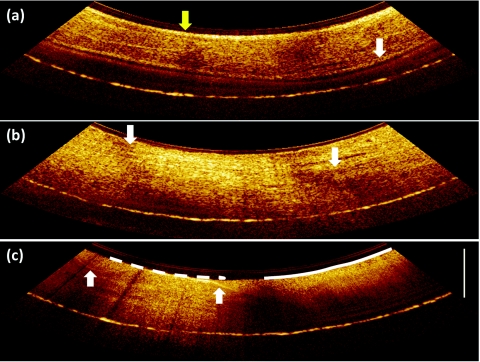
Three representative OCT images are shown in Fig. 3. Figure 3a was acquired in the right atrium. The full thickness of the wall of the atrium was imaged by OCT. The endocardium and epicardium are clearly identified in the image (arrows). The tissue next to the epicardium is also visible. The movie linked with this image shows that high quality images can be continuously acquired in vivo in the actively beating heart. Figure 3b shows an OCT image of the endocardial wall of the right ventricle. Two diffuse dark bands (arrows) are clearly visible in the OCT image. By manipulating a polarization controller in the reference arm of the OCT interferometer, we observed shifting of the dark bands, which confirms that the bands are polarization-dependent and related to the birefringence of the myocardium. We have previously shown that these polarization-dependent bands can be used as a marker to monitor the process of RFA.4 Catheter-tissue contact is another critical factor for efficient RFA. OCT can provide in vivo feedback of catheter-tissue contact during RFA treatment. Figure 3c demonstrates an OCT image acquired with the catheter in partial contact with the tissue. Contact and noncontact are readily differentiated by observing that the OCT appearance of blood is very different than the OCT appearance of myocardial tissue. The imaging depth in blood, i.e., without catheter-tissue contact, is much shallower because of significantly high scattering of the blood, and also lacks the layered structure apparent in myocardium. In addition, the boundary between tissue and blood is visible as the arrows marked in Fig. 3c, where a thin blood layer (around several hundred micrometers) between the catheter and the tissue can be identified. The protocol was repeated in the four swine and successful imaging was achieved in each case.
Figure 3.
(a) OCT image of atrial endocardial wall, visualized transmurally; endocardium (yellow, upper one) and epicardium (white) (relatively bright lines) are marked by arrows, respectively (Video 1); (b) OCT image of ventricular endocardial wall with polarization-dependent bands marked as arrows; (c) OCT image demonstrating incomplete catheter-tissue contact. The segment in contact marked by the dashed line shows a deeper, layered image of myocardium, while the segment not in contact marked by the solid line shows a shallower, homogeneous image of blood. The tissue and blood boundary are marked by the arrows. Scale bar: 1 mm.
The cone-scanning OCT catheter has several unique features. For linear scanning, the imaging range is limited by the diameter of the catheter. However, the imaging range of cone scanning is determined by the circumference of the scanning cone, which is around three times larger than the corresponding linear scan. In addition, the cone scanning catheter is actuated proximally through a remote motor. This eliminates the need for an actuator at the distal tip of the catheter7, 8 and enables a catheter with a short rigid length at the tip, which is essential for achieving great flexibility for accessing endocardial tissue at various locations.
In our previous ex vivo studies, we have shown that the polarization-dependent dark bands are a highly-correlated marker of untreated myocardium, and that the progressive disappearance of this marker indicates the process of RFA lesion formation.5, 6 However, during in vivo percutaneous imaging, we observed that the appearance and position of polarization-dependent dark bands varied rapidly with heart beats. This limits our ability to quantify lesion formation using our previously described image analysis method. Moving forward, this limitation will be addressed by making use of polarization sensitive OCT (PS-OCT) to enable unambiguous monitoring of myocardial birefringence and integrate it with an RFA catheter.
Complete catheter-tissue contact is essential for efficient ablation. Currently, lesion formation is indirectly monitored by electrode temperature, impedance, and delivered power. These indicators are unreliable because of variable tissue contact and blood flow cooling. Our cone-scanning forward-viewing OCT can image all orientations of the tissue and identify even subtle noncontact with very thin blood layer sandwiched between the catheter and the tissue. This information could be useful for orienting the catheter optimally for delivery of RF energy to the tissue. By combining with tissue birefringence change during ablation, OCT will be able to provide a direct imaging guidance during RFA.
In conclusion, we report the first in vivo intracardiac OCT imaging through percutaneous access. Using a new fabricated cone-scanning forward-viewing OCT catheter, we continuously acquired high quality OCT images of the endocardial wall within the right atrium and right ventricle of actively beating adult swine hearts through remote steering. OCT images can penetrate the thin atrial wall, capture polarization artifacts related to myocardium birefringence, and provide in vivo monitoring of catheter-tissue contact. These observations indicate that OCT could be a promising technique for in vivo guidance of RFA. Next, the necessary steps toward “electro-structural” substrate-guided ablation include validating the OCT appearance of critical endocardial and epicardial structures, and implementing real-time PS-OCT for robust monitoring of RFA lesion formation.
Video 1.
OCT imaging of right atrium. (MPEG, 1 MB)
Acknowledgments
The project was supported by the Wallace H. Coulter Foundation, the National Institutes of Health and National Science Foundation (HL085939, HL083048, RR1246, CA114276, and IIP-0917940).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Scheinman M. M., “Catheter ablation: A personal perspective,” J. Cardiovasc. Electrophysiol. 12(9), 1083–1088 (2001). 10.1046/j.1540-8167.2001.01083.x [DOI] [PubMed] [Google Scholar]
- Stevenson W. G., Ellison K. E., Lefroy D. C., and Friedman P. P. L., “Ablation therapy for cardiac arrhythmias,” Am. J. Cardiol. 80(8, Supplement 1), 56G–66G (1997). 10.1016/S0002-9149(97)00714-5 [DOI] [PubMed] [Google Scholar]
- Wittkampf F. H. M. and Nakagawa H., “RF catheter ablation: Lessons on lesions,” Pacing Clin. Electrophysiol. 29(11), 1285–1297 (2006). 10.1111/j.1540-8159.2006.00533.x [DOI] [PubMed] [Google Scholar]
- Fleming C. P., Quan K., Wang H., Amit G., and Andrew M. R., “In vitro characterization of cardiac radiofrequency ablation lesions using optical coherence tomography,” Opt. Express 18(3), 3079–3092 (2010). 10.1364/OE.18.003079 [DOI] [PubMed] [Google Scholar]
- Fleming C. P., Rosenthal N., Rollins A. M., and Arruda M., “First in vivo real-time imaging of endocardial radiofrequency ablation by optical coherence tomography: Implications on safety and the birth of ‘electro-structural’ substrate-guided ablation,” Innovations in Cardiac Rhythm Management 2(3), 199–201 (2011). [Google Scholar]
- Fleming C. P., Wang H., Quan K. J., and Rollins A. M., “Real-time monitoring of cardiac radio-frequency ablation lesion formation using an optical coherence tomography forward-imaging catheter,” J. Biomed. Opt. 15(3), 030516–030513 (2010). 10.1117/1.3459134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munce N. R., Mariampillai A., Standish B. A., Pop M., Anderson K. J., Liu G. Y., Luk T., Courtney B. K., Wright G. A., Vitkin I. A., and Yang V. X. D., “Electrostatic forward-viewing scanning probe for Doppler optical coherence tomography using a dissipative polymer catheter,” Opt. Lett. 33(7), 657–659 (2008). 10.1364/OL.33.000657 [DOI] [PubMed] [Google Scholar]
- Wu T., Ding Z., Wang K., Chen M., and Wang C., “Two-dimensional scanning realized by an asymmetry fiber cantilever driven by single piezo bender actuator for optical coherence tomography,” Opt. Express 17(16), 13819–13829 (2009). 10.1364/OE.17.013819 [DOI] [PubMed] [Google Scholar]